Abstract
BACKGROUND:
Percutaneous coronary intervention (PCI) with coronary stenting is a common medical procedure that is used to treat the symptoms of both stable angina and acute coronary syndromes. Drug-eluting stents (DES) decrease restenosis and repeat revascularization procedures but are more expensive than bare-metal stents. A proper cost-effectiveness analysis of DES requires an understanding of the health value patients place on the avoidance of restenosis accompanied by a repeat PCI.
OBJECTIVE:
To estimate quality-of-life (QoL) benefits ascribed to avoiding the return of coronary symptoms and the need for a repeat revascularization procedure.
METHODS:
A prospective, single-centre study was conducted involving PCI patients. A time trade-off (TTO) question, based on a hypothetical restricted lifespan of 10 years, was used to estimate the QoL benefits patients attach to the avoidance of recurrent symptoms and a repeat PCI. This was accomplished by interviewing the patients by telephone, two weeks post-PCI. The TTO question was also administered to the catheterization laboratory staff.
RESULTS:
Between January and March 2007, and between April and June 2008, 103 interviews were completed. The median TTO was zero weeks (interquartile range zero to 1.7 weeks). Six interventional cardiologists and eight cardiac catheterization nurses reported a similar median disutility.
CONCLUSION:
Despite acknowledgement of the substantial clinical benefits of DES, the results of the present study suggest that patients do not place a great disutility on avoiding restenosis, thereby providing little QoL justification for the large incremental cost associated with this technology.
Keywords: Angioplasty, Quality of life, Restenosis
Abstract
HISTORIQUE :
L’intervention coronaire percutanée (ICP) accompagnée d’une endoprothèse coronaire est souvent utilisée pour traiter des symptômes d’angine stables et des syndromes coronariens aigus. Les endoprothèses à élution de médicament (EEM) réduisent l’apparition d’une resténose et la reprise des interventions de revascularisation mais sont plus coûteuses que les endoprothèses à métal nu. Pour effectuer une analyse coût-efficacité convenable des EEM, il faut comprendre la valeur pour leur santé que les patients accordent à éviter une resténose et une reprise de l’ICP.
OBJECTIF :
Évaluer les bienfaits sur la qualité de vie (QdV) attribués à éviter la réapparition des symptômes coronariens et le besoin d’une nouvelle intervention de revascularisation.
MÉTHODOLOGIE :
Les chercheurs ont mené une étude monocentrique prospective auprès de patients ayant subi une ICP. Une question sur les compromis dans le temps (CDT), fondée sur une diminution hypothétique de l’espérance de vie de dix ans, a permis d’évaluer les bienfaits sur la QdV que les patients accordent à éviter la récurrence des symptômes et la reprise de l’ICP. Pour ce faire, les chercheurs ont procédé à une entrevue téléphonique des patients, deux semaines après l’ICP. La question sur les CDT a également été posée au personnel du laboratoire de cathétérisme.
RÉSULTATS :
Entre janvier et mars 2007 et entre avril et juin 2008, 103 entrevues ont été effectuées. Le CDT médian était de zéro semaine (plage interquartile de zéro à 1,7 semaine). Six cardiologues interventionnistes et huit infirmières en cathétérisme cardiaque ont déclaré une désutilité médiane similaire.
CONCLUSION :
Même si on tient compte des bienfaits cliniques marqués de l’EEM, les résultats de la présente étude indiquent que les patients n’accordent pas une grande désutilité à l’évitement d’une resténose. Ainsi, la QdV justifie peu le coût incrémentiel important associé à cette technologie.
Percutaneous coronary intervention (PCI) is a common medical procedure with approximately 50,000 performed annually in Canada and 1,000,000 in the United States. PCI is used to treat the symptoms of both chronic angina and acute coronary syndromes. Coronary stenting has become the predominant PCI technique, although the health benefits of a systematic use of coronary stents over a restrained provisional stenting policy appear to be small (1). The main advantage of coronary stenting is a reduction in restenosis rates compared with plain old balloon angioplasty. Bare-metal stents (BMS) have mitigated but not eliminated restenosis, which is caused by elastic recoil of the vessel wall, remodelling of the vessel and neointimal proliferation. In an attempt to decrease the risk of restenosis further, drug-eluting stents (DES) were developed. These coated stents elute drugs that are either immune suppressants (eg, sirolimus) or antimitotics (eg, paclitaxel), thereby reducing neointimal proliferation by suppressing inflammation or decreasing local cell division.
Numerous studies show that DES substantially decrease angiographic restenosis and the need for repeat revascularization procedures compared with BMS (2–5). However, no differences in mortality and myocardial infarctions have been observed (6–9), and there is conflicting evidence regarding the long-term safety of DES (10–13). DES do substantially decrease restenosis rates and the need for subsequent revascularization (6–9). Results from cost-effectiveness studies are also conflicting (14) and are due, in part, to the lack of an unbiased measure of the health benefit that patients associate with an absence of coronary restenosis. Most studies express the costs associated with DES per avoided event (8,14,15). These measures render comparative analyses difficult, thereby complicating decision making by policy-makers.
Quality-of-life (QoL) measures, although not without their limits, do provide decision makers with common utilities that are comparable for any treatment. QoL measures not only implicitly recognize the health benefits of extended survival but also of avoided morbidity. The reduction in QoL from perfect health is also referred to as a disutility. The objective of the present study was to estimate patient perspective QoL benefits ascribed to the avoidance of symptomatic coronary restenosis following PCI.
METHODS
A cross-sectional study was performed using the preference-based measure time trade-off (TTO) as an estimate of the value associated with an avoidance of recurrent symptoms and an additional revascularization procedure.
Study population
Over two 10-week periods – January to March 2007, and April to June 2008 – PCI patients at the McGill University Health Centre in Montreal, Quebec, were recruited. Patients were eligible if they underwent a PCI for chronic or stable angina, unstable angina or non-ST segment elevation myocardial infarction. Exclusion criteria were high-risk clinical acuity including primary PCI or serious PCI complication, previous PCI less than one year ago, cognitive impairment, delirium, hearing and/or visual disabilities, or inability to converse in English or French.
The schedule in the cardiac catheterization unit was consulted daily to identify consecutive eligible subjects. After the procedure, a catheterization nurse who was independent of the study team verified whether the patient was stable and willing to be contacted by a member of the research team. The study was explained to each patient who was willing to be contacted. Those who verbally expressed interest in the study were given a package to take home, which included a descriptive pamphlet, the study questionnaire and the consent form, which was later returned to the study coordinator. Patients were called within three to four days to schedule an appointment for the QoL interview. As close as possible to 14 days post-PCI, a trained interviewer telephoned the patient and completed the questionnaire. Because the patients had the questionnaire in their packages, they could read along with the interviewer. The interview took approximately 15 min to complete. To provide a comparison with the patient population, the questionnaire was also administered individually to health care professionals with an in-depth understanding of the risks and benefits of this technology (six interventional cardiologists and eight full-time catheterization nurses). The study was approved by the research ethics board of Royal Victoria Hospital (Montreal).
Measurement
Demographic and clinical information was obtained from the patient’s medical charts. Lesion severity (classified according to the American College of Cardiology guidelines), severity of the stenosis, vessel size and patient stability were recorded by the interventionalist. Also, following recruitment, the recruiter scored the level of health using a five-point scale. The interview included questions about educational level, financial situation, severity of coronary symptoms and personal experience with the PCI intervention. Patients were also asked to rate their own health status on a scale from 1 to 100. QoL was measured by TTO. An advantage of TTO is its ability to be directly converted to quality-adjusted life years (QALYs).
A TTO question (16) was used to measure preferences for a health state. Subjects were asked how much time of living in a suboptimal health state they were willing to sacrifice to live in perfect health. In this study, patients were asked to imagine a situation in which they only had 10 years to live and where a repeat angioplasty procedure is required within six months because the symptoms had returned. The phrase ‘within six months’ was included because the goal was to measure the disutility of restenosis, which is generally accepted to occur within the first six months following a PCI (17). The specific study question was, “If there was a possibility to avoid a return of symptoms and the need for a repeat procedure by giving up some of these make-believe 10 years, how many of these make-believe 10 years would you be willing to give up to avoid a return of symptoms and the need for a repeat procedure within 6 months?”
If patients declined to trade off any years, they were asked if they would be willing to sacrifice any months or weeks of their imaginary 10-year lifetime. This study question was preceded by two other TTO questions to increase the respondents’ familiarity with the concept; the situations for these questions were ‘being in chronic pain and bedridden’ and ‘wearing glasses’. These questions were used to assess the study subject’s comprehension of this process because it was reasonable to anticipate that there would be no TTO for wearing glasses but a substantial TTO for being in chronic pain and bedridden. After answering these trial questions, the participants’ responses were discussed with the study team to optimally prepare them for the research question. (For the last 60 patients, their responses to these two preparatory questions were recorded. As expected, the median TTO was 0.0 years and 5.0 years for wearing glasses and being bedridden, respectively, indicating good comprehension of the TTO activity even before discussion of these sample questions.)
Finally, study subjects were presented with a list of common medical procedures along with their costs and were asked where they would place a coronary angioplasty.
Statistical analysis
Continuous data are presented either as means ± SDs or, in the case of skewed distributions, as medians with interquartile ranges (IQRs). Categorical outcome variables are reported as frequencies. TTO outcomes are presented with descriptive characteristics as well as a frequency distribution. Univariate analysis was performed to explore differences between the first and second period of data collection, between interviews conducted in French and English, and between PCI patients who did and did not participate in the interview. The disutility was calculated as the number of years a patient was willing to trade off divided by 10.
TTO outcomes were dichotomized at the median value (zero years versus more than zero years) and logistic regression was performed to examine any explanatory associations. Variables that were considered included demographic variables (sex, age, language, and educational, financial and marital status), clinical variables (previous procedure, diabetes, high blood pressure, dyslipidemia, stenosis and symptom severity), procedural variables (American College of Cardiology lesion severity, stable during the procedure, femoral versus radial approach, number of stents and stress of the procedure) and other variables (date of the interview, recruiter’s perception of health status, preliminary TTO responses and self-rated health). Each variable was tested separately using logistic regression and variables that had a P<0.15 were included in a multivariate logistic regression model. The analysis was performed using SAS version 9.1 (SAS Institute Inc, USA).
RESULTS
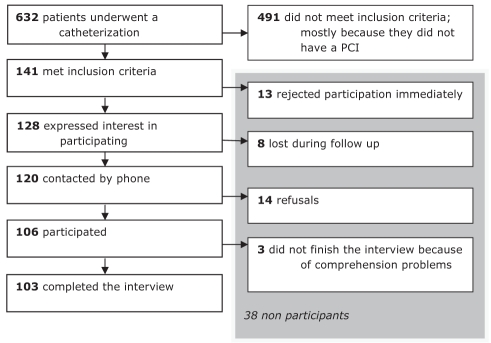
In total, 632 patients underwent a PCI procedure during the two study periods, of which, 141 met the study’s inclusion criteria. Of these 141 patients, 103 subjects completed the interview. The schematic flow of the patient recruitment is displayed in Figure 1. The median time to interview completion was 14 days (IQR 14 to 15 days). A general description of the population can be found in Table 1. The mean (± SD) age of the study population was 61.9±11.0 years; 74 participants were men and approximately one-half of the subjects spoke French. Most patients were stented with a BMS (66%), 34 had undergone a previous PCI or a coronary artery bypass graft surgery more than one year previously, and 57% suffered from hypertension, 38% from diabetes and 53% from dyslipidemia. Table 1 also provides a basic description of the nonparticipants, who resembled participants, except for being an average of 5.5 years older. Additionally, there was a trend toward increased male participation. There were no statistically significant differences in basic demographic and outcome measures between the subjects recruited in 2007 and those recruited in 2008, or between interviews conducted in English or French (data not shown).
Figure 1).
Schematic representation of patient recruitment. PCI Percutaneous coronary intervention
TABLE 1.
Population characteristics
| Variable | Participants (n=103) | Nonparticipants (n=38) | P |
|---|---|---|---|
| Male sex | 74 (72) | 21 (55) | 0.0624 |
| Age, years, mean ± SD | 61.9±11.0 | 67.4±12.1 | 0.0112 |
| Language (French) | 51 (49) | ||
| Live with spouse | 71 (69) | ||
| Educational level | |||
| Completed high school | 78 (78)* | ||
| Have taken university courses | 32 (32)* | ||
| Current procedure | 0.100 | ||
| PCI with BMS | 68 (66) | 22 (67)† | |
| PCI with DES | 26 (25) | 6 (18)† | |
| PCI with both | 8 (8) | 2 (6)† | |
| PCI without stent | 1 (1) | 3 (9)† | |
| Previous procedure | 0.0905 | ||
| PCI or CABG >1 year ago | 34 (33) | 7 (18) | |
| Comorbidities | |||
| Hypertension | 59 (57) | 27 (71) | 0.1369 |
| Diabetes | 39 (38) | 10 (26) | 0.2013 |
| Dyslipidemia | 55 (53) | 19 (50) | 0.7200 |
| Treatment | |||
| Stable during PCI | 77 (79)‡ | 23 (68)§ | 0.1660 |
| Lesion severity (% of lumen blocked) | 88 | 88 | 0.9611 |
| Number of stents¶ | 1.9±1.3 | 1.7±1.6 | 0.5325 |
| Time to interview, days post-PCI, median (IQR) | 14 (14–15) | ||
Data presented as n (%) unless otherwise indicated.
Data from three participants are missing;
Data from five participants are missing;
Data from six participants are missing;
Data from four participants are missing;
Data presented as mean ± SD. BMS Bare-metal stent; CABG Coronary artery bypass graft; DES Drug-eluting stent; IQR Interquartile range; PCI Percutaneous coronary intervention
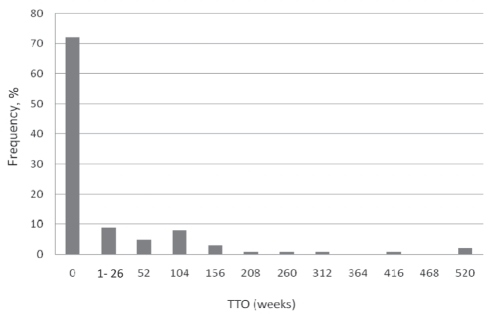
The distribution of the TTO question can be found in Figure 2; the median TTO was zero weeks (IQR zero to 1.7 weeks). Converted to QALYs, this represents a median disutility of zero years for restenosis and the need for a repeat vascularization. In comparison, among the 14 specialized health care workers, there was also a median willingness to exchange zero life years to avoid restenosis and a repeat PCI (13 of 14 reported a TTO of zero years). No statistically significant associations were observed to explain the dichotomized TTO (zero versus more than zero years) outcome.
Figure 2).
Distribution of time trade-off (TTO) for the need for a repeat percutaneous coronary intervention within six months (n=103)
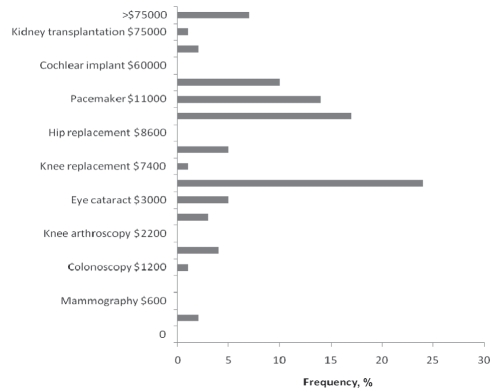
Finally, patients were asked to value angioplasty by benchmarking it on a list of commonly used medical procedures (Figure 3). The answers varied from less than $600 (cheaper than a mammography) to more than $75,000 (indicating a value higher than a kidney transplantation).
Figure 3).
Distribution of the monetary value patients assigned to a percutaneous coronary intervention compared with other procedures (n=96; seven patients were unable to answer)
DISCUSSION
The present study suggests that restenosis requiring a repeat PCI procedure, as assessed by direct patient questioning using the TTO approach, was not viewed as a major health outcome by the majority of patients who assigned it a negligible disutility. There was some variability in the TTO responses with a small minority of outliers, but we were unable to identify any explanatory variables. Nevertheless, overall, there was general consistency in the TTO results because 70% of the subjects were unwilling to trade off any time for the avoidance of symptomatic restenosis.
A natural first question is whether these results mean that most participants did not understand what they were supposed to be doing during the interview, or that patients did not highly value the health benefits associated with avoiding restenosis following PCI. However, patients were able, in general, to approximately estimate the financial cost of PCI relative to other procedures, suggesting that they understood the overall process. Interestingly, experienced cardiac personnel shared a similar view to the majority of patients regarding the disutility of restenosis and accompanying PCI, which also lends support to the latter hypothesis.
Nevertheless, patients did have some difficulties in understanding and articulating the complex concepts of value preferences. This became more evident when financial benchmarking of repeat angioplasty was examined. The Canadian publicly funded health care system does not expose people to actual medical costs, which may help to explain the variability of the benchmark responses. When patients were asked to place a value on a PCI in comparison with other procedures, there was some variability in their answers, confirming that a minority of patients do have difficulty in relating costs to health care procedures and benefits.
The present study was the first to directly estimate the impact of restenosis by providing QoL information based on individual patient preferences and, hence, makes a unique contribution to the existing literature. Until now, only a few studies (18–20) using indirect methods have addressed this issue. For example, QoL has been measured one-year post-PCI, and the difference in QALYs between patients who did and did not have restenosis was calculated retrospectively and assumed to be totally attibuted to restenosis. Obviously, other factors could be contributing to these differences and, indeed, as expected, the observed disutilities (0.06 [19] and 0.08 [20]) were greater than what we observed. A second indirect method calculated the difference between the QoL associated with angina and angina-free states, and then multiplied them by the wait and recovery times. This approach has been applied by two health technology assessment agencies. The United Kingdom National Institute for Health and Clinical Excellence (8) estimated the impact to be 0.024, accounting for a six-week waiting time. The Belgian Federaal Kenniscentrum voor de Gezondheidszorg (21) assessment used a disutility of approximately 0.018 for restenosis, based on a waiting time of four weeks. These health technology assessment reports assume that the restenosis symptoms equate to those of chronic stable angina. They do have the advantage of explicitly allocating waiting times but, in many clinical contexts, restenosis is treated promptly so that this advantage may be somewhat moot.
The median disutility found in the present study was lower than the studies described above. Possible reasons include different patient populations, different cultural perceptions or different methodological approaches. One strength of our study was the direct approach used and the unselected patient population addressed.
Limitations
One limitation of the present study was our deliberate simplification of the TTO question. We ignored the reality that DES does not eliminate restenosis but only reduces it by approximately 75% (7) and implied that an intervention existed that would completely eliminate the chance of all restenosis, recurrent symptoms and revascularization in the first six months post-PCI. However, this limitation would tend to bias our results toward an overestimation of the value of DES to reduce this outcome. Because the QoL concept is dependent on the context within which it is presented, a more realistic and detailed question may have been appropriate, but the increased complexity may have hindered its comprehension. Despite the simplified approach, we suspect that a minority of the patients had comprehension problems (compare the four outliers in Figure 2 willing to trade off more than five years of their life to avoid a transient episode of restenosis). Another limiting factor is that the results were based on a single-centre study – confirmatory studies from other centres are definitely required. Also, the number of subjects studied was relatively small. Finally, although the empirical literature favours TTO to reflect the strengths of preference for health states, it is recognized that patients are often unwilling to make a sacrifice in the valuation task (17). This TTO limitation may be present in our study because more than one-half of the patients were not willing to trade off any years, months or weeks of their lifespan.
The measurement of health benefits is necessary for the full appreciation of the value of medical technologies. The present study demonstrates that preference-based measures require a precise approach and are difficult to obtain in clinical studies. It also demonstrates that QoL is a complex concept for patients to quantify. Nevertheless, we were able to estimate the QoL value that PCI patients associate with an avoidance of a return of symptoms and a repeat revascularization procedure. Although DES have demonstrated substantial clinical benefits with a reduction in restenosis rates, the present study suggests that both patients and health care workers do not place a great disutility on this health outcome. Therefore, there seems to be little QoL justification for the large incremental cost attached to these devices.
Footnotes
FUNDING: Dr Brophy is a research scholar supported by le Fonds de la Recherche en Santé du Québec (Montreal, Quebec). Marleen Ploegmakers received financial support from the Dutch Heart Foundation.
REFERENCES
- 1.Brophy JM, Belisle P, Joseph L. Evidence for use of coronary stents. A hierarchical bayesian meta-analysis. Ann Intern Med. 2003;138:777–86. doi: 10.7326/0003-4819-138-10-200305200-00005. [DOI] [PubMed] [Google Scholar]
- 2.Morice MC, Serruys PW, Sousa JE, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002;346:1773–80. doi: 10.1056/NEJMoa012843. [DOI] [PubMed] [Google Scholar]
- 3.Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349:1315–23. doi: 10.1056/NEJMoa035071. [DOI] [PubMed] [Google Scholar]
- 4.Schampaert E, Cohen EA, Schluter M, et al. The Canadian study of the sirolimus-eluting stent in the treatment of patients with long de novo lesions in small native coronary arteries (C-SIRIUS) J Am Coll Cardiol. 2004;43:1110–5. doi: 10.1016/j.jacc.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Schofer J, Schluter M, Gershlick AH, et al. Sirolimus-eluting stents for treatment of patients with long atherosclerotic lesions in small coronary arteries: Double-blind, randomised controlled trial (E-SIRIUS) Lancet. 2003;362:1093–9. doi: 10.1016/S0140-6736(03)14462-5. [DOI] [PubMed] [Google Scholar]
- 6.Indolfi C, Pavia M, Angelillo IF. Drug-eluting stents versus bare metal stents in percutaneous coronary interventions (a meta-analysis) Am J Cardiol. 2005;95:1146–52. doi: 10.1016/j.amjcard.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 7.Babapulle MN, Joseph L, Belisle P, et al. A hierarchical Bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet. 2004;364:583–91. doi: 10.1016/S0140-6736(04)16850-5. [DOI] [PubMed] [Google Scholar]
- 8.Hill RA, Boland A, Dickson R, et al. Drug-eluting stents: A systematic review and economic evaluation. Health Technol Assess. 2007;11:iii, xi–iii, 221. doi: 10.3310/hta11460. [DOI] [PubMed] [Google Scholar]
- 9.Stettler C, Wandel S, Allemann S, et al. Outcomes associated with drug-eluting and bare-metal stents: A collaborative network meta-analysis. Lancet. 2007;370:937–48. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 10.Laskey WK, Yancy CW, Maisel WH. Thrombosis in coronary drug-eluting stents: Report from the meeting of the Circulatory System Medical Devices Advisory Panel of the Food and Drug Administration Center for Devices and Radiologic Health, December 7–8, 2006. Circulation. 2007;115:2352–7. doi: 10.1161/CIRCULATIONAHA.107.688416. [DOI] [PubMed] [Google Scholar]
- 11.McFadden EP, Stabile E, Regar E, et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet. 2004;364:1519–21. doi: 10.1016/S0140-6736(04)17275-9. [DOI] [PubMed] [Google Scholar]
- 12.Shuchman M. Trading restenosis for thrombosis? New questions about drug-eluting stents. N Engl J Med. 2006;355:1949–52. doi: 10.1056/NEJMp068234. [DOI] [PubMed] [Google Scholar]
- 13.Douglas PS, Brennan JM, Anstrom KJ, et al. Clinical effectiveness of coronary stents in elderly persons: Results from 262,700 Medicare patients in the American College of Cardiology-National Cardiovascular Data Registry. J Am Coll Cardiol. 2009;53:1629–41. doi: 10.1016/j.jacc.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ligthart S, Vlemmix F, Dendukuri N, et al. The cost-effectiveness of drug-eluting stents: A systematic review. CMAJ. 2007;176:199–205. doi: 10.1503/cmaj.061020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuukasjarvi P, Rasanen P, Malmivaara A, et al. Economic evaluation of drug-eluting stents: A systematic literature review and model-based cost-utility analysis. Int J Technol Assess Health Care. 2007;23:473–9. doi: 10.1017/S0266462307070560. [DOI] [PubMed] [Google Scholar]
- 16.Green C, Brazier J, Deverill M. Valuing health-related quality of life. A review of health state valuation techniques. Pharmacoeconomics. 2000;17:151–65. doi: 10.2165/00019053-200017020-00004. [DOI] [PubMed] [Google Scholar]
- 17.Weintraub WS. The pathophysiology and burden of restenosis. Am J Cardiol. 2007;100:3K–9K. doi: 10.1016/j.amjcard.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Groeneveld PW, Suh JJ, Matta MA. The costs and quality-of-life outcomes of drug-eluting coronary stents: A systematic review. J Interv Cardiol. 2007;20:1–9. doi: 10.1111/j.1540-8183.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- 19.Shrive FM, Manns BJ, Galbraith PD, et al. Economic evaluation of sirolimus-eluting stents. CMAJ. 2005;172:345–51. doi: 10.1503/cmaj.1041062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen DJ, Taira DA, Berezin R, et al. Cost-effectiveness of coronary stenting in acute myocardial infarction: Results from the stent primary angioplasty in myocardial infarction (stent-PAMI) trial. Circulation. 2001;104:3039–45. doi: 10.1161/hc5001.100794. [DOI] [PubMed] [Google Scholar]
- 21.Neyt M, Van Brabandt H, Devriese S, et al. Drug Eluting Stents in België: Health Technology Assessment. KCE reports 66A, 2007 [Google Scholar]