Short abstract
A new humidifier for use during mechanical ventilation in endotracheally intubated patients is described and tested. The humidifier is based on a heat-moisture exchanger, which absorbs the expired heat and moisture and releases it into the inspired air. External heat and water are then added at the patient side of the heat-moisture exchanger, so that the inspired gas should reach 100% humidity (44 mg/l) at 37°C. In bench tests using constant and decelerating inspiratory flow and minute volumes of 3–25 l the device gave an absolute humidity of 41–44 mg/l, and it reduced the amount of water consumed in eight mechanically ventilated patients compared with a conventional active humidifier. During a 24-h test period there was no water condensation in the ventilator tubing with the new device.
Keywords: airway humidification, heated humidifier, intensive care, mechanical ventilation
Abstract
Introduction:
Devices for active humidification of the inspired air in mechanically ventilated patients cause water condensation in the ventilator tubing, which may become contaminated or interfere with the function of the ventilator. The present study describes and tests the performance of a new humidifier, which is designed to eliminate water condensation.
Objectives:
To test the performance of the new humidifier at different ventilator settings in a lung model, and to compare this new humidifier with a conventional active humidifier in ventilator-treated critically ill patients.
Materials and methods:
The humidifier (Humid-Heat; Louis Gibeck AB, Upplands Väsby, Sweden) consists of a supply unit with a microprocessor and a water pump, and a humidification device, which is placed between the Y-piece and the endotracheal tube. The humidification device is based on a hygroscopic heat-moisture exchanger (HME), which absorbs the expired heat and moisture and releases it into the inspired gas. External heat and water are then added to the patient side of the HME, so the inspired gas should reach 100% humidity at 37°C (44 mg H2O/l air). The external water is delivered to the humidification device via a pump onto a wick and then evaporated into the inspired air by an electrical heater. The microprocessor controls the water pump and the heater by an algorithm using the minute ventilation (which is fed into the microprocessor) and the airway temperature measured by a sensor mounted in the flex-tube on the patient side of the humidification device.
The performance characteristics were tested in a lung model ventilated with a constant flow (inspiratory:expiratory ratio 1:2, rate 12–20 breaths/min and a minute ventilation of 3–25 l/min) or with a decelerating flow (inspiratory:expiratory ratio 1:2, rate 12–15 breaths/min and a minute ventilation of 4.7–16.4 l/min). The device was also tested prospectively and in a randomized order compared with a conventional active humidifier (Fisher & Paykel MR730, Auckland, New Zealand) in eight mechanically ventilated, endotracheally intubated patients in the intensive care unit. The test period with each device was 24 h. The amount of fluid consumed and the amount of water in the water traps were measured. The number of times that the water traps were emptied, changes of machine filters, the suctions and quality of secretions, nebulizations, and the amount of saline instillations and endotracheal tube obstruction were recorded. In order to evaluate increased expiratory resistance due to the device, the airway pressure was measured at the end of a prolonged end-expiratory pause at 1 h of use and at the end of the test, and was compared with the corresponding pressure before the experiment. The body temperature of the patient was measured before and after the test of each device.
Results:
Both with constant flow and decelerating flow, the Humid-Heat gave an absolute humidity of 41–44 mgH2O/l at 37°C, with the lower level at the highest ventilation. In the patients, both Humid-Heat and the conventional active humidifier (MR730) maintained temperatures, indicating that they provided the intended heat and moisture to the inspired air. With both devices, the body temperature was maintained during the test period. There was no difference in the amount of secretions, the quality of the secretions and the frequency of suctions, saline instillations or nebulizations between the test periods with the two devices. There was no endotracheal tube obstruction, and after 1 h of use and at the end of the test no increased airway resistance was found with either device. When the MR730 was used, however, the water traps needed to be emptied six to 14 (mean eight) times (total amount of fluid in the traps was 100–300 ml) and the machine filters were changed two to six (mean four) times due to an excessive amount of condensed water with flow obstruction. No condensation of water was found in the tubing with the Humid-Heat. The water consumption was 23–65 ml/h (mean 30 ml/h) with the MR730 and 4–8 ml/h (mean 6 ml/h) with the Humid-Heat (P < 0.0008). The same relations were found when the water consumption was corrected for differences in minute ventilation.
Discussion:
The new humidifier, the Humid-Heat, gave an absolute humidity of 41–44 mg/l at 37°C in the bench tests. The tests in ventilated patients showed that the device was well tolerated and that condensation in the tubing was eliminated. There was no need to empty water traps. The test period was too short to evaluate whether the new device had any other advantages or disadvantages compared with conventional humidifiers.
Introduction
Due to dry medical gases, humidification of the inspired gases is essential during prolonged artificial ventilation in endotracheally intubated patients. Without sufficient humidification the secretions will desiccate and the epithelium of the airway will be injured. This increases the risks of atelectasis and pneumonia [1,2].
Passive heat–moisture exchangers (HMEs), which are based on a hygroscopic condenser principle, usually provide adequate humidity (up to 32 mgH2O/l air) in the inspired gas during ventilator treatment [3,4]. In about 5–10% of the patients, however, with thick secretions for example, active humidifiers that can provide 100% humidity are needed [3,4]. These devices cause free water condensation in the tubing with risks of contamination and of compromising the ventilator function [3,5,6]. To avoid this, a new humidifier, which is a hybrid of a hygroscopic HME and an active humidifier, has been developed.
The aims of the present study were to test the performance of this new humidifier at different ventilator settings in a lung model, and to compare this humidifier with a conventional active humidifier in ventilator-treated critically ill patients.
Materials and methods
The part of the study that involved patients was approved by the local human study ethics committee.
The humidifier, Humid-Heat (Louis Gibeck AB, Upplands Väsby, Sweden; Fig.1), consists of a supply unit with a microprocessor and a water pump, and a humidification device that is placed between the Y-piece and the endotracheal tube. The humidification device is based on a hygroscopic HME, which absorbs the expired heat and moisture and releases it into the inspired gas. External heat and water are then added to the patient side of the HME, so the inspired gas should reach 100% humidity at 37°C (44 mgH2O/l air). The external water is delivered to the humidification device via a pump onto a wick and then evaporated into the inspired air by an electrical heater. The microprocessor controls the water pump and the heater by an algorithm using the minute ventilation (which is entered manually into the microprocessor) and the airway temperature as measured by a sensor mounted in the flex-tube on the patient side of the humidification device. The HME in the device has a dead space of 54 ml and the flex-tube has a dead space of 19 ml. The weight of the humidification device is 79 g.
Figure 1.
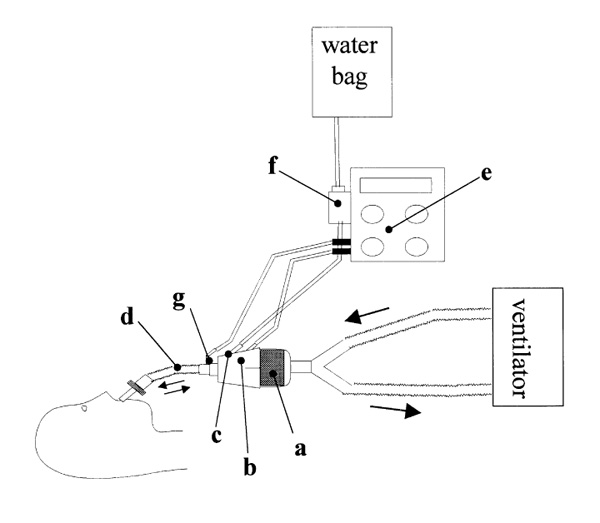
The Humid-Heat device is based on a heat-moisture exchanger (HME), which (a) absorbs the expired heat and moisture and releases it into the inspired gas. External heat (b) and water (c) are then added on the patient side of the HME so that the inspired gas (d) reaches about 100% relative humidity at 37°C. The patient's minute volume is entered into the microprocessor (e) by the operator. The microprocessor uses this information and the actual airway temperature measured by a temperature probe (g) to control a water pump (f) and a heater (b) to deliver the correct amount of water and heat. The arrows indicate the direction of the inspiratory and the expiratory flow.
Lung model tests
The first part of the experiment involved testing of the performance characteristics during constant and decelerating flow in a lung model. The lung model (Fig. 2) was based on the ISO 9360 International Standard, with the exception that the water bath temperature was regulated to maintain a constant temperature of 36 ± 0.5°C. This will give 100% humidity at 35.5 ± 0.5°C in the air expired from the model, simulating the humidity and temperature in the human trachea. The model was ventilated with a constant or a decelerating inspiratory flow by a ventilator (Siemens 900 B, Solna, Sweden) for 90min. The ventilator was fed with pressurized dry air from a gas cylinder. The temperature in the room and in the inspiratory ventilator tubing was maintained at 21°C. The temperature in the expiratory ventilator tubing was 21–22°C. During the constant flow ventilation the ventilator was set at a minute ventilation of 5–25l/min, an inspiratory:expiratory ratio of 1:2, and a rate of 12, 15 or 20 breaths/min. To obtain a decelerating flow, the pressure in the ventilator bellows (machine pressure) was reduced from 60 to 20 and 38 cmH2O, producing an almost constant inspiratory pressure in the ventilator tubing and tidal volumes of 390 and 1370 ml, respectively. The rate was 12 or 15 breaths/min and the minute ventilation was 4.7–16.4l.
Figure 2.
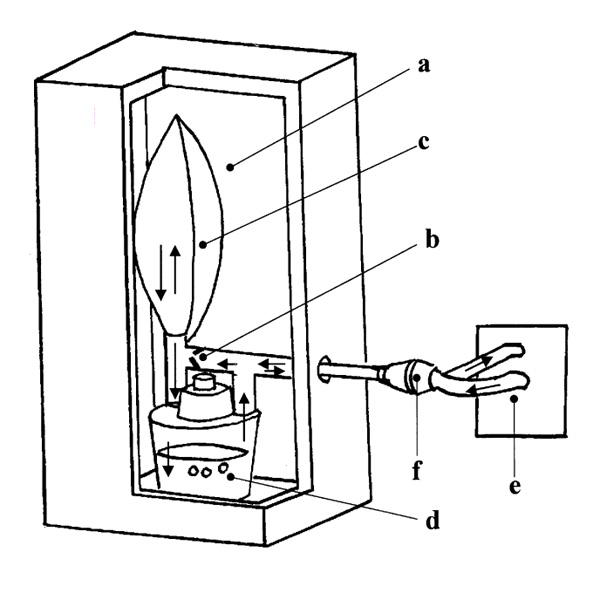
The lung model consists of a box (a) in which the temperature is maintained at 36.0°C, a one-way valve (b), an elastic balloon (c) and a water bath (d). During the inspiratory phase the air passes from the ventilator (e) through the humidifier (f) via the one way-valve to the balloon. During the expiratory phase the air passes from the balloon and bubbles through the water-bath in order to reach 100% humidity at 35.5°C by the time it leaves the lung model. The arrows indicate the direction of the airflow.
As mentioned, the microprocessor of the humidifier uses the patient's minute ventilation for governing the water pump. The user has to enter the minute ventilation into the microprocessor manually. In order to test the tolerance to an unrecognized change in ventilation, we entered the erroneous minute ventilation values of 8 and 12 l/min into the microprocessor, when the actual minute ventilation at both occasions was 10 l with a constant flow pattern.
The calculation of the absolute humidity of the inspired air was based on the following conditions: the air expired from the lung model was fully saturated at 35.5°C (the lung model consists of a water bath with a measured temperature of 36.0°C, see Fig. 2); the inspired gas had a temperature of 37°C (also verified by continuous measurement), meaning that it will carry 44 mgH2O/l without condensation occurring; and a change of the amount of water in the lung model during the test period was due to the difference in water content between the inspired and expired air.
Thus, absolute humidity = (WLchange/Σ VT) + Hout, where WLchange is the change of water content in the lung model, Σ VT is the total ventilation during the 90-min test period and Hout is the absolute humidity of the expired air from the lung model (100% saturated at 35.5°C=41 mg/l). The change in the water content was found by weighing the whole model before and after the experiment. To study the reproducibility, the tests at 3, 5, 6, 8, 10 and 15l minute ventilation were made in duplicate. The water consumption was registered. The absolute humidity in the inspiratory and expiratory ventilator tubings was measured continuously by the Humidity Sensor System (Louis Gibeck AB, Upplands Väsby, Sweden) and electronically averaged.
Tests in ventilator-treated patients
The second part of the experiment was the testing of the Humid-Heat in ventilated patients and comparing it with a conventional active humidifier in a prospective, controlled and randomized manner. Eight consecutive intensive care patients (six males and two females, body weight 66–110 kg), in whom we anticipated a minimum of 48 h of ventilator treatment, were enrolled. The study was performed during 2 separate weeks (six patients the first week and two the second week). The Humid-Heat was used for 24 h (range 14–27 h) and then replaced with a conventional active device (MR730; Fisher & Paykel, Auckland, New Zealand) with a heated wire in the inspiratory limb, or vice versa. The order was randomized. In the test with the MR730, the Y-piece was connected via a flex-tube (dead space 20 ml) to the endotracheal or tracheostomy tube. The patients were ventilated using a Siemens 300 ventilator: four with pressure control, three with pressure support and one with volume control. The range (mean) of peak inspiratory pressure was 15–34 (29) cmH2O and the range (mean) of positive end-expiratory pressure was 5–15 (11) cmH2O. The minute ventilation was 8–14l (mean 10l with the Humid-Heat and 11 l with the MR730; P = 0.37) and the tidal volume was 400–700 ml (mean 560 ml with the Humid-Heat and 630 ml with the MR730; P = 0.40.) The range (mean) of respiratory rate was 11–26 (20) breaths/min. The Humid-Heat was preset to keep the temperature of the inspired gas at 37°C and the MR730 was set at 36°C in the humidifier and 40°C at the Y-piece according to recommendations from the manufacturer (Blyth A, FPCare, personal communication). The room temperature was 21°C.
The temperature of the patient was measured before and after the test of each device. The temperature at the Y-piece (MR730) and in the flex-tube (Humid-Heat) was registered after 30min of use and at the end of the test period. The number of times that the water traps were emptied, changes of machine filters, suctions and quality (thick, normal or thin) of secretions, nebulizations, and the amount of saline instillations and endotracheal tube obstruction were recorded. The amount of fluid consumed was measured by weighing the fluid bags that supplied the humidifiers with water before and after the testing of each device. Likewise, the amount of water in the water-traps was measured by weighing. In order to evaluate increased expiratory resistance due to the device, the airway pressure was measured at the end of a prolonged end-expiratory pause at 1 h of use of the humidifier and at the end of the experiment, and compared with the pressure before the experiment.
Statistics
The data are given as range and mean when not otherwise indicated. Statview (SAS institute Inc, Cary, North Carolina, USA) was used for the statistical analysis. The correlation between absolute humidity and minute ventilation was analyzed by regression. The difference between absolute humidity at the two tests with similar minute volumes was expressed as the coefficient of variation [i.e. as standard deviation/mean (= D/m × √ 2, where D is the absolute value of the difference between the values of absolute humidity and m is the mean)]. The difference between flow patterns in the bench test was analyzed using Mann–Whitney U test. Likewise, the differences between the two test periods with the humidifiers in the patient study were analyzed with Mann–Whitney U test, except for the difference in sputum quality, which was analyzed using the χ2 test. The differences in airway pressures within the two test periods were analyzed using analysis of variance.
Results
Lung model tests
No significant difference in absolute humidity of inspired air between constant and decelerating flow was found (43.2 ± 1.7 and 42.5 ± 0.6 mg/l (mean ± standard deviation), respectively; P =0.19). With both flow patterns the Humid-Heat gave an absolute humidity of 41–44 mgH2O/l, with the lower level at the highest ventilation (Fig. 3). The regression equation was as follows: absolute humidity ( mg/l) = 44.4–0.12 × minute volume (l/min), r2 = 0.49; P =0.003. The temperature of the inspired air leaving the humidifier was 36.9 ± 0.5°C (mean ± standard deviation). The coefficient of variation of absolute humidity for the double tests was 3.5% (0.3–7.4%). The water consumption was 10.1 ± 1.6 mg/l inspired air (mean ± standard deviation) and the absolute humidity in the expiratory ventilator tubing was 7.5 ± 2.2 mg/l (mean ± standard deviation). This corresponds to 42 ± 12% (mean ± standard deviation) relative humidity at the prevailing temperature (21°C). The absolute humidity in the inspiratory ventilator tubing was 0.14 ± 0.15 mg/l (mean ± standard deviation).
Figure 3.
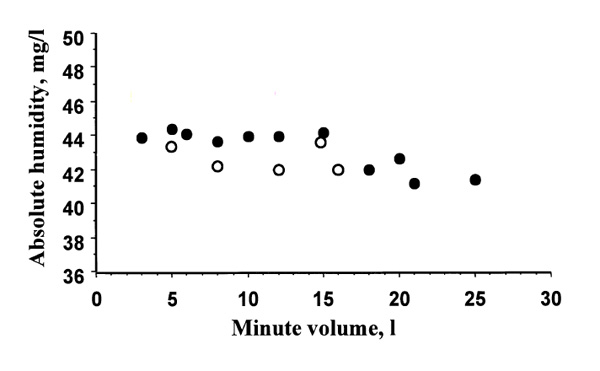
Results from the lung model experiments. The filled and unfilled circles indicate the absolute humidity in the inspired air at different minute volumes during a constant and decelerating flow, respectively.
The absolute humidity at the actual minute ventilations of 10 l/min when the incorrect minute ventilation values of 8 and 12 l/min had been entered were 41.3 and 43.5 mgH2O/l, respectively.
Tests in ventilator-treated patients
For the results of the test in ventilator-treated patients, see Table 1. Both devices maintained the set temperatures, indicating that they were supplying the intended heat and moisture to the inspired air. The MR730 consumed on average 43 μ lH2O/l inspired air, which theoretically would give an absolute humidity of about 43 mg/l. The Humid-Heat consumed in average 9 μ l H2O/l inspired air, which was similar to the water consumption in the bench test, in which the absolute humidity in the inspired air was 41–44 mg/l. With both devices, the patient's body temperature was maintained during the test period. There was no difference in the amount or quality of the secretions or in the frequency of suctions, saline instillations or nebulizations between the test periods with the two devices. There was no endotracheal tube obstruction. With both devices, the airway pressure at the end of a prolonged expiratory pause was the same before, after 1h of use and just before the end of the experiment, indicating that neither device increased airway resistance. When the MR730 was used, however, the water traps needed to be emptied six to 14 (eight) times (total amount of fluid in the traps was 100–300 ml) and the machine filters were changed two to six (four) times due to an excessive amount of condensed water with flow obstruction. No condensation of water was found in the ventilator tubings with the Humid-Heat. The water consumption was 23–65 (30) ml/h with the MR730 and 4–8 (6) ml/h with the Humid-Heat (P < 0.0008).
Table 1.
The patient test
| Humid-Heat | Fisher & Paykel MR730 | P | |
| Duration of the test (h) | 24 ± 0.5 | 22± 4.0 | 0.27 |
| Change in the patient's body temperature (°C) | -0.28 ± 0.36 | +0.01 ± 1.1 | 0.56 |
| Change in the temperature at the Y-piece or the flex-tube (°C) | -0.13 ± 0.64 | 0.0 ± 0.54 | 0.71 |
| Suctions (n) | 10.4 ± 3.9 | 9.2 ± 3.2 | 0.75 |
| Saline instillations (n) | 5.9 ± 3.1 | 4.6 ± 2.9 | 0.43 |
| Total volume of saline instilled (ml) | 30 ± 20 | 24 ± 23 | 0.41 |
| No of nebulizations (salbutamol 2.5 mg plus 200 mg N-acetylcystein | 3.6 ± 1.8 | 3.9 ± 2.0 | 0.75 |
| diluted with saline to a total of 5 ml) | |||
| Quality of secretions at the start of the experiment (thick, normal, thin) (n) | thick 2, normal 2, thin 4 | thick 4, normal 3, thin 1 | 0.26 |
| Quality of secretions at the end of the experiment, patients (n) | thick 0, normal 5, thin 3 | thick 1, normal 5, thin 2 | 0.18 |
| Change in thickness of secretions (i = increase, d = decrease, | d = 3, i = 3, O = 2 | D = 3, i = 1, O = 4 | 0.44 |
| O = no change), patients (n) | |||
| Change in airway pressure at a prolonged expiratory pause | 0 | 0 | 0.99 |
| Water consumed/h (ml) | 5.6 ± 1.2 | 30 ± 15 | 0.0008 |
| Water consumed/l inspired gas (ml) | 0.009 ± 0.003 | 0.043 ± 0.018 | 0.0008 |
| Number of times that the water traps were emptied | 0 | 8.3 ± 3.2 | 0.0008 |
| Total amount of fluid in the water traps (ml) | 0 | 213 ± 84 | 0.0008 |
| Number of changes of machine filters due to excessive water condensation | 0 | 4.7 ± 1.6 | 0.0008 |
The numbers are presented as mean ± standard deviation when applicable.
Discussion
This study shows that a new type of humidifier, the Humid-Heat, produced 41–44 mg/l absolute humidity at 37°C when tested in a lung model and that, compared with a conventional active humidifier in patients, it decreased the amount of fluid consumed and eliminated water condensation in the ventilator tubing.
Recent studies have shown that hygroscopic HMEs provide adequate humidification of the inspired air in most ventilated patients [3,4,6,7,8]. These devices are simple to use and may also reduce the incidence of ventilator-associated pneumonia [9]. In some patients, however, active humidification is still needed. With the conventional active humidifiers there is a substantial condensation of water in the ventilator tubing, which may cause problems with the ventilator function and often become contaminated with microbiological agents. In fact, many studies have shown that after 24 h of use with a conventional active humidifier, the ventilator tubing is contaminated in 60–80% of cases [5,6,10]. Theoretically, under the same conditions as in the present study, if an active humidifier produces an absolute humidity of approximately 44 mg/l at 37°C in the inspired air, as the MR730 did, then at steady state (ie when the inspired and expired absolute humidity is equal) this will cause water condensation in the expiratory ventilator tubing at about 18 ml/h. Indeed, during the test period with the MR730 we could retrieve on average about 10 ml/h condensed water from the water traps. In clinical practice a common way to reduce excessive water condensation in the tubing when using an active humidifier is to reduce the temperature of the inspired air to about 30°C. Although this will reduce the amount of condensed water, it also reduces the absolute humidity. In fact, the performance of the device will be similar to an HME [8].
The Humid-Heat was designed to eliminate the problem of water condensation. However, it has two potential drawbacks. First, it cannot be used in patients with copious secretions and, second, the temperature of the inspired air is fixed at 37°C at the proximal end (to the Y-piece) of the flex-tube. We have not measured the air temperature closer to the patient, but the temperature of the inspired air will probably be somewhat lower in the trachea. The optimal temperature of inspired air in mechanically ventilated, endotracheally intubated patients is not known, however. The temperature in the trachea during inspiration is about 31°C and about 33°C at the carina in healthy individuals, spontaneously and quietly breathing room air [11]. Although we could not find any signs of overhydration during the 24-h test period in the patients studied, we cannot exclude that the set temperature of 37°C may be too high in some patients. This device is designed for use in critically ill patients, however, in whom the humidification by an HME, which gives 30–32 mg/l humidity at a temperature of 30–32°C, is not sufficient [3,4]. Indeed, some experts have recommended that the humidity of the inspired air should be 44 mg/l, as achieved by the Humid-Heat, during artificial ventilation [12,13].
The tests in the ventilator-treated patients showed that the device was well tolerated and that condensation in the tubing was eliminated. The water consumption was 9 μ l/l inspired air, and if this amount of water is expired it will give a relative humidity of about 50% at 21°C in the expiratory ventilator tubing. This assumption is also supported by the results from the bench test, in which the relative humidity was 42± 12% (mean± standard deviation) in the expiratory tubing, which is below the threshold of condensation. There was no need to empty water traps or to change machine filters. The test period was too short to evaluate whether the new device had any other advantages or disadvantages compared with conventional humidifiers. No potential problem such as increased resistance to airflow through the humidifier was seen, however. This indicates that the HME in the device can deal with the extra water load without becoming obstructed. Our results agree well with a very recently published study [14] that also examined the performance of the Humid-Heat in ventilator-treated patients.
In conclusion, the Humid-Heat provided 41–44 mg/l absolute humidity at 37°C and did not cause any water condensation in the ventilator tubing. The results of this 24 h study are promising, but further tests are needed to evaluate patient tolerance during longer periods of use.
References
- Chalon J, Loew DA, Malebranche J. Effect of dry anesthetic gases on tracheobronchial ciliated epithelium. Anesthesiology. 1972;37:338–343. doi: 10.1097/00000542-197209000-00010. [DOI] [PubMed] [Google Scholar]
- Marfatia S, Donahoe PK, Hendron WH. Effect of dry and humidified gases on the respiratory epithelium in rabbits. J Pediatr Surg. 1975;10:583–592. doi: 10.1016/0022-3468(75)90360-7. [DOI] [PubMed] [Google Scholar]
- Branson RD, Davis K, Jr, Campbell RS, et al. Humidification in the intensive care unit. Prospective study of a new protocol utilizing heated humidification and a hygroscopic condensor device. Chest. 1993;104:1800–1805. doi: 10.1378/chest.104.6.1800. [DOI] [PubMed] [Google Scholar]
- Kollef MH, Shapiro SD, Boyd V, et al. A randomized clinical trial comparing an extended-use hygroscopic condensor humidifier with heated-water humidification in mechanically ventilated patients. . Chest. 1998;113:759–767. doi: 10.1378/chest.113.3.759. [DOI] [PubMed] [Google Scholar]
- Craven DE, Goularte TA, Make BJ. Contaminated condensate in mechanical ventilator circuits. Am Rev Respir Dis. 1984;129:625–628. [PubMed] [Google Scholar]
- Boots RJ, Howe S, George N, Harris FM, Fagiolli J. Clinical utility of hygroscopic heat and moisture exchangers in intensive care patients. Crit Care. 1997;25:1707–1712. doi: 10.1097/00003246-199710000-00021. [DOI] [PubMed] [Google Scholar]
- Thomachot L, Vialet R, Arnaud S, et al. Do the components of heat and moisture exchanger filters affect their humidifying efficacy and the incidence of nosocomial pneumonia. . Crit Care Med . 1999;27:923–928. doi: 10.1097/00003246-199905000-00026. [DOI] [PubMed] [Google Scholar]
- Thomachot L, Viviand X, Arnaud S, et al. Preservation of humidity and heat of respiratory gases in spontaneously breathing, tracheotomized patients. Acta Anaesthesiol Scand. 1998;42:841–844. doi: 10.1111/j.1399-6576.1998.tb05331.x. [DOI] [PubMed] [Google Scholar]
- Cook D, De Jonghe B, Brochard L, Brun-Buisson C. Influence of airway management on ventilator-associated pneumonia : evidence from randomized trials. JAMA. 1998;279:781–787. doi: 10.1001/jama.279.10.781. [DOI] [PubMed] [Google Scholar]
- Dreyfuss D, Djedaini , Gros I, et al. Mechanical ventilation with heated humidifiers or heat and moisture exchangers: effects on patient colonization and incidence of nosocomial pneumonia. Am J Respir Crit Care Med. 1995;151:986–992. doi: 10.1164/ajrccm/151.4.986. [DOI] [PubMed] [Google Scholar]
- McFadden ER, Pichurko BM, Bowman HF, et al. Thermal mapping of the airways in humans. J Appl Physiol. 1985;58:564–570. doi: 10.1152/jappl.1985.58.2.564. [DOI] [PubMed] [Google Scholar]
- Boys JE, Howells TH. Humidification in anaesthesia: a review of the present situation. Br J Anaesth. 1972;44:879–886. doi: 10.1093/bja/44.8.879. [DOI] [PubMed] [Google Scholar]
- Stone DR, Downs JB, Paul WL, Perkins HM. Adult body temperature and heated humidification of anesthetic gases during general anesthesia. . Anesth Analg. 1981;60:736–741. [PubMed] [Google Scholar]
- Branson RD, Campbell RS, Johannigman JA, et al. Comparison of conventional heated humidification with a new hygroscopic heat and moisture exchanger in mechanically ventilated patients. Respir Care. 1999;44:912–917. [Google Scholar]


