Abstract
There is unequivocal evidence of an inverse association between plasma high-density lipoprotein (HDL) cholesterol concentrations and the risk of cardiovascular disease, a finding that has led to the hypothesis that HDL protects from atherosclerosis. This review details the experimental evidence for this “HDL hypothesis”. In vitro studies suggest that HDL has a wide range of anti-atherogenic properties but validation of these functions in humans is absent to date. A significant number of animal studies and clinical trials support an atheroprotective role for HDL; however, most of these findings were obtained in the context of marked changes in other plasma lipids. Finally, genetic studies in humans have not provided convincing evidence that HDL genes modulate cardiovascular risk. Thus, despite a wealth of information on this intriguing lipoprotein, future research remains essential to prove the HDL hypothesis correct.
Keywords: cardiovascular disease, risk factors, biology, animal studies, genetics, therapy
In 1951, Barr et al. (1) reported that plasma levels of high-density lipoprotein cholesterol (HDL-C) were reduced in patients with coronary artery disease. In 1977, Gordon et al. (2) subsequently showed that low HDL-C is a risk factor for coronary heart disease in the Framingham study. These important findings have given rise to a large number of diverse HDL studies over the last few decades. The numerous different and apparently unrelated beneficial effects that have since been ascribed to HDL appeal to the imagination. Because of a general consensus that HDL protects against atherosclerosis, what we shall term the HDL hypothesis, strategies have been developed to raise plasma HDL levels or to improve HDL function. However, it is increasingly questioned whether such interventions will indeed reduce the risk of atherosclerosis. This review summarizes the reported evidence that supports the HDL hypothesis.
EPIDEMIOLOGY
A low plasma HDL-C concentration is among the strongest, statistically independent risk factors for cardiovascular disease (CVD) (2). In a widely cited meta-analysis of four large studies (total number of individuals studied: 15,252), a 1 mg/dl increase of HDL-C levels was reported to be associated with a 2–3% decreased CVD risk (3). This result provides an epidemiological argument in favor of therapeutically raising HDL-C levels. One may draw parallels with the detrimental consequences of elevated low-density lipoprotein cholesterol (LDL-C) levels and blood pressure, which have been successfully controlled through therapy, resulting in significant reductions of cardiovascular mortality and morbidity (4, 5). It should be noted, however, that the associations between elevated LDL-C and blood pressure and increased CVD risk reflect causal relationships, whereas such a relation between low HDL-C levels and increased CVD is not undisputed (6, 7). This is related to the fact that HDL-C levels are influenced by many different variables that also affect CVD risk: 1) Men have on average lower HDL-C levels than women (8). 2) Smokers have 14% lower HDL-C levels than nonsmokers, and this relationship appears to be dose-dependent, (9) whereas individuals who quit smoking show a subsequent increase in HDL-C levels (10). Even in individuals who acutely smoke two cigarettes, HDL-C levels drop 6 mg/dl (11). 3) A recent meta-analysis of 25 studies (total number of individuals studied: 2,027) shows that programs of regular aerobic exercise increased HDL-C levels by 2.5 mg/dl on average (12). 4) Obesity, especially abdominal obesity, is also associated with lower HDL-C levels (13), whereas weight loss results in an elevation of HDL-C levels (14). 5) Patients with type 2 diabetes mellitus display several lipid abnormalities of which a low HDL-C level is a prominent feature (15). 6) Metabolic syndrome, a cluster of pathologies comprising abdominal obesity, hypertension, impaired glucose tolerance, high triglycerides, and low HDL-C levels, is regarded by investigators as a single disease entity resulting from insulin resistance (16). 7) In parallel, (postprandial) hypertriglyceridemia results in low HDL-C levels, associated with an increased cholesteryl ester transfer protein (CETP) driven exchange of cholesteryl esters and triglycerides between pro-atherogenic apolipoprotein (apo)B-containing lipoproteins (VLDL and LDL) and HDL (17). In fact, over 50% of the patients with low HDL-C levels also present with increased fasting triglycerides. (18) With this in mind, HDL-C levels may be seen as a stable reflection of disturbances in triglyceride metabolism, whereas plasma triglyceride levels themselves are subject to large inter-individual and intra-individual variability. 8) Systemic inflammation (as observed in rheumatoid arthritis and systemic lupus erythematosus), a recognized risk factor for CVD (19), is associated with a secondary dyslipidemia characterized by low HDL-C levels (20). 9) Finally, a low socioeconomic status is an independent predictor of low HDL-C (21). Interestingly, even in baboons, socially subordinate males show 31% lower HDL-C levels than dominant males, possibly related to chronic social stress (22).
Thus, many different factors affect both CVD risk as well as HDL-C levels. A recent very large meta-analysis comprising 302,430 individuals has once again made clear that HDL-C is a strong predictor of cardiovascular events, even after statistical adjustment for these variables (23). Such adjustments, however, do not guarantee the absence of residual confounding (24), and one may ask what the meaning of statistical outcomes is when the adjustments concern parameters that are intrinsically related to HDL metabolism. In addition to plain HDL-C measurements, many investigators have focused on HDL-related parameters, such as levels of apoA-I (HDL's most important structural protein), or HDL subclasses (as assessed by, e.g., nuclear magnetic resonance or 1- and 2-dimensional gel electrophoresis), and have shown that some of these parameters are superior to HDL-C in cardiovascular-risk assessment. (25) Although these studies are of interest, these epidemiological relationships are subject to the same confounding variables as those concerning HDL-C itself and are therefore not fit to prove that HDL is responsible for atheroprotection.
In conclusion, the epidemiological association between HDL and CVD is strong and is largely responsible for the formulation of the HDL hypothesis, but in itself does not prove a causal relationship.
HDL FUNCTION
In line with the HDL hypothesis, HDL has been reported to exhibit many anti-atherogenic properties [for an extensive review, see (26)] that are addressed in this section.
Reverse cholesterol transport
In 1982, Fielding and Fielding (27) demonstrated that HDL can act as an acceptor of cellular cholesterol, which is proposed to constitute the first step in a hypothetical pathway that is known as reverse cholesterol transport (RCT). In its broadest sense, RCT is defined as the uptake of cholesterol from peripheral cells by lipid-poor apoA-I and HDL that is mediated by lipid transporter molecules such as ATP-binding cassette transporter A1 and G1 (ABCA1 and ABCG1) and scavenger receptor B-I (SR-BI), and the subsequent delivery to the liver for ultimate excretion into the feces as neutral sterols or bile acids. HDL can deliver cholesterol to the liver through hepatic SR-BI, or, alternatively, CETP shuttles cholesterol from HDL to (V)LDL, which can be taken up via the LDL receptor (LDLr) pathway. The overall RCT hypothesis, especially with respect to the relationship between plasma HDL cholesterol and fecal cholesterol excretion, has been challenged by findings in both mice and humans.
For mice, it has been reported that (total body) ABCA1 deficiency, causing near complete HDL deficiency, does not affect hepatobiliary flux of cholesterol (28). Similarly, modulation of apoA-I, lecithin-cholesterol acyl transferase (LCAT; an enzyme critically involved in HDL maturation), and SR-BI, resulting in large changes in plasma HDL-C concentrations, had no effect on sterol excretion (29). In addition, the infusion of apoA-I-phospholipid complexes in apoA-I knockout mice did not increase fecal sterol excretion (29). Thus, marked manipulation of HDL metabolism in mice apparently does not result in changes in net fecal cholesterol excretion. Another method to study whole body RCT in mice has been developed by deGoma et al. (30). In short, macrophages loaded with radiolabeled cholesterol are injected into the peritoneal cavity of mice, after which the distribution of this cholesterol in plasma, liver, and feces is quantified. These studies have provided insight into which factors control the RCT pathway in mice but have not provided data on net fecal cholesterol output.
In humans, the data on HDL dependent fecal cholesterol output are equivocal. Both a negative as well as the absence of a relationship between plasma HDL-C concentrations and fecal sterol excretion have been reported (31–33) and a recent study in seven individuals with genetically determined low HDL-C indicated reduced fecal cholesterol output (34). Intervention studies that increase plasma HDL-C levels also provided mixed results: the infusion of pro-apoA-I or reconstituted HDL (rHDL; apoA-I purified from human blood, reconstituted with phospholipids) was reported to result in an increase of sterol excretion (35, 36), but CETP inhibition (which blocks the exchange of cholesterol from HDL to LDL, resulting in a marked HDL-C increase as well as an LDL-C decrease) had no effect (37). Thus, human studies have only provided little evidence that HDL-C levels correlate with fecal cholesterol output. In fact, according to cholesterol flux modeling studies by Schwartz et al. (38), the role of HDL in total body cholesterol homeostasis is suggested to be minimal. Studying cholesterol exchange processes from another angle, Turner and Hellerstein (39) have recently developed a technique that estimates tissue cholesterol efflux by means of the steady-state isotope dilution principle. Although its value remains to be determined, a potential strength of this technique is that it may be applied in both case-control settings as well as to assess the impact of novel drugs.
HDL may have its most relevant role regarding vascular protection in the initial steps of the RCT pathway. Macrophages in the vessel wall take up (oxidized) LDL, turn into foam cells, and add to a pro-inflammatory environment that promotes atherosclerotic plaque formation and ultimately plaque instability. In this context, apoA-I and HDL-mediated cholesterol efflux from lipid-laden macrophages is a conceptually attractive atheroprotective mechanism. Accordingly, the cholesterol acceptor capacity of (apoB depleted) serum, or isolated HDL has been studied as a biomarker for studies that test HDL-modulating therapies (30). Some of these studies showed promising data. For example, HDL isolated from patients after treatment with the CETP inhibitor torcetrapib was shown to be able to elicit more cholesterol efflux from cultured cholesterol-loaded cells than HDL taken from patients at baseline (40). However, the only study in humans to report on the predictive value of serum cholesterol acceptor capacity for CVD showed that those patients with a recurrent cardiovascular event were, paradoxically, characterized by a high serum cholesterol acceptor capacity (41). The authors speculated that a high serum acceptor capacity reflects an abundance of small lipid-poor HDL particles, as a consequence of an inherent inability of these patients to saturate their serum HDL with cholesterol (41). Although this may or may not be the correct interpretation, this finding clearly illustrates the difficulties that arise in the translation of in vitro findings to the in vivo situation.
Another method to study cholesterol efflux is to assess the efflux capacity of donor cells. It is known that cellular cholesterol homeostasis is controlled by ABCA1 (42), ABCG1 (43), and SR-BI (44–47), although a large percentage of cholesterol efflux remains unexplained (48).
To date, only two studies addressed the relationship between cellular cholesterol donor capacity and atherosclerosis progression in humans. The first study showed a significant association between cholesterol efflux from human skin fibroblasts and increased carotid intima media thickness (cIMT; a surrogate endpoint for cardiovascular endpoints) in nine individuals (49). The second study, of 142 subjects undergoing coronary angiography, showed that cholesterol efflux from cultured primary macrophages to HDL and apoA-I was not different between subjects with and without significant stenosis. After adjustment for age and sex (the group with stenosis was on average 6 years older and consisted of significantly more men), cholesterol efflux to HDL became significantly lower in the stenosis group (50).
Altogether, there is no evidence for a role of HDL in the net removal of cholesterol from the body (or vascular wall) and subsequent excretion into feces in mice, whereas evidence in humans is very scarce. To date, there are no assays to measure cholesterol efflux that have proven value in predicting cardiovascular events in humans. This reflects the inherent difficulty of finding a measure for the complex dynamics of cellular cholesterol exchange in atherosclerotic lesions.
Other potentially atheroprotective properties
In in vitro experiments, HDL has been shown to inhibit the expression of endothelial adhesion molecules (51) and to inhibit LDL-induced monocyte transmigration (52). By blocking lipopolysaccharide activity and decreasing CD11b/CD18 upregulation, rHDL has also been shown to decrease lipopolysaccharide-induced adhesion of leukocytes to human endothelial cells (53). In addition, the anti-oxidative activity of HDL is typically characterized by its ability to inhibit LDL oxidation (54) but it has also been shown to inhibit the formation of reactive oxygen species (55, 56). In rabbits, the infusion of rHDL or low dose apoA-I can, moreover, prevent or even reverse an inflammatory response when provoked by placement of a nonocclusive silastic collar around a carotid artery (57, 58). Several years ago, two assays assessing the anti-oxidative and anti-inflammatory capacity of HDL were reported to distinguish between CVD patients and healthy controls with similar HDL-C levels (59, 60). These results held promise with regard to the need of valuable biomarkers to study HDL modulating therapies. Unfortunately, these findings have as of yet not been reproduced.
Apoptotic cell death following injury of vascular endothelium is assumed to play an important role in the pathogenesis of atherosclerosis (61). HDL has been shown to protect endothelial cells from apoptosis induced by mildly oxidized LDL (62). Similarly, preincubation of human umbilical venous endothelial cells with HDL can prevent apoptosis induced by tumor necrosis factor-α (63). HDL also potently protects endothelial cells against growth factor deprivation-induced apoptosis via suppression of the mitochondrial apoptotic pathway (64). Both apoA-I (62) and sphingosine-1-phosphate (65, 66), a lipid component of HDL, have been proposed to contribute significantly to HDL-mediated cytoprotection.
HDL can affect platelet function through the promotion of nitric oxide production (67) and coagulation by the inhibition of several coagulation factors, such as tissue factor, factor Va, VIIIa, and Xa (68). Purified HDL, but not LDL, significantly enhanced inactivation of factor Va by activated protein C (APC) and protein S (69). HDL has also been shown to scavenge anionic phospholipids, thereby abolishing their pro-coagulant properties (70). Whether these anti-thrombotic effects apply to humans is unknown. There are reports of an epidemiological relationship between HDL-C and thrombosis risk (71), but this relationship is subject to confounding by important health parameters [e.g., obesity (72) or the metabolic syndrome (73)] along the lines discussed above.
One study, in 2001, has shown that HDL can induce vasodilation by stimulating the release of nitric oxide by endothelial cells in mice (74). In line with this, infusion of rHDL into hypercholesterolemic type 2 diabetic patients and subjects with low HDL-C was reported to partially restore endothelium-dependent vasodilation (75–77). These studies point toward a direct role for HDL in atheroprotection taken that endothelial dysfunction precedes atherosclerosis. To date, however, there are no assays that can be used to assess this type of HDL functionality ex vivo in a clinical setting.
In conclusion, there is considerable evidence for a direct protective role of HDL in inflammatory, oxidative, apoptotic, and thrombotic processes but these studies are primarily performed in in vitro settings. With respect to protection from endothelial dysfunction, some evidence suggests that in vitro findings may apply to in vivo situations as well but studies are small. In each case, a direct link between ex vivo measurements (biomarkers) and cardiovascular risk is yet to be established. Because such evidence could strengthen the concept that HDL is an actor rather than a bystander in atherogenesis, an important challenge for the coming years will be the translation of HDL function assays from bench to bedside. These assays are particularly needed in view of the ongoing testing of novel HDL drugs in clinical trials where early indications of success or failure are absolutely vital.
ANIMAL MODELS
Many animal models have been developed that mimic human atherosclerosis (78). This section focuses on evidence that HDL provides direct atheroprotection in animal models in which key HDL modulators were studied through overexpression, knockout, and cross-breeding experiments.
Strengths and limitations of animal studies
The most studied animal, the mouse, almost exclusively uses HDL to transport cholesterol in the circulation, whereas in humans most cholesterol is carried by LDL. This major difference is closely related to the natural absence and presence of CETP in mice and humans, respectively. Because mice are not normally prone to atherosclerosis, this urges investigators to use genetic and dietary manipulation to induce this phenotype. Another point that deserves attention, especially when interpreting earlier mouse studies (1990–2000), is the use of a mixed genetic background, which in view of strong differences in atherosclerosis susceptibility among congenic lines makes correct interpretation difficult (79). The wide-spread use of cholate-containing atherogenic diets, especially in that period, causing liver toxicity and gall stone formation, further complicates matters (80). Furthermore, most data have been generated in supraphysiological settings using high copy-number transgenics and adenovirus to mediate strong hepatic expression. Taken together, it is not surprising that many mouse studies have provided equivocal data and interpretations with regard to effects of HDL- related factors on atherosclerosis. In more recent years, more dedicated mouse models have been developed that closely mimic human atherosclerosis, e.g., the CETPtgxLDLrKO (81) and CETPtgxapoE3Leiden (82) mouse. In addition, the use of (conditional) tissue-specific knockout models rather than whole body knockout models, the use of endogenous promoters, and knock-in models have provided better tools to study lipid biology and the natural course of atherogenesis. Finally, bone marrow transplantation represents another promising tool to study vascular macrophages.
ApoA-I
ApoA-I is the most important structural protein of HDL. Consequently, apoA-I knockout mice have abnormal (apoE-enriched) HDL and 75% lower HDL-C levels. However, on an atherogenic diet these mice do not exhibit increased atherosclerosis (83). Knocking out apoA-I in human (h)ApoB transgenic mice did result in increased atherosclerosis, but only in female mice after feeding a Western-type diet for 6 months and in the context of profound hypertriglyceridemia (84). Similarly, knocking out apoA-I in LDLr−/− mice increased atherosclerosis, but these mice also displayed a robust increase of VLDL cholesterol and abnormal and potentially pro-atherogenic apoA-I negative HDL, with a density overlapping that of LDL (85). In another study, a lack of apoA-I was studied in LDLr−/−/apobec−/− (LA) mice (86), which express full-length apoB100 and have 3-fold higher plasma levels of apoB100 than LDLr−/− mice (87). In this case, there was a gene-dose-dependent increase in atherosclerosis with each missing apoA-I allele in both male and female mice. Interestingly, the lipid profiles of these mice barely differed with respect to LDL and VLDL cholesterol, suggesting that the apoA-I HDL fraction was indeed responsible for the observed differences in atherosclerosis formation. Together, these data suggest more atherosclerosis as a result of a lack of apoA-I. Also, the data may imply a direct protective role for apoA-I as some observations were made in the absence of concurrent deleterious changes in other (apo)lipoprotein fractions.
Extending these findings, overexpression of hApoA-I in mice has provided very uniform results. Expression of hApoA-I inhibited preatherosclerotic fatty streak lesion formation in C57Bl/6 mice on an atherogenic diet and increased HDL-C levels in the absence of significant changes in nonHDL-C (88). In addition, the expression of hApoA-I in apoE deficient mice and in hApo(a)-transgenic mice yielded similar results (89–91). A reduction of atherosclerosis has been reproduced in various apoA-I gene transfer protocols in different animal models (92–95). Finally, weekly infusions of purified rabbit apoA-I (96) and transgenic overexpression of hApoA-I (97) in cholesterol-fed rabbits also reduced progression of atherosclerosis.
Taken together, the currently published animal data provide good evidence in favor of a direct atheroprotective effect of apoA-I.
ABCA1 and ABCG1
ATP-binding cassette (ABC) transporter A1 is instrumental for the de novo synthesis of HDL in the liver and small intestine by mediating the efflux of phospholipids and cholesterol to apoA-I that is produced in these organs (98). ABCG1 constitutes another important player in HDL metabolism with a special role in the delivery of cholesterol to larger HDL.
Total body knockout studies have provided the following data on these transporters: ABCA1−/− mice have virtually no HDL but show no increased atherosclerosis, not even when fed an atherogenic diet on an LDLr−/− or on an apoE−/− background (99). ABCG1−/− mice specifically accumulate cholesterol esters in lung macrophages, but show unaltered plasma lipid levels and atherosclerosis development on a Western-type diet (100). Interestingly, knocking out both genes in the same mouse again induced marked HDL-C reductions but did not increase lipid accumulation in the vascular wall (after one year) (101). Thus, a complete loss of ABCA1, ABCG1, or both does not result in increased atherosclerosis in mice.
Five studies have addressed whether increasing ABCA1 or ABCG1 function affects atherosclerosis. Transgenic ABCA1 overexpression in the liver of LDLr−/− mice was shown to result in high apoB levels and a 10-fold accelerated atherosclerosis development (102) whereas it was associated with minimal changes in the lipid profile and a 2- to 3-fold increase of atherosclerosis in apoE−/− mice (103). In contrast, overexpression of hABCA1 under control of its endogenous promoter was shown to protect against atherosclerosis in apoE−/− mice (104). Two studies on ABCG1 overexpression showed increased or unchanged atherosclerosis in LDLr−/− mice (105) and apoE−/− mice, respectively (106). Thus, only one out of these five studies showed a beneficial effect on atherosclerosis of the overexpression of either ABCA1 or ABCG1.
Bone marrow transplantation studies have offered a different view on the role of both transporters in the vascular wall. In the absence of effects on plasma lipids, repopulating apoE−/− mice with ABCA1−/− macrophages resulted in accelerated atherosclerosis (99). In the context of unexplained hypertriglyceridemia, an ABCA1−/− bone marrow transplantation in LDLr−/− mice also resulted in larger and more advanced atherosclerotic lesions (107). In line with an atheroprotective role of ABCA1, transplantation of macrophages of ABCA1tg mice into LDLr−/− mice resulted in decreased atherosclerotic lesion progression, again without effects on lipid profiles (108). On the other hand, data on ABCG1−/− bone marrow transplantation studies provide a less clear picture; two studies showed reduced and one study increased atherosclerosis (109).
In conclusion, total body knockout and transgenic overexpression experiments have indicated that ABCA1 and ABCG1 do not have the anticipated effect on atherosclerosis (with the exception of one out of seven studies). With bone marrow transplantation experiments, however, ABCA1 was clearly shown to provide atheroprotection, albeit in the absence of effects on plasma lipids, whereas similar experiments with a focus on ABCG1 have given contrasting results. Despite a clear indication that upregulation of ABCA1 may be beneficial, none of these studies support a direct protective effect of plasma HDL against atherosclerosis.
LCAT
Lecithin-cholesteryl acyltransferase (LCAT) is an enzyme that plays a key role in regulating HDL-C levels through the esterification of free cholesterol on HDL (110). In contrast to what one may expect, a marked reduction of HDL-C as a result of LCAT deficiency causes reduced atherosclerosis in C57/Bl6, LDLr−/−, apoE−/−, and CETP transgenic mice (111). These results, however, sharply contrast with those reported by Furbee et al. (112) who showed that LCAT deficiency led to increased atherosclerosis in apoE−/− and LDLr−/− mice. The latter authors hypothesized that differences in diet and plasma apoB lipoprotein levels might explain this discrepancy (112). A further study by Mertens et al. (113) supported a beneficial role for LCAT by showing that LCAT gene transfer reduces atherosclerosis by reducing oxidative stress in LDLr−/−;ob/ob mice, but these effects were seen in the absence of changes in HDL-C levels.
In line with this series of diverse results when studying loss of LCAT, transgenic studies have not provided an answer as to whether LCAT is pro- or anti-atherogenic, either. A 100-fold overexpression of human LCAT in C57Bl/6N mice resulting in a 2.5-fold rise of HDL-C and a 3.5-fold rise of apoA-I levels in the absence of a change in apoB levels was associated with a dose-dependent increase of diet-induced atherosclerosis (114). Interestingly, overexpressing hCETP in these mice normalized HDL-C levels, which reduced the atherogenic phenotype (115). Finally, other investigators showed that moderate overexpression of human LCAT had no effect on atherogenesis (116–118).
In addition to mouse studies, there are a number of interesting studies on LCAT in rabbits. A 15-fold LCAT overexpression in transgenic rabbits (with endogenous CETP) has been shown to protect against diet-induced atherosclerosis (119) in the context of both marked increases in apoA-I and decreases in apoB containing lipoproteins, as further underlined in another study by these investigators (120). However, in a later study, overexpression of LCAT on an LDLr−/− background did not affect aortic lipid concentrations nor the extent of aortic atherosclerosis in rabbits (121).
Taken together, LCAT studies in mice and rabbits have not provided clear answers when it comes to the role of this enzyme in atherogenesis, which in rabbits may be due to effects on apoB lipoproteins. These studies illustrate the impossibility to predict a shift in atherosclerosis vulnerability on the basis of changes in plasma HDL-C concentration.
CETP
CETP mediates the transfer of cholesteryl esters and triglycerides between apoA-I and apoB lipoproteins. Wild-type mice are naturally CETP deficient, carry most of their cholesterol in HDL, and are not prone to atherosclerosis. The introduction of human CETP in mice has greatly improved our insight into lipoprotein metabolism. In cholesterol-fed C57BL/6 mice, it led to a marked shift of cholesterol from apoA-I to apoB containing lipoproteins, resulting in reduced HDL-C and increased LDL-C levels. These changes were associated with increased atherosclerosis (122). In line with this, the expression of hCETP in apoE−/− or apoE*3-Leiden mice decreased HDL-C levels, elevated VLDL, LDL, and intermediate-density lipoprotein cholesterol, and also increased atherosclerosis (82, 123). Interestingly, inhibition of CETP with torcetrapib in the latter mice did not offer improvement when used on top of atorvastatin (124), mimicking the torcetrapib studies in humans (addressed below). In Dahl salt-sensitive hypertensive rats (also naturally CETP-deficient), the introduction of hCETP led to a dose-dependent increase of atherosclerosis (125). However, these animals also displayed very strong dose-dependent increases in plasma cholesterol (up to 6-fold) and triglycerides (up to 35-fold) (125). In contrast, in hApoCIII transgenic mice (severely hypertriglyceridemic with an increased tendency for atherosclerosis), CETP expression led to lower plasma HDL-C concentrations, lower total cholesterol levels, and decreased atherosclerosis (126). Similarly, CETP expression has been shown to rescue the atherogenic phenotypes of LCATtg mice (115) and SR-BI−/− mice (127), in conjunction with a reduction of the elevated HDL-C levels.
Rabbits naturally express CETP at high levels. When fed cholesterol, CETP inhibition using various methods generally resulted in a lower atherosclerosis burden (128–132). However, in most of these studies, the drop in nonHDL-C was stronger than the increase in HDL-C. Of note, one study failed to show an effect of CETP inhibition on atherosclerosis in the context of a nonsignificant decrease of nonHDL-C levels (128). On the other hand, a more recent study demonstrated a linear association between HDL-C increase and atherosclerosis reduction after using torcetrapib in rabbits (132).
In conclusion, studies in rabbits show that CETP inhibition can offer atheroprotection, whereas many mouse studies indicate that CETP may be pro- or anti-atherogenic depending on the metabolic context. In line with the role of CETP in lipoprotein metabolism, any modulation with an impact on CETP has marked effects on all lipoprotein parameters. As for LCAT, the CETP mouse studies show that it is not possible to predict how changes in plasma HDL-C concentrations affect atherosclerosis.
SR-BI
SR-BI is a hepatic HDL receptor (133) and plays a role in cellular cholesterol homeostasis. Paradoxically, SR-BI−/− mice have 2.5-fold increased plasma HDL-C (134) but show accelerated atherosclerosis (135). On an apoE−/− background, these mice even develop spontaneous myocardial infarctions because of coronary atherosclerosis on a chow diet (136). As mentioned above, the introduction of human CETP in SR-BI−/− mice normalized HDL-C levels and attenuated atherosclerosis (127). The anti-atherogenic role of SR-BI was furthermore underlined by Kozarsky et al. (137) who showed that gene transfer and hepatic ovexpression of SR-BI can protect from atherosclerosis. SR-BI is also expressed in macrophages, where it mediates cellular cholesterol exchange (44–47). In bone-marrow transplantation studies, SR-BI has been shown to modulate atherosclerosis development without effects on circulating lipids (138, 139).
These SR-BI studies reiterate that modulation of HDL-C levels may have a paradoxical impact on atherosclerosis.
HL
Hepatic lipase (HL) hydrolyzes both triglycerides and phospholipids and exerts this catalytic function on all classes of lipoproteins (140, 141). Overexpression of human HL in mice resulted in decreased total and HDL cholesterol levels and decreased aortic cholesterol content (142). This effect on lipids and atherosclerosis was also seen in a murine HL/LDLR double −/− context (143, 144). In HL/apoE double −/− mice, the introduction of liver-specific human HL also lowered total and HDL cholesterol. However, in this study an increase in plaque size was observed (145).
HL−/− mice display a mildy altered lipid phenotype, including a 21% increase in HDL-C and a 35% increase in total cholesterol, but showed no change in atherosclerosis. Female HL/apoE double −/− mice presented with reduced aortic atherosclerosis in the context of increases in all lipoproteins including HDL (146). In contrast, in HL/LDLR double −/− mice more atherosclerosis was observed (147).
Thus, mouse studies into the role of HL in atherosclerosis have provided equivocal data, illustrating the impact of the type of mouse model applied. Here too, levels of HDL-C are a poor predictor of the atherogenicity of a particular model.
EL
Endothelial lipase (EL) exhibits a high phospholipase activity and low triglyceride lipase activity (143). It primarily hydrolyzes HDL lipids. Mouse studies into the effect of EL overexpression on atherosclerosis have not yet been reported. EL/apoE double −/− mice had reduced atherosclerotic aortic lesion area in one study (148) but no change in plaque area compared with apoE −/− mice in another study (149). Both studies reported an increase in HDL-C and phospholipids and no change in triglyceride levels.
More data are needed to evaluate the link between EL, HDL, and atherosclerosis.
LXR
Liver X receptors (LXR) α and β are nuclear receptors that control cellular cholesterol homeostasis through transcriptional regulation of target genes such as ABCA1, APOE, and ABCG1 (150). The importance of these receptors was shown by knocking out LXRα and β, which caused a 26% reduction of HDL-C, a 83% increase of LDL-C, and a 27-fold accumulation of cholesterol in arterial wall macrophages in mice on a normal chow diet (although aortic lesions did not progress to advanced atheroma) (151). It has been hypothesized that upregulation of LXR target genes can provide atheroprotection. Indeed, systemic administration of synthetic LXR agonists has been shown to reduce plaque formation in mice (152). Moreover, bone marrow transplantation studies have shown that this atheroprotection can be attributed to macrophage LXRs (153). In addition, others have shown that LDLr−/− mice transplanted with LXRαβ−/− bone marrow demonstrate a 3-fold increase in atherosclerosis in the absence of changes in plasma lipids. (154) Unfortunately, systemic administration of first generation LXR agonists results in elevated plasma triglycerides, fatty liver (155, 156), and disturbance of growth hormone and thyroid axes (157).
These studies show that cholesterol mobilization from the vascular macrophage constitutes an important step in atheroprotection. However, these studies do not support a direct role for HDL as an atheroprotective entity.
Reviewing the data of major animal studies that have focused on primary modulators of HDL metabolism, it is clear that the vast majority of animal studies have thus far not provided evidence that HDL protects from atherosclerosis. Although many studies may have indicated that modulation of HDL metabolism is associated with atheroprotection, a careful analysis shows that this is often seen in the context of a simultaneous modulation of apoB-containing lipoproteins, which obscures the reported effects of HDL on atherosclerosis. The most positive and convincing data have been generated by studies of overexpression of human apoA-I in mice and apoA-I infusion in rabbits. Paradoxically, high HDL-C levels have also been associated with accelerated atherosclerosis in SR-BI−/− or LCAT transgenic animals. The capacity to reverse atherosclerosis in these mice through CETP expression underlines the interdependency of various HDL modulators to achieve atheroprotection. Finally, bone marrow transplantation experiments and studies with LXR agonists have provided good evidence that promotion of cellular cholesterol efflux from the vascular macrophage confers atheroprotection by promoting the initial steps of the RCT pathway. However, it should be noted that these processes bear no apparent relationship to plasma lipid levels, including those of HDL-C.
GENETIC STUDIES IN HUMANS
Studying families with genetic disorders of HDL metabolism and thus a life-long exposure to high or low levels of HDL-C may help to unravel whether HDL provides direct atheroprotection or not. A life-long exposure to 30–60% reductions of HDL-C levels as a consequence of mutations in ABCA1, APOAI, or LCAT has been reported to be associated with increased cIMT and CVD risk in several family studies (49, 158–162) but other investigators have not found this (163, 164). The APOA1Milano defect, leading to very low levels of HDL-C, has been associated with a normal cIMT in carriers (165). This has led some to believe that apoA-IMilano is more atheroprotective than normal apoA-I, (165) but one may also interpret this as evidence that HDL does not protect. Although this specific apoA-I mutation has been reported to induce enhanced cellular cholesterol efflux compared with wild-type apoA-I (165), others have disputed this (166).
Human studies of functional mutations in genes that are associated with higher HDL-C plasma levels have not given a clear picture thus far. In line with the HDL hypothesis, carriers of CETP mutations were initially reported to have vascular benefit but this concept was not supported by later studies (167). Several reports have indicated that HL deficiency is associated with high HDL-C but the number of subjects studied is too small to draw conclusions on the effect on atherosclerosis (168). Individuals with functional mutations in EL have been reported to exhibit increased HDL-C levels but to date there is no information on the risk of atherosclerosis in these carriers (169). Thus far, only one family study by our group describes a mutation in SR-BI affecting HDL metabolism (unpublished observations).
Under the assumptions of Mendelian randomization (170), the existence of a causal relationship between HDL-C levels and CVD would imply that associations between a gene variant and HDL-C levels will translate into an altered risk of disease. This concept was recently used by Danish investigators who studied the impact of mutations in ABCA1 and HL on future CVD in the general population. In two population cohorts and a large case-control study, Frikke-Schmidt et al. (171) have studied ABCA1 mutations and found that an ∼30% lower HDL-C associated with functional mutations in ABCA1 did not predict cardiovascular risk in the general population and in CVD patients. For HL, three functional variants have been shown to be associated with a modest rise in HDL-C levels without changing the risk of CVD (172).
Single nucleotide polymorphisms (SNP) in CETP presumably have the highest impact on HDL-C of all common genetic variants that have hitherto been studied throughout the genome. A recent meta-analysis on CETP genotypes and CAD risk in 196,367 subjects (46 studies combined) showed 5% risk reductions for three CETP polymorphisms, all of which are associated with lower CETP concentration and activity. Because these variants conferred both ∼5% higher HDL-C levels as well as ∼1% lower LDL-C and ∼2% lower triglyceride levels (173), it cannot be excluded that the association of these variants with apoB lipoproteins was responsible for the observed impact on CVD risk. In fact, a 5% risk reduction for a lifelong 1% reduction in LDL-C is proportional to that found for a common genetic variant in the LDL receptor gene, where a 5% increase in LDL-C was associated with an odds ratio for CVD of 1.29 (174).
Genome-wide association studies have recently provided new data on loci that modulate lipids and (apo)lipoproteins as well as CVD risk. In 2,000 CAD cases and more than 12,000 controls, it was shown that 11 SNPs associated with elevated LDL-C levels increased CVD risk. (174) In contrast, 16 SNPs associated with changes in HDL-C levels (in or near CETP, LIPC, LPL, GALNT2, LIPG, ABCA1, MVK/MMAB, LCAT, and GRIN3A) were not associated with CVD risk (174). In addition, Kathiresan et al. (175) reported that a genotype score, crafted from a combination of four HDL SNPs and five LDL SNPs, was an independent risk factor for CVD. Genotype scores for HDL-C or LDL-C also predicted cardiovascular events separately, but the effects of the individual SNPs on risk were not reported (175).
In conclusion, the published cross-sectional family-based candidate gene studies suffer from small numbers, ascertainment bias, and lack of prospective follow-up. This means that the results may be skewed because samples are taken from families who have come to a physician's attention rather than from the general population (171). Bypassing referral bias and cross-sectional designs, large prospective population studies have indicated that nonsynonymous mutations in ABCA1 and HL have no effect on CVD risk, nothwithstanding profound effects on HDL metabolism. Recent evidence obtained from large epidemiological and genome-wide association study analyses do not support the HDL hypothesis, either. In fact, a direct head-to-head comparison between genetic variants affecting either plasma LDL-C or HDL-C in a very large study (174) indicated that only the former predict CVD.
CLINICAL TRIALS
This section focuses on therapeutic modalities that affect HDL and have been studied for anti-atherosclerotic efficacy in humans or show particular promise for the future.
Fibric acid
Fibrates have primarily been developed on the basis of their cholesterol- and triglyceride-lowering activity in rodents. This class of drugs comprises agonists of the peroxisome proliferator-activator receptor-α (PPAR-α) mostly expressed in muscle and liver. They induce triglyceride catabolism and hepatic fatty acid uptake, reduce hepatic triglyceride production, increase the removal of LDL from plasma, reduce CETP activity, and increase the production of apoA-I and apoA-II (176). In humans, fibrates have been shown to reduce triglyceride levels by 18–48% and LDL-C levels by 8–13% while increasing HDL-C up to 10% (177, 178). In a posthoc analysis of the Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial (VA-HIT), which studied the atheroprotective effect of gemfibrozil in 2,531 men with a history of coronary heart disease, the cardiovascular event rate was found to be inversely associated with on-trial HDL-C levels. This has been interpreted as evidence in favor of a causal relationship between HDL-C and CVD (178). However, in light of the much stronger triglyceride-lowering effect, the strong inverse biological relationship between HDL-C and triglycerides, and the much higher variability of triglyceride measurements, this interpretation is not conclusive. On the other hand, a recent meta-analysis suggests that fibrates are efficacious: they were shown to reduce the risk of nonfatal myocardial infarction by 22% without influencing mortality, cancer, or stroke (179).
Nicotinic acid
Nicotinic acid, also known as niacin or vitamin B3, lowers triglycerides and LDL-C by 20% and 12%, respectively, and can increase HDL-C levels up to 23% (177). Niacin inhibits hepatic triglyceride synthesis, thereby decreasing plasma apoB-containing lipoproteins, and raises HDL-C levels by decreasing hepatic holoparticle HDL uptake through inhibition of the expression of hepatic ATP synthase β chain. A third target for niacin is the G-protein-coupled receptor GPR109A (PUMA-G in mice). Although this receptor has been shown to be critical to niacin's lipid-altering effects in mice, the relevance of this receptor in humans is controversial (180). An argument against a role for GPR109A is the absence of its expression in the human liver, which is thought to be a primary target organ of niacin (180). Finally, experiments with APOE*3-Leiden/CETPtg mice showed that the HDL-C increasing effect of niacin is at least partly mediated by inhibition of hepatic CETP expression (181). Niacin was reported to improve subclinical measures of atherosclerosis as well as cardiovascular event rates in a few small trials. In 160 patients, the HDL-Atherosclerosis Treatment Study (HATS) showed that a niacin simvastatin combination therapy led to a lower cardiovascular event rate compared with placebo (182). The subsequent Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2 study examined the impact of the addition of extended-release niacin to statin therapy on cIMT progression in 167 patients with established coronary heart disease (and low HDL-C). In this study, no significant difference in cIMT progression was found between the treatment arms, but a significant cIMT progression occurred in the statin-only arm versus baseline in absence of a significant progression in the niacin arm (183). In the ARBITER 3 study, 104 participants were treated with extended-release niacin and these subjects showed a net cIMT regression. However, in these cases an open-label design and the lack of a control arm constitute serious limitations (184). Very recently, two carotid imaging studies provided additional encouraging evidence of atheroprotection conferred by extended-release niacin on top of statins (185, 186). Although these reports strongly emphasized the impact of niacin on HDL-C levels, the studies show similar profound changes in triglyceride levels.
The development of fibrates and nicotinic acid derivatives was not founded on the HDL hypothesis; rather, their potential to increase HDL-C has been welcomed as a side-effect. Although these drugs unmistakably have atheroprotective potential, given their broad spectrum of effects on lipid metabolism, it is difficult to confidently ascribe this beneficial effect to their impact on HDL-C.
HDL-like particles
Several investigators have studied the effects of infusion of HDL-like particles. In a study performed by Eriksson et al. (35), the intravenous infusion of human proapoA-I liposome complexes in four subjects with heterozygous familial hypercholesterolemia was shown to increase fecal cholesterol excretion, lending support to the classical RCT concept. In 2003, a widely-cited study reported regression of coronary plaque atheroma volume compared with baseline after infusion of recombinant apoA-IMilano/phospholipid complexes (187). This study was of great conceptual importance but it only comprised 45 patients in the active arm and 12 patients in the placebo arm, leaving it underpowered for a formal direct comparison between treatment arms. In addition, the investigators did not observe a dose-effect relation (188). Other investigators used a similar compound, rHDL, in a larger study. In this placebo-controlled trial with 145 patients, four weekly infusions of rHDL proved ineffective in reducing coronary plaque atheroma volume versus placebo, although plaque regression relative to baseline in the active arm of the study was observed (189).
Larger studies with HDL infusion protocols showing reduced plaque burden and a reduction in hard clinical endpoints could provide a good basis for the HDL hypothesis. At this point, however, the data on the effect of relatively short-term HDL infusion studies are scarce and in our opinion disappointing.
CETP inhibition
By inhibiting CETP, the normal exchange of neutral lipids between apoA-I and apoB-containing lipoproteins is blocked, which results in higher HDL-C and lower LDL-C levels (190). Administration of CETP inhibitors dalcetrapib (previously denoted as JTT-705), torcetrapib, and anacetrapib has been shown to potently increase plasma HDL-C concentrations in humans (191–193). Although phase III trials with dalcetrapib and anacetrapib were recently initiated, similar studies with torcetrapib were prematurely halted in 2006: the large phase III mortality and morbidity trial Investigation of Lipid Level Management to Understand its IMpact IN ATherosclerotic Events (ILLUMINATE) was terminated because of significantly higher cardiovascular and noncardiovascular mortality rates in the atorvastatin/torcetrapib arm (194). Concurrent imaging trials did not show positive effects of torcetrapib treatment on cIMT (195, 196) nor on coronary percent atheroma volume when applied on top of atorvastatin therapy (197). The question is whether the failure of torcetrapib can be attributed to CETP inhibition in general or to off-target toxicity. Focusing on the latter, torcetrapib use has consistently been associated with increased blood pressure, elevated plasma aldosterone levels, and electrolyte changes (194–198). These effects appear to be specific to torcetrapib because other CETP inhibitors have no effect on blood pressure (199). Moreover, these effects were independent of the inhibition of CETP as torcetrapib also evoked an acute increase in blood pressure and plasma adrenal steroids in naturally CETP deficient mice whereas anacetrapib had no such effects (200). Although these findings indicate off-target toxicity for torcetrapib, they leave open the question whether CETP inhibition constitutes a viable strategy for atheroprotection. Results from ongoing CETP inhibition trials may provide the answer in the next few years.
ApoA-I mimetic peptides and stimulation of apoA-I synthesis
These peptides, seldom affecting HDL cholesterol levels, shift the focus to functional attributes of HDL. Some apoA-I mimetic peptides have been reported to result in the formation of preβ-like HDL particles, to increase anti-oxidative paraoxonase activity, and to decrease HDL lipid hydroperoxides (201). One of these peptides, orally administered D-4F, has been show to be safe and well tolerated in a first trial in humans (202) but data in humans on the efficacy of these compounds is unavailable at this point. In contrast to the scant data in humans, mouse studies with apoA-I mimetic peptides have shown promise to reduce atherosclerosis and endothelial dysfunction (203).
Based on the positive data on apoA-I overexpression in animal models, strategies to increase apoA-I synthesis are vigorously pursued. RVX-208 is a compound that was specifically developed to increase endogenous apoA-I production. In African green monkeys, oral administration resulted in increased levels of plasma apoA-I and HDL-C (204). Serum taken from these animals was shown to mediate enhanced cholesterol efflux from J774 macrophages via the ABCA1 pathway, probably related to higher concentrations of small HDL particles (204). At this point, there are no published data available regarding effects on atherosclerosis. A phase III clinical trial is currently planned.
In summary, there is evidence for fibrates and niacin as anti-atherosclerotic agents, but because both drugs have major effects on other blood lipids, this does not prove that HDL is causal to the observed atheroprotection. A large ongoing outcome trial with niacin (HPS2-THRIVE) may provide the statistical power to indirectly assess the effect of an increase in HDL-C in 2013. The use of apoA-I mimetic peptides has yet to be proven to have clinical relevance, whereas infusions of HDL-like particles have shown promise in preclinical studies and small-scale clinical trials but have thus far not improved cardiovascular outcome in larger studies. To date, the most powerful tools to raise plasma HDL-C concentrations are CETP inhibitors. Whether these drugs decrease CVD risk may be learned from two large outcome trials of which the results are expected in 2012. Drugs that specifically upregulate apoA-I may be the ultimate means to prove that HDL protects from CVD in humans, but these compounds are in early clinical development.
CONCLUSIONS
A considerable and diverse body of evidence has been generated to support the hypothesis that HDL protects against atherosclerosis. However, caution is needed as the strong urge for novel drugs to decrease CVD risk may have biased this field of research. The most convincing evidence for the HDL hypothesis has been generated through tissue culture and animal experiments with suggestive evidence from epidemiological studies. However, direct evidence from human studies is almost absent.
Adjusting for confounders in the relationship between HDL and CVD
Many risk factors for CVD also influence HDL-C levels, thereby blurring the relationship between HDL and CVD. Statistical adjustment for these potential confounders relies on three assumptions: that the relationships between confounders and HDL-C and CVD are linear, independent of each other, and assessed with great precision. It is, however, safe to state that, for many confounders, none of these assumptions hold. It is well established that associations between parameters in epidemiological studies can only aid the formulation of hypotheses, which need to be tested by experimental research. In this respect, the results of vitamin E supplementation, hormonal replacement therapy, or homocysteine lowering by folic acid and vitamin B supplementation are unsettling examples of promising epidemiological relationships which turned sour in a clinical trial setting (205–207). The HDL hypothesis, too, should be subjected to rigorous experimental testing.
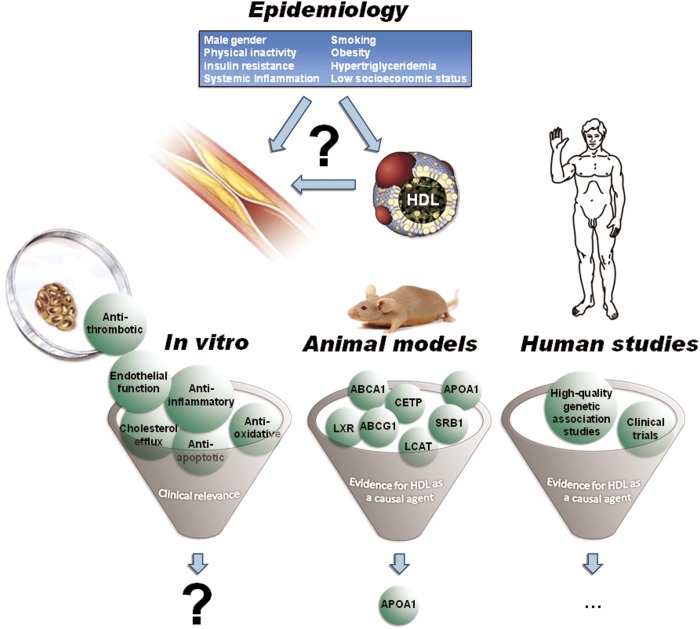
In our view, the HDL hypothesis remains a hypothesis to date (summarized in Fig. 1). This relates first of all to the challenge to study HDL independent from effects on other plasma lipids and lipoproteins, which is true for epidemiology and animal studies as well as for clinical trials. The heterogeneity of HDL represents a second major hurdle. Most studies carried out thus far have focused on plasma HDL-C concentrations as a marker of the protection that is associated with HDL. However, it has become increasingly clear that this may be an oversimplification. The studies with the CETP inhibitor torcetrapib are a hallmark in this respect, with increased levels of HDL-C obviously not being predictive of a better outcome (194). Moreover, earlier studies have shown that interventions in HDL metabolism may affect atherosclerosis in the absence of effects on plasma HDL-C concentrations (104, 201). Although it is conceivable that HDL subspecies, or individual HDL components will better predict atherosclerosis, studies into these matters have thus far only provided many hypotheses (208) and the translation of such data to clinical practice is in its infancy. Strategies aimed at improving HDL function may prove useful, but HDL function, a poorly defined concept to date, is not easily assessed. What is needed first is convincing evidence that HDL function parameters can both predict the occurrence of CVD as well as a beneficial therapeutic intervention in humans.
Fig. 1.
Evidence for the HDL hypothesis. Although epidemiological studies have established a strong negative relationship between HDL cholesterol and cardiovascular disease, there are many variables which affect HDL cholesterol levels as well as cardiovascular disease risk simultaneously; the role of these potential confounders is unclear. On the basis of in vitro experiments, HDL has been credited with many putative atheroprotective qualities, but clinical relevance has not been convincingly proven for any of these properties. Animal models yielded conflicting results for most of the key players in HDL metabolism with respect to their effect on plasma HDL levels and atherosclerosis propensity. Only apoA-I, the primary structural protein of HDL, showed a strong and consistent atheroprotective tendency in overexpression and infusion models. In humans, both high-quality genetic association studies and clinical trials have thus far not provided clear-cut evidence in favor of the hypothesis that HDL protects from atherosclerosis.
Genetic studies offer another interesting means to study the HDL hypothesis. Data from very large genetic association studies will soon provide the statistical power needed to test whether HDL gene variation affects atherosclerosis or not. However, many of the genetic variants that affect HDL-C levels also affect other lipid parameters.
With respect to clinical trials, only those compounds causing an isolated HDL increase can be expected to offer a direct answer to the primary question of this review. Atherosclerosis imaging and clinical endpoint trials with specific apoA-I agonists are best suited to this goal, because these compounds target the de novo HDL production at its natural production site and have little or no effect on other lipid parameters. The infusion of HDL-like macromolecules constitutes another means to study whether HDL provides atheroprotection but, if successful, the intravenous route of administration is bound to limit its application in daily clinical practice.
Irrespective of the outcome of ongoing trials, the identification of putative drug targets related to HDL pathways remains of great importance. Research into macrophage cholesterol homeostasis and, more specifically, cholesterol efflux has already provided interesting targets for therapy. With macrophages at the culprit of atherosclerotic plaque development, the right intervention directed at these cells can be expected to provide atheroprotection. However, here too, stronger evidence to link macrophage cholesterol efflux to CVD in humans would be welcome.
Acknowledgments
We are indebted to Haydn Pritchard (University of British Columbia, Vancouver) for valuable suggestions and textual advice.
Footnotes
Abbreviations:
- ABC
- ATP-binding cassette
- apo
- apolipoprotein
- CETP
- cholesteryl ester transfer protein
- cIMT
- carotid intima media thickness
- CVD
- cardiovascular disease
- EL
- endothelial lipase
- HDL-C
- HDL cholesterol
- HL
- hepatic lipase
- LCAT
- lecithin-cholesterol acyl transferase
- LDL-C
- LDL cholesterol
- LDLr
- LDL receptor
- LXR
- Liver X receptor
- RCT
- reverse cholesterol transport
- rHDL
- reconstituted HDL
- SNP
- single nucleotide polymorphism
- SR-BI
- scavenger receptor B-I
HDL research at the Academic Medical Center in Amsterdam is supported by a grant from the EU (FP6-LSHM-CT-2006-037631; HDLomics). A. G. Holleboom is supported by a grant from the Netherlands Organisation for Scientific Research (NWO; project number 021.001.035). M.V., A.G.H. and J.A.K. have no conflicts of interest to report. J.J.P.K. reports receiving consulting fees from Sankyo, ISIS, Novartis, Genzyme, Pfizer, Roche, AstraZeneca, Merck, and Schering-Plough; being paid lecture fees from Pfizer, Roche, AstraZeneca, Genzyme, Merck, and Schering-Plough; and receiving grant support from AstraZeneca, Merck, Pfizer, Roche, and Schering-Plough.
REFERENCES
- 1.Barr D. P., Russ E., Eder H. 1951. Protein-lipid relationships in human plasma. II. In atherosclerosis and related conditions. Am. J. Med. 11: 480–493. [DOI] [PubMed] [Google Scholar]
- 2.Gordon T., Castelli W. P., Hjortland M. C., Kannel W. B., Dawber T. R. 1977. High density lipoprotein as a protective factor against coronary heart disease: The Framingham study. Am. J. Med. 62: 707–714. [DOI] [PubMed] [Google Scholar]
- 3.Gordon D. J., Probstfield J. L., Garrison R. J., Neaton J. D., Castelli W. P., Knoke J. D., Jacobs D. R., Jr., Bangdiwala S., Tyroler H. A. 1989. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 79: 8–15. [DOI] [PubMed] [Google Scholar]
- 4.Blood Pressure Lowering Treatment Trialists’ Collaboration. 2008. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 336: 1121–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cholesterol Treatment Trialists’ (CTT) Collaborators. 2005. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 366: 1267–1278. [DOI] [PubMed] [Google Scholar]
- 6.Hausenloy D. J., Yellon D. M. 2008. Targeting residual cardiovascular risk: raising high-density lipoprotein cholesterol levels. Heart. 94: 706–714. [DOI] [PubMed] [Google Scholar]
- 7.Wild S., Byrne C. D. 2008. Time to rethink high-density lipoprotein? Heart. 94: 692–694. [DOI] [PubMed] [Google Scholar]
- 8.Hansel B., Kontush A., Giral P., Bonnefont-Rousselot D., Chapman M. J., Bruckert E. 2006. One third of the variability in HDL-cholesterol level in a large dyslipidaemic population is predicted by age, sex and triglyceridaemia: The Paris La Pitie Study. Curr. Med. Res. Opin. 22: 1149–1160. [DOI] [PubMed] [Google Scholar]
- 9.Criqui M. H., Wallace R. B., Heiss G., Mishkel M., Schonfeld G., Jones G. T. 1980. Cigarette smoking and plasma high-density lipoprotein cholesterol. The Lipid Research Clinics Program Prevalence Study. Circulation. 62: IV70–IV76. [PubMed] [Google Scholar]
- 10.Hulley S. B., Cohen R., Widdowson G. 1977. Plasma high-density lipoprotein cholesterol level. Influence of risk factor intervention. JAMA. 238: 2269–2271. [PubMed] [Google Scholar]
- 11.Gnasso A., Haberbosch W., Schettler G., Schmitz G., Augustin J. 1984. Acute influence of smoking on plasma lipoproteins. Klin. Wochenschr. 62(Suppl 2): 36–42. [PubMed] [Google Scholar]
- 12.Kodama S., Tanaka S., Saito K., Shu M., Sone Y., Onitake F., Suzuki E., Shimano H., Yamamoto S., Kondo K., et al. 2007. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch. Intern. Med. 167: 999–1008. [DOI] [PubMed] [Google Scholar]
- 13.Rashid S., Genest J. 2007. Effect of obesity on high-density lipoprotein metabolism. Obesity (Silver Spring). 15: 2875–2888. [DOI] [PubMed] [Google Scholar]
- 14.Busetto L., Sergi G., Enzi G., Segato G., De Marchi F., Foletto M., De Luca M., Pigozzo S., Favretti F. 2004. Short-term effects of weight loss on the cardiovascular risk factors in morbidly obese patients. Obesity (Silver Spring). 12: 1256–1263. [DOI] [PubMed] [Google Scholar]
- 15.Chahil T. J., Ginsberg H. N. 2006. Diabetic dyslipidemia. Endocrinol. Metab. Clin. North Am. 35: 491–510. [DOI] [PubMed] [Google Scholar]
- 16.Lann D., LeRoith D. 2007. Insulin resistance as the underlying cause for the metabolic syndrome. Med. Clin. North Am. 91: 1063–1077. [DOI] [PubMed] [Google Scholar]
- 17.Hayek T., Azrolan N., Verdery R. B., Walsh A., Chajek-Shaul T., Agellon L. B., Tall A. R., Breslow J. L. 1993. Hypertriglyceridemia and cholesteryl ester transfer protein interact to dramatically alter high density lipoprotein levels, particle sizes, and metabolism. Studies in transgenic mice. J. Clin. Invest. 92: 1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tai E. S., Emmanuel S. C., Chew S. K., Tan B. Y., Tan C. E. 1999. Isolated low HDL cholesterol: an insulin-resistant state only in the presence of fasting hypertriglyceridemia. Diabetes. 48: 1088–1092. [DOI] [PubMed] [Google Scholar]
- 19.van Leuven S. I., Franssen R., Kastelein J. J., Levi M., Stroes E. S. G., Tak P. P. 2008. Systemic inflammation as a risk factor for atherothrombosis. Rheumatology. 47: 3–7. [DOI] [PubMed] [Google Scholar]
- 20.Khovidhunkit W., Memon R. A., Feingold K. R., Grunfeld C. 2000. Infection and inflammation-induced proatherogenic changes of lipoproteins. J. Infect. Dis. 181: S462–S472. [DOI] [PubMed] [Google Scholar]
- 21.Heiss G., Haskell W., Mowery R., Criqui M. H., Brockway M., Tyroler H. A. 1980. Plasma high-density lipoprotein cholesterol and socioeconomic status. The Lipid Research Clinics Program Prevalence Study. Circulation. 62: IV108–IV115. [PubMed] [Google Scholar]
- 22.Sapolsky R. M., Mott G. E. 1987. Social subordinance in wild baboons is associated with suppressed high density lipoprotein-cholesterol concentrations: the possible role of chronic social stress. Endocrinology. 121: 1605–1610. [DOI] [PubMed] [Google Scholar]
- 23.Di Angelantonio E., Sarwar N., Perry P., Kaptoge S., Ray K. K., Thompson A., Wood A. M., Lewington S., Sattar N., Packard C. J., et al. 2009. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 302: 1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becher H. 1992. The concept of residual confounding in regression models and some applications. Stat. Med. 11: 1747–1758. [DOI] [PubMed] [Google Scholar]
- 25.Asztalos B. F., Cupples L. A., Demissie S., Horvath K. V., Cox C. E., Batista M. C., Schaefer E. J. 2004. High-density lipoprotein subpopulation profile and coronary heart disease prevalence in male participants of the Framingham Offspring Study. Arterioscler. Thromb. Vasc. Biol. 24: 2181–2187. [DOI] [PubMed] [Google Scholar]
- 26.Kontush A., Chapman M. J. 2006. Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis. Pharmacol. Rev. 58: 342–374. [DOI] [PubMed] [Google Scholar]
- 27.Fielding C. J., Fielding P. E. 1982. Cholesterol transport between cells and body fluids. Role of plasma lipoproteins and the plasma cholesterol esterification system. Med. Clin. North Am. 66: 363–373. [DOI] [PubMed] [Google Scholar]
- 28.Groen A. K., Bloks V. W., Bandsma R. H., Ottenhoff R., Chimini G., Kuipers F. 2001. Hepatobiliary cholesterol transport is not impaired in Abca1-null mice lacking HDL. J. Clin. Invest. 108: 843–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alam K., Meidell R. S., Spady D. K. 2001. Effect of up-regulating individual steps in the reverse cholesterol transport pathway on reverse cholesterol transport in normolipidemic mice. J. Biol. Chem. 276: 15641–15649. [DOI] [PubMed] [Google Scholar]
- 30.deGoma E. M., deGoma R. L., Rader D. J. 2008. Beyond high-density lipoprotein cholesterol levels evaluating high-density lipoprotein function as influenced by novel therapeutic approaches. J. Am. Coll. Cardiol. 51: 2199–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miettinen T. A., Kesaniemi Y. A. 1989. Cholesterol absorption: regulation of cholesterol synthesis and elimination and within-population variations of serum cholesterol levels. Am. J. Clin. Nutr. 49: 629–635. [DOI] [PubMed] [Google Scholar]
- 32.Gylling H., Miettinen T. A. 1992. Non-cholesterol sterols, absorption and synthesis of cholesterol and apolipoprotein A-I kinetics in a Finnish lecithin-cholesterol acyltransferase deficient family. Atherosclerosis. 95: 25–33. [DOI] [PubMed] [Google Scholar]
- 33.Beher W. T., Gabbard A., Norum R. A., Stradnieks S. 1983. Effect of blood high density lipoprotein cholesterol concentration on fecal steroid excretion in humans. Life Sci. 32: 2933–2937. [DOI] [PubMed] [Google Scholar]
- 34.El-Harchaoui K., Franssen R., Hovingh G. K., Bisoendial R. J., Stellaard F., Kuipers F., Kastelein J. J., Kuivenhoven J. A., Stroes E. S., Groen A. K. 2009. Reduced fecal sterol excretion in subjects with familial hypoalphalipoproteinemia. Atherosclerosis. 207: 614–616. [DOI] [PubMed] [Google Scholar]
- 35.Eriksson M., Carlson L. A., Miettinen T. A., Angelin B. 1999. Stimulation of fecal steroid excretion after infusion of recombinant proapolipoprotein A-I: potential reverse cholesterol transport in humans. Circulation. 100: 594–598. [DOI] [PubMed] [Google Scholar]
- 36.Nanjee M. N., Cooke C. J., Garvin R., Semeria F., Lewis G., Olszewski W. L., Miller N. E. 2001. Intravenous apoA-I/lecithin discs increase pre-beta-HDL concentration in tissue fluid and stimulate reverse cholesterol transport in humans. J. Lipid Res. 42: 1586–1593. [PubMed] [Google Scholar]
- 37.Brousseau M. E., Diffenderfer M. R., Millar J. S., Nartsupha C., Asztalos B. F., Welty F. K., Wolfe M. L., Rudling M., Bjorkhem I., Angelin B., et al. 2005. Effects of cholesteryl ester transfer protein inhibition on high-density lipoprotein subspecies, apolipoprotein A-I metabolism, and fecal sterol excretion. Arterioscler. Thromb. Vasc. Biol. 25: 1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwartz C. C., Berman M., Vlahcevic Z. R., Halloran L. G., Gregory D. H., Swell L. 1978. Multicompartmental analysis of cholesterol metabolism in man. Characterization of the hepatic bile acid and biliary cholesterol precursor sites. J. Clin. Invest. 61: 408–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Turner S. M., Hellerstein M. K. 2005. Emerging applications of kinetic biomarkers in preclinical and clinical drug development. Curr. Opin. Drug Discov. Devel. 8: 115–126. [PubMed] [Google Scholar]
- 40.Yvan-Charvet L., Matsuura F., Wang N., Bamberger M. J., Nguyen T., Rinninger F., Jiang X. C., Shear C. L., Tall A. R. 2007. Inhibition of cholesteryl ester transfer protein by torcetrapib modestly increases macrophage cholesterol efflux to HDL. Arterioscler. Thromb. Vasc. Biol. 27: 1132–1138. [DOI] [PubMed] [Google Scholar]
- 41.Chirinos J. A., Zambrano J. P., Chakko S., Schob A., Goldberg R. B., Perez G., Mendez A. J. 2005. Ability of serum to decrease cellular acylcoA:cholesterol acyl transferase activity predicts cardiovascular outcomes. Circulation. 112: 2446–2453. [DOI] [PubMed] [Google Scholar]
- 42.Oram J. F., Lawn R. M., Garvin M. R., Wade D. P. 2000. ABCA1 is the cAMP-inducible apolipoprotein receptor that mediates cholesterol secretion from macrophages. J. Biol. Chem. 275: 34508–34511. [DOI] [PubMed] [Google Scholar]
- 43.Wang N., Lan D., Chen W., Matsuura F., Tall A. R. 2004. ATP-binding cassette transporters G1 and G4 mediate cellular cholesterol efflux to high-density lipoproteins. Proc. Natl. Acad. Sci. USA. 101: 9774–9779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pagler T. A., Rhode S., Neuhofer A., Laggner H., Strobl W., Hinterndorfer C., Volf I., Pavelka M., Eckhardt E. R., van der Westhuyzen D. R., et al. 2006. SR-BI-mediated high density lipoprotein (HDL) endocytosis leads to HDL resecretion facilitating cholesterol efflux. J. Biol. Chem. 281: 11193–11204. [DOI] [PubMed] [Google Scholar]
- 45.Pirillo A., Uboldi P., Kuhn H., Catapano A. L. 2006. 15-Lipoxygenase-mediated modification of high-density lipoproteins impairs SR-BI- and ABCA1-dependent cholesterol efflux from macrophages. Biochim. Biophys. Acta. 1761: 292–300. [DOI] [PubMed] [Google Scholar]
- 46.Stangl H., Cao G., Wyne K. L., Hobbs H. H. 1998. Scavenger receptor, class B, type I-dependent stimulation of cholesterol esterification by high density lipoproteins, low density lipoproteins, and nonlipoprotein cholesterol. J. Biol. Chem. 273: 31002–31008. [DOI] [PubMed] [Google Scholar]
- 47.Ji Y., Jian B., Wang N., Sun Y., Moya Mdl L., Phillips M. C., Rothblat G. H., Swaney J. B., Tall A. R. 1997. Scavenger Receptor BI promotes high density lipoprotein-mediated cellular cholesterol efflux. J. Biol. Chem. 272: 20982–20985. [DOI] [PubMed] [Google Scholar]
- 48.Wang X., Collins H. L., Ranalletta M., Fuki I. V., Billheimer J. T., Rothblat G. H., Tall A. R., Rader D. J. 2007. Macrophage ABCA1 and ABCG1, but not SR-BI, promote macrophage reverse cholesterol transport in vivo. J. Clin. Invest. 117: 2216–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Dam M. J., de Groot E., Clee S. M., Hovingh G. K., Roelants R., Brooks-Wilson A., Zwinderman A. H., Smit A. J., Smelt A. H., Groen A. K., et al. 2002. Association between increased arterial-wall thickness and impairment in ABCA1-driven cholesterol efflux: an observational study. Lancet. 359: 37–42. [DOI] [PubMed] [Google Scholar]
- 50.Linsel-Nitschke P., Jansen H., Aherrarhou Z., Belz S., Mayer B., Huber F., Kremer W., Kalbitzer H. R., Erdmann J., Schunkert H. 2009. Macrophage cholesterol efflux correlates with lipoprotein subclass distribution and risk of obstructive coronary artery disease in patients undergoing coronary angiography. Lipids Health Dis. 8: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cockerill G. W., Rye K. A., Gamble J. R., Vadas M. A., Barter P. J. 1995. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler. Thromb. Vasc. Biol. 15: 1987–1994. [DOI] [PubMed] [Google Scholar]
- 52.Navab M., Imes S. S., Hama S. Y., Hough G. P., Ross L. A., Bork R. W., Valente A. J., Berliner J. A., Drinkwater D. C., Laks H. 1991. Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J. Clin. Invest. 88: 2039–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moudry R., Spycher M. O., Doran J. E. 1997. Reconstituted high density lipoprotein modulates adherence of polymorphonuclear leukocytes to human endothelial cells. Shock. 7: 175–181. [DOI] [PubMed] [Google Scholar]
- 54.Navab M., Berliner J. A., Subbanagounder G., Hama S., Lusis A. J., Castellani L. W., Reddy S., Shih D., Shi W., Watson A. D., et al. 2001. HDL and the inflammatory response induced by LDL-derived oxidized phospholipids. Arterioscler. Thromb. Vasc. Biol. 21: 481–488. [DOI] [PubMed] [Google Scholar]
- 55.Lee C. M., Chien C. T., Chang P. Y., Hsieh M. Y., Jui H. Y., Liau C. S., Hsu S. M., Lee Y. T. 2005. High-density lipoprotein antagonizes oxidized low-density lipoprotein by suppressing oxygen free-radical formation and preserving nitric oxide bioactivity. Atherosclerosis. 183: 251–258. [DOI] [PubMed] [Google Scholar]
- 56.Robbesyn F, Garcia V, Auge N, Vieira O, Frisach MF, Salvayre R, Negre-Salvayre A. 2003. HDL counterbalance the proinflammatory effect of oxidized LDL by inhibiting intracellular reactive oxygen species rise, proteasome activation, and subsequent NF-κB activation in smooth muscle cells. FASEB J. 02–0240fje. [DOI] [PubMed] [Google Scholar]
- 57.Puranik R., Bao S., Nobecourt E., Nicholls S. J., Dusting G. J., Barter P. J., Celermajer D. S., Rye K. A. 2008. Low dose apolipoprotein A-I rescues carotid arteries from inflammation in vivo. Atherosclerosis. 196: 240–247. [DOI] [PubMed] [Google Scholar]
- 58.Nicholls S. J., Dusting G. J., Cutri B., Bao S., Drummond G. R., Rye K. A., Barter P. J. 2005. Reconstituted high-density lipoproteins inhibit the acute pro-oxidant and proinflammatory vascular changes induced by a periarterial collar in normocholesterolemic rabbits. Circulation. 111: 1543–1550. [DOI] [PubMed] [Google Scholar]
- 59.Ansell B. J., Navab M., Hama S., Kamranpour N., Fonarow G., Hough G., Rahmani S., Mottahedeh R., Dave R., Reddy S. T., et al. 2003. Inflammatory/antiinflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation. 108: 2751–2756. [DOI] [PubMed] [Google Scholar]
- 60.Navab M., Hama S. Y., Hough G. P., Subbanagounder G., Reddy S. T., Fogelman A. M. 2001. A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J. Lipid Res. 42: 1308–1317. [PubMed] [Google Scholar]
- 61.Davies P. F., Remuzzi A., Gordon E. J., Dewey C. F., Jr., Gimbrone M. A., Jr. 1986. Turbulent fluid shear stress induces vascular endothelial cell turnover in vitro. Proc. Natl. Acad. Sci. USA. 83: 2114–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Suc I., Escargueil-Blanc I., Troly M., Salvayre R., Negre-Salvayre A. 1997. HDL and apoA prevent cell death of endothelial cells induced by oxidized LDL. Arterioscler. Thromb. Vasc. Biol. 17: 2158–2166. [DOI] [PubMed] [Google Scholar]
- 63.Sugano M., Tsuchida K., Makino N. 2000. High-density lipoproteins protect endothelial cells from tumor necrosis factor-[alpha]-induced apoptosis. Biochem. Biophys. Res. Commun. 272: 872–876. [DOI] [PubMed] [Google Scholar]
- 64.Nofer J. R., Levkau B., Wolinska I., Junker R., Fobker M., von Eckardstein A., Seedorf U., Assmann G. 2001. Suppression of endothelial cell apoptosis by high density lipoproteins (HDL) and HDL-associated lysosphingolipids. J. Biol. Chem. 276: 34480–34485. [DOI] [PubMed] [Google Scholar]
- 65.Kimura T., Sato K., Kuwabara A., Tomura H., Ishiwara M., Kobayashi I., Ui M., Okajima F. 2001. Sphingosine 1-phosphate may be a major component of plasma lipoproteins responsible for the cytoprotective actions in human umbilical vein endothelial cells. J. Biol. Chem. 276: 31780–31785. [DOI] [PubMed] [Google Scholar]
- 66.Kimura T., Sato K., Malchinkhuu E., Tomura H., Tamama K., Kuwabara A., Murakami M., Okajima F. 2003. High-density lipoprotein stimulates endothelial cell migration and survival through sphingosine 1-phosphate and Its receptors. Arterioscler. Thromb. Vasc. Biol. 23: 1283–1288. [DOI] [PubMed] [Google Scholar]
- 67.Chen L. Y., Mehta J. L. 1994. Inhibitory effect of high-density lipoprotein on platelet function is mediated by increase in nitric oxide synthase activity in platelets. Life Sci. 55: 1815–1821. [DOI] [PubMed] [Google Scholar]
- 68.Nofer J. R., Kehrel B., Fobker M., Levkau B., Assmann G., von Eckardstein A. 2002. HDL and arteriosclerosis: beyond reverse cholesterol transport. Atherosclerosis. 161: 1–16. [DOI] [PubMed] [Google Scholar]
- 69.Griffin J. H., Kojima K., Banka C. L., Curtiss L. K., Fernandez J. A. 1999. High-density lipoprotein enhancement of anticoagulant activities of plasma protein S and activated protein C. J. Clin. Invest. 103: 219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oslakovic C., Krisinger M. J., Andersson A., Jauhiainen M., Ehnholm C., Dahlbäck B. 2009. Anionic phospholipids lose their procoagulant properties when incorporated into high- density lipoproteins. J. Biol. Chem. 284: 5896–5904. [DOI] [PubMed] [Google Scholar]
- 71.Deguchi H., Pecheniuk N. M., Elias D. J., Averell P. M., Griffin J. H. 2005. High-density lipoprotein deficiency and dyslipoproteinemia associated with venous thrombosis in men. Circulation. 112: 893–899. [DOI] [PubMed] [Google Scholar]
- 72.Pomp ER, le Cassie S., Rosendaal F. R., Doggen C. J. 2007. Risk of venous thrombosis: obesity and its joint effect with oral contraceptive use and prothrombotic mutations. Br. J. Haematol. 139: 289–296. [DOI] [PubMed] [Google Scholar]
- 73.Alessi M. C., Juhan-Vague I. 2008. Metabolic syndrome, haemostasis and thrombosis. Thromb. Haemost. 99: 995–1000. [DOI] [PubMed] [Google Scholar]
- 74.Yuhanna I. S., Zhu Y., Cox B. E., Hahner L. D., Osborne-Lawrence S., Lu P., Marcel Y. L., Anderson R. G. W., Mendelsohn M. E., Hobbs H. H., et al. 2001. High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nat. Med. 7: 853–857. [DOI] [PubMed] [Google Scholar]
- 75.Nieuwdorp M, Vergeer M, Bisoendial RJ, op 't Roodt J., Levels H., Birjmohun R. S., Kuivenhoven J. A., Basser R., Rabelink T. J., Kastelein J. J., Stroes E. S. 2008. Reconstituted HDL infusion restores endothelial function in patients with type 2 diabetes mellitus. Diabetologia. 51: 1081–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Spieker L. E., Sudano I., Hurlimann D., Lerch P. G., Lang M. G., Binggeli C., Corti R., Ruschitzka F., Luscher T. F., Noll G. 2002. High-density lipoprotein restores endothelial function in hypercholesterolemic men. Circulation. 105: 1399–1402. [DOI] [PubMed] [Google Scholar]
- 77.Bisoendial R. J., Hovingh G. K., Levels J. H., Lerch P. G., Andresen I., Hayden M. R., Kastelein J. J., Stroes E. S. 2003. Restoration of endothelial function by increasing high-density lipoprotein in subjects with isolated low high-density lipoprotein. Circulation. 107: 2944–2948. [DOI] [PubMed] [Google Scholar]
- 78.Russell J. C., Proctor S. D. 2006. Small animal models of cardiovascular disease: tools for the study of the roles of metabolic syndrome, dyslipidemia, and atherosclerosis. Cardiovasc. Pathol. 15: 318–330. [DOI] [PubMed] [Google Scholar]
- 79.Lusis A. J., Yu J., Wang S. S. 2007. The problem of passenger genes in transgenic mice. Arterioscler. Thromb. Vasc. Biol. 27: 2100–2103. [DOI] [PubMed] [Google Scholar]
- 80.Lichtman A. H., Clinton S. K., Iiyama K., Connelly P. W., Libby P., Cybulsky M. I. 1999. Hyperlipidemia and atherosclerotic lesion development in LDL receptor-deficient mice fed defined semipurified diets with and without cholate. Arterioscler. Thromb. Vasc. Biol. 19: 1938–1944. [DOI] [PubMed] [Google Scholar]
- 81.Plump A. S., Masucci-Magoulas L., Bruce C., Bisgaier C. L., Breslow J. L., Tall A. R. 1999. Increased atherosclerosis in apoE and LDL receptor gene knock-out mice as a result of human cholesteryl ester transfer protein transgene expression. Arterioscler. Thromb. Vasc. Biol. 19: 1105–1110. [DOI] [PubMed] [Google Scholar]
- 82.Westerterp M., van der Hoogt C. C., de Haan W., Offerman E. H., Dallinga-Thie G. M., Jukema J. W., Havekes L. M., Rensen P. C. 2006. Cholesteryl ester transfer protein decreases high-density lipoprotein and severely aggravates atherosclerosis in APOE*3-Leiden mice. Arterioscler. Thromb. Vasc. Biol. 26: 2552–2559. [DOI] [PubMed] [Google Scholar]
- 83.Li H., Reddick R. L., Maeda N. 1993. Lack of apoA-I is not associated with increased susceptibility to atherosclerosis in mice. Arterioscler. Thromb. 13: 1814–1821. [DOI] [PubMed] [Google Scholar]
- 84.Voyiaziakis E., Goldberg I. J., Plump A. S., Rubin E. M., Breslow J. L., Huang L. S. 1998. ApoA-I deficiency causes both hypertriglyceridemia and increased atherosclerosis in human apoB transgenic mice. J. Lipid Res. 39: 313–321. [PubMed] [Google Scholar]
- 85.Moore RE, Kawashiri M. A., Kitajima K., Secreto A., Millar J. S., Pratico D., Rader D. J. 2003. Apolipoprotein A-I deficiency results in markedly increased atherosclerosis in mice lacking the LDL receptor. Arterioscler. Thromb. Vasc. Biol. 23: 1914–1920. [DOI] [PubMed] [Google Scholar]
- 86.Moore R. E., Navab M., Millar J. S., Zimetti F., Hama S., Rothblat G. H., Rader D. J. 2005. Increased atherosclerosis in mice lacking apolipoprotein A-I attributable to both impaired reverse cholesterol transport and increased inflammation. Circ. Res. 97: 763–771. [DOI] [PubMed] [Google Scholar]
- 87.Nakamuta M., Taniguchi S., Ishida B. Y., Kobayashi K., Chan L. 1998. Phenotype interaction of apobec-1 and CETP, LDLR, and apoE gene expression in mice: role of apoB mRNA editing in lipoprotein phenotype expression. Arterioscler. Thromb. Vasc. Biol. 18: 747–755. [DOI] [PubMed] [Google Scholar]
- 88.Rubin E. M., Krauss R. M., Spangler E. A., Verstuyft J. G., Clift S. M. 1991. Inhibition of early atherogenesis in transgenic mice by human apolipoprotein AI. Nature. 353: 265–267. [DOI] [PubMed] [Google Scholar]
- 89.Plump A. S., Scott C. J., Breslow J. L. 1994. Human apolipoprotein A-I gene expression increases high density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse. Proc. Natl. Acad. Sci. USA. 91: 9607–9611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Paszty C., Maeda N., Verstuyft J., Rubin E. M. 1994. Apolipoprotein AI transgene corrects apolipoprotein E deficiency-induced atherosclerosis in mice. J. Clin. Invest. 94: 899–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu A. C., Lawn R. M., Verstuyft J. G., Rubin E. M. 1994. Human apolipoprotein A-I prevents atherosclerosis associated with apolipoprotein[a] in transgenic mice. J. Lipid Res. 35: 2263–2267. [PubMed] [Google Scholar]
- 92.Tangirala R. K., Tsukamoto K., Chun S. H., Usher D., Pure E., Rader D. J. 1999. Regression of atherosclerosis induced by liver-directed gene transfer of apolipoprotein A-I in Mice. Circulation. 100: 1816–1822. [DOI] [PubMed] [Google Scholar]
- 93.Benoit P., Emmanuel F., Caillaud J. M., Bassinet L., Castro G., Gallix P., Fruchart J. C., Branellec D., Denefle P., Duverger N. 1999. Somatic gene transfer of human apoA-I inhibits atherosclerosis progression in mouse models. Circulation. 99: 105–110. [DOI] [PubMed] [Google Scholar]
- 94.Belalcazar L. M., Merched A., Carr B., Oka K., Chen K. H., Pastore L., Beaudet A., Chan L. 2003. Long-term stable expression of human apolipoprotein A-I mediated by helper-dependent adenovirus gene transfer inhibits atherosclerosis progression and remodels atherosclerotic plaques in a mouse model of familial hypercholesterolemia. Circulation. 107: 2726–2732. [DOI] [PubMed] [Google Scholar]
- 95.Lebherz C., Sanmiguel J., Wilson J., Rader D. 2007. Gene transfer of wild-type apoA-I and apoA-I Milano reduce atherosclerosis to a similar extent. Cardiovasc. Diabetol. 6: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Miyazaki A., Sakuma S., Morikawa W., Takiue T., Miake F., Terano T., Sakai M., Hakamata H., Sakamoto Y. I., Naito M., et al. 1995. Intravenous injection of rabbit apolipoprotein A-I inhibits the progression of atherosclerosis in cholesterol-fed rabbits. Arterioscler. Thromb. Vasc. Biol. 15: 1882–1888. [DOI] [PubMed] [Google Scholar]
- 97.Duverger N., Kruth H., Emmanuel F., Caillaud J. M., Viglietta C., Castro G., Tailleux A., Fievet C., Fruchart J. C., Houdebine L. M., et al. 1996. Inhibition of atherosclerosis development in cholesterol-fed human apolipoprotein A-I-transgenic rabbits. Circulation. 94: 713–717. [DOI] [PubMed] [Google Scholar]
- 98.Wang N., Tall A. R. 2003. Regulation and mechanisms of ATP-binding cassette transporter A1-mediated cellular cholesterol efflux. Arterioscler. Thromb. Vasc. Biol. 23: 1178–1184. [DOI] [PubMed] [Google Scholar]
- 99.Aiello R. J., Brees D., Bourassa P. A., Royer L., Lindsey S., Coskran T., Haghpassand M., Francone O. L. 2002. Increased atherosclerosis in hyperlipidemic mice with inactivation of ABCA1 in macrophages. Arterioscler. Thromb. Vasc. Biol. 22: 630–637. [DOI] [PubMed] [Google Scholar]
- 100.Kennedy M. A., Barrera G. C., Nakamura K., Baldan A., Tarr P., Fishbein M. C., Frank J., Francone O. L., Edwards P. A. 2005. ABCG1 has a critical role in mediating cholesterol efflux to HDL and preventing cellular lipid accumulation. Cell Metab. 1: 121–131. [DOI] [PubMed] [Google Scholar]
- 101.Out R., Jessup W., Le Goff W., Hoekstra M., Gelissen I. C., Zhao Y., Kritharides L., Chimini G., Kuiper J., Chapman M. J., et al. 2008. Coexistence of foam cells and hypocholesterolemia in mice lacking the ABC transporters A1 and G1. Circ. Res. 102: 113–120. [DOI] [PubMed] [Google Scholar]
- 102.Joyce C. W., Wagner E. M., Basso F., Amar M. J., Freeman L. A., Shamburek R. D., Knapper C. L., Syed J., Wu J., Vaisman B. L., et al. 2006. ABCA1 overexpression in the liver of LDLr-KO mice leads to accumulation of pro-atherogenic lipoproteins and enhanced atherosclerosis. J. Biol. Chem. 281: 33053–33065. [DOI] [PubMed] [Google Scholar]
- 103.Joyce C. W., Amar M. J. A., Lambert G., Vaisman B. L., Paigen B., Najib-Fruchart J., Hoyt R. F., Neufeld E. D., Remaley A. T., Fredrickson D. S., et al. 2002. The ATP binding cassette transporter A1 (ABCA1) modulates the development of aortic atherosclerosis in C57BL/6 and apoE-knockout mice. Proc. Natl. Acad. Sci. USA. 99: 407–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Singaraja R. R., Fievet C., Castro G., James E. R., Hennuyer N., Clee S. M., Bissada N., Choy J. C., Fruchart J. C., McManus B. M., et al. 2002. Increased ABCA1 activity protects against atherosclerosis. J. Clin. Invest. 110: 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Basso F., Amar M. J., Wagner E. M., Vaisman B., Paigen B., Santamarina-Fojo S., Remaley A. T. 2006. Enhanced ABCG1 expression increases atherosclerosis in LDLr-KO mice on a western diet. Biochem. Biophys. Res. Commun. 351: 398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Burgess B., Naus K., Chan J., Hirsch-Reinshagen V., Tansley G., Matzke L., Chan B., Wilkinson A., Fan J., Donkin J., et al. 2008. Overexpression of human ABCG1 does not affect atherosclerosis in fat-fed ApoE-deficient mice. Arterioscler. Thromb. Vasc. Biol. 28: 1731–1737. [DOI] [PubMed] [Google Scholar]
- 107.Van Eck M., Bos I. S., Kaminski W. E., Orso E., Rothe G., Twisk J., Bötccher A., Van Amersfoort E. S., Christiansen-Weber T. A., Fung-Leung W. P., et al. 2002. Leukocyte ABCA1 controls susceptibility to atherosclerosis and macrophage recruitment into tissues. Proc. Natl. Acad. Sci. USA. 99: 6298–6303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Van Eck M., Singaraja R. R., Ye D., Hildebrand R. B., James E. R., Hayden M. R., Van Berkel T. J. C. 2006. Macrophage ATP-binding cassette transporter A1 overexpression inhibits atherosclerotic lesion progression in low-density lipoprotein receptor knockout mice. Arterioscler. Thromb. Vasc. Biol. 26: 929–934. [DOI] [PubMed] [Google Scholar]
- 109.Curtiss L. K. 2006. Is two out of three enough for ABCG1? Arterioscler. Thromb. Vasc. Biol. 26: 2175–2177. [DOI] [PubMed] [Google Scholar]
- 110.Jonas A. 2000. Lecithin cholesterol acyltransferase. Biochim. Biophys. Acta. 1529: 245–256. [DOI] [PubMed] [Google Scholar]
- 111.Lambert G., Sakai N., Vaisman B. L., Neufeld E. B., Marteyn B., Chan C. C., Paigen B., Lupia E., Thomas A., Striker L. J., et al. 2001. Analysis of glomerulosclerosis and atherosclerosis in lecithin cholesterol acyltransferase-deficient mice. J. Biol. Chem. 276: 15090–15098. [DOI] [PubMed] [Google Scholar]
- 112.Furbee J. W., Jr., Sawyer J. K., Parks J. S. 2002. Lecithin:cholesterol acyltransferase deficiency increases atherosclerosis in the low density lipoprotein receptor and apolipoprotein E knockout mice. J. Biol. Chem. 277: 3511–3519. [DOI] [PubMed] [Google Scholar]
- 113.Mertens A., Verhamme P., Bielicki J. K., Phillips M. C., Quarck R., Verreth W., Stengel D., Ninio E., Navab M., Mackness B., et al. 2003. Increased low-density lipoprotein oxidation and impaired high-density lipoprotein antioxidant defense are associated with increased macrophage homing and atherosclerosis in dyslipidemic obese mice: LCAT gene transfer decreases atherosclerosis. Circulation. 107: 1640–1646. [DOI] [PubMed] [Google Scholar]
- 114.Berard A. M., Foger B., Remaley A., Shamburek R., Vaisman B. L., Talley G., Paigen B., Hoyt R. F., Marcovina S., Brewer H. B., et al. 1997. High plasma HDL concentrations associated with enhanced atherosclerosis in transgenic mice overexpressing lecithinchoesteryl acyltransferase. Nat. Med. 3: 744–749. [DOI] [PubMed] [Google Scholar]
- 115.Foger B., Chase M., Amar M. J., Vaisman B. L., Shamburek R. D., Paigen B., Fruchart-Najib J., Paiz J. A., Koch C. A., Hoyt R. F., et al. 1999. Cholesteryl ester transfer protein corrects dysfunctional high density lipoproteins and reduces aortic atherosclerosis in lecithin cholesterol acyltransferase transgenic mice. J. Biol. Chem. 274: 36912–36920. [DOI] [PubMed] [Google Scholar]
- 116.Mehlum A., Muri M., Hagve T. A., Solberg L. A., Prydz H. 1997. Mice overexpressing human lecithin: cholesterol acyltransferase are not protected against diet-induced atherosclerosis. APMIS. 105: 861–868. [DOI] [PubMed] [Google Scholar]
- 117.Mehlum A., Gjernes E., Solberg L. A., Hagve T. A., Prydz H. 2000. Overexpression of human lecithin:cholesterol acyltransferase in mice offers no protection against diet-induced atherosclerosis. APMIS. 108: 336–342. [DOI] [PubMed] [Google Scholar]
- 118.Furbee J. W., Parks J. S. 2002. Transgenic overexpression of human lecithin: cholesterol acyltransferase (LCAT) in mice does not increase aortic cholesterol deposition. Atherosclerosis. 165: 89–100. [DOI] [PubMed] [Google Scholar]
- 119.Hoeg J. M., Santamarina-Fojo S., Berard A. M., Cornhill J. F., Herderick E. E., Feldman S. H., Haudenschild C. C., Vaisman B. L., Hoyt R. F., Jr., Demosky S. J., Jr., et al. 1996. Overexpression of lecithin:cholesterol acyltransferase in transgenic rabbits prevents diet-induced atherosclerosis. Proc. Natl. Acad. Sci. USA. 93: 11448–11453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Brousseau M. E., Santamarina-Fojo S., Vaisman B. L., Applebaum-Bowden D., Berard A. M., Talley G. D., Brewer H. B., Jr., Hoeg J. M. 1997. Overexpression of human lecithin:cholesterol acyltransferase in cholesterol-fed rabbits: LDL metabolism and HDL metabolism are affected in a gene dose-dependent manner. J. Lipid Res. 38: 2537–2547. [PubMed] [Google Scholar]
- 121.Brousseau M. E., Kauffman R. D., Herderick E. E., Demosky S. J., Jr., Evans W., Marcovina S., Santamarina-Fojo S., Brewer H. B., Jr., Hoeg J. M. 2000. LCAT modulates atherogenic plasma lipoproteins and the extent of atherosclerosis only in the presence of normal LDL receptors in transgenic rabbits. Arterioscler. Thromb. Vasc. Biol. 20: 450–458. [DOI] [PubMed] [Google Scholar]
- 122.Marotti K. R., Castle C. K., Boyle T. P., Lin A. H., Murray R. W., Melchior G. W. 1993. Severe atherosclerosis in transgenic mice expressing simian cholesteryl ester transfer protein. Nature. 364: 73–75. [DOI] [PubMed] [Google Scholar]
- 123.Plump A. S., Masucci-Magoulas L., Bruce C., Bisgaier C. L., Breslow J. L., Tall A. R. 1999. Increased atherosclerosis in ApoE and LDL receptor gene knock-out mice as a result of human cholesteryl ester transfer protein transgene expression. Arterioscler. Thromb. Vasc. Biol. 19: 1105–1110. [DOI] [PubMed] [Google Scholar]
- 124.de Haan W., de Vries-van der Weij J., van der Hoorn J. W. A., Gautier T., van der Hoogt C. C., Westerterp M., Romijn J. A., Jukema J. W., Havekes L. M., Princen H. M. G., et al. 2008. Torcetrapib does not reduce atherosclerosis beyond atorvastatin and induces more proinflammatory lesions than atorvastatin. Circulation. 117: 2515–2522. [DOI] [PubMed] [Google Scholar]
- 125.Herrera V. L., Makrides S. C., Xie H. X., Adari H., Krauss R. M., Ryan U. S., Ruiz-Opazo N. 1999. Spontaneous combined hyperlipidemia, coronary heart disease and decreased survival in Dahl salt-sensitive hypertensive rats transgenic for human cholesteryl ester transfer protein. Nat. Med. 5: 1383–1389. [DOI] [PubMed] [Google Scholar]
- 126.Hayek T., Masucci-Magoulas L., Jiang X., Walsh A., Rubin E., Breslow J. L., Tall A. R. 1995. Decreased early atherosclerotic lesions in hypertriglyceridemic mice expressing cholesteryl ester transfer protein transgene. J. Clin. Invest. 96: 2071–2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Harder C., Lau P., Meng A., Whitman S. C., McPherson R. 2007. Cholesteryl ester transfer protein (CETP) expression protects against diet induced atherosclerosis in SR-BI deficient mice. Arterioscler. Thromb. Vasc. Biol. 27: 858–864. [DOI] [PubMed] [Google Scholar]
- 128.Huang Z., Inazu A., Nohara A., Higashikata T., Mabuchi H. 2002. Cholesteryl ester transfer protein inhibitor (JTT-705) and the development of atherosclerosis in rabbits with severe hypercholesterolaemia. Clin. Sci. (Lond.). 103: 587–594. [DOI] [PubMed] [Google Scholar]
- 129.Okamoto H., Yonemori F., Wakitani K., Minowa T., Maeda K., Shinkai H. 2000. A cholesteryl ester transfer protein inhibitor attenuates atherosclerosis in rabbits. Nature. 406: 203–207. [DOI] [PubMed] [Google Scholar]
- 130.Rittershaus C. W., Miller D. P., Thomas L. J., Picard M. D., Honan C. M., Emmett C. D., Pettey C. L., Adari H., Hammond R. A., Beattie D. T., et al. 2000. Vaccine-induced antibodies inhibit CETP activity in vivo and reduce aortic lesions in a rabbit model of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 20: 2106–2112. [DOI] [PubMed] [Google Scholar]
- 131.Sugano M., Makino N., Sawada S., Otsuka S., Watanabe M., Okamoto H., Kamada M., Mizushima A. 1998. Effect of antisense oligonucleotides against cholesteryl ester transfer protein on the development of atherosclerosis in cholesterol-fed rabbits. J. Biol. Chem. 273: 5033–5036. [DOI] [PubMed] [Google Scholar]
- 132.Morehouse L. A., Sugarman E. D., Bourassa P. A., Sand T. M., Zimetti F., Gao F., Rothblat G. H., Milici A. J. 2007. Inhibition of CETP activity by torcetrapib reduces susceptibility to diet- induced atherosclerosis in New Zealand White rabbits. J. Lipid Res. 48: 1263–1272. [DOI] [PubMed] [Google Scholar]
- 133.Acton S., Rigotti A., Landschulz K. T., Xu S., Hobbs H. H., Krieger M. 1996. Identification of scavenger receptor SR-BI as a high density lipoprotein receptor. Science. 271: 518–520. [DOI] [PubMed] [Google Scholar]
- 134.Rigotti A., Trigatti B. L., Penman M., Rayburn H., Herz J., Krieger M. 1997. A targeted mutation in the murine gene encoding the high density lipoprotein (HDL) receptor scavenger receptor class B type I reveals its key role in HDL metabolism. Proc. Natl. Acad. Sci. USA. 94: 12610–12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Huby T., Doucet C., Dachet C., Ouzilleau B., Ueda Y., Afzal V., Rubin E., Chapman M. J., Lesnik P. 2006. Knockdown expression and hepatic deficiency reveal an atheroprotective role for SR-BI in liver and peripheral tissues. J. Clin. Invest. 116: 2767–2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Braun A., Trigatti B. L., Post M. J., Sato K., Simons M., Edelberg J. M., Rosenberg R. D., Schrenzel M., Krieger M. 2002. Loss of SR-BI expression leads to the early onset of occlusive atherosclerotic coronary artery disease, spontaneous myocardial infarctions, severe cardiac dysfunction, and premature death in apolipoprotein E-deficient mice. Circ. Res. 90: 270–276. [DOI] [PubMed] [Google Scholar]
- 137.Kozarsky K. F., Donahee M. H., Glick J. M., Krieger M., Rader D. J. 2000. Gene transfer and hepatic overexpression of the HDL receptor SR-BI reduces atherosclerosis in the cholesterol-fed LDL receptor-deficient mouse. Arterioscler. Thromb. Vasc. Biol. 20: 721–727. [DOI] [PubMed] [Google Scholar]
- 138.Covey S. D., Krieger M., Wang W., Penman M., Trigatti B. L. 2003. Scavenger receptor class B type I-mediated protection against atherosclerosis in LDL receptor-negative mice involves its expression in bone marrow-derived cells. Arterioscler. Thromb. Vasc. Biol. 23: 1589–1594. [DOI] [PubMed] [Google Scholar]
- 139.van Eck M., Bos I. S., Hildebrand R. B., Van Rij B. T., van Berkel T. J. 2004. Dual role for scavenger receptor class B, type I on bone marrow-derived cells in atherosclerotic lesion development. Am. J. Pathol. 165: 785–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.McCoy M. G., Sun G. S., Marchadier D., Maugeais C., Glick J. M., Rader D. J. 2002. Characterization of the lipolytic activity of endothelial lipase. J. Lipid Res. 43: 921–929. [PubMed] [Google Scholar]
- 141.Ehnholm C., Shaw W., Greten H., Brown W. V. 1975. Purification from human plasma of a heparin-released lipase with activity against triglyceride and phospholipids. J. Biol. Chem. 250: 6756–6761. [PubMed] [Google Scholar]
- 142.Busch S. J., Barnhart R. L., Martin G. A., Fitzgerald M. C., Yates M. T., Mao S. J., Thomas C. E., Jackson R. L. 1994. Human hepatic triglyceride lipase expression reduces high density lipoprotein and aortic cholesterol in cholesterol-fed transgenic mice. J. Biol. Chem. 269: 16376–16382. [PubMed] [Google Scholar]
- 143.Dichek H. L., Qian K., Agrawal N. 2004. Divergent effects of the catalytic and bridging functions of hepatic lipase on atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 24: 1696–1702. [DOI] [PubMed] [Google Scholar]
- 144.Freeman L., Amar M. J., Shamburek R., Paigen B., Brewer H. B., Jr., Santamarina-Fojo S., Gonzalez-Navarro H. 2007. Lipolytic and ligand-binding functions of hepatic lipase protect against atherosclerosis in LDL receptor-deficient mice. J. Lipid Res. 48: 104–113. [DOI] [PubMed] [Google Scholar]
- 145.Gonzalez-Navarro H., Nong Z., Amar M. J., Shamburek R. D., Najib-Fruchart J., Paigen B. J., Brewer H. B., Jr., Santamarina-Fojo S. 2004. The ligand-binding function of hepatic lipase modulates the development of atherosclerosis in transgenic mice. J. Biol. Chem. 279: 45312–45321. [DOI] [PubMed] [Google Scholar]
- 146.Mezdour H., Jones R., Dengremont C., Castro G., Maeda N. 1997. Hepatic lipase deficiency increases plasma cholesterol but reduces susceptibility to atherosclerosis in apolipoprotein E-deficient mice. J. Biol. Chem. 272: 13570–13575. [DOI] [PubMed] [Google Scholar]
- 147.Barcat D., Amadio A., Palos-Pinto A., Daret D., Benlian P., Darmon M., Berard A. M. 2006. Combined hyperlipidemia/hyperalphalipoproteinemia associated with premature spontaneous atherosclerosis in mice lacking hepatic lipase and low density lipoprotein receptor. Atherosclerosis. 188: 347–355. [DOI] [PubMed] [Google Scholar]
- 148.Ishida T., Choi S. Y., Kundu R. K., Spin J., Yamashita T., Hirata K., Kojima Y., Yokoyama M., Cooper A. D., Quertermous T. 2004. Endothelial lipase modulates susceptibility to atherosclerosis in apolipoprotein-E-deficient mice. J. Biol. Chem. 279: 45085–45092. [DOI] [PubMed] [Google Scholar]
- 149.Ko K. W., Paul A., Ma K., Li L., Chan L. 2005. Endothelial lipase modulates HDL but has no effect on atherosclerosis development in apoE−/− and LDLR−/− mice. J. Lipid Res. 46: 2586–2594. [DOI] [PubMed] [Google Scholar]
- 150.Tall A. R., Costet P., Wang N. 2002. Regulation and mechanisms of macrophage cholesterol efflux. J. Clin. Invest. 110: 899–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Schuster G. U., Parini P., Wang L., Alberti S., Steffensen K. R., Hansson G. K., Angelin B., Gustafsson J. A. 2002. Accumulation of foam cells in liver X receptor-deficient mice. Circulation. 106: 1147–1153. [DOI] [PubMed] [Google Scholar]
- 152.Joseph S. B., McKilligin E., Pei L., Watson M. A., Collins A. R., Laffitte B. A., Chen M., Noh G., Goodman J., Hagger G. N., et al. 2002. Synthetic LXR ligand inhibits the development of atherosclerosis in mice. Proc. Natl. Acad. Sci. USA. 99: 7604–7609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Levin N., Bischoff E. D., Daige C. L., Thomas D., Vu C. T., Heyman R. A., Tangirala R. K., Schulman I. G. 2005. Macrophage liver X receptor is required for antiatherogenic activity of LXR agonists. Arterioscler. Thromb. Vasc. Biol. 25: 135–142. [DOI] [PubMed] [Google Scholar]
- 154.Tangirala R. K., Bischoff E. D., Joseph S. B., Wagner B. L., Walczak R., Laffitte B. A., Daige C. L., Thomas D., Heyman R. A., Mangelsdorf D. J., et al. 2002. Identification of macrophage liver X receptors as inhibitors of atherosclerosis. Proc. Natl. Acad. Sci. USA. 99: 11896–11901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Schultz J. R., Tu H., Luk A., Repa J. J., Medina J. C., Li L., Schwendner S., Wang S., Thoolen M., Mangelsdorf D. J., et al. 2000. Role of LXRs in control of lipogenesis. Genes Dev. 14: 2831–2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Grefhorst A., Elzinga B. M., Voshol P. J., Plosch T., Kok T., Bloks V. W., van der Sluijs F. H., Havekes L. M., Romijn J. A., Verkade H. J., et al. 2002. Stimulation of lipogenesis by pharmacological activation of the liver X receptor leads to production of large, triglyceride-rich very low density lipoprotein particles. J. Biol. Chem. 277: 34182–34190. [DOI] [PubMed] [Google Scholar]
- 157.Davies J., Kotokorpi P., Lindahl U., Oscarsson J., Wells T., Mode A. 2008. Effects of the synthetic liver X receptor agonist T0901317 on the growth hormone and thyroid hormone axes in male rats. Endocrine. 33: 196–204. [DOI] [PubMed] [Google Scholar]
- 158.Schaefer E. J., Zech L. A., Schwartz D. E., Brewer H. B., Jr. 1980. Coronary heart disease prevalence and other clinical features in familial high-density lipoprotein deficiency (Tangier disease). Ann. Intern. Med. 93: 261–266. [DOI] [PubMed] [Google Scholar]
- 159.Clee S. M., Kastelein J. J., van Dam M., Marcil M., Roomp K., Zwarts K. Y., Collins J. A., Roelants R., Tamasawa N., Stulc T., et al. 2000. Age and residual cholesterol efflux affect HDL cholesterol levels and coronary artery disease in ABCA1 heterozygotes. J. Clin. Invest. 106: 1263–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hovingh G. K., Hutten B. A., Holleboom A. G., Petersen W., Rol P., Stalenhoef A., Zwinderman A. H., de Groot E., Kastelein M. D. J. J. P., Kuivenhoven J. A. 2005. Compromised LCAT function is associated with increased atherosclerosis. Circulation. 112: 879–884. [DOI] [PubMed] [Google Scholar]
- 161.Hovingh G. K., Brownlie A., Bisoendial R. J., Dube M. P., Levels J. H., Petersen W., Dullaart R. P., Stroes E. S., Zwinderman A. H., de Groot E., et al. 2004. A novel apoA-I mutation (L178P) leads to endothelial dysfunction, increased arterial wall thickness, and premature coronary artery disease. J. Am. Coll. Cardiol. 44: 1429–1435. [DOI] [PubMed] [Google Scholar]
- 162.Karathanasis S. K., Norum R. A., Zannis V. I., Breslow J. L. 1983. An inherited polymorphism in the human apolipoprotein A-I gene locus related to the development of atherosclerosis. Nature. 301: 718–720. [DOI] [PubMed] [Google Scholar]
- 163.Miller M., Rhyne J., Hong S. H., Friel G., Dolinar C., Riley W. 2007. Do mutations causing low HDL-C promote increased carotid intima-media thickness? Clin. Chim. Acta. 377: 273–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hong S. H., Riley W., Rhyne J., Friel G., Miller M. 2002. Lack of association between increased carotid intima-media thickening and decreased HDL-cholesterol in a family with a novel ABCA1 variant, G2265T. Clin. Chem. 48: 2066–2070. [PubMed] [Google Scholar]
- 165.Chiesa G., Sirtori C. R. 2003. Apolipoprotein A-I(Milano): current perspectives. Curr. Opin. Lipidol. 14: 159–163. [DOI] [PubMed] [Google Scholar]
- 166.Weibel G. L., Alexander E. T., Joshi M. R., Rader D. J., Lund-Katz S., Phillips M. C., Rothblat G. H. 2007. Wild-type apoA-I and the Milano variant have similar abilities to stimulate cellular lipid mobilization and efflux. Arterioscler. Thromb. Vasc. Biol. 27: 2022–2029. [DOI] [PubMed] [Google Scholar]
- 167.Sirtori C. R., Mombelli G. 2008. Viability of developing CETP inhibitors. Cardiovasc. Ther. 26: 135–146. [DOI] [PubMed] [Google Scholar]
- 168.Klos K. L., Kullo I. J. 2007. Genetic determinants of HDL: monogenic disorders and contributions to variation. Curr. Opin. Cardiol. 22: 344–351. [DOI] [PubMed] [Google Scholar]
- 169.Edmondson A. C., Brown R. J., Kathiresan S., Cupples L. A., Demissie S., Manning A. K., Jensen M. K., Rimm E. B., Wang J., Rodrigues A., et al. 2009. Loss-of-function variants in endothelial lipase are a cause of elevated HDL cholesterol in humans. J. Clin. Invest. 119: 1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Davey Smith, G., Ebrahim S. 2003. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int. J. Epidemiol. 32: 1–22. [DOI] [PubMed] [Google Scholar]
- 171.Frikke-Schmidt R., Nordestgaard B. G., Stene M. C., Sethi A. A., Remaley A. T., Schnohr P., Grande P., Tybjaerg-Hansen A. 2008. Association of loss-of-function mutations in the ABCA1 gene with high-density lipoprotein cholesterol levels and risk of ischemic heart disease. JAMA. 299: 2524–2532. [DOI] [PubMed] [Google Scholar]
- 172.Johannsen T. H., Kamstrup P. R., Andersen R. V., Jensen G. B., Sillesen H., Tybjaerg-Hansen A., Nordestgaard B. G. 2009. Hepatic lipase, genetically elevated high-density lipoprotein, and risk of ischemic cardiovascular disease. J. Clin. Endocrinol. Metab. 94: 1264–1273. [DOI] [PubMed] [Google Scholar]
- 173.Thompson A., Di Angelantonio E., Sarwar N., Erqou S., Saleheen D., Dullaart R. P. F., Keavney B., Ye Z., Danesh J. 2008. Association of cholesteryl ester transfer protein genotypes with CETP mass and activity, lipid levels, and coronary risk. JAMA. 299: 2777–2788. [DOI] [PubMed] [Google Scholar]
- 174.Willer C. J., Sanna S., Jackson A. U., Scuteri A., Bonnycastle L. L., Clarke R., Heath S. C., Timpson N. J., Najjar S. S., Stringham H. M., et al. 2008. Newly identified loci that influence lipid concentrations and risk of coronary artery disease. Nat. Genet. 40: 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kathiresan S., Melander O., Anevski D., Guiducci C., Burtt N. P., Roos C., Hirschhorn J. N., Berglund G., Hedblad B., Groop L., et al. 2008. Polymorphisms associated with cholesterol and risk of cardiovascular events. N. Engl. J. Med. 358: 1240–1249. [DOI] [PubMed] [Google Scholar]
- 176.Staels B., Dallongeville J., Auwerx J., Schoonjans K., Leitersdorf E., Fruchart J. C. 1998. Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation. 98: 2088–2093. [DOI] [PubMed] [Google Scholar]
- 177.Birjmohun R. S., Hutten B. A., Kastelein J. J. P., Stroes E. S. G. 2005. Efficacy and safety of high-density lipoprotein cholesterol-increasing compounds: A meta-analysis of randomized controlled trials. J. Am. Coll. Cardiol. 45: 185–197. [DOI] [PubMed] [Google Scholar]
- 178.Robins S. J., Collins D., Wittes J. T., Papademetriou V., Deedwania P. C., Schaefer E. J., McNamara J. R., Kashyap M. L., Hershman J. M., Wexler L. F., et al. , for the VA-HIT Study Group. 2001. Relation of gemfibrozil treatment and lipid levels with major coronary events: VA-HIT: a randomized controlled trial. JAMA. 285: 1585–1591. [DOI] [PubMed] [Google Scholar]
- 179.Saha S. A., Kizhakepunnur L. G., Bahekar A., Arora R. R. 2007. The role of fibrates in the prevention of cardiovascular disease–a pooled meta-analysis of long-term randomized placebo-controlled clinical trials. Am. Heart J. 154: 943–953. [DOI] [PubMed] [Google Scholar]
- 180.Kamanna V. S., Vo A., Kashyap M. L. 2008. Nicotinic acid: recent developments. Curr. Opin. Cardiol. 23: 393–398. [DOI] [PubMed] [Google Scholar]
- 181.van der Hoorn J. W., de Haan W., Berbee J. F., Havekes L. M., Jukema J. W., Rensen P. C., Princen H. M. 2008. Niacin increases HDL by reducing hepatic expression and plasma levels of cholesteryl ester transfer protein in APOE*3Leiden.CETP mice. Arterioscler. Thromb. Vasc. Biol. 28: 2016–2022. [DOI] [PubMed] [Google Scholar]
- 182.Brown B. G., Zhao X. Q., Chait A., Fisher L. D., Cheung M. C., Morse J. S., Dowdy A. A., Marino E. K., Bolson E. L., Alaupovic P., et al. 2001. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N. Engl. J. Med. 345: 1583–1592. [DOI] [PubMed] [Google Scholar]
- 183.Taylor A. J., Sullenberger L. E., Lee H. J., Lee J. K., Grace K. A. 2004. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation. 110: 3512–3517. [DOI] [PubMed] [Google Scholar]
- 184.Taylor A. J., Lee H. J., Sullenberger L. E. 2006. The effect of 24 months of combination statin and extended-release niacin on carotid intima-media thickness: ARBITER 3. Curr. Med. Res. Opin. 22: 2243–2250. [DOI] [PubMed] [Google Scholar]
- 185.Taylor A. J., Villines T. C., Stanek E. J., Devine P. J., Griffen L., Miller M., Weissman N. J., Turco M. 2009. Extended-release niacin or ezetimibe and carotid intima-media thickness. N. Engl. J. Med. 361: 2113–2122. [DOI] [PubMed] [Google Scholar]
- 186.Lee J. M. S., Robson M. D., Yu L. M., Shirodaria C. C., Cunnington C., Kylintireas I., Digby J. E., Bannister T., Handa A., Wiesmann F., et al. 2009. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: a randomized, placebo-controlled, magnetic resonance imaging study. J. Am. Coll. Cardiol. 54: 1787–1794. [DOI] [PubMed] [Google Scholar]
- 187.Nissen S. E., Tsunoda T., Tuzcu E. M., Schoenhagen P., Cooper C. J., Yasin M., Eaton G. M., Lauer M. A., Sheldon W. S., Grines C. L., et al. 2003. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 290: 2292–2300. [DOI] [PubMed] [Google Scholar]
- 188.Rader D. J. 2003. High-density lipoproteins as an emerging therapeutic target for atherosclerosis. JAMA. 290: 2322–2324. [DOI] [PubMed] [Google Scholar]
- 189.Tardif J. C., Gregoire J., L'Allier P. L., Ibrahim R., Lesperance J., Heinonen T. M., Kouz S., Berry C., Basser R., Lavoie M. A., et al. 2007. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 297: 1675–1682. [DOI] [PubMed] [Google Scholar]
- 190.Tall A. R. 2007. CETP inhibitors to increase HDL cholesterol levels. N. Engl. J. Med. 356: 1364–1366. [DOI] [PubMed] [Google Scholar]
- 191.de Grooth G. J., Kuivenhoven J. A., Stalenhoef A. F., de Graaf J., Zwinderman A. H., Posma J. L., van Tol A., Kastelein J. J. 2002. Efficacy and safety of a novel cholesteryl ester transfer protein inhibitor, JTT-705, in humans: a randomized phase II dose-response study. Circulation. 105: 2159–2165. [DOI] [PubMed] [Google Scholar]
- 192.Brousseau M. E., Schaefer E. J., Wolfe M. L., Bloedon L. T., Digenio A. G., Clark R. W., Mancuso J. P., Rader D. J. 2004. Effects of an inhibitor of cholesteryl ester transfer protein on HDL cholesterol. N. Engl. J. Med. 350: 1505–1515. [DOI] [PubMed] [Google Scholar]
- 193.Krishna R., Anderson M. S., Bergman A. J., Jin B., Fallon M., Cote J., Rosko K., Chavez-Eng C., Lutz R., Bloomfield D. M., et al. 2007. Effect of the cholesteryl ester transfer protein inhibitor, anacetrapib, on lipoproteins in patients with dyslipidaemia and on 24-h ambulatory blood pressure in healthy individuals: two double-blind, randomised placebo-controlled phase I studies. Lancet. 370: 1907–1914. [DOI] [PubMed] [Google Scholar]
- 194.Barter P. J., Caulfield M., Eriksson M., Grundy S. M., Kastelein J. J., Komajda M., Lopez-Sendon J., Mosca L., Tardif J. C., Waters D. D., et al. 2007. Effects of torcetrapib in patients at high risk for coronary events. N. Engl. J. Med. 357: 2109–2122. [DOI] [PubMed] [Google Scholar]
- 195.Bots M. L., Visseren F. L., Evans G. W., Riley W. A., Revkin J. H., Tegeler C. H., Shear C. L., Duggan W. T., Vicari R. M., Grobbee D. E., et al. 2007. Torcetrapib and carotid intima-media thickness in mixed dyslipidaemia (RADIANCE 2 study): a randomised, double-blind trial. Lancet. 370: 153–160. [DOI] [PubMed] [Google Scholar]
- 196.Kastelein J. J. P., van Leuven S. I., Burgess L., Evans G. W., Kuivenhoven J. A., Barter P. J., Revkin J. H., Grobbee D. E., Riley W. A., Shear C. L., Duggan W. T., Bots M. L., the RADIANCE investigators. 2007. Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N. Engl. J. Med. 356: 1620–1630. [DOI] [PubMed] [Google Scholar]
- 197.Nissen S. E., Tardif J. C., Nicholls S. J., Revkin J. H., Shear C. L., Duggan W. T., Ruzyllo W., Bachinsky W. B., Lasala G. P., Tuzcu E. M., The ILLUSTRATE Investigators. 2007. Effect of torcetrapib on the progression of coronary atherosclerosis. N. Engl. J. Med. 356: 1304–1316. [DOI] [PubMed] [Google Scholar]
- 198.Vergeer M., Bots M. L., van Leuven S. I., Basart D. C., Sijbrands E. J., Evans G. W., Grobbee D. E., Visseren F. L., Stalenhoef A. F., Stroes E. S., et al. 2008. Cholesteryl ester transfer protein inhibitor torcetrapib and off-target toxicity: a pooled analysis of the rating atherosclerotic disease change by imaging with a new CETP inhibitor (RADIANCE) trials. Circulation. 118: 2515–2522. [DOI] [PubMed] [Google Scholar]
- 199.Vergeer M., Stroes E. S. 2009. The pharmacology and off-target effects of some cholesterol ester transfer protein inhibitors. Am. J. Cardiol. 104: 32E–38E. [DOI] [PubMed] [Google Scholar]
- 200.Forrest M. J., Bloomfield D., Briscoe R. J., Brown P. N., Cumiskey A. M., Ehrhart J., Hershey J. C., Keller W. J., Ma X., McPherson H. E., et al. 2008. Torcetrapib-induced blood pressure elevation is independent of CETP inhibition and is accompanied by increased circulating levels of aldosterone. Br. J. Pharmacol. 154: 1465–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Navab M., Anantharamaiah G. M., Reddy S. T., Hama S., Hough G., Grijalva V. R., Yu N., Ansell B. J., Datta G., Garber D. W., et al. 2005. Apolipoprotein A-I mimetic peptides. Arterioscler. Thromb. Vasc. Biol. 25: 1325–1331. [DOI] [PubMed] [Google Scholar]
- 202.Bloedon L. T., Dunbar R., Duffy D., Pinell-Salles P., Norris R., DeGroot B. J., Movva R., Navab M., Fogelman A. M., Rader D. J. 2008. Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients. J. Lipid Res. 49: 1344–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Navab M., Anantharamaiah G. M., Reddy S. T., Van Lenten B. J., Fogelman A. M. 2008. Apo A-1 mimetic peptides as atheroprotective agents in murine models. Curr. Drug Targets. 9: 204–209. [DOI] [PubMed] [Google Scholar]
- 204.Krimbou L., Jahagirdar R., Ruel I., Johansson J., Genest J. 2007. Abstract 679: oral administration of compound RVX-208 increases serum levels of apoA-I and improves high-density lipoprotein-mediated cholesterol efflux in african green monkeys. Circulation. 116: II. [Google Scholar]
- 205.Writing Group for the Women's Health Initiative Investigators. 2002. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative Randomized Controlled Trial. JAMA. 288: 321–333. [DOI] [PubMed] [Google Scholar]
- 206.The HOPE and HOPE-TOO Trial Investigators. 2005. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA. 293: 1338–1347. [DOI] [PubMed] [Google Scholar]
- 207.The Heart Outcomes Prevention Evaluation (HOPE). 2006. Homocysteine lowering with folic acid and B vitamins in vascular disease. N. Engl. J. Med. 354: 1567–1577. [DOI] [PubMed] [Google Scholar]
- 208.Vaisar T., Pennathur S., Green P. S., Gharib S. A., Hoofnagle A. N., Cheung M. C., Byun J., Vuletic S., Kassim S., Singh P., et al. 2007. Shotgun proteomics implicates protease inhibition and complement activation in the antiinflammatory properties of HDL. J. Clin. Invest. 117: 746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]