Abstract
My assigned task today is to provide a history of liver transplantation in pediatric patients. The history is a relatively brief one, not much more than 25 years in duration. The seeds for the liver trials were planted in the laboratory in 1958 and 1959, with resulting descriptions of the operation and of the pathological changes caused by rejection. These quite extensive studies were completed before chemical immunosuppression was a reality.1–3
IMMUNOSUPPRESSION AND KIDNEY TRANSPLANTATION
Such immunosuppression was first tested in patients after the far more simple operation of renal transplantation. The drugs that were used throughout the years included azathioprine alone,4 azathioprine plus prednisone5 to which antilymphocyte globulin (ALG) could be added as an adjunct,6 and more recently, cyclosporine (CsA) alone7 or with steroids8 and/or monoclonal ALG.9 The most important immunosuppressive programs of the last 25 years are summarized in Table 1.
Table 1.
The Principal Developments in Immunosuppression, Developed With Kidney Transplantation and Applied to the Liver
In the early 1960s when renal transplantation was first tried in any numbers, few children were included except at our own center at the University of Colorado. One of the pediatricians there who had sent us an 8-year-old girl for renal transplantation witnessed so much morbidity in his own patient that he wrote a thoughtful editorial in the Journal of Pediatrics in 1964 that questioned deeply whether such endeavors should be allowed to go forward.10 One of his principal concerns was that with the necessity for long-term high-dose steroid therapy (combined with azathioprine), normal growth could not be expected. As it turned out, Dr Riley’s little patient is today a practicing physician, and many other renal recipients of that era are still alive and well. It was not until 5 or 6 years later that it was realized that catch-up growth in many such children could be expected, especially if living related donors had been used with the consequent ability to greatly reduce steroid therapy for long-term maintenance.11
In 1966, the first systematic application of renal transplantation in children was described in Pediatric Clinics of North America12 In that article, it was noted in a general sense that
the greatest application of whole organ transplantation may prove to be in the field of pediatric medicine, in which the progression of disease is often due to failure of a single organ system. Under these circumstances the provision of good renal or hepatic or cardiac function might be expected to restore normal health. In adult patients comparable problems are frequently and sometimes unexpectedly complicated by disorders other than those to which treatment was originally directed.
The results with renal transplantation were so striking that many other centers began similar efforts, most notably at the Medical College of Virginia where Hume worked.13
In the same Pediatric Clinics article, a brief notation was made about the possibility of liver transplantation as follows:
It has been natural to think of extending comparable replacement therapy to diseases which result in functional failure of other organs. At present, liver transplantation appears to offer the most immediate possibility of clinical utility. Such hope derives principally from studies in dogs.
THE FIRST LIVER TRIALS
Such optimism might have seemed excessive at that time since seven known clinical attempts at liver transplantation had already been made, five in Denver14 and one each subsequently in Boston and in Paris, all unsuccessful. However, the basis for hope was demonstrable in a large series of dogs given nonrelated mongrel livers in 1963 and 1964 who had survived for more than 4 postoperative months and whose therapy with azathioprine was then stopped.15 A number of these dogs lived for long subsequent periods,16 and one died of old age more than a decade later.
On July 23, 1967, a 19-month-old child with a large hepatoma was treated with liver replacement. Although she died 13 months later of metastases from the original malignancy, she provided the first prolonged survival after orthotopic liver transplantation.17 During the next 13 years, many additional examples of prolonged survival came from the Colorado program18 and from other centers, most notably the Cambridge University and Kings College (London) consortium.19 One of our patients from that era is the longest survivor in the world today, more than 17 years postoperative.
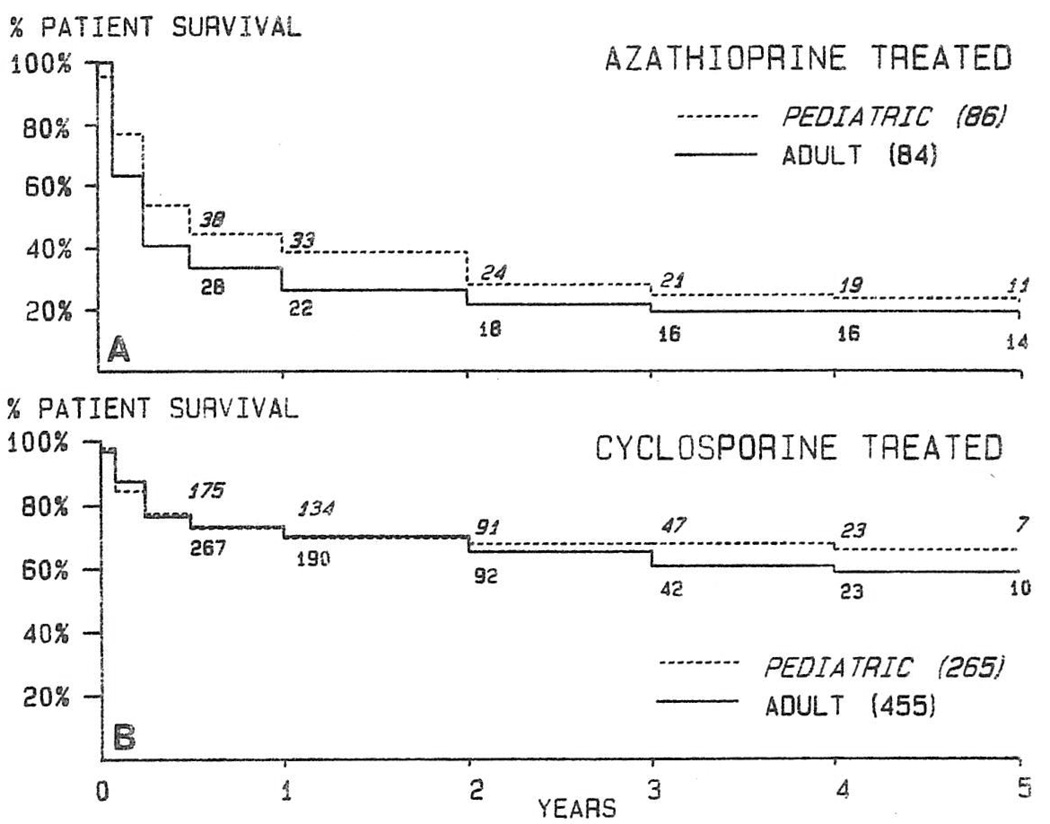
However, during any time period between 1967 and 1980, between three fourths and half of all recipients of livers died during the first postoperative year.18 These discouraging results were not appreciably improved with the acquisition of more experience. The most encouraging results were in children who throughout the years had a slight survival advantage both early and long after transplantation (Fig 1A).
Fig. 1.
Total experience with orthotopic liver transplantation of 170 patients from 1963 to 1979 (A) and of 720 patients from 1980 to 1986 (B). Note the slight survival advantage of the pediatric recipients in both eras. Case accrual in the CsA era was until August 31, 1986, and follow-ups were to October 31, 1986.
There were a number of reasons for the poor results from 1967 through 1979 including uncertainty about the best method of biliary tract reconstruction, the commission of numerous technical errors, the use of livers before 1968 and 1969 from donors under other than brain death conditions, and the tendency to assume without ruling out other causes that rejection was always responsible for hepatic dysfunction in the posttransplantation period. However, the principal problem was that the immunosuppressive regimens used up to 1980 had little or no margin of safety in the context of liver transplantation.
THE INFLUENCE OF CsA
In 1976, Borel and his associates described the remarkable new immunosuppressive agent CsA.20 The subsequent clinical trials with this drug and its eventual marriage with steroids in a modern-day, double-drug program had a revolutionary effect on liver transplantation.18 The one year survival more than doubled almost overnight, an advantage which has continued for at least the first 5 postoperative years (Figure 1B).
Since the introduction of CsA, a further refinement in immunosuppression has been the clinical use of monoclonal anti-T lymphocyte antibodies9,21 manufactured with the hybridoma technique of Kohler and Milstein.22 The monoclonal ALGs produced with this method are many times more powerful than the older polyclonal preparations, and they are being used most commonly to reverse established rejection.9,21
TECHNICAL REFINEMENTS
For children, the most important change in technique through the years was the standardization of bile duct reconstruction. In more than three fourths of pediatric cases, the recipient common duct is absent (biliary atresia) or too small to permit duct-to-duct reconstruction. Consequently, the most common procedure is duct-to-jejunal anastomosis after construction of a Roux limb.18 It is astonishing how this simple conclusion required so much time for final delineation, but until then one of the principal causes of failure was biliary tract obstruction or bile fistula formation postoperatively.
During the removal of the diseased native liver and the sewing-in of the new organ, occlusion of the systemic and splanchnic venous circulations can lead to such severe venous hypertension that all aspects of the operation are in a crisis atmosphere. Decompression of these pools with venovenous bypass techniques has made the operation of liver transplantation a more easily taught conventional procedure in adults.18,23,24
Increasingly, the venovenous bypass techniques have made their way into the pediatric hospital. Initially, it was thought that a minimum bypass flow of 1,000 mL/min would be necessary before the heparin-free venovenous bypasses would be safe. However, lower-flow bypasses have been complication free, and it is our present policy to use bypasses for all children over 15 kg.
Today, the most common technical complications in small recipients are of the vascular anastomoses, especially of the artery. Hepatic artery thrombosis is second only to rejection as a cause for retransplantation in infants.
THE ORGAN PROCUREMENT PROBLEM
The multiple-organ procurement techniques developed in the early 1980s have become standard worldwide.25 With the original technique, meticulous dissection of the hepatic hilum was carried out before infusions were begun in situ with cold solutions. In a more recent modification, the hilar dissection has been omitted, and all of the hilar preparation is done on the back table.26 Removal of the heart, kidneys, and liver can be completed in 30 to 60 minutes.
Pediatric recipients, particularly very small ones, still die because of the lack of small donors. The possibility of reducing livers from larger donors by a partial hepatic resection has been extensively examined in the Catholic University of Louvain program by Dr Jean Otte. The most common procedure has been to remove the lateral segment of the left lobe for transplantation and discard the full right lobe or more. Although such procedures of transplanting partial hepatic remnants have been described before, the Belgium team has acquired the most extensive and encouraging experience.
It is possible that the criteria for acceptance of pediatric donors are too inflexible, with consequent wastage of organs. In a recent retrospective study of our Pittsburgh cases in which donors were thought to be good, bad, or poor on the basis of liver function test results, blood gas determinations, and cardiocirculatory status, there was no correlation between the outcome of the recipient and the quality classification of the donor.27 Our conclusion has been that there is almost no such thing as a poor pediatric donor.
FACTORS IN SURVIVAL
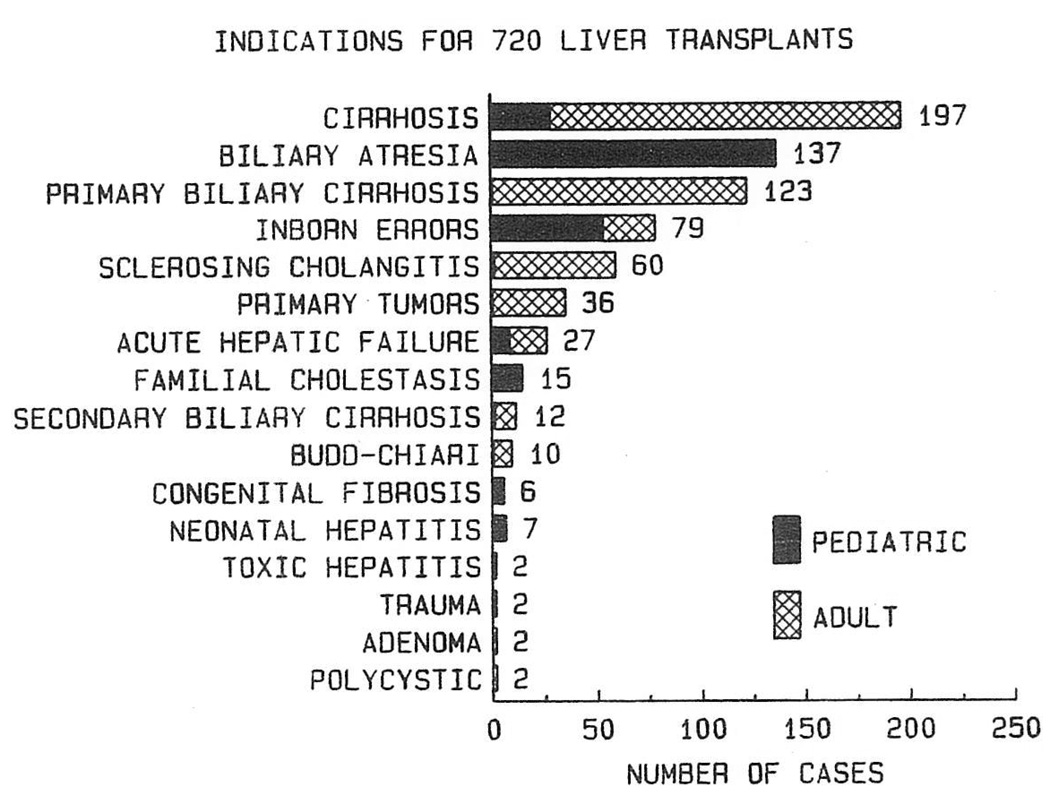
Throughout the history of liver transplantation, a slight (and frequently statistically insignificant) advantage has been enjoyed by the pediatric recipient (Fig 1). Since 1980, the 5-year actuarial survival rate of children has been just below 70%, marginally better than in adults. Most of the difference was accounted for by inclusion in the adult series of two diseases, chronic active hepatitis caused by B virus and malignant tumors, which have a high rate of recurrence after transplantation28 (Fig 2).
Fig. 2.
Diseases in 720 patients that led to liver replacement during 1980 to 1986. Note that malignant tumors and chronic active hepatitis were not heavily represented in the children. These latter diagnoses have carried a bad posttransplant prognosis in adults because of a high rate of recurrence of the original disease.
In children, there have been no “bad diseases” (Fig 3), and so far, there have been no recurrences of original diseases. However, the poorest results have been with biliary atresia. With biliary atresia, the 5-year survival rate is projected at 64%, compared with almost ten percentage points higher than this for the other common pediatric diseases (Fig 3). The reason is the great difficulty of treating patients with biliary atresia after extensive prior operations for the performance of portoenterostomy or revisions of such procedures.
Fig. 3.
Five-year actuarial survival rates of pediatric recipients with the most frequent diagnoses who were treated in the CsA era.
The age of the recipient has proved to be the single most important prognostic factor in pediatric liver transplantation. Our own experience with recipients of tiny size has been somewhat discouraging. Through June 1986 we have performed transplants on 20 patients weighing 5.2 to 9.7 kg.29 The ages of these recipients were 3 to 11 months, and all were profoundly ill. Otherwise, they would have been permitted to grow to a more advantageous size. Eight of the 20 recipients have died, including seven deaths in the early post-operative period and one late death from aspiration. Technical problems were frequent. Hepatic artery thrombosis occurred in five patients, but only one death was related to this complication. Three of these patients have received retransplants. One patient is stable and being allowed to grow before retransplantation will be done. Other technical problems included defects of biliary tract reconstruction and multiple intestinal perforations from earlier futile portoenterostomies.
Encouraging as the overall results have been, the outlook would be less optimistic by about 20% without the frequent application of retransplantation. 18,l3 Thus, retransplantation has become one of the most common indications for hepatic replacement.
SUMMARY
Liver transplantation, which once was an experimental procedure of no practical interest, has become the preferred treatment for infants and children dying of almost all non-neoplastic end-stage liver diseases. Liver replacement is being provided by many well-trained teams on all of the continents, as is evident from the program today—the first international symposium on pediatric liver transplantation. I have been honored in giving the first paper in the process of introducing the remarkable work of a gifted younger generation of physicians and surgeons.
Acknowledgments
Supported by Research Project Grant AM-29961 from the National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Starzl TE, Kaupp HA, Brock DR, et al. Surg Gynecol Obstet. 1960;111:733. [PMC free article] [PubMed] [Google Scholar]
- 2.Moore FD, Wheeler HB, Demissianos HV, et al. Ann Surg. 1960;152:374. [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Kaupp HA, Brock DR, et al. Surg Gynecol Obstet. 1961;112:135. [PMC free article] [PubMed] [Google Scholar]
- 4.Murray JE, Merrill JP, Harrison JH, et al. N Engl J Med. 1963;268:1315. doi: 10.1056/NEJM196306132682401. [DOI] [PubMed] [Google Scholar]
- 5.Starzl TE, Marchioro TL, Waddell WR. Surg Gynecol Obstet. 1963;117:385. [PMC free article] [PubMed] [Google Scholar]
- 6.Starzl TE, Marchioro TL, Porter KA, et al. Surg Gynecol Obstet. 1967;124:301. [PMC free article] [PubMed] [Google Scholar]
- 7.Calne RY, Rolles K, White DJG, et al. Lancet. 1979;2:1033. doi: 10.1016/s0140-6736(79)92440-1. [DOI] [PubMed] [Google Scholar]
- 8.Starzl TE, Weil R, III, Iwatsuki S, et al. Surg Gynecol Obstet. 1980;151:17. [PMC free article] [PubMed] [Google Scholar]
- 9.Fung JJ, Demetris AJ, Porter KA, et al. Nephron. 1987 doi: 10.1159/000184431. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riley CM. J Pediatrics. 1964;65:797. [Google Scholar]
- 11.Lilly JR, Giles G, Hurwitz R, et al. Pediatrics. 1971;47:548. [PMC free article] [PubMed] [Google Scholar]
- 12.Starzl TE, Marchioro TL, Porter KA, et al. Pediatr Clin North Am. 1966;13:381. doi: 10.1016/s0031-3955(16)31843-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams GM, Lee HM, Hume DM. Transplant Proc. 1969;1:262. [PubMed] [Google Scholar]
- 14.Starzl TE, Marchioro TL, Von Kaulla KN, et al. Surg Gynecol Obstet. 1963;117:659. [PMC free article] [PubMed] [Google Scholar]
- 15.Starzl TE, Marchioro TL, Porter KA, et al. Surgery. 1965;58:131. [PMC free article] [PubMed] [Google Scholar]
- 16.Starzl TE. with the assistance of Putnam CW): Experience in Hepatic Transplantation. Philadelphia: Saunders; 1969. [Google Scholar]
- 17.Starzl TE, Groth CT, Brettschneider L, et al. Ann Surg. 1968;168:392. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Hepatology. 1982;2:614. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calne RY, Williams R. Curr Probl Surg. 1979;16:3. doi: 10.1016/s0011-3840(79)80004-0. [DOI] [PubMed] [Google Scholar]
- 20.Borel JF, Feurer C, Gubler HU, et al. Agents Actions. 1976;6:468. doi: 10.1007/BF01973261. [DOI] [PubMed] [Google Scholar]
- 21.Cosmi AB, Colvin RB, Burton RC, et al. N Engl J Med. 1981;305:308. doi: 10.1056/NEJM198108063050603. [DOI] [PubMed] [Google Scholar]
- 22.Kohler G, Milstein C. Nature. 1975;256:495. doi: 10.1038/256495a0. [DOI] [PubMed] [Google Scholar]
- 23.Shaw BW, Jr, Martin DJ, Marquez JM, et al. Ann Surg. 1984;200:524. doi: 10.1097/00000658-198410000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Starzl TE, Iwatsuki S, Esquivel CO, et al. Semin Liver Dis. 1985;5:349. doi: 10.1055/s-2008-1040632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Starzl TE, Hakala TR, Shaw BW, Jr, et al. Surg Gynecol Obstet. 1984;158:223. [PMC free article] [PubMed] [Google Scholar]
- 26.Starzl TE, Miller C, Broznick B, et al. Surg Gynecol Obstet. 1987 in press. [PMC free article] [PubMed] [Google Scholar]
- 27.Makowka L, Gordon RD, Todo S, et al. Transplant Proc. 1987;19:2378–2382. [PMC free article] [PubMed] [Google Scholar]
- 28.Starzl TE, Iwatsuki S, Shaw BW, Jr, et al. Semin Liver Dis. 1985;5:334. doi: 10.1055/s-2008-1040630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Esquivel CO, Koneru B, Karrer F, et al. J Pediatrics. 1987;110:545–548. doi: 10.1016/s0022-3476(87)80545-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw BW, Jr, Gordon RD, Iwatsuki S, et al. Semin Liver Dis. 1985;5:394. doi: 10.1055/s-2008-1040638. [DOI] [PMC free article] [PubMed] [Google Scholar]