Abstract
Itching is a common symptom in dermatologic diseases and causes restless scratching of the skin, which aggravates the condition. The mechanism of the itch sensation, however, is enigmatic. The present study included behavioral tests and electrophysiological recordings from rat dorsal root ganglion (DRG) neurons in vivo to analyze the response to pruritic stimuli induced by topical application of 5-hydroxytryptamine (5-HT) to the skin. Topically applied 5-HT to the rostral back evoked scratching, whereas application of the vehicle did not. Following subcutaneous injection of the opioid receptor antagonist naloxone, the number of scratches decreased, suggesting that the scratching was preferentially mediated by itch but not pain sensation. To elucidate the firing properties of DRG neurons in response to topically applied 5-HT, intracellular recordings were made from DRG neurons in vivo. None of the Aβ and Aδ neurons responded to 5-HT; in contrast, 25 of 91 C neurons (27%) exhibited repetitive firing in response to 5-HT, which could be classified into two firing patterns: one was a transient type, characterized by low firing frequency that decreased within 5 min; the other was a long-lasting type, having high firing frequency that continued increasing after 5 min. The time course of the firing pattern of long-lasting C neurons was comparable to the scratching behavior. Intriguingly, the long-lasting-type neurons had a significantly smaller fast afterhyperpolarization than that of the 5-HT-insensitive neurons. These observations suggest that the long-lasting-firing C neurons in rat DRG sensitive to 5-HT are responsible for conveying pruritic information to the spinal cord.
INTRODUCTION
Itching is an unpleasant sensation that can occasionally degrade the quality of life. There are some similarities between itching and pain; both are unpleasant sensations and most pruritogens, such as histamine, can also produce pain (Dray 1995; Schmelz et al. 2003). The behavioral response in rats or mice to these two types of stimuli, however, has some differences. Itch stimuli evoke scratching or biting, whereas noxious stimuli evoke a withdrawal reflex, flinching, or licking (Kuraishi et al. 1995, 2008; Nojima et al. 2004). Opioids, which are commonly used for alleviation of pain, elicit itching (Hales 1980; Jeon et al. 2005; Maxwell et al. 2005; Slappendel et al. 2000); conversely, the opioid receptor antagonist naloxone enhances pain but inhibits the itch sensation (Metze et al. 1999; Robertson et al. 2008).
To elucidate the characteristics of itch-sensing primary afferents, electrophysiological recordings of these afferents have been made. Microneurography reveals that histamine applied to human skin elicits low-frequency activity in polymodal C fibers (Handwerker et al. 1991; Torebjörk 1974; Van Hees and Gybels 1972). Tuckett and Wei recorded the activity of A and C fibers in cats and found that only polymodal C fibers were activated by the application of cowhage, which is pruritic in humans (Tuckett and Wei 1987a,b). Polymodal C fiber that responds to cowhage is also reported in monkeys (Johanek et al. 2008) and humans (Namer et al. 2008). Histamine-sensitive polymodal C fibers are also responsive to mustard oil, which is known to activate TRPA1, and there is no significant difference in the discharge patterns caused by itching or burning stimuli (Handwerker et al. 1991). A new subtype of C fibers that is insensitive to mechanical stimuli was reported to respond to itch stimuli (Schmelz et al. 1997). However, these fibers also respond to algogens such as capsaicin or bradykinin (Schmelz et al. 2003).
Several chemicals have been used experimentally to elicit the itch sensation. However, the itch-inducing potency of these chemicals differs between species. Histamine, for instance, is a well-known pruritogen in humans. It evokes scratching in ICR mice, hairless guinea pig, and monkeys (Inagaki et al. 2001; Johanek et al. 2008; Woodward et al. 1995), but it is generally less effective in ddY mice and Sprague–Dawley rats (Jinks and Carstens 2002; Kuraishi et al. 1995). Instead of histamine, 5-hydroxytryptamine (5-HT) is often used in mice and rat itch models (Inagaki et al. 2001; Nojima and Carstens 2003a,b; Nojima et al. 2003; Thomsen et al. 2001; Yamaguchi et al. 1999). Interestingly, 5-HT is only weakly pruritic for humans (Schmelz et al. 2003). 5-HT is released from aggregated platelets and mast cells in rats (Weisshaar et al. 1997). 5-HT produces itching when applied to the human skin (Weisshaar et al. 1997) and is considered to be a cause of pruritus accompanied by polycythemia vera (Fitzsimons et al. 1981). In rats, intradermal injection of 5-HT into the rostral back evokes a scratch response and this behavior is depressed by subcutaneous injection of the opioid receptor antagonist naltrexone (Nojima and Carstens 2003a; Nojima et al. 2003). These observations indicate that 5-HT is a potent pruritogen in rats and suitable for clarifying the properties of afferent fibers conveying the itch sensation to the spinal cord.
In the present study, we intended to answer the following questions. 1) What types of primary afferents are responsible for the reaction to topically applied 5-HT on a receptive field? and 2) What is the characteristic feature of itch-sensing neurons? To address these questions, we made intracellular recordings from rat dorsal root ganglion (DRG) neurons in vivo and analyzed the response to itch stimulation induced by topical application of 5-HT to the skin.
METHODS
All experimental procedures involving the use of animals were approved by the Committee on the Ethics of Animal Experiments, Kyushu University, and were in accordance with the Guidelines of the Japanese Physiological Society. All efforts were made to minimize animal suffering and the number of animals used for the studies. At the end of the experiments, the rats were given an overdose of urethane and then exsanguinated.
Behavioral experiments
In all, 43 male Sprague–Dawley rats (aged 6–9 wk) were used. They were housed under controlled temperature and light. Food and water were freely available. The hair of the rostral back, right hindlimb, thigh, and hip was clipped one day before the behavioral experiments. Before the experiments, the animals were placed in an acrylic cage for about 1 h for acclimation. Behavioral changes were recorded by digital video camera for 1 h. On the clipped rostral back, 5-HT (1% [47 mM] in 99% ethanol, 50 μl) and the vehicle (99% ethanol, 50 μl) were applied on the target skin by using a micropipette instead of being injected intradermally, to avoid eliciting pain by inserting a needle and expanding the skin. The number of scratches to the application site by the hindpaw was counted. We used ethanol as the vehicle. Ethanol can activate TRPV1 and is painful on a skin wound. However, we did not believe it would be painful in this study for two reasons. One is that topical application of ethanol is often used in studies on humans and rarely evokes pain (Hatem et al. 2006; Namer et al. 2008; Wasner et al. 2004) and the other is that the amount of penetration of topically applied ethanol to the skin is small (Pendlington et al. 2001). We also applied 1% 5-HT (50 μl) to the right hindpaw and observed biting behavior since the electrophysiological experiments were performed from L4 to L6, mainly L5 DRG neurons, which innervate the hindpaw, thigh, and hip. In mouse itch models, biting behavior was elicited by 5-HT injection or under the condition of chronic dermatitis or dry skin (Kuraishi et al. 2008; Maekawa et al. 2002; Nojima et al. 2004). In contrast, a formalin application, which is known to initiate pain behavior, causes licking in mice (Abbott et al. 1995; Hunskaar et al. 1985; Tjølsen et al. 1992). Thus the biting behavior is considered as itch-related behavior. In some experiments, rats were given a subcutaneous injection of naloxone (1 mg·kg−1) or saline at a volume of 1 ml·kg−1 into the back skin 15 min before the topical application of 5-HT.
Electrophysiological recordings
In all, 88 rats were used for the electrophysiological experiments. After anesthesia of the rats with urethane (1.2 g·kg−1, administered intraperitoneally), laminectomy was performed at the lumbar level and the right DRG (L4–L6, mainly L5) was carefully exposed with a rongeur. Animals were fixed rigidly in a stereotaxic apparatus and then the skin flaps were stretched by nylon fibers to make a pool for perfusion of DRG. Connective tissues covering the surface of the DRG were removed using fine forceps and the exposed DRG was perfused with Krebs solution (in mM: NaCl, 117; KCl, 3.6; CaCl2, 2.5; MgCl2, 1.2; NaH2PO4, 1.2; glucose, 11; and NaHCO3, 25) equilibrated with 95% O2-5% CO2 at 37 ± 1°C. In vivo intracellular recordings were made using 1.5-mm thick-walled, borosilicate glass pipettes filled with a solution containing 4 M potassium acetate or 0.1 M potassium chloride. Tip resistance was 30–60 MΩ with 4 M potassium acetate and 80–150 MΩ with 0.1 M potassium chloride. Microelectrodes with shank and tip that were relatively shorter and larger, respectively, than those for conventional intracellular recordings were used. Although the input resistance of these electrodes was much higher than that of the electrodes containing 3 M potassium chloride, 0.1 M potassium chloride was more suitable for obtaining stable recordings from small C neurons. Signals were amplified using an Axoclamp 2B (Axon Instruments/Molecular Devices, Sunnyvale, CA) in bridge mode. Analogue data were digitized by a Digidata 1440A (Axon Instruments/Molecular Devices) and analyzed by pCLAMP 10 software (Axon Instruments/Molecular Devices). We determined the receptive fields by applying nonnoxious mechanical stimuli with a paint brush or noxious stimuli with toothed forceps. If the neurons were insensitive to either nonnoxious or noxious stimuli, then electrical stimulation with a monopolar electrode was applied for further confirmation of the receptive fields of recorded neurons. If a receptive field was not found, the neurons were discarded. When we recorded more than two neurons from the same animal, we made sure that each neuron had different receptive fields. DRG neurons were classified into three types according to the conduction velocity of the corresponding fiber: C fibers <2.0 ms−1, Aδ fibers 2.0–10 ms−1, and Aβ fibers >10 ms−1, referring to published reports (Lawson and Waddell 1991; McCarthy and Lawson 1989; Pinto et al. 2008; Villière and McLachlan 1996). Conduction velocity was estimated by the length from the stimulating point to the DRG and the latency between onset of electrical stimulation and orthodromic action potential. In some neurons, the mechanical threshold was determined by von Frey filaments. Subsequently, we gently applied the vehicle (ethanol 20 μl) and then 5-HT (serotonin hydrochloride 20 μl; Sigma) on the receptive field by using a micropipette. We observed the activity of the neurons ≥2 min after applying the drugs to evaluate whether they were responsive to the drugs. Capsaicin (0.05% in ethanol 20 μl; Wako) was applied to the receptive fields of eight 5-HT-insensitive neurons. We did not test the effect of capsaicin on 5-HT-sensitive neurons, since we could not exclude the possibility that previously applied 5-HT would redissolve into the capsaicin solution and activate the 5-HT receptors. C neurons that had membrane potential more positive than −50 mV were excluded from further analysis; however, the firing response of those neurons to 5-HT application or mechanical stimuli was included in the present study due to the difficulty in obtaining recordings from C neurons. Neurons showing spontaneous firing without 5-HT or mechanical stimuli were discarded.
Statistical analysis
Total scratching and biting was evaluated by unpaired t-test. Electrophysiological data were evaluated by Mann–Whitney U test or Kruskal–Wallis H test. P < 0.05 was considered significant.
RESULTS
Scratching and biting behavior in response to topically applied 5-HT
Topically applied 5-HT to the rostral back evoked scratching behavior, whereas the vehicle did not (Fig. 1, A and B; n = 8 in each group). The scratching began within 5 min after application of 5-HT and reached a peak within 10 min; the scratching frequency reached 30 scratches per 5 min and then gradually decreased. The scratching behavior lasted for >40 min. There was a significant delay in the beginning of scratching after 5-HT application, probably due to the diffusion time for 5-HT to reach the nerve terminals. The mean total number of scratch bouts in 1 h induced by 5-HT was 197 ± 27 (mean ± SE, n = 8). Following subcutaneous injection of naloxone (1 mg·kg−1), the scratching was reduced to less than one third (Fig. 1C, vehicle 172 ± 38, n = 8; naloxone 51 ± 18, n = 7), which was statistically significant (P < 0.01), suggesting that the scratching is due to itch but not pain sensation. Before performing an intracellular recording analysis, behavioral changes induced by the topically applied 5-HT from the sole to the ankle of the right hindpaw were tested. Rats exhibited biting behavior to the 5-HT-applied region but not to the vehicle-applied region (Fig. 1D; n = 6 each group). The biting time course was similar to the scratching time course (Fig. 1E). These observations further indicate that 5-HT applied at the hindpaw, thigh, or hip also initiates itch sensation in rats.
Fig. 1.
Behavioral response to topically applied 5-hydroxytryptamine (5-HT, serotonin) and vehicle. A: time course of scratching induced by topically applied 1% 5-HT (square) or vehicle (ethanol: circle) to the skin of the rat rostral back. The number of scratching bouts was counted every 5 min (n = 8). B: total number of scratching bouts (n = 8 in each group). **P < 0.01 (unpaired t-test). C: the effect of naloxone. Saline or naloxone (1 mg/kg) was injected subcutaneously 15 min before applying 1% 5-HT (n = 8 saline, n = 7 naloxone). **P < 0.01 (unpaired t-test). D: total number of biting bouts induced by topically applied 1% 5-HT or vehicle (ethanol) to the rat hindpaw (n = 6 in each group). **P < 0.01 (unpaired t-test). Data are presented as the mean and SE.
Response of C neurons to topically applied 5-HT
Intracellular recordings were made from 29 neurons with Aβ, 25 neurons with Aδ, and 91 neurons with C-fiber in L5 DRG in vivo (Table 1). Receptive fields of the recorded neurons were identified by applying mechanical or electrical stimulation to the skin. Subsequently, ethanol (99%, 20 μl) or 5-HT (1%, 20 μl) was applied to the receptive field. Neither Aβ nor Aδ neurons responded to topical application of 5-HT (Table 1). Twenty-five of the 91 C neurons (27%) showed orthodromic firing in response to 5-HT application (Table 1). Vehicle application did not produce firings, except one Aδ neuron and one C neuron, which might be cool-sensitive neurons because they responded to the gentle application of ice.
Table 1.
Summary of the recorded neurons
| 5-HT-Sensitive |
|||
|---|---|---|---|
| Factor | 5-HT-Insensitive | Transient | Long-Lasting |
| A. A β neurons (n = 29) | |||
| Touch | 17 (59%) | 0 | 0 |
| Pinch | 11 (38%) | 0 | 0 |
| Mechanically insensitive | 1 (3%) | 0 | 0 |
| Total | 29 (100%) | 0 | 0 |
| B. Aδ neurons (n = 25) | |||
| Touch | 3 (12%) | 0 | 0 |
| Pinch | 19 (76%) | 0 | 0 |
| Mechanically insensitive | 3 (12%) | 0 | 0 |
| Total | 25 (100%) | 0 | 0 |
| C. C neurons (n = 91) | |||
| Touch | 0 | 1 (1%) | 1 (1%) |
| Pinch | 56 (62%) | 12 (13%) | 11 (12%) |
| Mechanically insensitive | 10 (11%) | 0 | 0 |
| Total | 66 (73%) | 13 (14%) | 12 (13%) |
Figure 2 shows an example of a 5-HT-sensitive C neuron (Fig. 2, A–D were recorded from the same neuron). This neuron was also sensitive to touch (arrows) and pinch stimuli (Fig. 2, A and B). Continuous firing began 32 s after topical application of 5-HT (Fig. 2, A and D) and was recorded for ≤50 min (Fig. 2D). As noticed from the continuous recording (Fig. 2A), action potential was followed by just a small-amplitude afterhyperpolarization (AHP) (Fig. 2C). We classified these neurons as a long-lasting type. These neurons continued to fire for a long time and the peak firing frequency was observed >5 min after 5-HT application. Twelve of the 91 C neurons (13%) were considered to be the long-lasting type and were responsive to noxious stimuli, except one neuron that responded to nonnoxious stimuli (Table 1). We found another type of 5-HT-sensitive C neuron that responded to topically applied 5-HT; however, unlike the long-lasting type, the peak firings were found within 5 min and most of them stopped firing within a few minutes (Fig. 3A). These neurons were sensitive to pinch stimuli (Fig. 3B). We classified these neurons as a transient type and they were also responsive to mechanical stimuli, except for one neuron that responded to nonnoxious stimuli (Table 1). Thirteen C neurons (14%) were considered to be the transient type (Table 1). This type also had a small-amplitude AHP. Figure 4 shows an example trace of a 5-HT-insensitive C neuron. This type of neuron was sensitive to pinch stimuli (Fig. 4B). The 5-HT-insensitive C neurons (73%) were largely sensitive to noxious stimuli, but not to nonnoxious stimuli. A substantial number of 5-HT-insensitive C neurons (11%) were insensitive to mechanical stimuli. 5-HT-insensitive neurons exhibited a relatively large-amplitude AHP, as shown in Fig. 4C.
Fig. 2.
Representative trace of 5-HT-sensitive C neuron (long-lasting type). A, B, C, and D were obtained from the same neuron. A: this neuron was sensitive to touch stimulation. Topical application of vehicle (ethanol) did not evoke action potential. After topical application of 1% 5-HT to the hindpaw, the neuron fired continuously. B: action potential to pinch stimuli. C: single action potential of long-lasting-type C neuron, which was followed by a small-amplitude afterhyperpolarization (AHP). D: continuous firing was recorded for ≤50 min. There was a 20-min time lapse between the 2nd and 3rd traces.
Fig. 3.
Representative trace of 5-HT-sensitive C neuron (transient type). A, B, and C were obtained from the same neuron. A: topical application of vehicle (ethanol) did not evoke action potential. After topical application of 1% 5-HT, spikes were elicited, although the firing ceased within a few minutes. B: action potential initiated by pinch stimuli. C: single action potential of transient-type C neuron. This neuron showed afterdepolarization rather than AHP.
Fig. 4.
Representative trace of 5-HT-insensitive C neuron. A, B, and C were obtained from the same neuron. A: neither vehicle (ethanol) nor 5-HT evoked action potential. B: action potential to pinch stimuli. C: single action potential of 5-HT-insensitive C neuron. The action potential was followed by a large-amplitude AHP.
Firing properties of 5-HT-sensitive neurons in response to 5-HT application
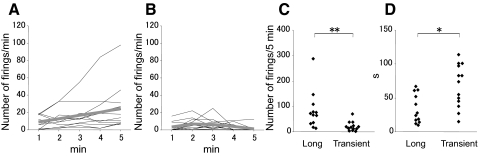
Next, we compared the firing properties of long-lasting and transient-type 5-HT-sensitive C neurons. The long-lasting type showed a continuous increase in the number of firings 5 min after the application of 5-HT (Fig. 5A). On the other hand, the number of firings in the transient type reached a peak within 3 min (median 2.5 min, range 1–3 min, n = 13) and then decreased (Fig. 5B). The long-lasting type exhibited a significantly higher firing rate than that of the transient type in the first 5 min (long-lasting type: median 70 spikes/min, range 15–288 spikes/min, n = 12; transient type: median 18 spikes/min, range 3–70 spikes/min, n = 13; P < 0.01; Fig. 5C). Furthermore, the long-lasting-type neurons began to fire much earlier than the transient firing neurons (long-lasting type: median 26 s, range 12–67 s, n = 12; transient type: median 75 s, range 14–115 s, n = 13; P < 0.05; Fig. 5D).
Fig. 5.
Firing property induced by topically applied 5-HT. A: firing time course of long-lasting-type C neuron. The number of firings is plotted for every minute until 5 min (n = 12). The mean number of firings is shown as a gray line. B: firing time course of transient-type C neuron. The number of firings is plotted for every minute until 5 min (n = 13). The mean number of firings is shown as a gray line. C: total number of firings within 5 min of long-lasting-type neuron (n = 12) and transient-type neuron (n = 13). **P < 0.01 (Mann–Whitney U test). D: latency between application of 5-HT and the first evoked action potential (long-lasting: n = 12; transient: n = 13). *P < 0.05 (Mann–Whitney U test).
Properties of action potential
The conduction velocity of 5-HT-insensitive and -sensitive C neurons was not significantly different. The median velocity was 0.6 ms−1 in 5-HT-insensitive neurons (range 0.3–1.9 ms−1, n = 66), 0.6 ms−1 in transient-type neurons (range 0.5–1.5 ms−1, n = 13), and 0.5 ms−1 in long-lasting-type neurons (range 0.5–0.7 ms−1, n = 12). There were no significant differences in height or duration of action potential among 5-HT-insensitive, transient, and long-lasting types (height, 5-HT-insensitive: median 83.9 mV, range 55.7–104.5 mV, n = 42; transient: median 80.6 mV, range 67.8–93.9 mV, n = 8; long-lasting: median 75.0 mV, range 56.7–102.7 mV, n = 11; duration, 5-HT-insensitive: median 1.6 ms, range 0.9–3.5 ms, n = 42; transient: median 1.6 ms, range 1.3–2.8 ms, n = 8; long-lasting: median 2.4 ms, range 0.8–4.9 mV, n = 11). Interestingly, the long-lasting type had a significantly smaller fast AHP than that of the 5-HT-insensitive and transient types (Fig. 6, A, B, and C; 5-HT insensitive: median 7.8 mV, range 0–16.5 mV, n = 42; transient: median 3.0 mV, range 0–10.0 mV, n = 8; long-lasting: median 0 mV, range 0–5.3 mV, n = 11) and they were significantly different. The long-lasting-type neurons also showed no apparent slow AHP following the fast AHP, even though the action potential had a large Ca2+ component in the falling phase.
Fig. 6.
Comparison of amplitude of AHP among C neurons. A: representative action potential of 5-HT-sensitive long-lasting-type neuron. B: representative action potential of 5-HT-insensitive C neuron. Note that obvious AHP was observed in 5-HT-insensitive C neuron. C: amplitudes of AHP of 5-HT-insensitive neurons (n = 42), 5-HT-sensitive long-lasting neurons (n = 11), and 5-HT-sensitive transient neurons (n = 8) are plotted. Filled circles represent mechanosensitive C neurons and open circles represent mechanoinsensitive C neurons. **P < 0.01 (Kruskal–Wallis H test).
Application of algogenic agents to 5-HT-insensitive C neurons
To clarify whether 5-HT-insensitive C neurons were responsive to algogenic stimuli, we topically applied capsaicin (0.05% in ethanol) to the receptive fields (Fig. 7, A and B). Before capsaicin application, 5-HT was topically applied to test whether a neuron responded to 5-HT (Fig. 7A) and then noxious pinch stimulation was added. The neuron shown in Fig. 7A responded to pinch stimuli but not to 5-HT. In the same neuron, topical application of capsaicin elicited continuous firing lasting for >5 min with long latency (median 62 s, range 46–77 s, n = 2). Two of eight neurons were responsive to capsaicin.
Fig. 7.
Representative trace of 5-HT-insensitive C neuron that responded to pinch stimuli and topically applied capsaicin. A: 5-HT did not evoke firing. B: continuous firing was elicited following topical application of capsaicin to the same neuron.
Location of the receptive fields
Figure 8 shows the location of the receptive fields that we recorded. They were located mostly on the hindpaw and hip. The distribution of long-lasting C neurons, transient C neurons, and 5-HT-insensitive C neurons did not vary.
Fig. 8.
Distribution of the receptive fields of long-lasting-type C neurons (diamond), transient-type C neurons (triangle), and 5-HT-insensitive C neurons (circle).
DISCUSSION
In the present study, intracellular recordings were made from C neurons in rat DRG in vivo to elucidate the firing properties of neurons in response to topically applied 5-HT to the skin, which elicited an itch-associated scratching response in rats. A small population of C neurons responded to the topical application of 5-HT and these 5-HT-responsive C neurons could be divided into two subtypes based on their firing duration, firing rate, and latency of the response. One type of C neurons showed long-lasting firing, higher firing frequency, and short latency. The firing duration was comparable to the behavioral changes induced by 5-HT topically applied to the hindlimb. The other type of C neurons exhibited transient firing that lasted for <5 min, low firing frequency, and long latency. These observations suggest that the long-lasting-type C neurons may express 5-HT receptors on the peripheral nerve endings and play an important role in carrying the itch sensation to the spinal cord in rats. The other possibility is that the shorter delay and longer duration of the 5-HT response could also be due to a higher density of 5-HT receptors.
Several chemicals have been reported to induce the itch sensation, including histamine, 5-HT (Nojima and Carstens 2003a,b; Thomsen et al. 2001; Yamaguchi et al. 1999), substance P (Andoh et al. 1998), trypsin (Ui et al. 2006), and prostaglandin E2 (Neisius et al. 2002). Histamine is the best-known itch mediator in humans, but not in rodents (Kuraishi et al. 1995), whereas 5-HT is a potent pruritogen in rats (Thomsen et al. 2001). In the majority of behavioral studies, 5-HT is administered by intradermal injection, whereas in the present study, topical application was used, which has the advantage of avoiding mechanical pain stimulation induced by intradermal injection. Similar to the results obtained in previous studies, the topical application of 5-HT evoked scratch behavior, which was reduced by prior application of naloxone, known to enhance the sensation of pain. In agreement with this finding, it is well known that intrathecal injection of an opioid initiates an itch sensation that can be blocked by naloxone (Hales 1980; Jeon et al. 2005; Maxwell et al. 2005; Slappendel et al. 2000). When 5-HT was injected into the hindpaw, rats bit the injected region instead of scratching, since it is difficult for them to scratch their hindpaw (Kuraishi et al. 2008). In the itch model that we used in the present study with topical application of 5-HT to the hindpaw, biting behavior was also observed. In contrast, an algogenic agent, such as formalin, applied to the hindpaw initiated licking but not biting behavior, further confirming the effect of 5-HT in eliciting the itch sensation in rats (Abbott et al. 1995; Hunskaar et al. 1985; Tjølsen et al. 1992).
The 5-HT-sensitive long-lasting-firing C neurons started firing earlier than the C neurons of the transient type. This suggests that the long-lasting C-afferent terminals exist at a more superficial layer of the skin than those of the transient type. Numerous fine nerve endings are spread out at a level just below the epidermis (Shelly and Arthur 1957) and free nerve endings in the dermoepidermal junction are regarded as a receptor for itch sensation (Wahlgren 1992). It is reported that patients with atopic dermatitis have an increased number of nerve fibers in the skin (Tobin et al. 1992; Urashima and Mihara 1998) and nerve growth factor–mediated sprouting of nerve fiber is found in patients with contact dermatitis (Kinkelin et al. 2000). These reports support our findings. Interestingly, the onset of scratching response was later than the onset of action potentials of long-lasting neurons. There may be two reasons why scratching appears later: one is that an itchy sensation that produces a behavioral change needs the accumulation of activity of itch-related neurons; the other is that transient-type neurons may transmit painful sensation and they may suppress the itch sensation transiently in the first several minutes. However, we do not have enough evidence at present to make such hypotheses.
In the present study, topically applied 5-HT to the receptive field evoked repetitive firing in a small population of C neurons but not in Aβ and Aδ neurons. Previous electrophysiological observations support the contribution of C-afferent fibers to the itch sensation; for instance, cowhage selectively activates polymodal C fibers in rats and monkeys (Johanek et al. 2008; Tuckett and Wei 1987b) and histamine activates a subset of C fibers in humans (Handwerker et al. 1991; Schmelz et al. 1997, 2003). Recently, it was reported that the histamine-induced itch sensation is mediated by the activation of TRPV1 receptors expressed at C afferents via an arachidonic acid metabolite produced by histamine receptor activation (Shim et al. 2007). These observations are consistent with our findings. However, it is possible that multiple pathways might be responsible for the itch sensation and it is still not clear whether 5-HT-sensitive C neurons belong to the previously reported itch-responsible primary afferents.
From our behavioral study, naloxone inhibited itch-associated scratching behavior. The site of opioid action on the itch sensation pathway has not been identified. It is well known that the μ-receptor agonist DAMGO ([D-Ala, N-Me-Phe, Gly-ol]-enkephalin) applied to the spinal cord inhibits the release of glutamate from the primary afferents, including C fibers (Ikoma et al. 2007; Kohno et al. 1999) and causes membrane hyperpolarization in substantia gelatinosa neurons (Yoshimura and North 1983), indicating that the analgesic effect of opioid is exerted both on the primary afferents and spinal interneurons. In contrast, subcutaneous injection of naltrexone does not affect the activity of cutaneous nerves innervating the chronic dermatitis area (Maekawa et al. 2002). Moreover, neither systemic morphine nor naltrexone affected the 5-HT-evoked c-Fos-like immunoreactivity in the superficial laminae of the spinal dorsal horn, whereas morphine significantly attenuated the intradermal capsaicin-induced immunoreactivity (Nojima et al. 2003). Therefore the μ-opioid receptor may modulate the itch sensation at the supraspinal level; however, further experiments are necessary to reveal how opioid receptors act on itch transmission.
Interestingly, the 5-HT-sensitive long-lasting-firing neurons had a significantly small, fast AHP. In general, nociceptive DRG neurons have a broader action potential than that of low-threshold mechanoreceptive neurons in the same conduction velocity group (Djouhri et al. 1998; Fang et al. 2005; Ritter and Mendell 1992). Nociceptive C neurons have a broader action potential and larger AHP than those of C neurons responsive to nonnoxious stimuli (Djouhri et al. 1998; Fang et al. 2005). The amplitude of AHP observed in this study was smaller than that previously reported (Fang et al. 2005), probably due to the more negative resting membrane potential of C neurons in our study. However, the resting membrane potential in three types of neurons was not significantly different in the present study; therefore the 5-HT-sensitive long-lasting C neurons may have smaller AHP compared with that of 5-HT-insensitive C neurons.
Regarding the issue of whether itch-sensing primary afferents respond to mechanical stimuli, Fang et al. (2005) reported that 54% of C fibers were nociceptors, 11% were nonnociceptors, and 34% were unresponsive to mechanical stimuli. The mechanical threshold of C fiber ranges from 16 to 608 mN (Pogatzki et al. 2002). In the present study, almost all 5-HT-sensitive C neurons responded to mechanical noxious stimuli and several were responsive to nonnoxious stimuli. Thus the 5-HT-sensitive neurons also responded to mechanical stimulation, indicating that the 5-HT-sensitive C neurons are polymodal. In this study, we did not apply thermal stimulation or capsaicin to the receptive fields of 5-HT-sensitive neurons. 5-HT receptor mRNAs were expressed in rat dorsal root ganglion neurons (Nicholson et al. 2003). 5-HT2A induces thermal hyperalgesia in acute injury and inflammation in rats (Tokunaga et al. 1998). Activation of metabotropic 5-HT receptors enhances the TRPV1 function in primary afferent neurons (Ohta et al. 2006). This evidence suggests that 5-HT-sensitive C neurons might be part of the polymodal neurons. Furthermore, we applied capsaicin to the 5-HT-insensitive neurons, 85% of which were activated by noxious mechanical stimuli, and some of them responded to capsaicin (Fig. 7), indicating that the 5-HT-insensitive primary C neurons include polymodal neurons. It is not known from our study whether 5-HT-responsive C neurons are the only pruritogen-sensitive primary afferents. Endopeptidases elicit a pure itch sensation without any wheal or flare (Arthur and Shelley 1955). It was found that itching could be induced by electrical stimulation to the wrist without generating an axon reflex (Ikoma et al. 2005). It has been reported that histamine and another typical itch agent, cowhage, activate separate populations of spinothalamic tract neurons (Davidson et al. 2007), implying that the itch sensation is not mediated by a single system. Recently, it was reported that gastrin-releasing peptide receptors mediate itch sensation in the spinal cord (Sun and Chen 2007). Gastrin-releasing peptide is expressed in a subset of small and medium-sized DRG neurons that are peptidergic unmyelinated fibers (Sun and Chen 2007). Since it is still unknown whether long-lasting-type 5-HT-sensitive C neurons express gastrin-releasing peptide or peptidergic markers such as substance P and calcitonin gene-related peptide, further experiments are needed to answer the question.
The 5-HT receptor subtype responsible for activation of the primary afferent is still unknown. In DRG, the mRNA for 5-HT1B, 5-HT2A, 5-HT2B, 5-HT3B, and 5-HT4 receptors was detected in small-diameter neurons (Nicholson et al. 2003). It is known that 5-HT2A and 5-HT3 receptors have a role in pain sensation (Eschalier et al. 1989; Giordano and Rogers 1989; Okamoto et al. 2002; Tokunaga et al. 1998). In vitro electrophysiological experiments showed that 5-HT modulates the activity of primary afferents. Activation of axonal 5-HT3 receptors enhances membrane excitability and modulates action potential trains in unmyelinated nerve fibers (Lang et al. 2006). Ohta et al. (2006) showed that 5-HT changed TRPV1 functions through the activation of 5-HT2A and 5-HT7 receptors in cultured DRG neurons. It is reported that 5-HT-evoked itching is mediated by 5-HT2 receptors (Nojima and Carstens 2003b; Yamaguchi et al. 1999); however, this study does not indicate the principal receptor for 5-HT-induced itching. Because the latency of firing after topical application of 5-HT was within 1 min in the majority of 5-HT-sensitive long-lasting C neurons, these data may suggest that 5-HT directly activates 5-HT receptors; however, we cannot exclude the possibility that the activation of long-lasting C neurons was mediated by surrounding tissues such as keratinocytes or mast cells with the release of certain chemicals.
In conclusion, the itch-sensing primary afferents might be polymodal C fibers that responded to topically applied 5-HT, resulting in continuous firing for ≤50 min. This long-lasting high-frequency firing was, in part, due to the small amplitude of fast AHP and the absence of slow AHP, even though the neurons had large Ca2+ components in the action potential. The functional significance of the transient-firing neurons evoked by 5-HT has not been clarified in the present study. In view of the fact that 5-HT is also an algesic substance and considering the long duration of the scratching behavior demonstrated in the present study, we assumed that the transient firing observed in a subpopulation of C neurons may be responsible for carrying pain sensation to the spinal dorsal horn.
GRANTS
This work was partly supported by a grant from the Ministry of Health, Labor, and Welfare of Japan.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
We thank T. Oyama and Y. Nakamura from Nippon Shinyaku Co., Ltd. for instruction in behavioral testing and itch stimulation using topical application of 5-HT.
REFERENCES
- Abbott et al., 1995.Abbott FV, Franklin KB, Westbrook RF. The formalin test: scoring properties of the first and second phases of the pain response in rats. Pain 60: 91–102, 1995 [DOI] [PubMed] [Google Scholar]
- Andoh et al., 1998.Andoh T, Nagasawa T, Satoh M, Kuraishi Y. Substance P induction of itch-associated response mediated by cutaneous NK1 tachykinin receptors in mice. J Pharmacol Exp Ther 286: 1140–1145, 1998 [PubMed] [Google Scholar]
- Arthur and Shelley, 1955.Arthur RP, Shelley WB. Experimental evidence for an enzymatic basis for itching in man. Nature 175: 901–902, 1955 [DOI] [PubMed] [Google Scholar]
- Davidson et al., 2007.Davidson S, Zhang X, Yoon CH, Khasabov SG, Simone DA, Giesler GJ., Jr The itch-producing agents histamine and cowhage activate separate populations of primate spinothalamic tract neurons. J Neurosci 27: 10007–10014, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djouhri et al., 1998.Djouhri L, Bleazard L, Lawson SN. Association of somatic action potential shape with sensory receptive properties in guinea pig dorsal root ganglion neurons. J Physiol 513: 857–872, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dray, 1995.Dray A. Inflammatory mediators of pain. Br J Anaesth 75: 125–131, 1995 [DOI] [PubMed] [Google Scholar]
- Eschalier et al., 1989.Eschalier A, Kayser V, Guilbaud G. Influence of a specific 5-HT3 antagonist on carrageenan-induced hyperalgesia in rats. Pain 36: 249–255, 1989 [DOI] [PubMed] [Google Scholar]
- Fang et al., 2005.Fang X, McMullan S, Lawson SN, Djouhri L. Electrophysiological differences between nociceptive and non-nociceptive dorsal root ganglion neurones in the rat in vivo. J Physiol 565: 927–943, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimons et al., 1981.Fitzsimons EJ, Dagg JH, McAllister EJ. Pruritus of polycythaemia vera: a place for pizotifen? (Letter). Br Med J(Clin Res Ed) 283: 277, 1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano and Rogers, 1989.Giordano J, Rogers LV. Peripherally administered serotonin 5-HT3 receptor antagonists reduce inflammatory pain in rats. Eur J Pharmacol 170: 83–86, 1989 [DOI] [PubMed] [Google Scholar]
- Hales, 1980.Hales P. Pruritus after epidural morphine (Letter). Lancet 316: 204, 1980 [DOI] [PubMed] [Google Scholar]
- Handwerker et al., 1991.Handwerker HO, Forster C, Kirchhoff C. Discharge patterns of human C-fibers induced by itching and burning stimuli. J Neurophysiol 66: 307–315, 1991 [DOI] [PubMed] [Google Scholar]
- Hatem et al., 2006.Hatem S, Attal N, Willer JC, Bouhassira D. Psychophysical study of the effects of topical application of menthol in healthy volunteers. Pain 122: 190–196, 2006 [DOI] [PubMed] [Google Scholar]
- Hunskaar et al., 1985.Hunskaar S, Fasmer OB, Hole K. Formalin test in mice, a useful technique for evaluating mild analgesics. J Neurosci Methods 14: 69–76, 1985 [DOI] [PubMed] [Google Scholar]
- Ikoma et al., 2005.Ikoma A, Handwerker H, Miyachi Y, Schmelz M. Electrically evoked itch in humans. Pain 113: 148–154, 2005 [DOI] [PubMed] [Google Scholar]
- Ikoma et al., 2007.Ikoma M, Kohno T, Baba H. Differential presynaptic effects of opioid agonists on Adelta- and C-afferent glutamatergic transmission to the spinal dorsal horn. Anesthesiology 107: 807–812, 2007 [DOI] [PubMed] [Google Scholar]
- Inagaki et al., 2001.Inagaki N, Nagao M, Igeta K, Kawasaki H, Kim JF, Nagai H. Scratching behavior in various strains of mice. Skin Pharmacol Appl Skin Physiol 14: 87–96, 2001 [DOI] [PubMed] [Google Scholar]
- Jeon et al., 2005.Jeon Y, Hwang J, Kang J, Han S, Rhee K, Oh Y. Effects of epidural naloxone on pruritus induced by epidural morphine: a randomized controlled trial. Int J Obstet Anesth 14: 22–25, 2005 [DOI] [PubMed] [Google Scholar]
- Jinks and Carstens, 2002.Jinks SL, Carstens E. Responses of superficial dorsal horn neurons to intradermal serotonin and other irritants: comparison with scratching behavior. J Neurophysiol 87: 1280–1289, 2002 [DOI] [PubMed] [Google Scholar]
- Johanek et al., 2008.Johanek LM, Meyer RA, Friedman RM, Greenquist KW, Shim B, Borzan J, Hartke T, LaMotte RH, Ringkamp M. A role for polymodal C-fiber afferents in nonhistaminergic itch. J Neurosci 28: 7659–7669, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinkelin et al., 2000.Kinkelin I, Mötzing S, Koltenzenburg M, Bröcker EB. Increase in NGF content and nerve fiber sprouting in human allergic contact eczema. Cell Tissue Res 302: 31–37, 2000 [DOI] [PubMed] [Google Scholar]
- Kohno et al., 1999.Kohno T, Kumamoto E, Higashi H, Shimoji K, Yoshimura M. Actions of opioids on excitatory and inhibitory transmission in substantia gelatinosa of adult rat spinal cord. J Physiol 518: 803–813, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuraishi et al., 1995.Kuraishi Y, Nagasawa T, Hayashi K, Satoh M. Scratching behavior induced by pruritogenic but not algesiogenic agents in mice. Eur J Pharmacol 275: 229–233, 1995 [DOI] [PubMed] [Google Scholar]
- Kuraishi et al., 2008.Kuraishi Y, Yageta Y, Konno M, Andoh T, Yamaguchi-Miyamoto T, Nojima H. Intracisternal, but not intrathecal, injection of naloxone inhibits cutaneous itch-related response in mice. Biol Pharm Bull 31: 2143–2135, 2008 [DOI] [PubMed] [Google Scholar]
- Lang et al., 2006.Lang PM, Moalem-Taylor G, Tracey DJ, Bostock H, Grafe P. Activity-dependent modulation of axonal excitability in unmyelinated peripheral rat nerve fibers by the 5-HT(3) serotonin receptor. J Neurophysiol 96: 2963–2971, 2006 [DOI] [PubMed] [Google Scholar]
- Lawson and Waddell, 1991.Lawson SN, Waddell PJ. Soma neurofilament immunoreactivity is related to cell size and fibre conduction velocity in rat primary sensory neurons. J Physiol 435: 41–63, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maekawa et al., 2002.Maekawa T, Yamaguchi-Miyamoto T, Nojima H, Kuraishi Y. Effects of naltrexone on spontaneous itch-associated responses in NC mice with chronic dermatitis. Jpn J Pharmacol 90: 193–196, 2002 [DOI] [PubMed] [Google Scholar]
- Maxwell et al., 2005.Maxwell LG, Kaufmann SC, Bitzer S, Jackson EV, Jr, McGready J, Kost-Byerly S, Kozlowski L, Rothman SK, Yaster M. The effects of a small-dose naloxone infusion on opioid-induced side effects and analgesia in children and adolescents treated with intravenous patient-controlled analgesia: a double-blind, prospective, randomized, controlled study. Anesth Analg 100: 953–958, 2005 [DOI] [PubMed] [Google Scholar]
- McCarthy and Lawson, 1989.McCarthy PW, Lawson SN. Cell type and conduction velocity of rat primary sensory neurons with substance P-like immunoreactivity. Neuroscience 28: 745–753, 1989 [DOI] [PubMed] [Google Scholar]
- Metze et al., 1999.Metze D, Reimann S, Beissert S, Luger T. Efficacy and safety of naltrexone, an oral opiate receptor antagonist, in the treatment of pruritus in internal and dermatological diseases. J Am Acad Dermatol 41: 533–539, 1999 [PubMed] [Google Scholar]
- Namer et al., 2008.Namer B, Kleggetveit IP, Handwerker H, Schmelz M, Jorum E. Role of TRPM8 and TRPA1 for cold allodynia in patients with cold injury. Pain 139: 63–72, 2008 [DOI] [PubMed] [Google Scholar]
- Neisius et al., 2002.Neisius U, Olsson R, Rukwied R, Lischetzki G, Schmelz M. Prostaglandin E2 induces vasodilation and pruritus, but no protein extravasation in atopic dermatitis and controls. J Am Acad Dermatol 47: 28–32, 2002 [DOI] [PubMed] [Google Scholar]
- Nicholson et al., 2003.Nicholson R, Small J, Dixon AK, Spanswick D, Lee K. Serotonin receptor mRNA expression in rat dorsal root ganglion neurons. Neurosci Lett 337: 119–122, 2003 [DOI] [PubMed] [Google Scholar]
- Nojima and Carstens, 2003a.Nojima H, Carstens E. Quantitative assessment of directed hind limb scratching behavior as a rodent itch model. J Neurosci Methods 126: 137–143, 2003a [DOI] [PubMed] [Google Scholar]
- Nojima and Carstens, 2003b.Nojima H, Carstens E. 5-Hydroxytryptamine (5-HT)2 receptor involvement in acute 5-HT-evoked scratching but not in allergic pruritus induced by dinitrofluorobenzene in rats. J Pharmacol Exp Ther 306: 245–252, 2003b [DOI] [PubMed] [Google Scholar]
- Nojima et al., 2004.Nojima H, Cuellar JM, Simons CT, Carstens MI, Carstens E. Spinal c-fos expression associated with spontaneous biting in a mouse model of dry skin pruritus. Neurosci Lett 361: 79–82, 2004 [DOI] [PubMed] [Google Scholar]
- Nojima et al., 2003.Nojima H, Simons CT, Cuellar JM, Carstens MI, Moore JA, Carstens E. Opioid modulation of scratching and spinal c-fos expression evoked by intradermal serotonin. J Neurosci 23: 10784–10790, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohta et al., 2006.Ohta T, Ikemi Y, Murakami M, Imagawa T, Otsuguro K, Ito S. Potentiation of transient receptor potential V1 function by the activation of the metabotropic 5-HT receptors in rat primary sensory neurons. J Physiol 576: 809–822, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto et al., 2002.Okamoto K, Imbe H, Morikawa Y, Itoh M, Sekimoto M, Nemoto K, Senba E. 5-HT2A receptor subtype in the peripheral branch of sensory fibers is involved in the potentiation of inflammatory pain in rats. Pain 99: 133–143, 2002 [DOI] [PubMed] [Google Scholar]
- Pendlington et al., 2001.Pendlington RU, Whittle E, Robinson JA, Howes D. Fate of ethanol topically applied to skin. Food Chem Toxicol 39: 169–174, 2001 [DOI] [PubMed] [Google Scholar]
- Pinto et al., 2008.Pinto V, Derkach VA, Safronov BV. Role of TTX-sensitive and TTX-resistant sodium channels in Aδ- and C-fiber conduction and synaptic transmission. J Neurophysiol 99: 617–628, 2008 [DOI] [PubMed] [Google Scholar]
- Pogatzki et al., 2002.Pogatzki EM, Gebhart GF, Brennan TJ. Characterization of Aδ- and C-fibers innervating the plantar rat hindpaw one day after an incision. J Neurophysiol 87: 721–731, 2002 [DOI] [PubMed] [Google Scholar]
- Ritter and Mendell, 1992.Ritter AM, Mendell LM. Somal membrane properties of physiologically identified sensory neurons in the rat: effects of nerve growth factor. J Neurophysiol 68: 2033–2041, 1992 [DOI] [PubMed] [Google Scholar]
- Robertson et al., 2008.Robertson LJ, Hammond GR, Drummond PD. The effect of subcutaneous naloxone on experimentally induced pain. J Pain 9: 79–87, 2008 [DOI] [PubMed] [Google Scholar]
- Schmelz et al., 1997.Schmelz M, Schmidt R, Bickel A, Handwerker HO, Torebjörk HE. Specific C-receptors for itch in human skin. J Neurosci 17: 8003–8008, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmelz et al., 2003.Schmelz M, Schmidt R, Weidner C, Hilliges M, Torebjörk HE, Handwerker HO. Chemical response pattern of different classes of C-nociceptors to pruritogens and algogens. J Neurophysiol 89: 2441–2448, 2003 [DOI] [PubMed] [Google Scholar]
- Shelley and Arthur, 1957.Shelley WB, Arthur RP. The neurohistology and neurophysiology of the itch sensation in man. AMA Arch Derm 76: 296–323, 1957 [DOI] [PubMed] [Google Scholar]
- Shim et al., 2007.Shim WS, Tak MH, Lee MH, Kim M, Kim M, Koo JY, Lee CH, Kim M, Oh U. Histamine-induced itch and its relationship with pain. J Neurosci 27: 2331–2337, 2007. 17329430 [Google Scholar]
- Slappendel et al., 2000.Slappendel R, Weber EW, Benraad B, van Limbeek J, Dirksen R. Itching after intrathecal morphine. Incidence and treatment. Eur J Anaesthesiol 17: 616–621, 2000 [DOI] [PubMed] [Google Scholar]
- Sun and Chen, 2007.Sun YG, Chen ZF. A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord. Nature 448: 700–703, 2007 [DOI] [PubMed] [Google Scholar]
- Thomsen et al., 2001.Thomsen JS, Petersen MB, Benfeldt E, Jensen SB, Serup J. Scratch induction in the rat by intradermal serotonin: a model for pruritus. Acta Derm Venereol 81: 250–254, 2001 [DOI] [PubMed] [Google Scholar]
- Tjølsen et al., 1992.Tjølsen A, Berge OG, Hunskaar S, Rosland JH, Hole K. The formalin test: an evaluation of the method. Pain 51: 5–17, 1992 [DOI] [PubMed] [Google Scholar]
- Tobin et al., 1992.Tobin D, Nabarro G, Baart de la Faille H, van Vloten WA, van der Putte SC, Schuurman HJ. Increased number of immunoreactive nerve fibers in atopic dermatitis. J Allergy Clin Immunol 90: 613–622, 1992 [DOI] [PubMed] [Google Scholar]
- Tokunaga et al., 1998.Tokunaga A, Saika M, Senba E. 5-HT2A receptor subtype is involved in the thermal hyperalgesic mechanism of serotonin in the periphery. Pain 76: 349–355, 1998 [DOI] [PubMed] [Google Scholar]
- Torebjörk, 1974.Torebjörk HE. Afferent C units responding to mechanical, thermal and chemical stimuli in human non-glabrous skin. Acta Physiol Scand 92: 374–390, 1974 [DOI] [PubMed] [Google Scholar]
- Tuckett and Wei, 1987a.Tuckett RP, Wei JY. Response to an itch-producing substance in cat. I. Cutaneous receptor populations with myelinated axons. Brain Res 413: 87–94, 1987a [DOI] [PubMed] [Google Scholar]
- Tuckett and Wei, 1987b.Tuckett RP, Wei JY. Response to an itch-producing substance in cat. II. Cutaneous receptor populations with unmyelinated axons. Brain Res 413: 95–103, 1987b [DOI] [PubMed] [Google Scholar]
- Ui et al., 2006.Ui H, Andoh T, Lee JB, Nojima H, Kuraishi Y. Potent pruritogenic action of tryptase mediated by PAR-2 receptor and its involvement in anti-pruritic effect of nafamostat mesilate in mice. Eur J Pharmacol 530: 172–178, 2006 [DOI] [PubMed] [Google Scholar]
- Urashima and Mihara, 1998.Urashima R, Mihara M. Cutaneous nerves in atopic dermatitis. A histological, immunohistochemical and electron microscopic study. Virchows Arch 432: 363–370, 1998 [DOI] [PubMed] [Google Scholar]
- Van Hees and Gybels, 1972.Van Hees J, Gybels JM. Pain related to single afferent C fibers from human skin. Brain Res 48: 397–400, 1972 [DOI] [PubMed] [Google Scholar]
- Villière and McLachlan, 1996.Villière V, McLachlan EM. Electrophysiological properties of neurons in intact rat dorsal root ganglia classified by conduction velocity and action potential duration. J Neurophysiol 76: 1924–1941, 1996 [DOI] [PubMed] [Google Scholar]
- Wahlgren, 1992.Wahlgren CF. Pathophysiology of itching in urticaria and atopic dermatitis. Allergy 47: 65–75, 1992 [DOI] [PubMed] [Google Scholar]
- Wasner et al., 2004.Wasner G, Schattschneider J, Binder A, Baron R. Topical menthol: a human model for cold pain by activation and sensitization of C nociceptors. Brain 127: 1159–1171, 2004 [DOI] [PubMed] [Google Scholar]
- Weisshaar et al., 1997.Weisshaar E, Ziethen B, Gollnick H. Can a serotonin type 3 (5-HT3) receptor antagonist reduce experimentally-induced itch? Inflamm Res 46: 412–416, 1997 [DOI] [PubMed] [Google Scholar]
- Woodward et al., 1995.Woodward DF, Nieves AL, Spada CS, Williams LS, Tuckett RP. Characterization of a behavioral model for peripherally evoked itch suggests platelet-activating factor as a potent pruritogen. J Pharmacol Exp Ther 272: 758–765, 1995 [PubMed] [Google Scholar]
- Yamaguchi et al., 1999.Yamaguchi T, Nagasawa T, Satoh M, Kuraishi Y. Itch-associated response induced by intradermal serotonin through 5-HT2 receptors in mice. Neurosci Res 35: 77–83, 1999 [DOI] [PubMed] [Google Scholar]
- Yoshimura and North, 1983.Yoshimura M, North RA. Substantia gelatinosa neurones hyperpolarized in vitro by enkephalin. Nature 305: 529–530, 1983 [DOI] [PubMed] [Google Scholar]