SUMMARY
Objective
Chronic medical problems might amplify suicide risk in later life. Feelings of happiness may reduce this risk. We tested the hypothesis that happiness attenuates the association between number of self-reported chronic diseases and suicidal distress.
Methods
A sample of 1,801 depressed, primary care patients. 60 years of age or older, entering a clinical trial, were assessed for the presence of positive emotion, suicidal distress and self-reported chronic medical problems.
Results
Chronic medical problems are associated with suicide ideation and, as hypothesized, happiness attenuates the relationship between self-reported diseases and suicidal distress.
Conclusions
Decreased risk for distressing thoughts of suicide in the context of medical illness is predicted by the presence of positive emotions. Our results suggest that treatments designed to help older primary care patients identify sources of joy and enhance happiness might decrease suicide risk.
Keywords: happiness, suicide ideation, chronic medical problems, neuroticism, older adults, primary care
INTRODUCTION
In addition to mood disorders (Conwell et al., 2002), chronic medical problems are risk factors for suicidal thoughts and behaviors in older adults (Leibenluft and Goldberg, 1988; Conwell et al., 2000; Juurlink et al., 2004). As severity of medical illness increases, individuals may be more likely to have thoughts of ending their own life (Druss and Pincus, 2000): this may be of critical importance as adults age and experience increased and more severe chronic medical problems. Because this segment of the population is expected to more than double in size by the year 2030, from 30 million to 72 million (He et al., 2005). a better understanding of how risk for suicide might be mitigated in older adult patients with chronic medical problems is required (Chochinov et al., 1998).
During times of medical or functional decline, hopelessness, depression and suicide ideation often co-occur (Roose et al., 2001). and may themselves contribute to further affective and cognitive distress. The Dynamic Model of Affect (DMA) (Zautra et al., 2001) suggests that experiences which are uncontrollable or unpredictable, such as chronic illness, pain and impairment, may make it more difficult for an individual to distinguish between the negative and positive aspects of a situation (Pruchno and Meeks, 2004). Under such circumstances, negative affective states tend to crowd out positive experiences (Zautra et al., 2001). The dynamic relationship between affect and experience has been documented in older adults, patients with self-reported poor physical health, chronic pain, fibromyalgia, and rheumatoid arthritis, and in depressed and anxious patients (Zautra et al., 2003; Zautra et al., 2005; Molnar et al., 2006: Strand et al., 2006). The presence of suicidal ideation may further contribute to this effect.
The predominance of negative affect in situations of poor health or functional impairment, however, does not preclude the existence of positive emotions. Indeed, the harmful physiological and psychological effects of chronic medical problems may be mitigated by positive emotions (Fredrickson, 2000; Zautra et al., 2003). The ability to maintain positive emotionality during periods of illness has been associated with improved physical and mental health and well-being in many studies (Ostir et al., 2000; Danner et al., 2001; Zautra et al., 2005; Strand et al., 2006), though of course there have been negative findings.
In the current study, we assessed subjective happiness, which is defined as a sense of subjective well-being, increased positive affect, and life satisfaction (Lyubomirsky et al., 2005). Happiness appears to be largely attributable to stable biological and volitional factors (Lyubomirsky et al., 2005; Steel et al., 2008), and is related to dispositional personality characteristics, particularly higher levels of extraversion (Lucas and Diener, 2000; Steel and Ones, 2002).
Although the presence of happiness in a depressed patient may seem implausible there is empirical support to suggest that depressed individuals have at least one area of their lives about which they are not depressed (Pelham, 1991; Snyder et al., 1991). Both the DMA (Zautra et., al, 2003) and the Evaluative Space Model (Cacioppo and Berntson, 1994) suggest that positive and negative emotions can be experienced simultaneously. The biological plausibility of these models has been established: negative emotions appear to be mediated by the right frontal cortex and amygdala, whereas positive emotions are associated with the left frontal cortex and the ventral tegmental area (Davidson, 1998; Larson et al., 2001). Importantly, the two emotion systems can be coactivated (Cacioppo and Berntson, 1994).
In this paper, we present secondary analyses of a large sample (n= 1,801) of older adults with depression and significant comorbid medical illness to examine the effect of happiness on distress related to suicide ideation. We hypothesized that happiness would moderate the relationship between number of self-reported chronic medical problems and the distress caused by having thoughts of taking one’s life, after accounting for sociodemographic characteristics, cognitive status, comorbid psychopathology and treatment history.
METHODS
Participants
We studied depressed, primary care patients, given that mood disorders and physical illness are strongly associated with suicidal behavior in older adults (Conwell et al., 2002). Older adults are also more likely to visit primary care physicians than mental health professionals, making primary care settings an important venue for identification of at-risk patients and implementation of intervention efforts (Luoma et al., 2002; Bruce et al., 2004; Unützer et al., 2006).
Patients were recruited as part of the IMPACT study, a multisite randomized controlled trial of a collaborative intervention program for late-life depression in primary care (Unützer et al., 2001, 2002). The IMPACT trial was conducted in 18 primary care clinics affiliated with eight diverse health care organizations in five states (Indiana, Texas, North Carolina, California, Washington). Procedures were approved by institutional review boards at all sites, and all participants provided written informed consent.
Each site used a two-pronged recruitment strategy involving clinic referrals and depression screening. We used baseline data for 1,801 subjects (86% of those eligible; See Table 1), which were obtained by trained interviewers using structured computerized interviews (Unützer et al., 2002). Patients who were 60 years of age or older, planned to use a participating clinic as their main source of general medical care for the upcoming year, and had a Structured Clinical Interview for DSM-IV (SCID) (First et al., 1997) diagnosis of current major depression or dysthymic disorder, were eligible. Patients who screened positive for current alcohol abuse, severe cognitive impairment, a history of bipolar disorder or psychosis, or who were receiving active treatment by a psychiatrist were excluded. Less than 1% of potential subjects were excluded due to acute suicide risk requiring immediate clinical intervention.
Table 1.
Baseline sociodemographic and clinical characteristics
| Mean (SD) [N(%)] | |
|---|---|
| Age | 71.18 (7.47) |
| Female Gender [N(%)] | 1168 (65%) |
| Level of Education [N(%)] | |
| Less than High School | 346 (19.21) |
| High School Graduate | 409 (22.71) |
| Some College | 636 (35.31) |
| College Graduate | 410 (22.77) |
| Income Level | $37,171 (63.157) |
| Cognitive screening score | 5.54 (.71) |
| Positive anxiety screen [N(%)] | 527 (29%) |
| Neuroticism score | 22.52 (5.25) |
| Prior depression treatment (antidepressant medications or psychotherapy). past 3 months | 828 (46%) |
| Mood disorder (SCID diagnosis) [N(%)] | |
| Major depression | 306 (17%) |
| Dysthymia | 544 (30.2%) |
| Major depression and dysthymia | 951 (52.8%) |
| Chronic medical problems (of a list of 11) | 3.22 ± 1.73 |
| Happiness | 2.92 (1.20) |
Cognitive screening score = six-item screening tool derived from MMSE; Anxiety Screening Score = Positive response for PTSD or Panic Disorder; Neuroticism = Subscale score from adaptation of NEO-PI-R; Prior Depression Treatment = Antidepressants or therapy in last 3 months; Mood Disorder = SCID diagnosis of Major Depression or Dysthymia or Both; Chronic medical problems = Number of self-reported diseases; Happiness = Item # 14 from SF-16.
Measures
Baseline interviews assessed sociodemographic characteristics, SCID diagnoses of major depression, dysthymia, or both (Williams et al., 1992; First et al., 1997), and screening questions for two anxiety disorders, panic disorder and posttraumatic stress disorder (Unützer et al., 2002). Respondents indicated whether they had been diagnosed with or treated for 11 common chronic medical problems in the past 3 years, including: chronic lung disease, hypertension, diabetes, arthritis, cancer, loss of hearing or vision, neurological disease, heart disease, chronic pain, gastrointestinal disease, and urinary tract or prostate disease. Respondents also answered questions regarding depression treatment, including the use of antidepressant medications, psychotherapy, and health service utilization in the past 3 months (Unützer et al., 2003). Happiness was assessed using a single item from the Rand 12 item Short Form (SF-12) (Ware et al., 1996): ‘How much of the time during the past 4 weeks have you been a happy person?’. Response options for this item were: ‘all of the time’, ‘most of the time’, ‘a good bit of the time’, ‘some of the time’, ‘a little of the time’ and ‘none of the time’. This self-report item has been successfully used to assess happiness in young adults and individuals with disabilities, and the larger Mental Health scale from which it is drawn is valid and reliable for use in depressed older adults (Perneger et al., 2004; Friedman et al., 2005; van Campen and Iedema, 2007). Higher scores indicate greater levels of happiness. Neuroticism, which refers to a predisposition to experience negative affects such as sadness and anxiety, was assessed using seven-items from the NEO Personality Inventory—Revised (NEO-PI-R) (Costa and McCrae. 1992), with higher scores indicating greater levels of neuroticism. Cognitive status was assessed using a six-item screening tool derived from the Mini-Mental Status Examination, which has exhibited adequate sensitivity and specificity for a diagnosis of dementia (Callahan et al., 2002). Lower scores indicate greater cognitive impairment.
Distress resulting from thoughts of suicide was assessed using a single, rater-administered item from the Hopkins Symptoms Checklist (HSCL) (Lipman et al., 1979). This question asked, ‘In the past month, how much were you distressed by thoughts of ending your life?’. Response choices were: ‘not at all’, ‘a little’, ‘quite a bit’ or ‘extremely’. Higher scores indicate greater levels of suicidal distress.
Statistical analyses
We examined demographic and baseline clinical characteristics of the enrolled sample (Table 1). Bivariate correlations were derived for all study variables (Table 2). Hierarchical, multivariate linear and logistic regressions were conducted to examine the associations of happiness, medical illness, and suicide ideation (Table 3). Consistent with recommendations for conducting moderator analyses (Baron and Kenny. 1986), covariates and predictors were entered on the first step of the regression model and interaction terms were entered on the second. For the logistic model, distress from suicide was dichotomized as no distress from suicide (0) or any distress from suicide (1). Predictor variables were centered prior to creating interaction terms. Distress from suicidal thoughts was square-root transformed to normalize the distribution of the dependent variable. The interaction was graphed comparing two sub-groups of patients: those who reported being happy (1) none of the time, a little of the time, or some of the time vs (2) all of the time, most of the time, or a good bit of the time. Covariates included age. gender, study site (categorical; seven sites), educational status, income level (continuous), positive screen for anxiety disorder (dichotomous), depression severity (dichotomous; major depression or dysthymia, vs major depression and dysthymia), neuroticism, cognitive screening score, and any type of depression treatment in the last 3 months (dichotomous). Data imputation strategies have been previously described (Tang et al., 2005).
Table 2.
Bivariate correlations for study variables (n = 1,801)
| Female gender |
Education Level |
Income | Cognitive Screening Score |
Positive Anxiety screen |
Neuroticism | Prior Depression Treatment |
Mood Disorder |
Chronic Medical Problems |
Happiness | Suicide Ideation |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 0.00 | 0.05* | 0.09** | .16** | 0.08** | 0.13** | −0.10** | 0.09** | 0.11** | 0.11** | −0.03 |
| Female gender | — | 0.07** | 0.09** | −0.07** | −0.04 | −0.15** | −0.10** | 0.03 | 0.09** | 0.03 | 0.01 |
| Education level | — | — | 0.19** | 0.15** | 0.03 | 0.14** | −0.03 | −0.04 | −0.12** | 0.02 | 0.02 |
| Income | — | — | — | 0.05 | −0.04 | −0.05* | 0.02 | 0.02 | −0.11** | 0.02 | −0.00 |
| Cognitive screening score | — | — | — | — | −0.01 | 0.04 | −0.02 | 0.01 | −0.05* | −0.05* | 0.02 |
| Positive anxiety screen | — | — | — | — | 0.23** | 0.07** | 0.10** | 0.09** | −0.13** | 0.15** | |
| Neuroticism | — | — | — | — | — | — | 0.05* | 0.21** | 0.09** | −0.23** | 0.21** |
| Prior Depression treatment | — | — | — | — | — | — | — | 0.05* | 0.00 | 00.04 | 0.03 |
| Mood disorder | — | — | — | — | — | — | — | — | 0.11** | −0.09** | 0.10** |
| Chronic medical problems | — | — | — | — | — | — | — | — | — | 0.03 | 0.04 |
| Happiness | — | — | — | — | — | — | — | — | — | — | −0.15** |
Note: Income = Total income level in the last year; Education level = less than high school, high school graduate, some college, college graduate; Cognitive screening score = 6-item screening tool derived from MMSE; Anxiety Screening Score = Positive response for PTSD or Panic Disorder; Neuroticism = Subscale score from adaptation of NEO-PI-R; Prior Depression Treatment = Antidepressants or therapy in last 3 months; Mood Disorder = SCID diagnosis of Major Depression or Dysthymia, or Both; Chronic medical problems = Number of self-reported diseases; Happiness = Item #14 from SF-16; Suicide Ideation = Item #13 from Hopkins Symptom Checklist. Correlations are Pearson’s r (for continuous variables) or point biserial (for dichotomous - gender, positive anxiety screen, prior depression treatment, and mood disorder).
Note:
= p<.01.
= p<.05.
Table 3.
Predictors of suicide ideation: multivariate linear regression analysis
| Predictor | Suicide Ideation (n= 1801) |
|||
|---|---|---|---|---|
| Step 1 |
Step 2 |
|||
| T-value | Unstandardized Beta (SE) | T-value | Unstandardized Beta (SE) | |
| Age | 0.86 | 0.00 (0.00) | 0.85 | 0.00 (0.00) |
| Female gender | 1.59 | 0.05 (0.03) | 1.66 | 0.05 (0.03) |
| Education level | 2.20* | 0.03 (0.02) | 2.24* | 0.03 (0.02) |
| Income | 0.03 | 0.00 (0.00) | −0.01 | −0.00 (0.00) |
| Cognitive screening score | 0.37 | 0.01 (0.02) | 0.45 | 0.01 (0.02) |
| Positive anxiety screening score | 4.17*** | 0.14 (0.04) | 4.20*** | 0.20 (0.03) |
| Neuroticism | 6.50*** | 0.02 (0.00) | 6.52*** | 0.02 (0.00) |
| Prior depression treatment | 0.55 | 0.02 (0.03) | 0.60 | 0.02 (0.03) |
| Mood disorder | 2.90** | 0.09 (0.03) | 2.90** | 0.09 (0.03) |
| Chronic medical problems | 0.27 | 0.00 (0.01) | 0.25 | 0.00 (0.01) |
| Happiness | −4.10*** | −0.06 (0.01) | −4.21*** | −0.06 (0.01) |
| Chronic medical problems X happiness | — | — | −2.28* | −0.02 (0.01) |
Income = Total income level in the last year; Education level = less than high school, high school graduate, some college, college graduate; Cognitive screening score = six-item screening tool derived from MMSE; Anxiety Screening Score = Positive response for PTSD or Panic Disorder; Neuroticism = Subscale score from adaptation of NEO-PI-R; Prior Depression Treatment = Antidepressants or therapy in last 3 months; Mood Disorder = SCID diagnosis of Major Depression or Dysthymia or Both; Chronic medical problems = Number of self-reported diseases; Happiness=Item #14 from SF-16: Suicide Ideation = Item #13 from Hopkins Symptom Checklist. Correlations are Pearson’s r (for continuous variables) or point biserial (for dichotomous—gender, positive anxiety screen, prior depression treatment, and mood disorder).
p < 0.001.
p <0.01.
p < 0.05.
RESULTS
Bivariate correlation analyses revealed significant positive correlations between suicide ideation and the anxiety screen as well as mood disorder severity; happiness was significantly negatively associated with suicidal distress (see Table 2). Fourteen percent (n = 258) of our sample reported experiencing at least some distress as a result of suicidal thoughts.
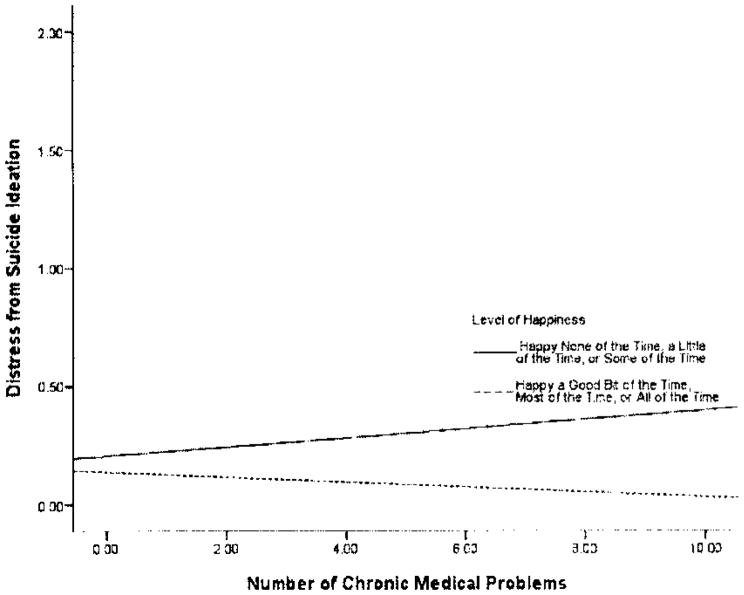
Level of happiness was a significant moderator of the relationship between chronic medical problems and distress from suicide ideation, t = − 2.28, Un ß (SE) = − 0.02 (0.01), p < 0.05. As the number or chronic medical problems increases, so does distress associated with suicide ideation, but the relationship is moderated by happiness (see Table 3). A graphic representation of the moderator interaction indicates a divergent pattern between the low happiness and high happiness subgroups (see Figure 1). Among patients who reported being happy ‘some of the time’ or less frequently, the association between medical illness and suicidal distress was positive. Remarkably, among patients who reported being happy a ‘good bit of the time’ or more frequently, the relationship between medical illness and suicidal distress was negative. Higher levels of education, greater depression severity, the presence of a positive screen for anxiety disorder, and higher levels of neuroticism were independently associated with higher levels of suicidal distress.
Figure 1.
Interaction of relationship between happiness, chronic medical problems, and distress from suicide ideation. Chronic medical problems = Number of self-reported diseases; Happiness=Item #14 from SF-16; Suicide Ideation = Item #13 from Hopkins Symptom Checklist (‘In the past month, how much were you distressed by thoughts of ending your life?’).
We also conducted a logistic regression, predicting whether or not a patient experienced distress from suicide ideation. Happiness was associated with the absence of suicidal distress [Odds Ratio (OR) = 0.80: 95% Confidence Intervals (CI) = 0.70–0.91 ], whereas anxiety (OR = 1.72, 95% CI = 1.29–2.29), neuroticism (OR = 1.09; 95% CI = 1.07–1.13) and severity of depression (OR = 1.39, 95% CI = 1.04–1.87) were associated with distress from suicide ideation. The OR (95% CI) for the interaction term between chronic medical problems and happiness was in the expected direction, 0.95 (0.89–1.02).
DISCUSSION
Our data suggest that happiness moderates the association between self-reported chronic disease and suicidal distress in depressed, primary care patients, 60 years of age or older. The effect is more evident in the linear model, likely due to constraints on statistical power in the logistic model. Our findings have implications for the conceptualization of prevention and treatment programs designed to mitigate suicide risk.
Although medical illness is a significant risk factor for suicide ideation and suicide in older adults (Conwell et al., 2000; Druss and Pincus, 2000), most older adults with chronic medical problems do not report suicidal thoughts. Our findings suggest that individuals with chronic medical problems who also report the presence of positive emotion at least ‘a good bit of the time’, are less distressed by thoughts of suicide. Our results also suggest the relative independence of positive and negative affect in depressed, older adults with chronic medical problems and provide support for the Evaluative Space Model of affect and Dynamic Model of Affect (Cacioppo and Berntson, 1994; Zautra et al, 2003).
The presence of positive affect should not be confused with the absence of negative affect. Although there is considerable support for a bipolar model of affect in which, for instance, the presence of sadness precludes the presence of happiness (Russell, 1980), there is also a growing body of support for the manifestation of positive and negative affect as orthogonal constructs (Tellegen, 1985). Degree of affective separation may depend on both the emotion-eliciting circumstance and the complexity of an individual’s emotional response to the experience (Larsen et al., 2001). Our findings point to the potentially protective effects of the presence of positive affect, as opposed to the absence of negative affect. Similar findings have been reported elsewhere (Young et al., 1996; Kunzmann et al., 2000; Ostir et al., 2000; Duberstein et al., 2001; Sullivan et al., 2001; Hirsch et al., 2007b). Happier individuals may lessen their risk for suicidal thoughts and behaviors, as well as other adverse health outcomes, through increased volitional behavior, including involvement in meaningful relationships and a greater willingness to set and strive toward future oriented goals (Linehan et al., 1983; Ormel et al., 1997;Vaillant, 2003; Hirsch et al., 2006). We recognize there may be some limits to this beneficial effect. In the face of negative life events, such as chronic medical problems, excessive or unrealistic levels of positive emotion or optimism may be detrimental (Pressman and Cohen, 2005; Segerstrom, 2005: Hirsch et al., 2007c), perhaps resulting in symptom denial, a lack of adherence to treatment, unrealistic expectations for recovery, and poor planning for the future.
Because positive emotional and cognitive characteristics have been shown to predict improved mental and physical health outcomes prospectively (Carver et al., 1994; Achat et al., 2000: Kubzansky et al., 2001), interventions designed to boost positive mood might enhance quality of life (Fredrickson, 2000; Lyubomirsky et al., 2005). It is important to note, however, that education level, anxiety, neuroticism, and mood disorder were also significant predictors of distress from suicide ideation in our model, suggesting that there is no single route to the reduction of suicide ideation.
With respect to the happiness findings, an analogy might be helpful. Just as positive and negative affective states may be simultaneously experienced, they may also need to be jointly addressed therapeutically. Treatments designed to reduce depression and suicidal thoughts and behaviors could also attempt to enhance positive affect and happiness (Johnson et al., 1996; Riskind et al., 1996; Stewart et al., 2001; Szanto et al., 2001; Townsend et al.. 2001).
Positive affect may be alterable via a variety of strategies (Fredrickson, 2000; Lyubomirsky et al., 2005). Individual and group format interventions emphasizing stress-reduction, goal identification and achievement, behavioral activation, relaxation and meditation, and changing attributions have resulted in increased happiness, hopefulness, optimism and positive affect in community-dwelling older adults, bereaved older adults and hypertensive patients (Elliot and Dweck, 1988; Fredrickson, 2000: Stewart et al., 2001; McCraty et al., 2003: West et al., 2004; Schreiner et al., 2005). Similar interventions have also led to reductions in depressive symptoms and suicidal thoughts and behaviors (Jaycox et al., 1994; Gillham and Reivich, 2004). Our results suggest that strategies designed to increase levels of happiness could be an important component of a suicide intervention program targeting older adults with chronic medical problems.
The current findings must be interpreted in the context of the study’s limitations. A small number (less than 1%) of potentially eligible subjects were excluded at baseline because they were felt to be acutely suicidal, requiring immediate intervention. Effect sizes are modest. Generalizability to other recruitment settings and demographic subgroups of depressed patients is unknown. Given the potential for biased self report of chronic medical problems, future research should incorporate objective measures. In this cross-sectional, secondary analysis, we did not have a more detailed assessment of suicidal ideation, and our use of a single item to assess positive emotion is not ideal.
Continued examination of the relationship between suicide ideation and behavior is also necessary. Although most older adults with thoughts of suicide do not act on them (Fawcett et al., 1993; Waern et al., 1999), suicidal ideation and the distress it creates are associated with increased risk of suicide attempt (Mann et al., 1999), which is frequently but not necessarily (Duberstein et al., 2006) a precursor to completed suicide (Hawton and Harriss, 2006; O’Connell et al., 2004). Future-orientation and positive affect appear to reduce risk for suicidal thoughts and behaviors in older adults (Hirsch et al., 2006, 2007a), and the encouragement of positive thoughts and emotions may initiate an upward spiral in mood and physical functioning (Fredrickson and Joiner, 2002), which has implications for treatment. Targeted interventions that attempt to promote positive thoughts and mood might decrease distress and suicidal thoughts and behaviors, as well as enhance some aspects of physical well-being and quality of life, for older adults with chronic medical problems.
KEY POINTS.
Chronic medical problems are associated with distressful suicidal thoughts, but feelings of happiness may reduce this risk;
Treatments designed to help older primary care patients identify sources of joy and enhance happiness might decrease suicide risk.
Acknowledgments
This study is supported by grants from the John A. Hartford Foundation, the California HealthCare Foundation, the Hogg Foundation, and the Robert Wood Johnson Foundation. Preparation of this manuscript was supported by PHS T32 MH020061 and K24MH072712. The study protocol was formulated independently by the investigators and approved by institutional review boards at the UCLA study coordinating center and all participating study sites. The sponsors of the study had no role in study design, data collection, data analysis, interpretation of the data, or in the decision to submit this manuscript for publication.
We would like to acknowledge the contributions and support of patients, primary care providers, and staff at the study coordinating center and at all participating study sites, which include: Duke University, Durham, NC; The South Texas Veterans Health Care System, The Central Texas Veterans Health Care System, and The San Antonio Preventive and Diagnostic Medicine Clinic; Indiana University School of Medicine, Indianapolis, IN; Health and Hospital Corporation of Marion County, Indianapolis, IN; Group Health Cooperative of Puget Sound in cooperation with the University of Washington, Seattle, WA; Kaiser Permanente of Northern California, Oakland and Hayward, CA; Kaiser Permanente of Southern California. San Diego, CA; Desert Medical Group. Palm Springs, CA. This study is the result of work supported in part with patients, resources, and the use of facilities at the South Texas Veterans Health Care System and the Central Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
We would also like to acknowledge the contributions the IMPACT study advisory board (Lisa Goodale, ACSW; Richard C. Birkel PhD; Howard Goldman, MD, PhD; Thomas Oxman, MD; Lisa Rubenstein, MD, MSPH; Cathy Sherbourne, PhD; Kenneth Wells, MD, MPH).
Footnotes
CONFLICT OF INTEREST
None known.
AUTHOR CONTRIBUTIONS
Jameson K. Hirsch—Study concept and design, analysis and interpretation of data, preparation of manuscript.
Paul R. Duberstein—study concept and design, analysis and interpretation of data, preparation of manuscript.
Jürgen Unützer—study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, preparation of manuscript.
References
- Achat H, Kawachi I, Spiro A, et al. Optimism and depression as predictors of physical and mental health functioning: the normative aging study. Ann Behav Med. 2000;22(2):127–130. doi: 10.1007/BF02895776. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Personality Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG. Relationship between attitudes and evaluative space: A critical review, with emphasis on the separability of positive and negative substrates. Psychological Bull. 1994;115:401–423. [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- Carver CS, Pozokaderman C, Harris SD, et al. Optimism versus pessimism predicts the quality of womens adjustment to early-stage breast-cancer. Cancer. 1994;73(4):1213–1220. doi: 10.1002/1097-0142(19940215)73:4<1213::aid-cncr2820730415>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Chochinov HM, Wilson KG, Enns M, Lander S. Depression, hopelessness, and suicidal ideation in the terminally ill. Psychosom. 1998;39(4):366–370. doi: 10.1016/S0033-3182(98)71325-8. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biological Psychiatry. 2002;52(3):193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Lyness JM, Duberstein P, et al. Completed suicide among older patients in primary care practices: A controlled study. J Am Geriatr Soc. 2000;48(1):23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five Factor Inventory (NEO-FFI) Professional Manual. Psychological Assessment Resources, Inc; Odessa, FL: 1992. [Google Scholar]
- Danner DD, Snowdon DA, Friesen WV. Positive emotions in early life and longevity: Findings from the nun study. J Personality Soc Psychology. 2001;80(5):804–813. [PubMed] [Google Scholar]
- Davidson RJ. Affective Style and affective disorders: perspectives from affective neuroscience. Cog Emotion. 1998;12(3):307–330. [Google Scholar]
- Druss B, Pincus H. Suicidal ideation and suicide attempts in general medical illnesses. Arch Intern Med. 2000;160(10):1522–1526. doi: 10.1001/archinte.160.10.1522. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conner KR, Conwell Y, Cox C. Personality correlates of hopelessness in depressed inpatients 50 years of age and older. J Personality Assess. 2001;77(2):380–390. doi: 10.1207/S15327752JPA7702_16. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Heisel MJ, Conwell Y. Suicide. In: Agronin ME, Maletta G, editors. Geriatric Psychiatry: Evaluation and Management. Lippincott Williams & Wilkins; Philadelphia, PA: 2006. pp. 393–406. [Google Scholar]
- Elliot ES, Dweck CS. Goals: an approach to motivation and achievement. J Personality Soc Psychol. 1988;54:5–12. doi: 10.1037//0022-3514.54.1.5. [DOI] [PubMed] [Google Scholar]
- Faweett JA, Clark DC, Bush KA. Assessing and treating the patient at risk for suicide. Psychiatric Ann. 1993;23:244–256. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0, 4/97 revision) Biometrics Research Department. New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Fredrickson B. Cultivating positive emotions to optimize health and well-being. PreventTreat. 2000;3:1–25. [Google Scholar]
- Fredrickson B, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychological Sri. 2002;13(2):172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Friedman B, Heisel M, Delavan R. Validity of the SF-36 five-item mental health index for major depression in functionally impaired, community-dwelling elderly patients. J Am Geriatr Soc. 2005;53(11):1978–1985. doi: 10.1111/j.1532-5415.2005.00469.x. [DOI] [PubMed] [Google Scholar]
- Gillham J, Reivich K. Cultivating optimism in childhood and adolescence. Ann Am Acad Political Soc Sci. 2004;591(1):146–163. [Google Scholar]
- Hawton K, Harriss L. Deliberate self-harm in people aged 60 years and over: Characteristics and outcome of a 20-year cohort. Int J Geriatr Psychiatry. 2006;21(6):572–581. doi: 10.1002/gps.1526. [DOI] [PubMed] [Google Scholar]
- He W, Sengupta M, Velkoff V, DeBarros K. 65+ in the United States: 2005. US Census Bureau; Washington, DC: 2005. [Google Scholar]
- Hirsch JK, Duberstein P, Conner KR, et al. Future orientation and suicide ideation and attempts in depressed adults ages 50 and over. Am J Geriatr Psychiatry. 2006;14:752–757. doi: 10.1097/01.JGP.0000209219.06017.62. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein P, Conner KR, et al. Hopelessness and future orientation as potential moderators of the relationship between functional impairment and suicide ideation in depressed adults ages 55 and over. Depression Anxiety. 2007a;24(3):196–201. doi: 10.1002/da.20224. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein PR, Chapman B, Lyness JM. Positive and negative affect and suicide ideation in older adult primary care patients. Psychology Aging. 2007b;22(2):80–85. doi: 10.1037/0882-7974.22.2.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JK, Wolford K, Brunk L, Parker-Morris A. Dispositional optimism as a moderator of the association between negative life events and suicide ideation and attempts. Cog Ther Res. 2007c;31:533–546. [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman ME. Prevention of depressive symptoms in school children. Behav Res Ther. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Crofton A, Feinstein SB. Enhancing attributional style and positive life events predict increased hopefulness among depressed psychiatric inpatients. Motivation Emotion. 1996;20(4):285–297. [Google Scholar]
- Juurlink DN, Herrmann N, Szalai JP, et al. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164(11):1179–1184. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the Normative Aging Study. Psychosom Med. 2001;63(6):910–916. doi: 10.1097/00006842-200111000-00009. [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Little TD, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychology Aging. 2000;15:511–526. doi: 10.1037//0882-7974.15.3.511. [DOI] [PubMed] [Google Scholar]
- Larsen JT, McGraw AP, Cacioppo JT. Can people feel happy and sad at the same time? J Personality Soc Psychol. 2001;81:684–696. [PubMed] [Google Scholar]
- Leibenluft E, Goldberg RL. The suicidal, terminally ill patient with depression. Psychosom. 1988;29(4):379–386. doi: 10.1016/S0033-3182(88)72337-3. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing yourself: The Reasons for Living Inventors. J Consulting Clin Psychol. 1983;51(2):276–286. doi: 10.1037//0022-006x.51.2.276. [DOI] [PubMed] [Google Scholar]
- Lipman RS, Covi L, Shapiro AK. The Hopkins Symptom Checklist (HSCL) - factors derived from the HSCL-90. J Affect Disord. 1979;1:9–24. doi: 10.1016/0165-0327(79)90021-1. [DOI] [PubMed] [Google Scholar]
- Lucas RE, Diener E. Personality and subjective well-being across the life span. In: Molfese VJ, Molfese DL, editors. Temperament and Personality Development Across the Life Span. Erlbaum; Mahwah, NJ: 2000. pp. 211–234. [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S, Sheldon KM, Schkade D. Pursuing happiness: the architecture of sustainable change. Gen Rev Psychol. 2005;9(2):111–131. [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- McCraty R, Atkinson M, Tomasino D. Impact of a workplace stress reduction program on blood pressure and emotional health in hypertensive employees. J Alternative Complementary Med. 2003;9(3):355–369. doi: 10.1089/107555303765551589. [DOI] [PubMed] [Google Scholar]
- Molnar DS, Reker DL, Culp NA, et al. A mediated model of perfectionism, affect, and physical health. J Res Personality. 2006;40(5):482–500. [Google Scholar]
- O’Connell H, Chin AV, Cunningham C, Lawlor BA. Recent developments: Suicide in older people. BMJ. 2004;329(7471):895–899. doi: 10.1136/bmj.329.7471.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Kempen GIJM, Penninx BWJH, et al. Chronic-medical conditions and mental health in older people: disability and psychosocial resources mediate specific mental health effects. Psychologic Med. 1997;27(5):1065–1077. doi: 10.1017/s0033291797005321. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. J Am Geriatr Soc. 2000;48:590–592. doi: 10.1111/j.1532-5415.2000.tb04991.x. [DOI] [PubMed] [Google Scholar]
- Pelham BW. On the benefits of misery: self-serving biases in the depressive self-concept. J Personality Soc Psychol. 1991;61:670–681. doi: 10.1037//0022-3514.61.4.670. [DOI] [PubMed] [Google Scholar]
- Perneger TV, Hudelson PM, Bovier PA. Health and happiness in young Swiss adults. Qual Life Res. 2004;13(1):171–178. doi: 10.1023/B:QURE.0000015314.97546.60. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bull. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Meeks S. Health related stress, affect, and depressive symptoms experienced by caregiving mothers of adults with a developmental disability. Psychol Aging. 2004;19:394–401. doi: 10.1037/0882-7974.19.3.394. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Sarampote CS, Mercier MA. For every malady a sovereign cure: optimism training. J Cog Psychother: Int Quart. 1996:10. [Google Scholar]
- Roose SP, Glassman AH, Seidman SN. Relationship between depression and other medical illnesses. JAMA. 2001;286(14):1687–1690. doi: 10.1001/jama.286.14.1687. [DOI] [PubMed] [Google Scholar]
- Russell JA. A circumplex model of affect. J Personality Soc Psychol. 1980;39:1161–1178. [Google Scholar]
- Schreiner AS, Yamamoto E, Shiotani H. Positive affect among nursing home residents with Alzheimer’s dementia: the effect of recreational activity. Aging Mental Health. 2005;V9(2):129–134. doi: 10.1080/13607860412331336841. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC. Optimism and immunity: do positive thoughts always lead to positive effects? Brain Behav Immunity. 2005;19(3):195–200. doi: 10.1016/j.bbi.2004.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder CR, Harris C, Anderson JR, et al. The will and the ways—development and validation of an individual-differences measure of hope. J Personality Soc Psychol. 1991;60(4):570–585. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- Steel P, Ones DS. Personality and happiness: a national level analysis. J Personality Soc Psychol. 2002;83:767–781. [PubMed] [Google Scholar]
- Steel P, Schmidt J, Shultz J. Refining the relationship between personality and subjective well-being. Psychological Bull. 2008;134:138–161. doi: 10.1037/0033-2909.134.1.138. [DOI] [PubMed] [Google Scholar]
- Stewart M, Craig D, MacPherson K, Alexanders Promoting positive affect and diminishing loneliness of widowed seniors through a support intervention. Public Health Nurs. 2001;18:54–63. doi: 10.1046/j.1525-1446.2001.00054.x. [DOI] [PubMed] [Google Scholar]
- Strand EB, Zautra AJ, Thoresen M, et al. Positive affect as a factor of resilience in the pain-negative affect relationship in patients with rheumatoid arthritis. J Psxchosom lies. 2006;60(5):477–484. doi: 10.1016/j.jpsychores.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, LaCroix AZ, Russo JE, Walker EA. Depression and self-reported physical health in patients with coronary disease: mediating and moderating factors. Psychosom Med. 2001;63(2):248–256. doi: 10.1097/00006842-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck PR, et al. Treatment outcome in suicidal vs. non-suicidal elderly patients. Am I Geriatr Psychiatry. 2001;9(3):261–268. [PubMed] [Google Scholar]
- Tang L, Song J, Belin TR, Unützer J. A comparison of imputation methods in a longitudinal randomized clinical trial. Stat Med. 2005;24:2111–2128. doi: 10.1002/sim.2099. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In: Tuma AH, Mason J, editors. Anxiety and the Anxiety Disorders. Erlbaum; Hillsdale, NJ: 1985. pp. 681–706. [Google Scholar]
- Townsend E, Hawton K, Altman DG, et al. The efficacy of problem-solving treatments after deliberate self-harm: meta-analysis of randomized controlled trials with respect to depression, hopelessness and improvement in problems. Psychological Med. 2001;31(6):979–988. doi: 10.1017/s0033291701004238. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Williams JW, Jr, et al. Improving primary care for depression in late life: The design of a multicenter randomized trial. Medical Care. 2001;39(8):785–799. doi: 10.1097/00005650-200108000-00005. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, et al. for the IMPACT lnvestigators. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. J Am Geriatr Soc. 2003;51(4):505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- Unützer J, Tang L, Oishi S, et al. Reducing suicidal ideation in depressed older primary care patients. J Am Geriatr Soc. 2006;54(10):1550–1556. doi: 10.1111/j.1532-5415.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- Vaillant GE. Mental health. Am J Psychiatry. 2003;160(8):1373–1384. doi: 10.1176/appi.ajp.160.8.1373. [DOI] [PubMed] [Google Scholar]
- van Campen C, Iedema J. Are persons with physical disabilities who participate in society healthier and happier? Structural equation modelling of objective participation and subjective well-being. Qual Life Res. 2007;16(4):635–645. doi: 10.1007/s11136-006-9147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waern M, Beskow J, Runeson B, Skoog I. Suicidal feelings in the last year of life in elderly people who commit suicide. Lancet. 1999;354(9182):917–918. doi: 10.1016/S0140-6736(99)93099-4. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–226. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- West J, Otte C, Geher K, Johnson J, Mohr DC. Effects of Hatha Yoga and African dance on perceived stress, effect, and salivary cortisol. Ann Behav Med. 2004;28(2):114–118. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, et al. The Structured Clinical Interview for DSM-III-R (SCID). II Multisite test–retest reliability. Arch Gen Psychiatry. 1992;49(8):630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Young MA, Fogg LF, Scheftner W, et al. Stable trait components of hopelessness: Baseline and sensitivity to depression. J Abnorm Psychol. 1996;105(2):155–165. doi: 10.1037//0021-843x.105.2.155. [DOI] [PubMed] [Google Scholar]
- Zautra A, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: application of a dynamic model of affect. J Consulting Clin Psychol. 2001;69:786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consulting Clin Psychol. 2005;73(2):212–220. doi: 10.1037/0022-006X.73.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Reich JW, Davis M. Dimensions of affect relationships: models and their integrative implications. Rev Gen Psychol. 2003;7:66–83. [Google Scholar]