Abstract
Background
Type 2 diabetes affects one in five African American women over the age of 60 years. These women face distinct challenges in managing diabetes self-care. Therefore, tailored self-care interventions for this population need to be developed and tested.
Objectives
The effectiveness of a tailored, four-visit, in-home symptom-focused diabetes intervention with and without booster telephone calls was compared to an attentional control focused on skills training for weight management and diet.
Methods
African American women (n = 180; > 55 years old, Type 2 diabetes mellitus > 1 year, HbA1c > 7%) were randomly assigned to the intervention or attentional control condition. Half the intervention participants were assigned to also receive a telephone-delivered booster intervention. Participants were evaluated at baseline and 3, 6, and 9 months.
Results
Baseline HbA1 was 8.3 in the intervention group (n=60), 8.29 in the intervention with booster group (n=55), and 8.44 in the attentional control condition (n=59). HbA1c declined significantly in the whole sample (0.57%) with no differences between study arms. Participants in the booster arm decreased HbA1c by 0.76%. Symptom distress, perceived quality of life, impact of diabetes, and self-care activities also improved significantly for the whole sample with no significant differences between study arms.
Discussion
Parsimonious interventions of 4 in-person visits yielded clinically significant decreases in HbA1c. Although the weight and diet program was intended as an attentional control, the positive effects suggest it met a need in this population. Since the content of both the intervention and attentional control were effective despite different approaches, a revised symptom-focused intervention that incorporates weight and diet skills training may offer even better results.
Keywords: African American, diabetes, symptoms
Over 7% of adults in the United States have been diagnosed with diabetes, and diabetes-related care now accounts for 11% of all U.S. health care expenditures (American Diabetes Association [ADA], 2005). Type 2 diabetes disproportionately affects African Americans, who are almost twice as likely to have the disease, are less likely to have good glycemic control, and have a higher incidence of diabetes complications when compared to Caucasian Americans (ADA, 2005; Saydah, Cowie, Eberhardt, De Rekeneire, & Narayan, 2007). Diabetes poses a particular burden for African American women over the age of 60 years, 20% of whom are diagnosed with diabetes (ADA, 2005). Many older African American women live in poverty, adding to their burden in managing care. Those who live in rural areas face further challenges due to the shortage of health care providers, lack of transportation, and limited community-based resources to support their self-care (Stoodt & Lengerich, 1993).
The goal of diabetes management is to improve glycemic control and thereby prevent or delay the onset of complications (ADA, 2008). The cornerstone of management is self-care, which consists of an often complex regimen of meal planning, daily foot care, regular physical activity, weight control, administration of insulin or oral medications, and self-monitoring of blood glucose. An older, African American woman's ability to implement a diabetes self-care regimen may be influenced by her functional abilities, resources, and culture. Diabetes and its acute and chronic complications can present atypically in older adults (Funnell & Merritt, 1993). Symptoms of other comorbidities also may limit their self-care. Rural, southern African Americans often have limited incomes and share cultural characteristics that may influence their diabetes self-care such as sense of duty to family and to God's will (Dilworth-Anderson, Goodwin, & Williams, 2004). Therefore, self-care management interventions are more effective when they attend to these differences (ADA, 2008; Sarkisian, Brown, Norris, Wintz, & Mangione, 2003). Yet few interventions tailored to the needs of older, rural African American women have been developed. Researchers have demonstrated the effectiveness of diabetes self-care interventions tailored for African Americans (Anderson et al., 2005; Feathers et al., 2007; Keyserling et al., 2002) and the elderly (Funnell, Arnold, Fogler, Merritt, & Anderson, 1998; Glasgow et al., 1992), but few have been focused on the distinct needs of African Americans who are also elders. Presented in this report is a test of the effectiveness of a symptom-focused approach to diabetes self-care tailored for older African American women as compared to a more traditional skills-based approach. Also assessed is the effect of a telephone booster follow-up for the symptom-focused approach.
A Symptom-Focused Approach to Diabetes Self-care Management
The conceptual model for the symptom-focused intervention is based on the University of California at San Francisco Symptom Management Model (Dodd, Miaskowski, & Paul, 2001; The University of California, San Francisco Symptom Management Group, 1994). The development of the conceptual model and how it was used to guide the design of the study and tailor the intervention is described in detail elsewhere (Skelly, Leeman, Carlson, Soward, & Burns, 2008). Symptom-focused interventions have demonstrated effectiveness at reducing symptom distress and improving health behaviors for a broad range of conditions (Given et al., 2004; Wassem & Dudley, 2003; Zimmerman et al., 2007). People with diabetes experience symptoms acutely and chronically throughout the course of their disease (Stover, Skelly, Holditch-Davis, & Dunn, 2001). While symptoms can provide individuals a way of understanding their illness and become a signal to implement appropriate diabetes self-care, individuals often do not recognize the relationships between their symptoms and disease. A central goal of a symptom-focused approach is to help individuals recognize and interpret symptoms so they can make appropriate decisions about self-care (Teel, Meek, McNamara, & Watson, 1997). A symptom-focused approach has the advantage of individualizing self-management education to the distinct experience of each individual.
The intervention was tailored for older African American women with diabetes residing in rural areas of the southeast based on findings from a series of pilot studies that detailed key symptoms, how symptoms affected these women's lives, and the strategies they used to manage symptoms and implement self-care. Although women presented with multiple diabetes-related symptoms, they often failed to recognize the relationship between diabetes and their symptoms. Many experienced their health and functioning as poor, and had comorbidities with the potential to interfere with their self-care (Stover et al., 2001). Women reported that spirituality and going to church were central means of coping and sources of emotional support. They also reported multiple caregiving responsibilities, which could serve as both barrier and facilitator to self-care. Women also reported high levels of life stress (Samuel-Hodge et al., 2000). During focus groups, women often used oral story telling as a means of sharing information.
Based on the findings of these studies, the intervention was tailored to include strategies to manage stress and, as appropriate, to incorporate the women's own coping strategies such as spirituality and the importance of family. The delivery format was tailored further to allow time for women to tell their stories about living with diabetes. A Community Advisory Board composed of 6 African American women residing in communities similar to the study population guided the development of study materials and advised about recruitment. The members of the board provided extensive feedback on study materials, and numerous changes were made based on their input. For example, they recommended placing “clogged arteries” in parentheses after the term “arteriosclerosis” and using a font size that would be readable without looking like it was designed for young children. The process used to tailor the intervention is described in detail elsewhere (Leeman, Skelly, Burns, Carlson, & Soward, 2008).
Objectives
To test the effectiveness of the symptom-focused diabetes intervention, it was compared to an attentional control focused on weight management and diet skills training in older African American women with type 2 diabetes, residing in the rural southeast. The intervention's effects on metabolic control (HBA1c level), symptom distress, perceived quality of life, and self-care practices were evaluated in comparison to the attentional control. Also evaluated was the impact of a booster intervention on sustaining the effects of the symptom-focused intervention.
Methods
A randomized, controlled three-group experimental design with two-thirds of subjects randomly assigned to the intervention and one-third to the attentional control (weight and diet) program was used. At the end of the intervention, half of the symptom-focused intervention participants were randomly assigned to receive the telephone booster.
Sample
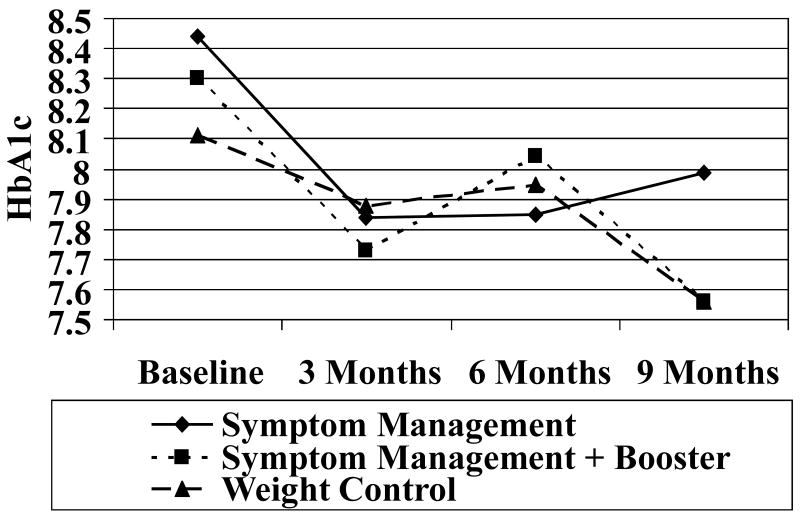
The sample consisted of 180 African American women recruited from health care centers, health department clinics, and primary care practices serving the target population in 5 rural counties in the southeast with high percentages of African Americans with diabetes living below the poverty line. Counties are classified as rural if they are outside the boundaries of a metropolitan area and include no cities with as many as 50,000 or more residents (Coward & Krout, 1998). The inclusion criteria for the study were female gender, age 50 years and older, African American ethnicity as defined by the participant, type 2 diabetes for greater than 1 year, and HbA1C greater than 7% (HbA1C less than 7% is the current standard established by the American Diabetes Association for acceptable glycemic control; ADA, 2008). Participants were required to have access to a telephone and be English-speaking. Of the 308 women screened, 180 (58%) met the inclusion criteria and were enrolled. The primary reason women were deemed ineligible was HbA1c levels below the 7% level required for inclusion (Figure 1). Participants were blocked by HbA1c (<10, >10), comorbidities (1, >1), and a factor to produce even accrual in the study arms over time. Study arm assignments were kept in sealed, opaque envelopes that were opened using a verifiable system, which assured that participants received assignment in the order in which they were enrolled.
Figure 1. Participants Enrolled.
Symptom-Focused Intervention
The symptom-focused intervention involved teaching and counseling modules delivered by a nurse in the participant's home over a series of four 60-minute bimonthly visits. The home was chosen as the delivery site to overcome rural African Americans' transportation-related barriers to care and also to allow the nurse to individualize teaching to the resources in each woman's home and community. For example, nurses went into women's kitchens to teach about reading nutrition labels the woman had on hand. Family members, if present, were invited to sit in during the intervention sessions, with the participant's approval. The intervention was guided by four modules addressing Symptoms of Hyperglycemia, Symptoms of Hypoglycemia, Numbness and Tingling in the Feet/Foot Pain, and Prevention of Cardiovascular Symptoms. These modules were based on symptom clusters identified in previous research (Stover et al., 2001). Each module was composed of (a) a brief overview of the symptom, (b) assessment parameters, (c) goals for the intervention, (d) symptom management strategies, and (e) materials on the prevention of symptoms. The nurse individualized the intervention by allowing participants to choose in which order to address symptoms and what management strategies to use. This approach covered not only the symptoms participants were experiencing but also other symptoms of diabetes they may encounter.
Telephone Booster
Three months after completion of the intervention, participants in the booster arm received four telephone calls at approximately 2-3 week intervals with the spacing of the calls covering a 12-week interval similar to that of the intervention. Calls averaged 15 minutes each. To build on the therapeutic relationship formed during home visits, the calls were made by the same intervention nurse that made the home visits, using an established protocol. The purpose of the telephone booster was to reinforce the strategies developed during home visits, engage in problem-solving, provide motivation and encouragement, and encourage reframing and adjustment as needed.
Attentional Control Condition
The attentional control was a weight and diet program consisting of four modules delivered in 60 minute sessions that addressed Weight Maintenance (two modules), Modifying Fat, and Modifying Sodium in the diet. The modules did not address symptoms directly. The program was designed to focus on diet with the expectation that it would be ineffective, as many individuals with diabetes have listened to advice to watch their weight for years without making the necessary changes in their behavior. The program took a skills-based, how-to approach with modules teaching skill-based strategies to enhance diabetes self-care (such as reading labels). The skills taught included counting carbohydrates, reading labels, determining portion sizes, finding healthy types of fat, and reducing saturated fat in the diet. Important components of the learning modules were practice exercises, shopping lists, and recipes. The modules also were individualized, allowing participants to choose which content areas to address and what management strategies to use.
Measurement
The effects of the intervention and attentional control on health and quality of life outcomes (metabolic control, symptom distress, perceived quality of life, and self-care practices) were assessed.
Metabolic control
Was assessed using HbA1c, a measure of the participant's weighted average blood glucose level over the preceding 2-3 months (Lebovitz, 1998). Microcapillary samples were obtained in the home using the Accubase A1c Test Kit (FDA approved; K983172; MDE#903510) and submitted for analysis to Diabetes Technologies, Inc.
Symptom distress
Was measured using the Diabetes Symptom Distress Scale (Cronbach's alpha = .86), a 20-item instrument developed by the investigators to measure the presence of 20 diabetes-related symptoms and the amount of distress caused by these symptoms (Skelly, Carlson, Leeman, Holditch-Davis, & Soward, 2005). The distress score correlates well with the severity and difficulty of management scores (.92 and .88, both p<.01). In a previous study, the scale had Cronbach's alpha of .90 for the severity scale, .86 for the distress scale and .84 for the symptom management scale (Skelly et al., 2005).
Quality of life was measured using two diabetes-specific measures. Diabetes-related Quality of Life was measured with the Quality of Life in Diabetes Scale. This scale is used to measure diabetes-related quality of life and was developed for use with older, rural African Americans. It is focused on the effects of diabetes self-care regimens, symptoms, and complications on an individual's mental and social well-being (Elasy et al., 2000). This 27-item instrument has two subscales measuring quality of life in two domains: mental well-being and social well-being; scores range between 1 and 4, where 4 is the highest quality of life. The scale's Cronbach's alphas are .83 and .93 respectively for the mental and social well-being subscales (Elasy et al., 2000). The instrument also has received extensive validation from focus groups and in structured interviews with African American women (Elasy et al., 2000). Other aspects of quality of life were measured using the Problem Areas in Diabetes survey (PAID; Polonsky et al., 1995, 2005). The PAID has high internal reliability with a Cronbach's alpha of .95. Concurrent validity was established by significant correlations between the PAID and diabetes-coping strategies (Welch, Jacobson, & Polonsky, 1997). The PAID is a 20-item instrument in which each item represents an area of diabetes-related psychosocial distress such as worry, frustration, anger, interpersonal distress, and coping concerns. It is scored on a scale of 0-100; higher scores indicate greater problems.
Diabetes self-care practices were measured using the Diabetes Self-Care Practices questionnaire, which has a Cronbach's alpha of .88 and test-retest reliability, measured at a 2-week interval of 95% (Skelly, Marshall, Haughey, Davis, & Dunford, 1995). This questionnaire is a self-report of daily diabetes-related self-care practices in five regimen areas: diet, medications/insulin, home glucose monitoring, physical activity/exercise, and foot care. This instrument was developed for use with African American women with type 2 diabetes mellitus and has been used effectively in prior research (Skelly et al., 2005). Performance is rated by the percent of time the practice was performed: 0% (not at all), 25%, 50%, 75%, or 100% of the time. To improve the stability of the analysis, the responses were grouped into compliant (100% and 75%) and noncompliant (50%, 25%, and 0%).
All instruments were reviewed by members of the investigative team and Community Advisory Board for cultural relevance and acceptability and pilot-tested with African American participants to assess readability and ease of administration (Skelly et al., 2005). All measures were at a 4th-6th grade reading level, wording was changed as needed, and measures were read to participants rather than self-administered.
Intervention Procedures
Approval was obtained from the Institutional Review Board at The University of North Carolina at Chapel Hill. After meeting the inclusion criteria and providing informed consent, participants completed the baseline study questionnaires during two initial visits and were then randomized to the test or attentional control arm. This was followed at 2-week intervals by four home visits delivered by a registered nurse during which participants received either the symptom-focused intervention or weight and diet attentional control program. Visits in the home lasted about 60 minutes (M = 63.5, SD = 12.02). Data collection visits conducted by a research assistant, who was blind to the study arm assignment, were made at baseline, 3 months (2 weeks after the last intervention visit), 6 months, and 9 months. A booster telephone intervention consisting of 4 15-minute monthly telephone calls was provided between months 6 and 9 to symptom-focused participants chosen randomly at month 6. The same nurse who had conducted the home intervention delivered this intervention.
Data Analysis
To preserve the integrity of the trial, each participant was analyzed in the study arm to which they were randomized, regardless of degree of adherence or whether they were observed at all of the data collection times. For HbA1c, Diabetes Symptom Distress, Diabetes Related Quality of Life, and Problem Areas in Diabetes, the effect of the symptom-focused intervention was compared to that of the weight and diet attentional control using linear mixed models. The immediate effects of treatment were assessed by comparing changes from baseline to 3 months between the intervention participants and the weight and diet participants where the symptom-focused and symptom-focused plus booster participants were one group (booster treatments were not delivered until 6 months). Changes from baseline to 9 months were compared between symptom-focused and weight and diet, and symptom-focused plus booster and weight and diet participants with the alpha level adjusted to .025. The effect of the booster was evaluated in a separate analysis comparing the change from 6 months to 9 months between the symptom intervention booster and nonbooster arms. Tests were one-sided since the hypotheses about the effects of the SF and SF/B interventions were directional.
For each outcome, the appropriate covariance structure was identified by examination of the observed autocorrelations and by comparing values of Akaike's Information Criteria (Akaike, 1974) that resulted from specifying different structures. To allow for variations in the actual times between observations, time was represented by the number of days elapsed from the baseline measurement. Quadratic and cubic terms for time were included in initial models to represent possible nonlinear effects and were dropped from subsequent models if they were nonsignificant.
For self-care practices, generalized estimating equations were used to estimate models similar to those for the health outcomes but with time represented by the data collection point (1 for the baseline measurement to 4 for the 9-month measure).
Results
The typical study participant was 67 years old, widowed, residing in her own home, with a history of diabetes for 12 years, a HbA1c of 8.3%, and less than a high school education. Her total family income was less than $15,000 per year. She was taking 8.4 prescribed medications daily and received Medicare. This typical participant presented with an average of 8.2 symptoms (SD = 4.1) related to diabetes and previously had received diabetes education primarily from her healthcare provider via printed materials. As detailed in Table 1, baseline values of patient characteristics and outcomes were equivalent across the three treatment groups with the exception of educational level and the PAIDS score.
Table 1. Baseline Patient Characteristics by Study Group.
| All | Symptom Intervention with Booster (a) |
Symptom Intervention (b) |
Weight Management and Diet (c) |
Comparisons | |
|---|---|---|---|---|---|
| Age | ns | ||||
| n | 174 | 55 | 60 | 59 | |
| Median | 67.0 | 65.0 | 68.5 | 68.0 | |
| Age at diagnosis | ns | ||||
| n | 166 | 52 | 59 | 55 | |
| Median | 54 | 54 | 54 | 55 | |
| Years with diagnosis | ns | ||||
| n | 168 | 51 | 60 | 57 | |
| M | 12 | 12 | 15 | 12 | |
| SD | 6.21 | 6.17 | 7.25 | 5.23 | |
| HbA1C | q | ns | |||
| n | 180 | 59 | 61 | 60 | |
| M | 8.29 | 8.30 | 8.44 | 8.11 | |
| SD | 1.62 | 1.64 | 1.63 | 1.61 | |
| Complications | ns | ||||
| n | 175 | 56 | 60 | 59 | |
| Median | 4.0 | 4.0 | 4.0 | 4.0 | |
| Symptoms | ns | ||||
| n | 172 | 55 | 59 | 58 | |
| M | 8.10 | 7.82 | 7.98 | 8.50 | |
| SD | 4.09 | 4.30 | 3.65 | 4.35 | |
| Diabetes medication | ns | ||||
| n | 174 | 55 | 60 | 59 | |
| % None | 2 | 4 | 2 | 0 | |
| % Oral | 44 | 45 | 42 | 46 | |
| % Insulin | 18 | 18 | 17 | 17 | |
| % Both | 36 | 33 | 40 | 36 | |
| Income | ns | ||||
| n | 170 | 53 | 59 | 58 | |
| Median category | < $10,000 | $10,000-14,000 | < $10,000 | $10,000-14,000 | |
| Education | (b)&(c) < (a) | ||||
| n | 172 | 53 | 60 | 59 | |
| % < high school | 51 | 36 | 60 | 56 | |
| % high school | 22 | 26 | 22 | 19 | |
| % > high school | 27 | 38 | 18 | 25 | |
| Mental quality of life | ns | ||||
| n | 172 | 55 | 59 | 58 | |
| M | 2.55 | 2.67 | 2.43 | 2.56 | |
| SD | 0.69 | 0.60 | 0.70 | 0.77 | |
| Social quality of life | ns | ||||
| n | 171 | 55 | 59 | 57 | |
| M | 3.25 | 3.41 | 3.19 | 3.17 | |
| SD | 0.66 | 0.57 | 0.67 | 0.71 | |
| PAID | (c) > (a) | ||||
| n | 165 | 51 | 56 | 58 | |
| M | 2.28 | 2.05 | 2.31 | 2.44 | |
| SD | 0.83 | 0.56 | 0.75 | 1.05 |
Notes. PAID = Problem Areas in Diabetes survey
Retention
The overall retention rate at 9 months was 90.6%. Retention rates for the four evaluation visits were 97% for time 1, 96% for time 2, 93% for time 3, and 91% for time 4. Seventeen women did not complete all four evaluation points. The reasons for attrition were death (n = 7), depressed or ill (n = 1), move out of state (n = 1), lost to follow-up (n = 7), and procedural error (n = 1). The likelihood of completing the study was not related to initial treatment assignment: 90.8% of the symptom-focused and symptom-focused plus booster participants completed the study compared to 88.3% of the weight and diet participants, chi-square (1) = 0.51, p = .47. Completion of the study also was not related to the primary physiological outcome, glycemic control. Mean and standard deviation of HbA1c levels at enrollment were 7.97% (1.57%) for those who did not complete the study versus 8.32% (1.63%) for those who did finish, F (1,178) = 0.70, p = .40.
Metabolic Control, Symptom Distress and Perceptions of Quality of Life
Metabolic control
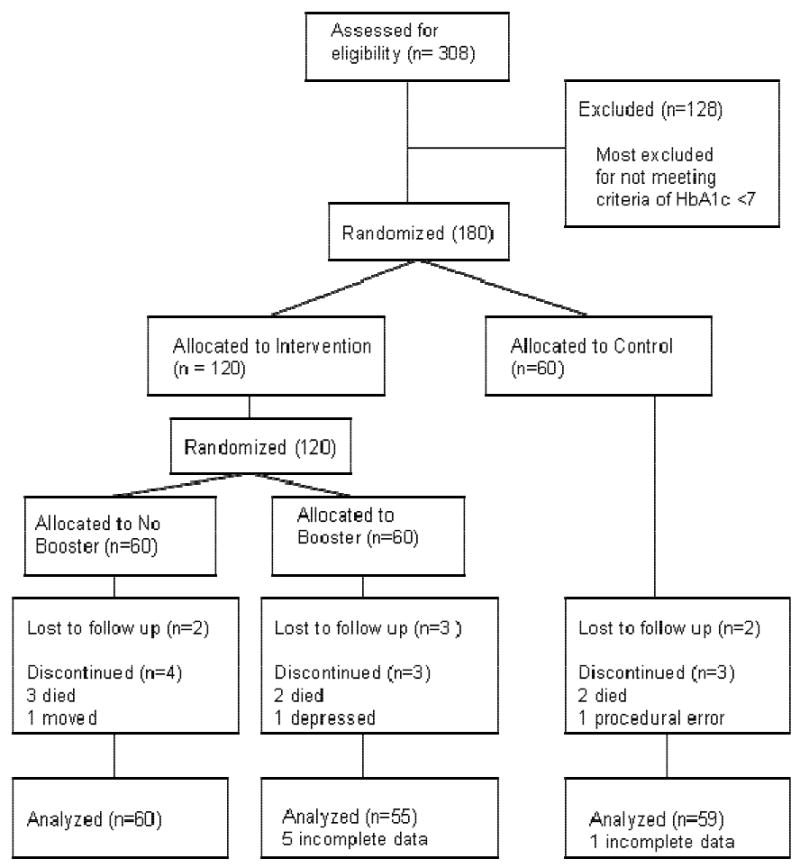
The mean HbA1c was 8.3% (SD = 1.6%) at baseline. As seen in Figure 2, over the 9-month study period, there was a significant decline in HbA1c from baseline for the entire sample (p = .01), but there were no significant differences in the amount of decline between the study arms. During the intervention period between baseline and 3 months, the decline was greater for the combined symptom-focused and symptom-focused plus booster participants than for weight and diet participants (p = .04). The symptom-focused plus booster participants improved significantly compared to symptom-focused participants during the period of booster follow-up (from 6 to 9 months, p = .04). Participants receiving the booster decreased their HbA1c by .76% over the 9 months of the study.
Figure 2. Mean HbA1c at Each Data Collection Point, by Treatment.
Symptom distress
Symptom distress declined throughout the study period for all treatment groups, more sharply for symptom-focused plus booster and weight and diet than for symptom-focused participants. On average participants across treatment groups reported a significant decrease in symptom distress at 9 months as compared to baseline (p < .01), but the hypothesized differences in decline between the treatment groups were not seen. The distress score correlated well with other diabetes specific measures: r = 0.62 (p < .01) with PAID, and r = 0.51 (p < .01) with the mental well-being score and r = 0.53 (p < .01) with the social well-being score of Diabetes-related Quality of Life. The distress score changed consistently with changes in HbA1c over 9 months (p = .02), demonstrating its ability to measure changes due to treatment.
Diabetes-related Quality of Life scale
There was a significant increase in the mean scores for mental and social well-being for the entire sample over the study period (p < .01 for each score), but there was no difference between study arms in the amount of increase. A Cronbach's alpha of 0.83 was reported for the mental well-being scale and 0.93 for the social well-being scale.
Problem Areas in Diabetes Survey
Over the study period, the decrease in the PAID score in the total sample was significant (p < .01), but no differences were observed between the treatment groups. Participants in the booster arm showed greater improvement than participants in the other symptoms management arm during the 6 to 9 month period, demonstrating a significant effect for the booster (p = .04).
Diabetes Self-Care Practices
Also examined were participants' self-care practices using the Diabetes Self-Care Practices questionnaire (Skelly et al., 1995, 2005). Based on previous research, each of the diabetes regimen areas was considered separately (diet, exercise, insulin/oral medication, home glucose monitoring, and foot care). Treatment assignment had no significant effect on changes in adherence for any of the self-care practices. The total sample improved in their self-care in regard to diet, oral medications, and foot care over the course of the study (p < .01 for each outcome). There were no significant changes over time in regard to physical activity, insulin use, or home glucose monitoring. The self-care practices that improved over the course of the study did not mediate the effects of the study on HbA1c, diabetes-related quality of life, or symptom distress. However, compliance with diet was correlated positively with the mental well-being scale of the Diabetes-related Quality of Life instrument.
Discussion
Effects on Health Outcomes
Over the 9 months of the study, self-care practices, metabolic control, symptom distress, and quality of life improved for the entire sample. The average drop in HbA1c for the entire sample was .57%, and the maximum drop was in the symptom management participants that received the telephone booster. Their HbA1c decreased by .76%. In the United Kingdom Prospective Diabetes Study (UKPDS; 1998) a decrease of 1% was found in HbA1c in patients with type 2 diabetes mellitus, which resulted in a 35% reduction in risk for microvascular disease. The observed decreases were a clinically important level of improvement for an intervention of 4 in-person contact hours and four telephone calls. However, no differences were found in change between the symptom-focused intervention and diet and weight attentional control. The absence of differences may be explained if improvements in outcomes were caused by both the treatment intervention and control condition or if they were the result of extraneous factors.
Both the symptoms intervention and the weight and diet attentional control condition were considered to be effective. To persuasively make this case, first addressed is the potential role of extraneous factors. Multiple extraneous factors can affect outcomes and threaten the validity of study findings. Potential threats to validity most relevant to the present study include reactivity of measurement, contamination, history effects, and other measurement issues (Becker, Roberts, & Voelmeck, 2003).
Reactivity of measurement
Refers to the effect that study measures themselves can have on an individual's knowledge and behaviors. By measuring symptom distress in all study participants, weight and diet participants' awareness of the relationship between their symptoms and diabetes may have been raised as well. However, the number of symptoms reported and the level of symptom distress declined. Since increased awareness of and knowledge about diabetes-related symptoms would be expected to increase the reports of symptoms and their associated distress, it seems that reactivity of measurement would work against an observed decline in those measures. Thus, the possibility that the study measurements had some impact on participants' diabetes-related behaviors cannot be ruled out, but that would not account for the decline in symptoms and symptom-related distress. Reasons for reactivity to measurement in other instruments are not readily apparent and reactivity is not relevant to HbA1c.
Contamination
Occurs when participants in the control group are exposed to components of the intervention. The study was designed to minimize opportunities for contamination. Different nurses were used to deliver the symptom management intervention and the attentional control program. The principal investigator met weekly with the nurses who delivered both the intervention and control conditions separately to discuss any problems and issues with delivery. Over the course of the study, she also made shared visits with all the study nurses to observe the fidelity of their delivery of the intervention or program they were assigned to deliver.
History
Refers to contextual factors occurring at the same time as the intervention that affect outcomes in study participants in both the test and control arms of the study. The study data suggest that the improvement from baseline to 9 months was not a historical effect. The baseline values for new participants' outcomes did not improve significantly as the trial progressed, suggesting that the results were not due to an improvement in the overall population during the course of the trial.
Other measurement issues
Include social desirability bias and the use of self-report. While these could account for improvement in self-care practices, they could not account for the improvement in HbA1c.
Explanation of Intervention Success
One explanation for the effectiveness of both the test intervention and attentional control is that both were effective in changing behaviors and improving health outcomes. This may be due in a large part to the fact that both were tailored and individualized. It may also be due to the use of two different but effective approaches. While the objectives and content of the two approaches differed (different mechanisms), both approaches were focused on the distinct experience and personal needs of participants who were encouraged to select the management strategies best suited to their personal situation. Also, both approaches provided the opportunity to answer questions one-to-one and receive support in a nonthreatening environment as opposed to participating with a group of strangers and having to acknowledge problems with diabetes publicly. Both approaches also were tailored for use with older, rural African American women living in the southeastern US. The content and mode of delivery was based on exploratory work, recognizing the influences of both the African American and southern cultures, and further refined through pilot work and consultation with a community advisory board (Leeman et al., 2008).
Although the objectives and content of the two approaches and the strategies used were different, both may have been effective. A central objective of the symptom-focused intervention was to teach participants to recognize and interpret symptoms so they could better use their experience of symptoms as a guide to self-care (Teel et al., 1997). The central objective of the attentional control program was to teach specific self-care skills and provide opportunities to practice them. Reviews of diabetes self-care education have found that skills training combined with practice is an effective approach to improving self-care (ADA, 2008). Discussions with the intervention nurses over the course of the study as well as review of their field notes emphasize how well participants responded to the specific skill training and exercises, particularly in regards to diet.
Although the attentional control was designed to focus on diet with the expectation that it would be ineffective, it had many advantages over the education typically offered because it was individualized and tailored, and provided one-to-one training, feedback, and practice opportunities in the women's homes. Thus, we believe that what was intended as an attentional control activity made a positive impact on a significant but unrecognized need in this sample. This points to the importance of including the opportunity for this type of skills training in any intervention where self-care will be a focus and not assuming that all participants are at the same level of skill.
The Effectiveness of the Booster
The importance of the booster was demonstrated in its significant effects on reducing HbA1c and symptom distress and improving psychosocial adjustment as measured by PAID. The parsimony of this phase of the intervention (4 telephone calls of approximately 15 minutes each) with the beneficial effects on metabolic control and well-being demonstrates the importance of continuing contact as a means of sustaining treatment effects. In this study, minimal contact produced a positive effect. The nurse who originally delivered the intervention delivered the booster telephone call. This preexisting therapeutic relationship is felt to be essential to a successful booster, as a trusting milieu for supportive communication has been established already.
Summary and Conclusions
In summary, the data support the effectiveness of both the symptom-focused intervention and weight and diet attentional control. The symptom-focused intervention was particularly effective when supplemented with a telephone booster, achieving a .76% drop in HbA1c over 9 months in a high-risk group of African American elders. Both approaches and the addition of the booster were parsimonious in terms of contact time (4 hours in-home visits + 1-1.5 hours of phone contacts for the booster) and, thereby, are readily translatable to practice. The high retention rates and positive feedback from participants indicate that the interventions were well-received by participants. The study findings suggest that the symptom-focused and weight and diet approaches can be combined into a revised intervention with the potential for a greater effect on outcomes.
Acknowledgments
Funded through grant #R01 NR008582 from the National Institute of Nursing Research to the School of Nursing, University of North Carolina at Chapel Hill.
Contributor Information
Anne H. Skelly, School of Nursing, The University of North Carolina at Chapel Hill.
John Carlson, School of Nursing, The University of North Carolina at Chapel Hill.
Jennifer Leeman, School of Nursing, The University of North Carolina at Chapel Hill.
April Soward, School of Nursing, The University of North Carolina at Chapel Hill.
Dorothy Burns, School of Nursing, Hampton University.
References
- Akaike H. A new look at the statistical model identification. Transaction on Automatic Control. 1974;AC-19:717–723. [Google Scholar]
- American Diabetes Association. Diabetes 4-1-1 facts, figures & statistics at a glance: Who's getting diagnosed, why and what it means for society. Alexandria, VA: Author; 2005. [Google Scholar]
- American Diabetes Association. Clinical practice recommendations 2008. Diabetes Care. 2008;31:S1–S108. [PubMed] [Google Scholar]
- Anderson RM, Funnell MM, Nwankwo R, Gillard ML, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: Results of a randomized controlled trial. Ethnicity & Disease. 2005;15(4):671–678. [PubMed] [Google Scholar]
- Becker H, Roberts G, Voelmeck W. Explanations for improvement in both experimental and control groups. Western Journal of Nursing Research. 2003;25(6):746–755. doi: 10.1177/0193945903253002. [DOI] [PubMed] [Google Scholar]
- Coward RT, Krout JA. Aging in rural settings: Life circumstances and distinctive features. New York: Springer; 1998. p. 16. [Google Scholar]
- Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2004;59(3):S138–S145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncology Nursing Forum. 2001;28(3):465–470. [PubMed] [Google Scholar]
- Elasy TA, Samuel-Hodge CD, DeVellis RF, Skelly AH, Ammerman AS, Keyserling TC. Development of a health status measure for older African-American women with type 2 diabetes. Diabetes Care. 2000;23(3):325–329. doi: 10.2337/diacare.23.3.325. [DOI] [PubMed] [Google Scholar]
- Feathers JT, Kieffer EC, Palmisano G, Anderson M, Janz N, Spencer MS, et al. The development, implementation, and process evaluation of the REACH Detroit Partnership's Diabetes Lifestyle Intervention. The Diabetes Educator. 2007;33(3):509–520. doi: 10.1177/0145721707301371. [DOI] [PubMed] [Google Scholar]
- Funnell MM, Arnold MS, Fogler J, Merritt JH, Anderson LA. Participation in a diabetes education and care program: Experience from the Diabetes Care for Older Adults project. The Diabetes Educator. 1998;24(2):163–167. doi: 10.1177/014572179802400205. [DOI] [PubMed] [Google Scholar]
- Funnell MM, Merritt JH. The challenges of diabetes and older adults. The Nursing Clinics of North America. 1993;28(1):45–60. [PubMed] [Google Scholar]
- Given C, Given B, Rahbar M, Jeon S, McCorkle R, Cimprich B, et al. Does a symptom management intervention affect depression among cancer patients: Results from a clinical trial. Psycho-Oncology. 2004;13(11):818–830. doi: 10.1002/pon.807. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving care among older patients with type II diabetes: The “Sixty Something…” Study. Patient Education and Counseling. 1992;19(1):61–74. doi: 10.1016/0738-3991(92)90102-o. [DOI] [PubMed] [Google Scholar]
- Hoerger TJ, Segel JE, Gregg EW, Saadine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31(1):81–86. doi: 10.2337/dc07-1572. [DOI] [PubMed] [Google Scholar]
- Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self-care behaviors of African American women with type 2 diabetes: Impact on physical activity. Diabetes Care. 2002;25(9):1576–1583. doi: 10.2337/diacare.25.9.1576. [DOI] [PubMed] [Google Scholar]
- Lebovitz H, editor. Therapy for diabetes and related disorders. 3rd. Alexandria, VA: American Diabetes Association, Inc.; 1998. [Google Scholar]
- Leeman J, Skelly AH, Burns D, Carlson J, Soward A. Tailoring a diabetes self-care intervention for use with older, rural African American women. The Diabetes Educator. 2008;34(2):310–317. doi: 10.1177/0145721708316623. [DOI] [PubMed] [Google Scholar]
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- Samuel-Hodge CD, Headon SW, Skelly AH, Ingram AF, Keyserling TC, Jackson EJ, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: Spirituality, the multicaregiving role, and other social context factors. Diabetes Care. 2000;23(7):928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- Sarkisian CA, Brown AF, Norris KC, Wintz RL, Mangione CM. A systematic review of diabetes self-care interventions for older, African American, or Latino adults. The Diabetes Educator. 2003;29(3):467–479. doi: 10.1177/014572170302900311. [DOI] [PubMed] [Google Scholar]
- Saydah S, Cowie C, Eberhardt MS, De Rekeneire N, Narayan KM. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethnicity & Disease. 2007;17(3):529–535. [PubMed] [Google Scholar]
- Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- Skelly AH, Carlson JR, Leeman J, Holditch-Davis D, Soward AC. Symptom-focused diabetes management for African American elders with Type 2 diabetes: A pilot study. Applied Nursing Research. 2005;18(4):213–220. doi: 10.1016/j.apnr.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Skelly AH, Leeman J, Carlson J, Soward AC, Burns D. Conceptual model of symptom-focused diabetes care for African Americans. Journal of Nursing Scholarship. 2008;40(3):261–267. doi: 10.1111/j.1547-5069.2008.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skelly AH, Marshall JR, Haughey BP, Davis PJ, Dunford RG. Self-efficacy and confidence in outcomes as determinants of self-care practices in inner-city, African-American women with non-insulin-dependent diabetes. The Diabetes Educator. 1995;21(1):38–46. doi: 10.1177/014572179502100107. [DOI] [PubMed] [Google Scholar]
- Stoodt G, Lengerich EJ. Reducing the burden of chronic disease in rural North Carolina. North Carolina Medical Journal. 1993;54(10):532–535. [PubMed] [Google Scholar]
- Stover JC, Skelly AH, Holditch-Davis D, Dunn PF. Perceptions of health and relationship to symptoms in African American women with type 2 diabetes. Applied Nursing Research. 2001;14(2):72–80. doi: 10.1053/apnr.2001.22372. [DOI] [PubMed] [Google Scholar]
- Teel CS, Meek P, McNamara AM, Watson L. Perspectives unifying symptom intepretation. Image: The Journal of Nursing Scholarship. 1997;29(2):175–181. doi: 10.1111/j.1547-5069.1997.tb01553.x. [DOI] [PubMed] [Google Scholar]
- United Kingdom Prospective Diabetes Study. UKPDS demonstrates benefit of intensive glucose control in type 2 diabetes Issues in Type 2 Diabetes. 3. Vol. 2. Seacaucus, NJ: Professional Postgraduate Services; 1998. [Google Scholar]
- The University of California, San Francisco Symptom Management Group. Image: The Journal of Nursing Scholarship. 4. Vol. 26. 1994. A model for symptom management; pp. 272–276. [PubMed] [Google Scholar]
- Wassem R, Dudley W. Symptom management and adjustment of patients with multiple sclerosis: A 4-year longitudinal intervention study. Clinical Nursing Research. 2003;12(1):102–117. doi: 10.1177/1054773803238743. [DOI] [PubMed] [Google Scholar]
- Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale: An evaluation of its clinical utility. Diabetes Care. 1997;20(5):760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- Zimmerman L, Barnason S, Schulz P, Nieveen J, Miller C, Hertzog M, et al. The effects of a symptom management intervention on symptom evaluation, physical functioning, and physical activity for women after coronary artery bypass surgery. The Journal of Cardiovascular Nursing. 2007;22(6):493–500. doi: 10.1097/01.JCN.0000297379.06379.b6. [DOI] [PubMed] [Google Scholar]