Orthotopic liver transplantation is frequently associated with hemostatic disorders and a bleeding diathesis.1,2 Accelerated fibrinolysis has been recognized as an important component of the hemostatic defect.1,2 The origin of this fibrinolytic activity, however, is still unclear. We investigated the role of tissue-type plasminogen activator (tPA), a potent activator of the fibrinolytic system, in the origin of increased fibrinolytic activity during orthotopic liver transplantation.
MATERIALS AND METHODS
Arterial blood samples were taken at regular intervals during 20 consecutive, first-time orthotopic liver transplantations in adults. Fibrinolysis was measured by euglobulin lysis time (ELT; normal >120 minutes) and whole blood clot lysis time, as determined by thromboelastography (normal > 150 minutes). tPA activity was measured in acidified plasma (pH 4.0–4.1) using Coaset tPA/PAI (Kabi Vitrum, Stockholm, Sweden) (normal: 0–1 IU/mL).
RESULTS
In all but one patient moderate to severe fibrinolysis, as measured by shortening of ELT or whole blood clot lysis time, was found in at least one blood sample during surgery. Intraoperative levels of tPA activity are shown in Fig 1. An intraoperative increase of tPA activity was found in 18 of the 20 patients. Comparison of the tPA activity levels and the corresponding values of the ELT showed that an increase of tPA activity to about 10 IU/mL resulted in a rapid shortening of the ELT, while a further increase had no additional effect. A more linear relation was found between tPA activity and the whole blood clot lysis time.
Fig 1.
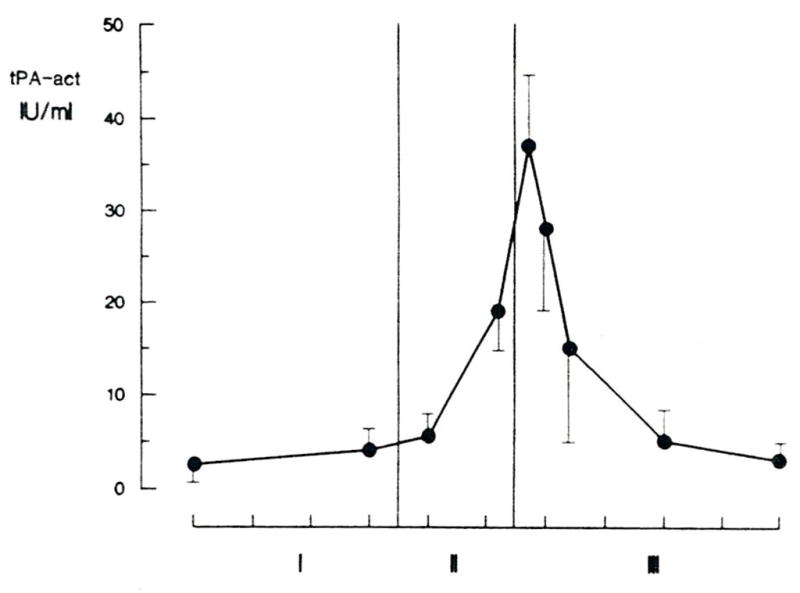
Tissue-type plasminogen activator activity during liver transplantation (n = 20). Blood samples were taken after induction of anesthesia, 30 minutes before the anhepatic stage, 10 minutes into the anhepatic stage, 5 minutes before reperfusion, 5 minutes, 30 minutes, 90 minutes, and 180 minutes after reperfusion, and at the end of the procedure.
DISCUSSION
It was demonstrated that orthotopic liver transplantation is associated with a high increase of plasma levels of tPA activity. A combination of increased release and reduced hepatic clearance may explain the initial increase during the anhepatic stage. This view is supported by the lack of fibrinolysis activation during auxiliary liver transplantation.3 An “explosive” increase in tPA activity occurred immediately after reperfusion. This is in agreement with the clinical findings of generalized oozing and increased blood loss during this period,2 and suggests a release of tPA from the donor liver. In a recent small study, increased plasma levels of tPA occurred primarily during the anhepatic stage of orthotopic liver transplantation.4 Since we observed an extreme increase in tPA activity only during a short period after reperfusion, this peak could have been missed if no blood samples were taken within 10 minutes after reperfusion. Although the systemic increase in tPA activity is transient, the clinical effect may extend over a considerably longer period, as tPA may bind to fibrin and become incorporated in newly formed hemostatic clots, resulting in early lysis and insufficient hemostatic function.
References
- 1.Groth CG. In: Experience in Hepatic Transplantation. Starzl TE, Putman CW, editors. Philadelphia: WB Saunders; 1969. p. 159. [Google Scholar]
- 2.Kang YG, Martin DJ, Marquez J, et al. Anesth Analg. 1985;64:888. [PMC free article] [PubMed] [Google Scholar]
- 3.Porte RJ, Knot EAR, de Maat MPM, et al. Fibrinolysis. 1988;2(suppl 3):67. [Google Scholar]
- 4.Dzik WH, Arkin CF, Jenkins RL, et al. Blood. 1988;71:1090. [PubMed] [Google Scholar]


