Abstract
Background
The overlap between anxiety and major depressive disorder (MDD), the increased risk for depression and anxiety in offspring of depressed parents, the sequence of onset with anxiety preceding MDD, and anxiety as a predictor of depression are well established. The specificity of anxiety disorders in these relationships is unclear. This study, using a longitudinal high-risk design, examined whether anxiety disorders associated with the emotions fear and anxiety mediate the association between parental and offspring depression.
Method
Two hundred and twenty-four second-generation and 155 third-generation descendants at high and low risk for depression because of MDD in the first generation were interviewed over 20 years. Probit and Cox proportional hazard models were fitted with generation 2 (G2) or G3 depression as the outcome and parental MDD as the predictor. In G2 and G3, fear- (phobia or panic) and anxiety-related [overanxious or generalized anxiety disorder (GAD)] disorders were examined as potential mediators of increased risk for offspring depression, due to parental MDD.
Results
In G2, fear-related disorders met criteria for mediating the association between parental MDD and offspring MDD whereas anxiety-related disorders did not. These results were consistent, regardless of the analytic methods used. Further investigation of the mediating effect of fear-related disorders by age of onset of offspring MDD suggests that the mediating effect occurs primarily in adolescent onset MDD. The results for G3 appear to follow similar patterns.
Conclusions
These findings support the separation of anxiety disorders into at least two distinct forms, particularly when examining their role in the etiology of depression.
Keywords: Anxiety, depression, fear, mediator, multi-generation
Introduction
There is considerable overlap between anxiety and major depressive disorder (MDD) (Brady & Kendall, 1992); parental depression increases the risk for offspring anxiety and depression (Downey & Coyne, 1990; Beardslee et al. 1998) and the onset of anxiety precedes the onset of depression in community as well as clinic samples of children, adolescents and adults (Kovacs et al. 1989; Lewinsohn et al. 1995). Prior anxiety often predicts subsequent depression (Breslau et al. 1995; Lewinsohn et al. 1995; Cole et al. 1998). The specificity of the anxiety disorders in these relationships is unclear. In a review of twin and family studies examining the co-morbidity of anxiety and depression, the results were consistent with anxiety and depression having an overlapping genetic etiology or one disorder being an epiphenomenon of the other (Middeldorp et al. 2005). Results from twin studies also suggest that generalized anxiety disorder (GAD) and MDD may be different forms of the same disorder (Kendler et al. 1992, 2007; Roy et al. 1995), genetic influences on depression after the age of 14 reflect liability to prior overanxious and phobic symptoms (Silberg et al. 2001), and family history of depression is associated with early onset anxiety, which is associated with a history of depression (Kendler et al. 2002, 2006). Findings from studies of animals and humans support the refinement of depressive phenotypes by taking into account the distinction between anxiety disorders related to the emotions of fear and anxiety (i.e. fear-related disorders, defined as panic or phobia, and anxiety-related disorders, defined as overanxious or GAD). This distinction may help to clarify the nature of the relationship between depression and anxiety disorder and the development of a familial form of depression (Hasler et al. 2004).
Anxiety as a predictor of depression
Numerous studies have shown an association between anxiety and depression. Few have examined specific anxiety disorders or anxiety as a predictor of depression. The studies that have examined the relationship in more detail have shown that anxiety is a mediator of the increased risk for MDD in females as compared to males (Breslau et al. 1995; Parker & Hadzi-Pavlovic, 2004), and that MDD co-morbid with anxiety disorders, as compared to either disorder alone, is more persistent, resistant to treatment and, therefore, more impairing (Fava et al. 1997; Merikangas et al. 2003). The presence of multiple anxiety disorders, impairment, persistent avoidance and panic-like attacks are the features of anxiety associated with an elevated risk for a subsequent onset of depression (Wittchen et al. 2000). Only three studies have examined specific anxiety disorders. Parker & Hadzi-Pavlovic (2004) found some specificity linking early adolescent onset depression with GAD and panic disorder. Pine et al. (1998 (2001) showed that phobic fear of the dark and overanxious disorder (OAD) were both associated with an equivalent increased risk for subsequent MDD. Neither study took into account familial risk for depression or anxiety. Biederman et al. (2007) determined separation anxiety to be predictive of subsequent onset of depression independent of parental diagnosis.
Unanswered questions
Although a link between the familial nature of anxiety disorders and depression has been established, several questions remain unanswered. Specifically, does separating anxiety disorders into those that are thought to be associated with differential but interconnected circuitry in the brain provide useful information regarding the etiology of a familial form of depression preceded by anxiety? Research with animals supports the separation of emotions relevant to anxiety disorders into fear and anxiety, but the validity of this distinction is less clear with humans. Studies in humans have suggested a greater number of emotions than just fear and anxiety potentially associated with anxiety disorders (Gray & McNaughton, 2003). Furthermore, the pathophysiology of anxiety disorders in humans is not well understood. There is disagreement on the primary neural circuits involved, the role of various structures such as the amygdala and hippocampus in each, and how best to explore the circuitry (LeDoux, 2002; Gray & McNaughton, 2003).
There are at least two theories regarding the underlying neural circuitry of anxiety disorders. LeDoux and others have argued for the primacy of the fear network, composed of systems (cognitive-language, motor-behavioral and psychophysiological) interacting through a neural network, with a greater role played by the amygdala as compared to the hippocampus in response to threat (LeDoux, 1996, 2002; Roth, 2005). Gray & McNaughton (2003), while acknowledging the role of the amygdala in the etiology of specific phobias, have developed a theoretical model that focuses on the septo-hippocampal system as the primary system in the etiology of anxiety disorders.
Much of the published literature on this topic appears to support LeDoux’s theory of a dominant role for the amygdala in a subset of anxiety disorders defined as ‘fear-related disorders’ (Neiho. & Kuhar, 1983; Bechara et al. 1995; Breiter et al. 1996; Onoe et al. 1996; Walker & Davis, 1997; File, 2000; Funayama et al. 2001; Phelps et al. 2001; Grillon, 2002). Cued fear-conditioning experiments have led to a greater understanding of the acquisition of fear in humans and animals and are relevant to understanding phobic disorders due to the presence of an identifiable cue; however, phobic disorders are heterogeneous. The hypersensitivity of the fear network and the amygdala has also been implicated in the etiology of panic disorder (Gorman et al. 2000; Gray & McNaughton, 2003; Herdade et al. 2006). By contrast, the bed nucleus of the stria terminalis (BNST) or hippocampus appears to play a dominant role in the development of the subset of anxiety disorders defined as ‘anxiety-related disorders’ (Phillips & LeDoux, 1992; Bechara et al. 1995; Davis, 1998; Grillon, 2002).
It has been suggested that hypersensitivity of the fear network may be a factor in risk for depression as well as anxiety (Gorman et al. 2000). Depression has been shown to be associated with increased amygdala and decreased hippocampal volumes (Frodl et al. 2002a, b). Increased amygdala volumes seem to be more prevalent in recent or first onset as compared to recurrent MDD and are thought to be related to increased blood flow and not predisposing structural abnormalities (Frodl et al. 2002a, b, 2003). Furthermore, at least one study has suggested that the amygdala–hippocampal ratio in MDD is associated with the severity of co-morbid anxiety (MacMillan et al. 2003). Increased amygdala and decreased hippocampal volumes may be more pronounced in familial than in non-familial patients with MDD (Rosenberg et al. 2006). These findings suggest that hypersensitivity of the fear network leading to increased activity in the amygdala may play a role in the onset of some subtypes of MDD.
Hypotheses to be tested
It is within this context that we examined the hypothesis that fear- or anxiety-related disorders examined separately mediate the association between parental and offspring MDD. To our knowledge, this hypothesis has not yet been examined.
The following sub-hypotheses were tested: (a) the pathway including anxiety- or fear-related disorders will explain a greater proportion of the association between parent and child depression than all other pathways; and (b) the association will vary by the child’s developmental phase and gender. Because of the increased risk for depression and anxiety in females as compared to males, as well as evidence that anxiety disorders partially mediate the increase in risk due to gender, we hypothesized that the association between fear and/or anxiety and depression would be stronger for females than males. As the familial nature of depression has been shown to vary as a function of developmental phase (Wickramaratne & Weissman, 1998; Jaffee et al. 2002), we conducted an exploratory analysis to determine whether the role of fear- and/or anxiety-related disorders in the prediction of depression varies as a function of whether the onset occurs in childhood, adolescence or adulthood.
Method
Sample
The study design was retrospective cohort, longitudinal and multi-generational. The hypotheses were tested in a sample followed over 20 years. This study has completed four waves of assessments between 1982 and 2002. The sample now includes three generations [grandparents (G1), parents (G2) and grandchildren (G3)] and consists of families at high or low risk for depression based on the depression status of the original sample (G1).
The G1 sample derives from the Yale Family Study of Depression (Weissman et al. 1984). Of the eligible families (n=105) with children aged between 6 and 23 years, 87.5% agreed to participate and those who refused were divided equally between depressed and non-depressed families. One or more of the parents from the depressed families had received treatment for depression. The non-depressed families derived from a community study in New Haven, Connecticut (Weissman & Myers, 1978) and reported no history of treatment or psychiatric illness. The depressed and non-depressed parents were white and group matched by age and sex.
The G2 sample included all those G2 who were interviewed at either wave 1 or wave 2 and followed up at either wave 3 or wave 4. Two hundred and sixty-three G2 were interviewed at wave 1 or wave 2. One had a mental disability and two died, leaving a potential sample of 260 to be re-interviewed at wave 3 and/or wave 4. Two hundred and twenty-four (86%) were re-interviewed. There were no significant differences between the 224 who were interviewed and the 36 who were not interviewed by G1 diagnosis of MDD, G2 MDD, anxiety, sex or age at wave 2.
The sample for G3 included all G3 directly interviewed at either wave 3 or wave 4 who are biologically related to G1 (n=155). There were no significant differences in the response rate of the grandchildren by sex or by depression status of their grandparent.
Assessment at waves 1, 2, 3 and 4
Assessment instruments
The Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS) Epidemiologic or Present Lifetime (Kaufman et al. 1997; Orvaschel, 2006) and child versions of the Schedule for Affective Disorders and Schizophrenia Lifetime version (SADS-LA) (Endicott & Spitzer, 1978; Mannuzza et al. 1986) were used for all subjects aged <18 years. The SADS-LA was used for all subjects aged ≥18 years. Detailed clinical narratives were prepared by the interviewers to document the context and basis for diagnosis.
Interviewers
Ph.D.- and Masters-level experienced mental health professionals conducted interviews in-person or over the telephone. Interviewers were blind to the diagnostic assessments from prior waves and the diagnostic assessment of subjects’ parents. For additional details on the sample, assessments, training, inter-rater reliability and monitoring for quality control, see Weissman et al. (1987, 1992, 1997, 2005).
Best Estimate (BE) diagnoses
All available diagnostic information on G1, G2 and G3 was reviewed blindly as to initial diagnostic assessments and the diagnostic assessment of their parents and/or offspring by a psychiatrist or psychologist who made Best Estimate (BE) diagnoses (Leckman et al. 1982). Each case was reviewed independently by a second BE. If there was disagreement, a consensus diagnosis was made. At wave 4, 178 adult and child cases were randomly selected and best estimated by a trained psychologist and psychiatrist. Inter-rater reliability measured by the k statistic was any mood disorder 0.83; MDD 0.82; dysthymia 0.89; any anxiety disorder 0.65; any phobic disorder 0.62; agoraphobia 0.52; social phobia 0.38; specific phobia 0.65; panic disorder 0.76; GAD/OAD 0.79; alcohol abuse/dependency 0.94; and drug abuse/dependency 1.00.
Depression
G1 MDD was defined according to Research Diagnostic Criteria modified to require 4 weeks’ duration and impairment. Lifetime DSM-IV MDD was used as the outcome for G2. For the G3 analyses, to approximate the depression criteria used in G1, impairment, as defined by a Global Assessment Scale score of <70, was used as a criterion for depression for G2 (Weissman et al. 2005). The age at earliest episode of depression was considered to be the age at onset for depression. For G3, any DSM-IV mood disorder that met either probable or definite criteria was used as the outcome. G3 mood disorder was used because they were too young to have passed through the peak age of risk for MDD, and childhood (not adult) dysthymia could be prodromal MDD (Kovacs et al. 1994). Mood disorder includes MDD, dysthymia, and depressive disorder not otherwise specified. Childhood onset depression was defined prior to age 13, adolescent onset between the ages of 13 and 18, and adult onset 19 years of age or older.
Offspring anxiety – G2 and G3
Two groups of lifetime anxiety disorders were created: (a) fear-related disorders, which included agoraphobia, social phobia, simple phobia, or panic disorder; and (b) anxiety-related disorders, which included OAD or GAD. All other anxiety disorders were treated as potential confounders.
Potential confounders
The factors below are potential confounders of the association between the intermediate variable and the outcome as well as confounders of the association between the exposure and the outcome.
Parental diagnoses – G1
Parental diagnoses of panic disorder, GAD, agoraphobia, simple phobia, social phobia, obsessive compulsive disorder (OCD), dysthymia and alcohol or drug abuse/dependence were examined as potential confounders.
Offspring diagnoses – G2 and G3
Offspring diagnoses of conduct disorder, oppositional defiant disorder, attention deficit disorder (ADD), alcohol and/or drug abuse/dependence, co-morbid anxiety disorders, and dysthymia (G2 only) were examined as confounders.
Statistical analysis
The definition of a mediator and conditions for mediation to exist follow the criteria laid out by Baron & Kenny (1986) and operationalized by Rothman & Greenland (1998). For the condition of mediation to exist, parental MDD must be associated in G2 or G3 with fear- and/or anxiety-related disorders and depression; fear- and/or anxiety-related disorders must be associated with depression; the effect of parental MDD in the presence of fear- and/or anxiety-related disorders must be less than in the absence of fear- and/or anxiety-related disorders; and the effect of offspring fear- and/or anxiety-related disorders on depression must remain with parental MDD in the model (Baron & Kenny, 1986). In addition, the onset of parental MDD must precede onset of anxiety and onset of fear- and/or anxiety-related disorders must precede the onset of depression.
Analyses were conducted as follows. For G2, initially prior fear- and/or anxiety-related disorders were used to predict MDD regardless of age of onset and subsequently to predict childhood, adolescent and adult onset MDD. For G3, initially we examined the association of fear- and anxiety-related disorders with mood disorder regardless of age of onset and subsequently to predict childhood and adolescent onset mood disorder.
We used both proportional hazards and path analyses because these analyses complement each other. In the proportional hazards analysis, the outcome is a dichotomous variable defined as whether or not the individual has the disorder. No other assumption is made about the distribution of the disorder. The limitations of using the proportional hazards model to test our specific hypotheses were that no formal tests of mediation are available. With path analysis, formal methods for testing for mediation are well established, but the underlying assumption that the outcome is a latent variable, that is liability to depression that is normally distributed, is untestable. If the results using each of the methods were consistent, it would give us more confidence in our conclusions.
Cox proportional hazards models were used instead of logistic regression to adjust for differential length of follow-up (Cox, 1972). For G2 and G3, fear- and anxiety-related disorders were treated as time-dependent covariates. The start of follow-up is time of birth. Correlated outcomes within family were adjusted for using the approach of Lin & Wei (1989). The effect of parental MDD on offspring depression in the presence as compared to absence of fear- or anxiety-related disorders was considered to be less if there was a 10% or greater reduction in the β associated with parental MDD (Rothman & Greenland, 1998). To assess variation of mediation effects by age of onset, first three separate Cox proportional hazard models (Cox, 1972; Cox & Oakes, 1984) were fitted, where the incidence of disorder in offspring in childhood, adolescence and adulthood were considered to be the outcomes. For G2 only, to formally test whether the effect of fear- and anxiety-related disorders on the association between parental and offspring depression statistically significantly varies by developmental phase, a single model was fitted with three dummy variables, one for each developmental phase using extended proportional hazards models (Kleinbaum, 1996). The fit of models with and without dummy variables was examined by comparing the log likelihoods. This will show whether the association of these disorders with depression varies by developmental phase.
The approach outlined above did not allow us to formally estimate the proportion of the association between parental depression and offspring depression mediated by fear- or anxiety-related disorders. To address this issue, path analysis was used, where the model assumes that fear- and anxiety-related disorders are represented by underlying continuous variables rather than assuming they are dichotomous variables. When the outcome exceeds a threshold, the individual is classified as having the disorder. This underlying variable may be interpreted as the liability to the disorder. The probability of exceeding the threshold is based on the assumption that the underlying variables are normally distributed. This model is referred to as a probit model. These models can be viewed as estimating the correlations between the underlying liabilities for fear- and anxiety-related disorders and depression. Model fitting for the path analysis was undertaken using MPLUS version 4.1, which allows categorical outcomes (Muthen & Muthen, 1998–2004). The fit function was weighted least squares. To address the issue that the distribution of parameters derived from the path analysis could deviate from a normal distribution, standard errors and confidence intervals were calculated using the bias-corrected bootstrap method (Shrout & Bolger, 2002). The coefficients are considered to be nonsignificant if the confidence interval includes zero. In addition, the models were run constraining the parameters to be equal to test whether the assumption that the models for males and females were the same was a good fit. Path analyses were only conducted for subgroups where the association between parental MDD and the outcome was significant.
Confounders
Cox proportional hazards and probit models were fitted with each potential confounder, entered one at a time and simultaneously to determine whether they explained the association. It was necessary to control for potential confounders of the association between the intermediate variable and the outcome as well as confounders of the association between the exposure and the outcome (Cole & Hernan, 2002).
Results
Sample characteristics of offspring
In G2, gender and age did not differ by G1 depression status. Sixty per cent of G2 were females and the mean age at last interview was 35.8 years (S.D.=6.7). For G3, gender did not differ by the G1 depression status. Fifty-four per cent were female. The median age was 11 years and the age range was 5–20 years. However, G3 from the low- as compared to the high-risk group were significantly younger at last interview (mean age of 10.7 v. 13.1 years respectively).
Is G1 MDD associated with G2 MDD and fear- and anxiety-related disorders?
G1 MDD was significantly associated with G2 MDD at all ages of onset and G2 fear-related disorders. There was a trend for G1MDDto be associated with an increase in risk for G2 anxiety-related disorders (Table 1). Not shown here, G2 fear-related disorders included agoraphobia (11%), social phobia (19%), specific phobia (53%) and panic disorder (42%).
Table 1.
Risk for depression and fear- and anxiety-related disorders due to parental MDD (G2 and G3)
| G1 MDD one or more |
G1 MDD neither |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Generation 2 | G1 MDD one or more | G1 MDD neither | Generation 3 | Generation 3 | ||||||
| G2 diagnoses | (n=155) n (%) | (n=69) n (%) | HR (95% CI)a | G3 diagnoses | (n=34) G2 MDD n (%) | (n=63) No G2 MDD n (%) | HR (95% CI)a | (n=12) G2 MDD n (%) | (n=46) No G2 MDD n (%) | HR (95% CI)a |
| Any MDD | 96 (61.9) | 19 (27.5) | 2.9 (1.7–5.2)**** | Any mood disorder | 13 (38.2) | 10 (15.9) | 2.5 (1.2–5.0)** | 0 (0.0) | 4 (8.7) | N.E. |
| Onset of MDDb | Onset of moodb | |||||||||
| Onset <13 | 21 (13.6) | 2 (2.9) | 5.2 (1.4–19.0)** | Onset <13 | 8 (23.5) | 8 (12.7) | 1.9 (0.80–4.4) | 0 (0.0) | 1 (2.1) | N.E. |
| Onset 13–18 | 35 (22.6) | 8 (11.6) | 2.4 (1.2–4.5)*** | Onset 13–18 | 5 (14.7) | 2 (3.2) | 4.8 (0.96–24.1)* | 0 (0.0) | 3 (6.5) | N.E. |
| Onset ≥19 | 40 (25.8) | 9 (13.0) | 2.7 (1.2–6.0)** | |||||||
| Fear-related disordersc | 67 (43.2) | 13 (18.8) | 3.6 (1.9–7.1)**** | Fear-related disordersc | 17 (50.0) | 8 (12.5) | 4.3 (1.9–9.6)**** | 2 (16.7) | 4 (8.7) | 2.2 (0.28–18.1) |
| Anxiety-related disordersd | 24 (15.5) | 4 (5.8) | 2.7 (0.96–7.3)* | Anxiety-related disordersd | 1 (2.9) | 3 (4.7) | 0.63 (0.07–5.9) | 0 (0.0) | 0 (0.0) | N.E. |
MDD, Major depressive disorder; HR, hazard ratio; CI, confidence interval; N.E., not estimated due to zero cells.
Adjusted for age and correlation within family.
Each onset group compared to G3 without mood disorder.
Panic/agoraphobia, social or specific phobia.
Overanxious/generalized anxiety disorder.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Are G1 MDD and G2 MDD associated with G3 mood disorder and fear- and anxiety-related disorders?
Among families with G1 MDD, (a) there was a significant association of G2 MDD with G3 mood disorder and fear-related disorders; and (b) there was no significant association between G2 MDD and anxiety-related disorders (Table 1). Not shown here, G3 fear-related disorders included agoraphobia (3%), social phobia (26%), specific phobia (71%) and panic disorder (16%).
Do G2 fear- or anxiety-related disorders increase the risk for G2 childhood, adolescent and adult MDD?
G2 fear-related disorders were associated with a 2–3-fold increase in risk for childhood, adolescent and adult MDD. Anxiety-related disorders were significantly associated with any MDD, and adolescent onset MDD. There was a trend for an association between anxiety-related disorders and adult onset MDD (Table 2).
Table 2.
Risk for depression due to fear- and anxiety-related disorders (G2 and G3)
| HR (95% CI)a | |
|---|---|
| Generation 2 (G2) | |
| G2 MDD | |
| Fear-related disordersb | 2.9 (1.9–4.4)**** |
| Anxiety-related disordersc | 2.6 (1.2–5.6)** |
| G2 Childhood onset (<13 years of age) MDD | |
| Fear-related disordersb | 2.7 (1.1–6.9)** |
| Anxiety-related disordersc | 1.8 (0.33–9.8) |
| G2 Adolescent onset (13–18 years of age) MDD | |
| Fear-related disordersb | 3.0 (1.7–5.5)**** |
| Anxiety-related disordersc | 3.4 (1.0–11.8)** |
| G2 Adult onset (19+ years of age) MDD | |
| Fear-related disordersb | 2.0 (0.97–4.3)* |
| Anxiety-related disordersc | 2.4 (1.1–5.2)** |
| Generation 3 (G3) | |
| G3 Any mood disorder | |
| Fear-related disordersb | 3.3 (1.5–7.7)*** |
| Anxiety-related disordersc | 3.7 (0.49–28.5) |
| G3 Childhood onset (<13 years of age) mood disorder | |
| Fear-related disordersb | 2.5 (0.83–7.4) |
| Anxiety-related disordersc | 5.9 (0.69–52.0) |
| G3 Adolescent onset (13–18 years of age) mood disorder | |
| Fear-related disordersb | 4.7 (1.3–16.2)** |
| Anxiety-related disordersc | 0.0 (0.0–0.0) |
MDD, Major depressive disorder; HR, hazard ratio; CI, confidence interval.
Adjusted for age and correlation within family.
Panic/social or simple phobia.
Overanxious/generalized anxiety disorder.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Do G3 fear- and anxiety-related disorders increase the risk for G3 mood disorder?
G3 fear-related disorders were significantly associated with any mood disorder and adolescent onset mood disorder (Table 2).
Is the effect of parental MDD on offspring depression less in the presence of fear- and anxiety-related disorders?
For G2, fear-related disorders were examined as mediators of the association between parent and child, adolescent and adult onset MDD. G2 anxiety-related disorders were examined as mediators of the association between parental and adolescent and adult onset MDD.
There was only a 10% or greater reduction in the β for parental MDD when fear-related disorders were entered into the proportional hazards model where any MDD or adolescent onset MDD was the outcome. In both models, fear-related disorders remained significant. There was a 0–2% decrease in the β for the association of G1 MDD with any MDD, adolescent and adult onset MDD, when anxiety-related disorders were entered into the model with G1 MDD (Table 3).
Table 3.
Risk for offspring depression due to parental MDD in the absence and presence of offspring fear- and anxiety-related disorders (G2 and G3)
| Adjusted for agea HR (95% CI) | Adjusted for age and fear-related disordersa % decrease in β for G1/G2 MDD | |
|---|---|---|
| Generation 2 (G2) | ||
| G2 MDD | ||
| G1 MDD | 2.9 (1.7–5.2)**** | |
| Adjusted for G2 | ||
| Fear-related disordersb | 2.5 (1.4–4.4)*** | 18 |
| Anxiety-related disordersc | 2.9 (1.6–5.1)**** | 0 |
| G2 MDD with onset <13 | ||
| G1 MDD | 5.2 (1.4–19.0)** | |
| Adjusted for G2 | ||
| Fear-related disordersb | 4.5 (1.1–17.6)** | 6 |
| G2 MDD with onset 13–18 | ||
| G1 MDD | 2.4 (1.3–4.5)*** | |
| Adjusted for G2 | ||
| Fear-related disordersb | 1.8 (0.89–3.7) | 31 |
| Anxiety-related disordersc | 2.3 (1.2–4.6)** | 0 |
| G2 MDD with onset 19+ | ||
| G1 MDD | 2.7 (1.2–6.0)** | |
| Adjusted for G2 | ||
| Fear-related disordersb | 2.5 (1.1–5.6)** | 9 |
| Anxiety-related disordersc | 2.6 (1.2–5.9)** | 2 |
| Generation 3 (G3) (in families where G1 had MDD) | ||
| Any G3 mood disorder | ||
| G2 MDD | 2.5 (1.2–5.0)** | |
| Adjusted for G3 | ||
| Fear-related disordersb | 1.9 (0.82–4.6) | 28 |
| G3 mood disorder onset 13–18 | ||
| G2 MDD | 4.8 (0.96–24.1)* | |
| Adjusted for G3 | ||
| Fear-related disordersb | 2.5 (0.28–22.6) | 43 |
MDD, Major depressive disorder; HR, hazard ratio; CI, confidence interval.
Adjusted for correlation within family.
Panic/agoraphobia, social or specific phobia.
Overanxious/generalized anxiety disorder.
p<0.1,
p<0.05,
p<0.01,
p<0.001.
For G3, parental MDD was not significantly associated with anxiety-related disorders. Therefore, anxiety-related disorders were not examined as possible mediators of the association between parent and offspring mood disorder. G3 fear-related disorders were examined as mediators of the association between parental MDD and G3 any mood disorder and adolescent onset mood disorder.
In families with G1 MDD, there was a 10%or greater reduction in the β for parental MDD when fear-related disorders were added to the proportional hazards model where any mood disorder or adolescent onset mood disorder was the outcome (Table 3).
Model fit
There was a trend for the model with, as compared to without, the dummy variables for fear-related disorders to be a better fit (χ2=4.77, df=2, 0.05<p<0.1).
Path analysis results for G2 and G3
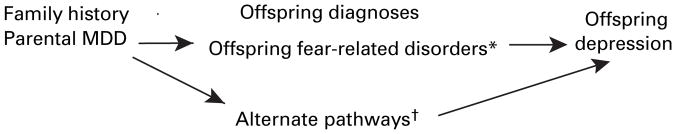
The pathway including fear-related disorders is referred to as the indirect pathway and the pathways that do not include fear-related disorders are labeled as alternate pathways. Figure 1 presents the mediational model tested. Anxiety-related disorders were only considered as a mediator in the model where any MDD was the outcome due to the small number of cases of the disorder. For G3, the model was restricted to the sample with G1 MDD.
Fig. 1.
Pathways from parental to offspring major depressive disorder (MDD). * Denotes indirect pathway; denotes direct and all other indirect pathways.
Generation 2
Any MDD – fear-related disorders
The indirect pathway was significant. Seventy-four per cent of the impact of parental MDD on the risk for MDD was through alternate pathways and 26% was through fear-related disorders. Not shown here, the patterns for males and females were not statistically significantly different (χ2=1.07, df=3, p=0.78).
Any MDD – anxiety-related disorders
The indirect pathway was not significant. Ninety-one per cent of the impact of parental MDD on the risk for MDD was through alternate pathways and 9% was through anxiety-related disorders (Table 4).
Table 4.
Alternate and indirect effects of parental MDD on liability to depression in generations 2 and 3
| Type of effect | Parental MDD |
||
|---|---|---|---|
| Effect | BC bootstrap (95% CI)a | % | |
| Generation 2 | |||
| All MDD – fear-related disorders | |||
| Alternate | 0.67 | (0.24–1.1) | 74 |
| Indirect | 0.23 | (0.05–0.55)* | 26 |
| Mediator – fear-related disorders | 0.30 | (0.02–0.50)* | |
| All MDD – anxiety-related disorders | |||
| Alternate | 0.86 | (0.41–1.3)* | 91 |
| Indirect | 0.09 | (−0.07 to 0.32) | 9 |
| Mediator – anxiety-related disorders | 0.20 | (−0.19 to 0.55) | |
| G2 Fear-related disorders by developmental phase | |||
| Childhood MDD | |||
| Alternate | 0.64 | (0.003–1.3) | 80 |
| Indirect | 0.16 | (−0.11 to 0.48) | 20 |
| Mediator – fear-related disorders | 0.19 | (−0.17 to 0.46) | |
| Adolescent MDD | |||
| Alternate | 0.07 | (−0.45 to 0.68) | 13 |
| Indirect | 0.46 | (0.17–0.91)* | 87 |
| Mediator – fear-related disorders | 0.49 | (0.19–0.69)* | |
| Adult MDD | |||
| Alternate | 0.66 | (0.18–1.2)* | 86 |
| Indirect | 0.11 | (−0.09 to 0.43) | 14 |
| Mediator – fear-related disorders | 0.17 | (−0.15 to 0.49) | |
| Generation 3 | |||
| All mood disorders | |||
| Alternate | 0.29 | (−0.47 to 0.99) | 42 |
| Indirect | 0.40 | (0.005–0.90)* | 58 |
| Mediator – fear-related disorders | 0.44 | (−0.07 to 0.71) | |
| Adolescent onset mood disorder | |||
| Alternate | 0.45 | (−0.64 to 1.6) | 40 |
| Indirect | 0.72 | (0.13–1.6)* | 60 |
| Mediator – fear-related disorders | 0.62 | (0.02–0.88)* | |
MDD, Major depressive disorder; BC, bias corrected; CI, confidence interval.
Intervals not including zero significant at p<0.05.
Childhood onset MDD
The indirect pathway was not significant. Eighty per cent of the impact of parental MDD on risk for childhood MDD was through alternate pathways and 20% through the indirect pathway. Not shown here, the indirect pathway was only statistically significant for males. The patterns for males and females are statistically significantly different (χ2=13.40, df=6, p=0.04) (Table 4).
Adolescent onset MDD
The indirect pathway was significant. Only 13% of the impact of parental MDD on adolescent MDD was through alternate pathways and 87% through the indirect pathway. Not shown here, parental MDD was not significantly associated with adolescent onset MDD for males, so path analyses were not conducted. For females, only the indirect pathway was significant (Table 4).
Adult onset MDD
The indirect pathway was not significant. Eighty-six per cent of the impact of parental MDD on risk for adult MDD was through alternate pathways and 14% was through the indirect pathway. Not shown here, the pattern for males and females are statistically significantly different (χ2=18.65, df=7, p=0.009) (Table 4).
Generation 3
Anxiety-related disorders
Path analyses were not conducted with anxiety-related disorders because parental MDD was not associated with G3 anxiety-related disorders.
Any mood disorder
The indirect pathway was significant. The percentage impact of parental MDD on risk for any mood disorder was slightly greater for the indirect as compared to alternate pathways (Table 4). The patterns for males and females were not statistically significantly different (χ2=6.38, df=5, p=0.27).
Childhood onset mood disorder
Parental MDD was not significantly associated with childhood onset mood disorder; therefore, path analyses were not conducted.
Adolescent onset mood disorder
The indirect pathway was not significant. The percentage impact of parental MDD on risk for adolescent mood disorder was greater for the indirect as compared to alternate pathways. Small sample size did not allow the models to be run separately for males and females (Table 4).
Model fit
In all models with fear-related disorders, the addition of the indirect pathway significantly improved the overall fit of the model (p<0.05).
G2 compared to G3
We constrained the outcome for G2 and G3 to be child or adolescent onset dysthymia or MDD in order to more directly compare the two generations (not shown here). For G2 and G3, the path coefficients for the indirect pathway were nearly identical (0.34 v. 0.30 respectively). Alternate pathways played a slightly greater role in predicting dysthymia or MDD for G3 as compared to G2 (0.46 v. 0.38 respectively).
Are the associations explained by confounders?
Confounders for G2
Neither G1 substance use or anxiety disorders in either parent nor G2 co-morbid anxiety, substance use, dysthymic or disruptive disorders explained any of the associations. Furthermore, G1 anxiety-related disorders increased the path coefficient associated with fear-related disorders while decreasing the coefficient associated with the alternate pathway.
Confounders for G3
Neither G2 substance use or anxiety disorders in either parent nor G3 co-morbid anxiety, substance use or disruptive disorders explained the relevant associations. Inclusion of G2 or G3 in the path models increased path coefficients associated with fear-related disorders, while decreasing the significance of the alternate pathway. For adolescent onset mood disorders, G2 childhood fear-related disorders partially explained associations between both G2 MDD and G3 childhood fear-related disorders, and that of G3 fear-related disorders and G3 adolescent onset MDD. By contrast, G3 anxiety-related disorders decreased the coefficient for alternate pathways.
Discussion
We sought to determine whether refining depressive phenotypes by differentiating between fear- and anxiety-related disorders clarifies the understanding of the development of, or pathways to, a specific type of depression transmitted across three generations. The refinement suggests that fear- and not anxiety-related disorders across multiple generations play a crucial role in the pathway to familial depression. If fear-related disorders have a stronger association with disturbances in brain circuitry dominated by the amygdala rather than the hippocampus or the BNST, then our results support a greater role for the amygdala and associated neural circuitry in the etiology of a type of familial MDD with an onset after childhood (Walker & Davis, 1997; LeDoux, 2002). Furthermore, risk for depression due to fear-related disorders appears to be specific to parental depression and is not due to co-morbid parental disorders. The risk for depression due to fear-related disorders in families with parental MDD is greater in the absence of parental anxiety-related disorders. While not an a priori hypothesis, parental anxiety-related disorders and parental substance use appear to be involved in pathways that do not involve fear-related disorders. When we divided the parents with MDD in our sample by whether they had co-morbid panic disorder or MDD alone, the rates of fear-related disorders in the two groups were equivalent (41%). This suggests that fear-related disorders in our sample are not associated exclusively with parental panic disorder and potentially represent a type of depression associated with hypersensitivity of the fear network. These findings also support the separation of anxiety disorders into at least two distinct forms, particularly when examining their role in the etiology of familial depression.
Consistent with other studies, we found that GAD and OAD predict a subsequent onset of depression (Pine et al. 1998; Parker & Hadzi-Pavlovic, 2004). These findings could indicate that certain types of depression are indistinguishable from GAD, which would be consistent with findings from some twin studies (Kendler et al. 1992, 2007; Roy et al. 1995). However, our findings are unique because they suggest that although the risk for major depression may be similar for these categories of anxiety disorder, only fear-related disorders appear to mediate the association between parental and offspring depression. These findings are consistent with those studies that have shown that increased stress sensitivity increases the risk for anxiety and depression (Heim & Nemeroff, 2001; Caspi et al. 2003). Fear-related disorders due to the presence of an identifiable object, such as an environmental event, could be hypothesized to be the anxiety disorders associated with increased stress sensitivity. The moderation of this association by the serotonin genotype suggests that this type of depression may be genetic and therefore familial. The effect of environmental stress and the effects of the serotonin genotypes are, however, beyond the scope of the present study.
The rate of anxiety-related disorders in this sample is lower than that reported in most community-based studies of children and adolescents (Cohen et al. 1993; Shaffer et al. 1996; Costello et al. 2003). In a 5-year follow-up study of children aged on average 10 years, at high and low risk for panic disorder and MDD, the lifetime rates of GAD were 27% for offspring with parents with panic and MDD and 11% for offspring of parents with MDD without panic (Biederman et al. 2006). The rates in our sample of anxiety-related disorders are closest to those among the offspring of parents with MDD without panic (i.e. 12.5%). Rates were lower in G3 because they have not passed through the peak age of risk for GAD. The GAD rates may have been higher and the onset earlier in the Biederman et al. (2006) sample because of high loading in the parents for anxiety disorders.
Finally, our findings shed light on the variation in risk for familial depression across developmental periods. Childhood depression has been shown to have risk factors that are distinct from those for depression with onset after childhood (Wickramaratne & Weissman, 1998; Jaffee et al. 2002). Childhood depression appears be associated with fear- and anxiety-related disorders; however, neither explain the association of parental MDD with childhood depression. In contrast to childhood onset depression, vulnerability to adolescent onset depression due to parental MDD is at least partially explained by fear-related disorders. Clinically, these findings suggest that treating children of depressed parents with phobic disorders may prevent a subsequent onset of depression. The findings also support the distinction between fear- and anxiety-related disorders.
Limitations
The generalizability of these findings is limited to samples generated from families with grandparents who had moderate to severe depression and had received treatment. The reliability and rates of the specific disorders included in fear-related disorders should be taken into account when interpreting the results. We had limited power to detect potential interactions, particularly for G3. It was not possible, given the design of the study, to determine what contribution genes make to the association between anxiety and depression. The results regarding anxiety-related disorders and gender differences should be interpreted with caution because of the low overall rates of anxiety-related disorders. Childhood disorders were not assessed in G1; therefore, it was not possible to examine the role of G1 childhood onset fear- and anxiety-related disorders in the association between offspring anxiety and depression. Furthermore, fear-related disorders are not a direct measure of disturbances in the fear network. These limitations are being addressed in the ongoing work in this sample, which includes examining fear- and context-potentiated startle response, neuroimaging and genotype data.
Acknowledgments
This work was partially supported by National Institute of Mental Health grant MH36197, Rockville, MD (to M.W.). M. Weissman has received support for investigator-initiated grants on depression from Lilly and from GlaxoSmithKline. Dr A. J. Fyer provided insights based on her clinical and research expertise, particularly in the area of anxiety disorders. Dr G. Bruder provided insightful comments throughout the process. M.-N. Anthony recruited wave 4 subjects and assisted with coordination and administrative work on wave 4. Dr L. Mufson provided clinical insights on earlier drafts of the paper.
Footnotes
Declaration of Interest
None.
References
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical consideration. Journal of Personality and Social Psychology. 1986;6:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Bechara A, Tranel D, Damasio H, Adolphs R, Rockland C, Damasio AR. Double dissociation of conditioning and declarative knowledge relative to the hippocampus in humans. Science. 1995;269:1115–1118. doi: 10.1126/science.7652558. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Hirshfeld-Becker AH, Faraone SV, Dang D, Jackubowski A, Rosenbaum JF. A controlled longitudinal 5-year follow-up study of children at high and low risk for panic disorder and major depression. Psychological Medicine. 2006;36:1141–1152. doi: 10.1017/S0033291706007781. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Hirshfeld-Becker DR, Henin A, Faraone SV, Fraire M, Henry B, McQuade J, Roesenbaum JF. Developmental trajectories of anxiety disorders in offspring at high risk for panic disorder and major depression. Psychiatry Research. 2007;153:245–252. doi: 10.1016/j.psychres.2007.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin. 1992;111:244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Breiter HC, Etco NL, Whalen P. Response and habituation of the human amygdala during the processing of facial expression. Neuron. 1996;17:875–887. doi: 10.1016/s0896-6273(00)80219-6. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz L, Peterson E. Sex differences in depression: a role for preexisting anxiety. Psychiatry Research. 1995;58:1–12. doi: 10.1016/0165-1781(95)02765-o. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J, Kasen S, Noemi Velez C, Hartmark C, Johnson J, Rojas M, Brook J, Streuning EL. An epidemiological study of disorders in late childhood and adolescence. 1 Age- and gender-specific prevalence. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66:451–460. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- Cole SR, Hernan MA. Fallibility in estimating direct effects. International Journal of Epidemiology. 2002;31:163–165. doi: 10.1093/ije/31.1.163. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society of Britain. 1972;34:187–220. [Google Scholar]
- Cox DR, Oakes D. Analysis of Survival Data. Chapman & Hall; London: 1984. [Google Scholar]
- Davis M. Are different parts of the extended amygdala involved in fear versus anxiety? Biological Psychiatry. 1998;44:1239–1247. doi: 10.1016/s0006-3223(98)00288-1. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: an integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fava M, Uebelacker LA, Alpert JE, Nierenberg AA, Pava JA, Rosenbaum JF. Major depressive subtypes and treatment response. Biological Psychiatry. 1997;42:568–576. doi: 10.1016/S0006-3223(96)00440-4. [DOI] [PubMed] [Google Scholar]
- File SE. The amygdala: anxiety and benzodiazepines. In: Aggleton J, editor. The Amygdala. Oxford University Press; Oxford: 2000. pp. 195–212. [Google Scholar]
- Frodl T, Meisenzahl E, Zetzsche T, Born C, Groll C, Jager M, Leinsinger G, Bottlender R, Hahn K, Möller H-J. Hippocampal changes in patients with a first episode of major depression. American Journal of Psychiatry. 2002a;159:1112–1118. doi: 10.1176/appi.ajp.159.7.1112. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl EM, Zetzsche T, Born C, Jäger M, Groll C, Bottlender R, Leinsinger G, Möller H-J. Larger amygdala volumes in first depressive episode as compared to recurrent major depression and healthy control subjects. Biological Psychiatry. 2003;53:338–344. doi: 10.1016/s0006-3223(02)01474-9. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl E, Zetzsche T, Bottlender R, Born C, Groll C, Jager M, Leinsinger G, Hahn K, Möller H-J. Enlargement of the amygdala in patients with a first episode of major depression. Biological Psychiatry. 2002b;51:708–714. doi: 10.1016/s0006-3223(01)01359-2. [DOI] [PubMed] [Google Scholar]
- Funayama ES, Grillon C, Davis M, Phelps EA. A double dissociation in the affective modulation of startle in humans: effects of unilateral temporal lobectomy. Journal of Cognitive Neuroscience. 2001;13:721–729. doi: 10.1162/08989290152541395. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Kent JM, Sullivan GM, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. American Journal of Psychiatry. 2000;157:493–505. doi: 10.1176/appi.ajp.157.4.493. [DOI] [PubMed] [Google Scholar]
- Gray JA, McNaughton N. An Enquiry into the Functions of the Septo-Hippocampal System. 2. Oxford University Press; Oxford: 2003. The Neuropsychology of Anxiety. [Google Scholar]
- Grillon C. Startle reactivity and anxiety disorders: aversive conditioning, context, and neurobiology. Biological Psychiatry. 2002;52:958–975. doi: 10.1016/s0006-3223(02)01665-7. [DOI] [PubMed] [Google Scholar]
- Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004;29:1765–1781. doi: 10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemero CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Herdade KCP, De Andrade Strauss CV, Junior HZ, De Barros Viana M. Effects of medial amygdala inactivation on a panic-related behavior. Behavioural Brain Research. 2006;172:316–323. doi: 10.1016/j.bbr.2006.05.021. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile onset and adult onset depression. Archives of General Psychiatry. 2002;58:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Mureci P, Williamson D. Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychological Medicine. 2007;37:453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. American Journal of Psychiatry. 2002;159:1133–1145. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. American Journal of Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and generalized anxiety disorder. Same genes, (partly) different environments? Archives of General Psychiatry. 1992;49:716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG. Survival Analysis. Springer-Verlag; New York: 1996. [Google Scholar]
- Kovacs M, Akiskal HS, Gatsonis C, Parrone PL. Childhood onset dysthymia disorder clinical features and prospective naturalistic outcome. Archives of General Psychiatry. 1994;51:365–374. doi: 10.1001/archpsyc.1994.03950050025003. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Gatsonis C, Paulauskas SL, Richards C. Depressive disorders in childhood. IV. A longitudinal study of comorbidity with and risk for anxiety disorders. Archives of General Psychiatry. 1989;46:776–782. doi: 10.1001/archpsyc.1989.01810090018003. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson D, Belanger A, Weissman MM. Best estimate of lifetime diagnosis: a methodological study. Archives of General Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. The Emotional Brain. Simon & Schuster; New York: 1996. [Google Scholar]
- LeDoux JE. Synaptic Self. Viking Penguin; Middlesex: 2002. [Google Scholar]
- Lewinsohn PM, Gotlib IH, Seeley JR. Adolescent psychopathology: IV. Specificity of psychosocial risk factors for depression and substance abuse in older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1221–1229. doi: 10.1097/00004583-199509000-00021. [DOI] [PubMed] [Google Scholar]
- Lin DY, Wei LJ. The robust inference for the proportional hazards model. Journal of the American Statistical Association. 1989;84:1074–1078. [Google Scholar]
- MacMillan S, Szeszko PR, Moore GJ, Madden R, Lorch E, Banerjee P, Rosenberg DR. Increased amygdala:hippocampal volume ratios associated with severity of anxiety in pediatric major depression. Journal of Child and Adolescent Psychopharmacology. 2003;13:65–73. doi: 10.1089/104454603321666207. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Fyer AJ, Klein DF, Endicott J. Schedule for Affective Disorder and Schizophrenia – Lifetime Version modified for the study of anxiety disorders (SADS-LA): rationale and conceptual development. Journal of Psychiatric Research. 1986;20:317–325. doi: 10.1016/0022-3956(86)90034-8. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study. Archives of General Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The comorbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychological Medicine. 2005;35:611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen B. Mplus User’s Guide. 3. Muthen & Muthen; Los Angeles, CA: 1998–2004. [Google Scholar]
- Nieho DL, Kuhar MJ. Benzodiazepine receptors: localization in rat amygdala. Journal of Neuroscience. 1983;3:2091–2097. doi: 10.1523/JNEUROSCI.03-10-02091.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onoe H, Tsukada H, Nishiyama S, Nakanishi S, Inoue O, Langstrom B, Watanabe YA. Subclass of GABAA/benzodiazepine receptor exclusively localized in the limbic system. Neuroreport. 1996;8:117–122. doi: 10.1097/00001756-199612200-00024. [DOI] [PubMed] [Google Scholar]
- Orvaschel H. Structured and semistructured interviews. In: Hersen M, editor. Clinician’s Handbook of Child Behavioral Assessment. Elsevier Academic Press; San Diego: 2006. pp. 159–179. [Google Scholar]
- Parker G, Hadzi-Pavlovic D. Is the female preponderance in major depression secondary to a gender difference in specific anxiety disorders? Psychological Medicine. 2004;34:461–470. doi: 10.1017/s0033291703001181. [DOI] [PubMed] [Google Scholar]
- Phelps EA, O’Connor KJ, Gatenby JC, Gore JC, Grillon C, Davis M. Activation of the left amygdala to a cognitive representation of fear. Nature Neuroscience. 2001;4:437–441. doi: 10.1038/86110. [DOI] [PubMed] [Google Scholar]
- Phillips RG, LeDoux JE. Differential contribution of amygdala and hippocampus to cued and contextual fear conditioning. Behavioral Neuroscience. 1992;106:274–285. doi: 10.1037//0735-7044.106.2.274. [DOI] [PubMed] [Google Scholar]
- Pine D, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Brook J. Adolescent fears as predictors of depression. Biological Psychiatry. 2001;50:721–724. doi: 10.1016/s0006-3223(01)01238-0. [DOI] [PubMed] [Google Scholar]
- Rosenberg DR, MacMaster FP, Mirza Y, Easter PC. Imaging and neurocircuitry of pediatric major depression. Clinical Neuropsychiatry. 2006;3:219–229. [Google Scholar]
- Roth WT. Physiological markers for anxiety: panic disorder and phobias. International Journal of Psychophysiology. 2005;58:190–198. doi: 10.1016/j.ijpsycho.2005.01.015. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S. Modern Epidemiology. 2. Lippincott-Raven; Philadelphia, PA: 1998. [Google Scholar]
- Roy MA, Neale MC, Pedersen NL, Mathe AA, Kendler KS. A twin study of generalized anxiety disorder and major depression. Psychological Medicine. 1995;25:1037–1049. doi: 10.1017/s0033291700037533. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Silberg JL, Rutter M, Eaves L. Genetic and environmental influences on the temporal association between earlier anxiety and later depression in girls. Biological Psychiatry. 2001;49:1040–1049. doi: 10.1016/s0006-3223(01)01161-1. [DOI] [PubMed] [Google Scholar]
- Walker DL, Davis M. Double dissociation between the involvement of the bed nucleus of the stria terminalis and the central nucleus of the amygdala in startle increases produced by conditioned and unconditioned fear. Journal of Neuroscience. 1997;17:9375–9383. doi: 10.1523/JNEUROSCI.17-23-09375.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Fendrich M, Warner V, Wickramaratne PJ. Incidence of psychiatric disorder in offspring at high and low risk for depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:640–648. doi: 10.1097/00004583-199207000-00010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Pruso BA, Sholomskas D. Children of depressed parents: increased psychopathology and early onset of major depression. Archives of General Psychiatry. 1987;44:847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gershon ES, Kidd KK, Pruso BA, Leckman JF, Dibble E, Hamovit J, Thompson DL, Guro JJ. Psychiatric disorders in the relatives of probands with affective disorders. The Yale University–National Institute of Mental Health Collaborative Study. Archives of General Psychiatry. 1984;41:13–21. doi: 10.1001/archpsyc.1984.01790120015003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Myers JK. Affective disorders in a United States community: the use of research diagnostic criteria in an epidemiological survey. Archives of General Psychiatry. 1978;35:1304–1311. doi: 10.1001/archpsyc.1978.01770350030002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: ten years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky D, Grillon C, Bruder G. Offspring at high and low risk for depression: a three generation study. Archives of General Psychiatry. 2005;62:29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- Wickramaratne PJ, Weissman MM. Onset of psychopathology in offspring by developmental phase and parental depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:933–942. doi: 10.1097/00004583-199809000-00013. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatric Scandinavica. 2000;102 (Suppl 406):14–25. [PubMed] [Google Scholar]