Abstract
A 72-year-old woman presented with a decreased level of consciousness and hypotension. The initial electrocardiogram demonstrated atrial fibrillation with a wide QRS complex. Her medical history revealed that she had just been started on propafenone. A diagnosis of propafenone toxicity was made and sodium bicarbonate was administered. A rare phenomenon in which toxicity occurred at therapeutic dosing is reported. Acute propafenone toxicity manifests in a wide range of organ systems; in particular, cardiovascular compromise in the form of hypotension, bradycardia and QRS widening can occur. Sodium bicarbonate therapy is advocated to directly counteract the toxic effects of propafenone. In the case described, this treatment resulted in rapid normalization of the QRS duration and stabilization of the hemodynamic profile.
Keywords: Class IC antiarrhythmics, Propafenone, Propafenone toxicity
Abstract
Une femme de 72 ans a présenté une diminution du niveau de conscience et de l’hypotension. L’électrocardiogramme initial a démontré une fibrillation auriculaire associé à un complexe QRS large. Ses antécédents médicaux ont révélé qu’elle venait de commencer à prendre du propafénone. On a posé un diagnostic de toxicité au propafénone et on lui a administré du bicarbonate de sodium. Il s’agit d’un phénomène rare dans lequel une toxicité s’est produite à une dose thérapeutique. La toxicité aiguë au propafénone se manifeste dans un grand nombre de systèmes organiques. Notamment, une atteinte cardiovasculaire sous forme d’hypotension, de bradycardie et d’élargissement du complexe QRS peut se produire. Une thérapie au bicarbonate de sodium est préconisée pour contrer directement les effets toxiques du propafénone. Dans le cas décrit, ce traitement a favorisé un rapide retour à la normale de la durée du complexe QRS et une stabilisation du profil hémodynamique.
Propafenone is a Vaughan-Williams class IC antiarrhythmic medication that is frequently used in the management of atrial fibrillation and other supraventricular arrhythmias. It works by blocking the fast inward sodium current and slowing the rate of increase of the action potential. This prolongs conduction and refractoriness in all areas of the myocardium, with a slightly more pronounced effect on intraventricular conduction.
It is well absorbed from the gastrointestinal tract, with a bioavailability in the range of 3% to 10%. Metabolism occurs in the liver, mainly via the cytochrome P450 2D6 complex, but also through 1A2 and 3A4. There are two genetically determined forms of metabolism: fast and slow. The half-life in fast metabolizers is approximately 7 h and can be as long as 17 h in slow metabolizers. Propafenone exhibits nonlinear pharmacokinetics. Increasing the dose from 300 mg to 900 mg per day results in a 10-fold increase in serum concentrations. This nonlinearity is believed to be due to a saturable first-pass effect in the liver. The usual dose of propafenone is 300 mg to 900 mg daily, divided into two or three doses.
We report a case of acute propafenone toxicity in which only a low dose of propafenone was ingested.
CASE PRESENTATION
A 72-year-old woman was brought to the emergency department after being found unresponsive by her family. She had reported feeling unwell the morning of presentation, with vomiting and diarrhea. On paramedic arrival, the patient was conscious and complaining of some central chest discomfort. She was bradycardic and her blood pressure was not palpable.
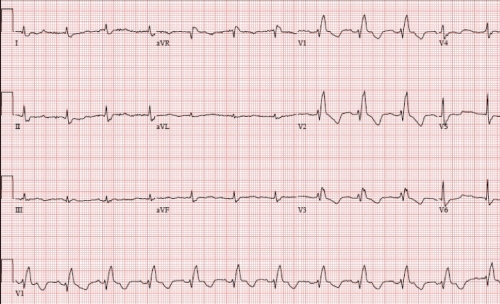
On arrival at the emergency department, she was found to be hypotensive with a systolic blood pressure of 50 mmHg to 60 mmHg and a heart rate of 60 beats/min to 80 beats/min. An electrocardiogram showed atrial fibrillation with a ventricular response of 80 beats/min, a QRS duration of 166 ms and a corrected QT interval of 536 ms (Figure 1). She was treated with aggressive fluid resuscitation to little effect. Bedside echocardiography showed an ejection fraction of 40% with global hypokinesis. She was treated with a dopamine infusion (up to 10 μg/kg/min).
Figure 1).
Electrocardiogram at presentation
She had a history of paroxysmal atrial fibrillation. Further questioning revealed that she had been seen by her cardiologist the day before and was found to be in atrial fibrillation with a fast ventricular response. Her cardiologist increased her verapamil dose from 80 mg three times a day (240 mg total) to 360 mg once a day and started her on propafenone 300 mg twice a day. She had taken one dose of propafenone the previous evening and one dose the morning of presentation. There was no history of ingestion of agents known to interact with propafenone or cause increased concentrations.
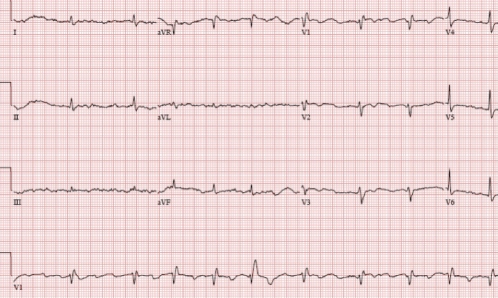
The possibility of propafenone toxicity was suggested, so a trial of intravenous sodium bicarbonate was administered. Following two ampules of sodium bicarbonate, her QRS duration narrowed to 116 ms (Figure 2) and her mean arterial pressure increased from 70 mmHg to 85 mmHg. She was then started on a continuous sodium bicarbonate infusion.
Figure 2).
Electrocardiogram after sodium bicarbonate administration
Within 8 h, her QRS duration had normalized, her hypotension had resolved and she was weaned off the dopamine infusion. The sodium bicarbonate infusion was also stopped. She was electrically cardioverted to normal sinus rhythm and discharged home on amiodarone and bisoprolol.
DISCUSSION
Propafenone toxicity
Toxicity related to propafenone ingestion involves a range of organ systems. Acute ingestions, as demonstrated in the present case, mainly involve cardiovascular compromise in the form of hypotension, bradycardia, ventricular dysrhythmias, QRS widening and heart block (1–3). Additional symptoms of nausea and vomiting as well as central nervous system depression and seizures have been noted to occur (1–3). The mortality from acute class IC toxicity is reported to be as high as 22.5% (1).
Several medications are known to increase plasma concentrations of propafenone through inhibition of the cytochrome P450 2D6 pathway. These include quinidine, cimetidine, desipramine, paroxetine, ritonavir and sertraline. Also, amiodarone, ketoconazole, saquinavir, erythromycin and grapefruit juice increase propafenone levels through inhibition of other cytochrome P450 pathways. As a high-extraction drug (low bioavailability), propafenone steady-state and/or peak concentrations could be significantly increased in the presence of a cytochrome P450 inhibitor. Assuming a bioavailability of 10% to 30%, complete inhibition of 2D6 metabolism could increase propafenone levels by as much as 300% to 1000%.
Treatment of propafenone toxicity
Treatment of acute propafenone toxicity largely involves supportive care. The principles of advanced cardiac life support take precedent in terms of monitoring for airway or hemodynamic decompensation. Placement on continuous cardiac monitoring as well as treatment of hypotension with fluids and inotropic support has been anecdotally shown to be successful in previous case reports (3,4). Cardiac pacing for symptomatic bradycardia has also been shown to be effective in cases of propafenone toxicity.
Sodium bicarbonate therapy has been proposed as a treatment for sodium channel blockade toxicity in conjunction with standard resuscitation measures (3,4). This therapy works by competitive displacement of propafenone from sodium channel binding sites (4). A second possible mechanism is the decreased affinity of propafenone for sodium channels in the setting of an increased pH level (4).
Gastric decontamination is theoretically useful but has not been researched. This therapy was not attempted in our patient because the ingestions did not fall into the 2 h window necessary for benefit.
There is little information on the utility of measuring propafenone levels in the context of acute toxicity. Other case reports (3) have described serum propafenone levels, but these have not been used to guide therapy. When available, these levels are used mainly to confirm the diagnosis of acute propafenone toxicity. Acute toxicity has been reported from therapeutic dosing of 675 mg daily to one-time ingestions of 8.1 g. The exact incidence of this complication with standard therapeutic doses is unknown. Propafenone levels were requested in the present case, but the blood drawn on admission had already been discarded. The possibility of obtaining concentrations from subsequent samples to back-calculate the original level was suggested at a later date.
There is a correlation between QRS duration and serum propafenone level, and, thus, the degree of propafenone toxicity (5). As such, QRS duration can be used to monitor resolution of the cardiotoxic effects of propafenone. We chose to use sodium bicarbonate as part of the management strategy for the above patient and monitored its effect with serial electrocardiograms. Administration of sodium bicarbonate resulted in an almost immediate reduction in QRS width and improvement in hemodynamics. Maintenance of this therapy, along with inotropic and fluid support, ultimately contributed to the recovery of the patient within hours. Follow-up echocardiography demonstrated improvement in her left ventricular function.
REFERENCES
- 1.Koppel C, Oberdisse U, Heinemeyer G. Clinical course and outcome in class IC antiarrythmic overdose. J Toxicol Clin Toxicol. 1990;28:433–44. doi: 10.3109/15563659009038586. [DOI] [PubMed] [Google Scholar]
- 2.Fonck K, Haenebalcke C, Hemeryck A, et al. ECG changes and plasma concentrations of propafenone and its metabolites in a case of severe poisoning. J Toxicol Clin Toxicol. 1998;36:247–51. doi: 10.3109/15563659809028948. [DOI] [PubMed] [Google Scholar]
- 3.Brubacher J. Bicarbonate therapy of unstable propafenone-induced wide complex tachycardia. Can J Emerg Med. 2004;6:349–56. doi: 10.1017/s1481803500009635. [DOI] [PubMed] [Google Scholar]
- 4.Griffin JP, D’Arcy PF. A Manual of Adverse Drug Interactions. 5th edn. Amsterdam: Elselvier Science BV; 1997. [Google Scholar]
- 5.Joglar JA, Hamdan MH, Page RL. Propafenone. Card Electrophysiol Rev. 1998;2:204–6. doi: 10.1023/a:1017920112995. [DOI] [PubMed] [Google Scholar]