Abstract
Shift work is highly prevalent in industrialized societies (>20%) but, when it includes night work, it has pronounced negative effects on sleep, subjective and physiological sleepiness, performance, accident risk, as well as on health outcomes such as cardiovascular disease and certain forms of cancer. The reason is the conflict between the day oriented circadian physiology and the requirement for work and sleep at the “wrong” biological time of day. Other factors that negatively impact work shift sleepiness and accident risk include long duration shifts greater than 12 hours and individual vulnerability for phase intolerance that may lead to a diagnosis of shift work disorder; i.e., those shift workers with the greatest sleepiness and performance impairment during the biological night and insomnia during the biological day. Whereas some countermeasures may be used to ameliorate the negative impact of shift work on nighttime sleepiness and daytime insomnia (combined countermeasures may be the best available), there seems at present to be no way to eliminate most of the negative effects of shift work on human physiology and cognition.
INTRODUCTION
Work hours that displace sleep to the daytime and work to the nighttime will interfere with the circadian and homeostatic regulation of sleep. Such work hours will in several ways constitute a health problem with respect to sleep and fatigue; cardiovascular disease, accidents, and cancer(1) (also see Litinski, Scheer and Shea in this issue). Here the focus will be sleep and fatigue. The terminology with regard to work that extends outside the day hours is somewhat diffuse and several attempts have been used to classify and bring order to the description of the types of schedules(2). Normally “Shift work” is used to denote work schedules that divide the 24 hours into roughly similar sizes and use three or more teams to provide full 24-hour coverage. The teams can alternate between early morning, afternoon (swing), and night shifts or may work a permanent shift. The latter is more common in the US, whereas rotating shifts dominate in Europe. Shift work is mainly used in the production industry. “Roster work” or other terms are used to denote schedules, which are more irregular but still cover all or most of the 24 hours. Roster work is more common in transport work and health care. Essentially, however, the same conflict occurs between circadian regulation and the sleep/work pattern, as is the case with shift work. For simplicity we will use the term “Shift work” for both of these types. There are also varieties of shift work, which do not infringe on the normal sleep hours. These will not be dealt with here.
Circadian and Homeostatic Regulation of Sleep and Wakefulness
The quality of waking cognition and of sleep is determined to a large extent by circadian and sleep homeostatic brain processes. From a circadian perspective, cognition is optimal during the internal biological day and sleep is optimal during the internal biological night. Homeostatic sleep drive increases with the duration of prior wakefulness, whether due to acute total sleep deprivation or chronic short sleep schedules. Higher homeostatic sleep drive results in impaired cognition, increased sleepiness and increased propensity for sleep. Importantly, these circadian and homeostatic processes interact to influence the quality of waking cognition and of sleep. As will be discussed, shift work schedules often require work to occur during the biological night when the circadian system is promoting sleep, and sleep to occur during the biological day when the circadian system is promoting wakefulness; the resulting misalignment between internal circadian time and the required wakefulness-sleep work-rest schedules leads to impaired wakefulness and disturbed sleep. See Dijk and Archer in this issue for further discussion of the circadian and homeostatic regulation of sleep and wakefulness.
Shift work and sleep
The dominating health problem reported by shift workers is disturbed sleep as acknowledged in early studies(3–5). At least 3/4 of the shift working population is affected (6). Disturbed sleep seems to be the decisive factor with respect to attitude to one’s work hours(7). Findings from a number of questionnaire studies(8) have shown sleep durations around 5–6 hours in relation to the night shift.
Objective assessment of sleep via EEG of rotating shift workers indicates that day sleep is 1–4 hours shorter than night sleep(9–14). Lockely et al showed similar values in interns on call.(15)
Night shifts are reported to result in greater loss of total sleep time than evening and slow rotating shift schedules(14;16;17). While some have argued that permanent night work may have benefits in terms of circadian adjustment to shift work, there is little support for this argument.(18) Rapid shift rotations are reported to be associated with reduced total sleep duration compared to slower rotations (e.g., at least 3 weeks per shift schedule).(16) Rapid counter clockwise rotations appear to especially disrupt sleep immediately prior to the night shift.(19) These effects are thought to be less severe for workers experiencing a clockwise rotation because of the natural tendency of the circadian clock to delay to a later hour(20;21) and increased time between shifts.(22) Some individuals have circadian clock periods that are shorter than 24 h and they would be expected to adapt easier to counterclockwise shift rotations. Prior to a counterclockwise rotation, 80% to 90% of workers nap before the midnight shift, as opposed to only 40% to 60% prior to a clockwise rotation, which may help to ameliorate some of the expected impairments in sleep and sleepiness during a counterclockwise rotation. This interpretation is also consistent with numerous studies demonstrating the beneficial effects of napping among shift workers.(23–27)
Sleep episodes during shift work are terminated after only 4–6 hours with the individual being unable to return to sleep; presumably because the internal circadian clock is promoting wakefulness during the schedule induced circadian misalignment. The sleep loss is primarily taken out of stage 2 sleep (the dominant sleep stage) and stage REM sleep (dream sleep). Stages 3 and 4 ("deep" sleep) do not seem to be affected. The latter changes in sleep architecture during shift work schedules are consistent with the sleep architecture changes observed during restricted sleep schedules(28;29) Furthermore, the time taken to fall asleep (sleep latency) is usually shorter. Night sleep before an early morning shift is also reduced, but the termination is through external means (i.e., awakening with an alarm) and the awakening usually difficult and unpleasant. (30–33). In a rotating system, some of the sleep loss appears to be repaid prior to working the afternoon shift, with sleep durations often extending beyond eight hours.
Interestingly, day sleep does not seem to improve much across a series of night shifts(34) (35). It appears, however, that night workers sleep slightly better (longer) than rotating workers on the night shift(36–38). The same lack of adjustment is reported in subjective sleep reports(39). The assumed explanation for non-adjustment is the conflict with the external light-dark cycle (39). Strict control over exposure to light and darkness can facilitate complete or partial circadian adaptation to permanent night work schedules(40–42). Application of circadian principles to shift work has been demonstrated to adjust the sleep duration, as well as alertness, in real night shift operations on Norwegian oil production platforms(43).
The long term effects of shift work on sleep are rather poorly understood. However, Dumont et al. (44;45) found that the amount of sleep/wake and related disturbances in present day workers were positively related to their previous experience of night work. Guilleminault et al. (46) found an overrepresentation of former shift workers with different clinical sleep/wake disturbances appearing at a sleep clinic. Recently, the first author and colleagues have shown that in pairs of twins discordant on night work exposure, the exposed twin reports somewhat deteriorated sleep quality and health after retirement(47).
As mentioned, disturbed sleep is reported as a major problem in shift work, but it is not clear to what an extent this actually constitutes a problem compared to the effect of an extended time awake or work at the circadian trough.
No study has attempted dissect the relative contributions of these factors in shift work but findings from other types of studies show that the short sleep durations found in shift work (≈6h) may cause meaningful sleepiness or impaired performance in the average shift worker(48–50). It is unknown whether extended sleep, after the night shift or during days off, compensates for prior loss during shift work operations.
In a recent representative health survey it was demonstrated that day and shift workers did not differ on most items of sleep quality questionnaire(51). The only item that did differ significantly was “sufficient sleep”. It was concluded that shift workers don’t consider their sleep “disturbed” more than do day workers. Furthermore, diagnosed insomniacs, with which the results were compared, scored much worse on most items. The lack of difference between shift workers and day workers could possibly be due to shift workers not seeing their sleep as disturbed since their sleep, although short, is consolidated, as documented in the polysomnographical studies listed above. Shift workers also sleep well before an early morning shift, even if the awakening is difficult. They also sleep well after an evening shift. Thus, the diagnosis of chronic insomnia may not be relevant for shift workers per see as their sleep problems are most directly related to their work schedules.
Physiological sleepiness
Whereas short or otherwise impaired sleep may the most common complaint in shift workers, it may be that the amount of sleepiness determines the level of difficulty with shift work. If sleep would be impaired without consequences to alertness it is doubtful that this would be seen as a problem.
In the sleep clinic, the Multiple Sleep Latency Test (MSLT) is considered the gold standard measure of physiological sleepiness. The MSLT is a series of brief nap opportunities provided across the day, typically in 2 hour increments, and the naps are ended after the patient falls asleep as determined by the EEG. The average latency to sleep across the day is then determined. Average latencies below 5 minutes are considered to represent a pathological level of physiological sleepiness(52) that is seen commonly in patients with sleep disorders such as sleep apnea and narcolepsy. An average latency to sleep between 5–10 minutes is considered an intermediate level of sleepiness and average latencies greater than 10 minutes are considered to represent low levels of physiological sleepiness. No study to date has been performed to document the incidence of pathological sleepiness in shift workers at night, but data from simulated shift work studies suggest that average MSLT sleep latencies are lower during the biological night(53;54).
Data from post-night shift bedtimes exist in field studies(9–14). Essentially they indicate short (<5 minutes) latencies, attesting to excessive sleepiness according to clinical criteria(52). Other indicators of physiological sleepiness include EEG measures of alpha (8–12Hz) and theta (4–8 Hz) activity(55) slow eye movements(56)or blink duration(57). In general, alpha is an EEG pattern associated with relaxed wakefulness and increased sleepiness and theta is a sleep EEG pattern. Slow eye movements are commonly seen during the transition from wakefulness to sleep(58). In laboratory studies, alpha and theta EEG activity, as well as slow eye movements and blink duration measures of physiological sleepiness have been shown to be increased when homeostatic sleep drive is high and when wakefulness occurs during the biological night (59).
Physiological measures give strong support to the notion of night shift sleepiness. In an EEG-study of night workers at work (train drivers) it was found that 1/4 showed pronounced increases in alpha (8–12Hz) and theta (4–8Hz) activity, as well as slow eye movements (SEM) towards the early morning but these were absent during day driving(60). The correlations with ratings of sleepiness were quite high (r=.74). In some instances obvious performance lapses, such as driving against a red light, occurred during bursts of slow eye movements (SEM) and of alpha/theta activity. The pattern is very similar in truck drivers during long-haul (8–10h) drives (14;61), and similar results have been demonstrated for aircrew during long haul flights(62) (Figure 4).
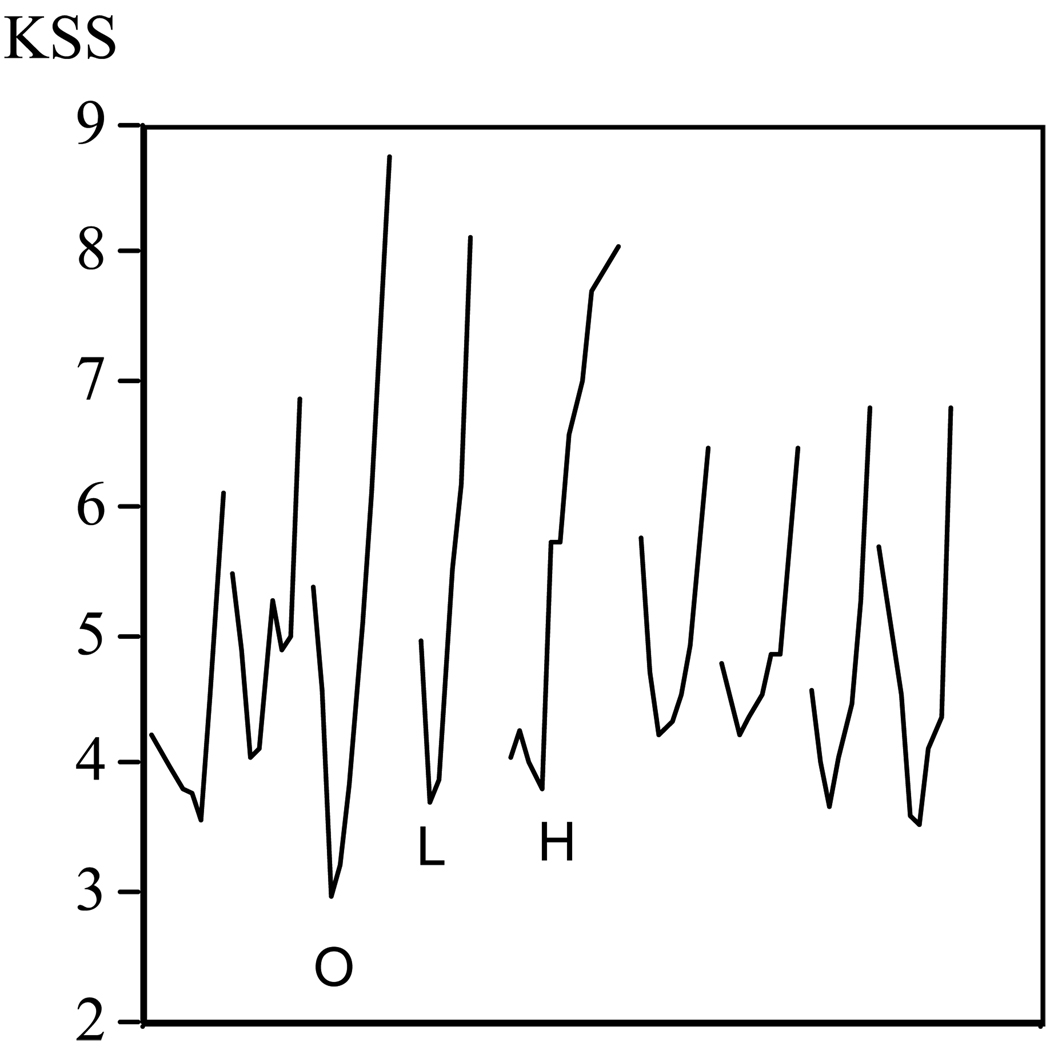
Figure 4.
Mean sleepiness in air crew before, during and after a westward flight across nine time zones (Copenhagen - Los Angelos). O = outbound flight day; L=Layover day in Los Angeles; H = Homebound flight day. Ratings are made from awakening to bedtime.
In process operators there was found not only sleepiness-related increases in alpha and theta activity, but also full-fledged sleep during the night shift(13). Such incidents of sleep proper occurred in approximately ¼ of the subjects. Usually they occurred during the second half of the night shift and never in connection with any other shift. Importantly, sleep on the job was not condoned by the company, nor was there any official awareness that sleep would or could occur during work hours. Interestingly, the subjects were unaware of having slept, but were aware of sleepiness. Furthermore, hospital interns on call showed "attentional failures" (defined as sleep intrusions in the EEG) particularly during early morning work(63). This was reduced when continuous on call duty across days was broken up to permit relatively normal amounts of sleep each day.
Increased alpha and theta activity in the waking EEG have also been demonstrated in truck drivers driving a truck simulator at night(64), in power station operators during a night shift(65), and in shiftworkers driving a simulator home after a normal night shift(66). Findings from these studies also showed large increases in subjective sleepiness. In addition, findings from the driving simulator studies showed impaired performance in the form of increased variation in lateral position on the road. The use of simulated night shift operations is however limited in that it is difficult to truly simulate real world operational demands, interpersonal interactions, and challenges.
Findings from the studies of physiological sleepiness clearly show strong effects of night shifts. It is possible however, that the degree of sleepiness is underestimated since it appears that many individuals start counteracting sleepiness when they start feeling the symptoms. This probably prevents sleepiness to appear in many physiological indicators since EEG and EOG signs of sleepiness only occur at higher levels of sleepiness when the individual is "fighting sleep" and has reached maximum level of sleepiness(56). Thus, physiological changes may occur only when no countermeasures are applied. This is, however, an unsystematic impression by the primary author from natural observations in many studies. Findings from laboratory studies indicate that signs of physiological sleepiness at night are still observed even when using wakefulness promoting countermeasures such as caffeine(67;68).
Subjective sleepiness
Subjective sleepiness is obviously easier to measure than physiological sleepiness. Thus, there is a wealth of results available for inspection. It has sometimes been argued that subjective measures are less valid than other measures. This will be commented on at relevant points below, but it should be emphasized that it is very seldom that objective measures bring an afflicted individual to seek medical help. This is certainly so for insomnia, the diagnosis of which is based on complaints of difficulties initiating and maintaining sleep or of non-restorative sleep(69).
In this context one should also point out that “sleepiness” is not the same thing as “fatigue”, at least not scientifically. It would lead to far to try to introduce strict definitions. However, “sleepiness” refers to the tendency of falling asleep(70). Fatigue may include sleepiness, but also states like physical and mental fatigue. Often the two are interconnected, but they need not be. The issue of the differential definition of sleepiness and fatigue has been subject to a constant debate(46;71). One clinically useful distinction between fatigue and sleepiness is that cognitive and muscle fatigue symptoms may be reduced by sedentary activity or rest without sleeping, whereas subjective sleepiness and the propensity for sleep are often exacerbated by sedentary activity or rest.
There is a wealth of early questionnaire studies suggesting that the overwhelming majority of shift workers experience sleepiness in connection with night shift work, whereas day work is associated with no, or marginal, sleepiness (5;72;73). The studies by Verhaegen (73) and Paley(72) and colleagues reported that fatigue increased on entering and decreased on leaving shift work. In many studies a majority of shift workers admit to having experienced involuntary sleep on the night shift, whereas this less common on day-oriented shifts(74–76).
Between 10 and 20 % report falling asleep during night work. The popular Epworth scale hasn't been used very frequently in relation to shift work but one recent study showed values of 9.2 in night workers, and 8.6 in rotating shift workers, and 8.0 in day workers(77). The differences are small, however, and the Epworth scale(78) in its present form may not be ideal for studying shift work since it contains questions, which often refer to activities that may be difficult to relate to night-time work, such as falling asleep at a red light (while in the drivers seat of a car).
If one wants to obtain a detailed impression of subjective sleepiness in shift work one needs to obtain multiple measurements across each shift and on days off, including during leisure time. When this has been done, the results indicate moderate to high sleepiness during the night shift and no sleepiness at all during the day shifts (30;79;80); again providing evidence that shift work sleepiness is associated with the work schedule and can not be considered a primary sleep disorder of excessive sleepiness that is always present. Below, we show data from studies to illustrate subjective sleepiness at night in the laboratory and during real shift work. We use these studies here since the same self-rating scale of sleepiness has been used in all of them and thus have the possibility of making comparisons. The scale is the Karolinska Sleepiness Scale (KSS) which ranges from 1–9, with 1 = very alert, 3 = rather alert 5 = nether alert nor sleepy, 7 sleepy but no difficulty remaining awake, 9 = very sleepy (fighting sleep, an effort to remain awake)(56). Physiological intrusions of sleep in the EEG or EOG usually starts at level 7 and dominates the recording at level 9. The KSS has been shown to be sensitive to sleepiness due to total sleep deprivation(81) and circadian phase (e.g., Figure 1), chronic sleep loss (82), sleep disorders(83;84), as well as treatment of sleepiness with wakefulness and sleep promoting countermeasures(84;85).
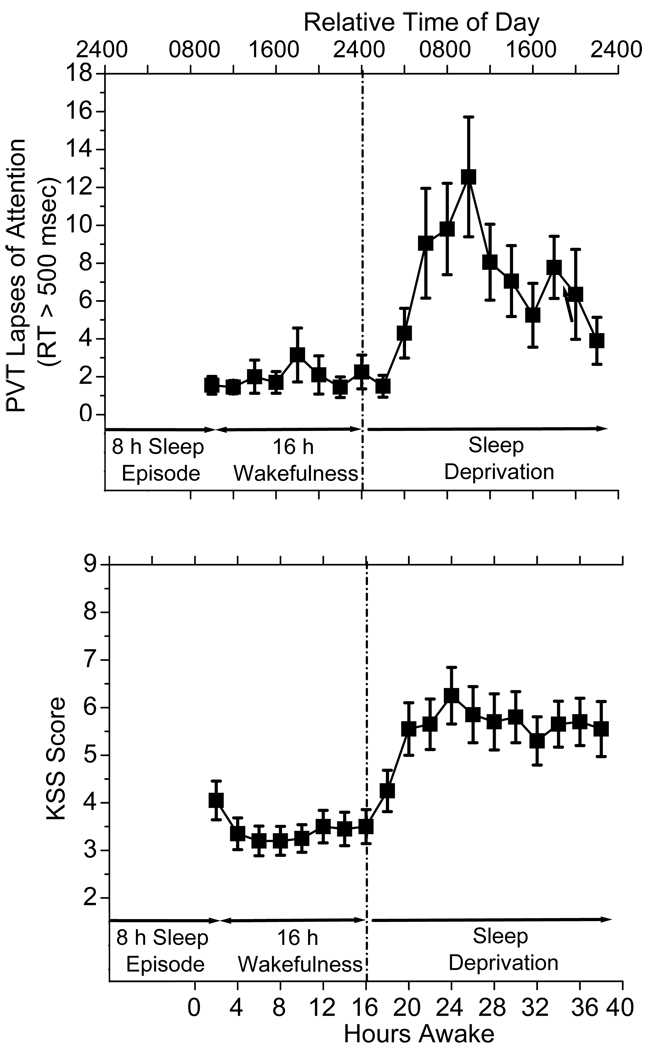
Figure 1.
Subjective sleepiness (KSS) and psychomotor vigilance test performance scores (PVT Lapses of Attention; Reaction times > 500 msec) across 40 hours of total sleep deprivation. As seen, sleepiness and performance lapses are low during the habitual day across the first ~16 hours of wakefulness, whereas thereafter, sleepiness and PVT lapses of attention increase across the habitual night with peaks around 26 hours awake. PVT lapses, and to a lesser extent KSS sleepiness, then improve the next day because the circadian clock promotes wakefulness even though sleep did not occur. These data show what would likely happen to sleepiness and performance on the first night shift in a series if shift workers did not nap prior to the shift.
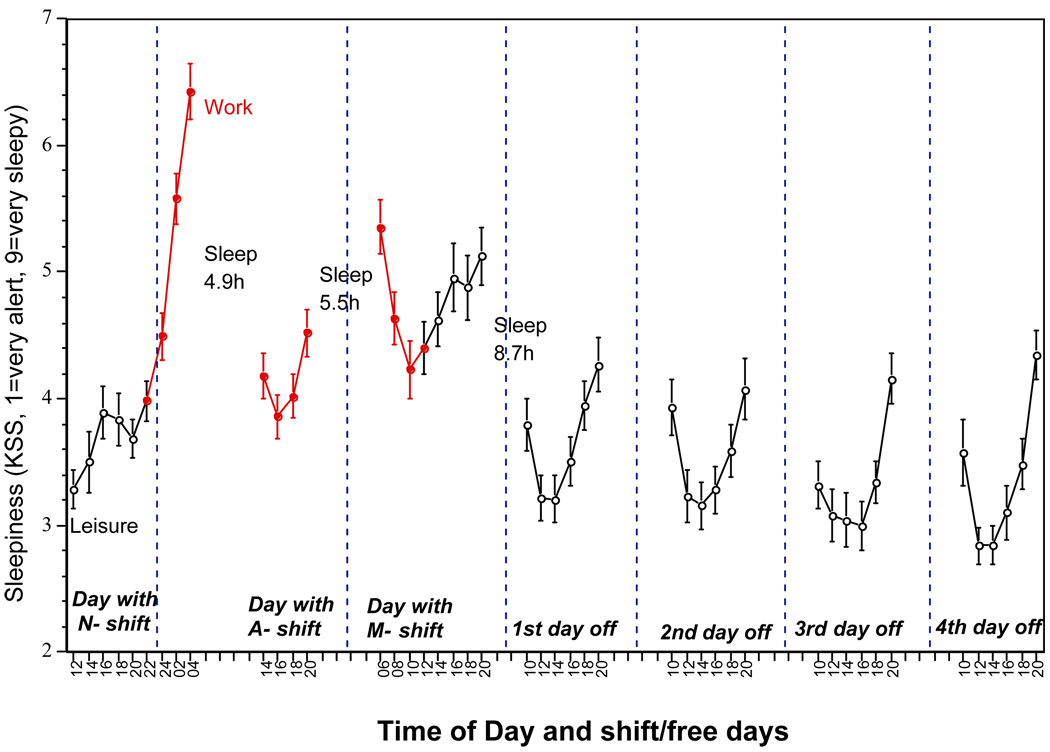
Findings from the first shift work study (Figure 2) show subjective sleepiness ratings in 60 workers in the paper industry working an extremely rapidly rotating shift system with very short rest between the shifts(7). Thus, the schedule started with a night shift (2100h-0600h), followed by 8 hours off, an afternoon shift (1400h–2100h), 8h off, and a morning shift (0600h–1400h). This "triad" was followed by 56 hours off and included two normal night sleeps. The triad pattern was repeated seven times and the cycle ended with 8 days off. The figure shows the last triad, together with the first two days off. Sleepiness rose to high levels during the first night shift (6.5), fell to intermediate levels (4–4.5) during the afternoon shift (after 5.4h of sleep), and reached high levels (5–5.5) again during the morning shift (after 4.5h of sleep). Sleepiness was back to normal levels (mostly < 4) on the first recovery day.
Figure 2.
Subjective sleepiness (KSS) in rapidly rotating shift workers (mean±se). Filled points (grey) indicate sleepiness during work hours.
As suggested above, the morning shift effect seems to be similar to mid-night shift levels but seems, on the other hand, to be present throughout the entire shift (79;86) and may reach very high levels (5–6) when the start-time is earlier than 6am(87). This sleepiness leads to an early afternoon nap in about 1/3 of the workers(88–90). It is interesting that morning work seems to be increasing in many areas, in particular in transport work and in media. One may also consider the effects of traffic congestion in large populated areas resulting in earlier commuting times in order for travelers to reduce travel time.
For comparison, burnout subjects (extreme exhaustion) show daytime values of 5–6, while controls show 3–4, and even lower values during days off(91). Healthy subjects reach levels of 6–7 after five days of 4h night sleep(82).
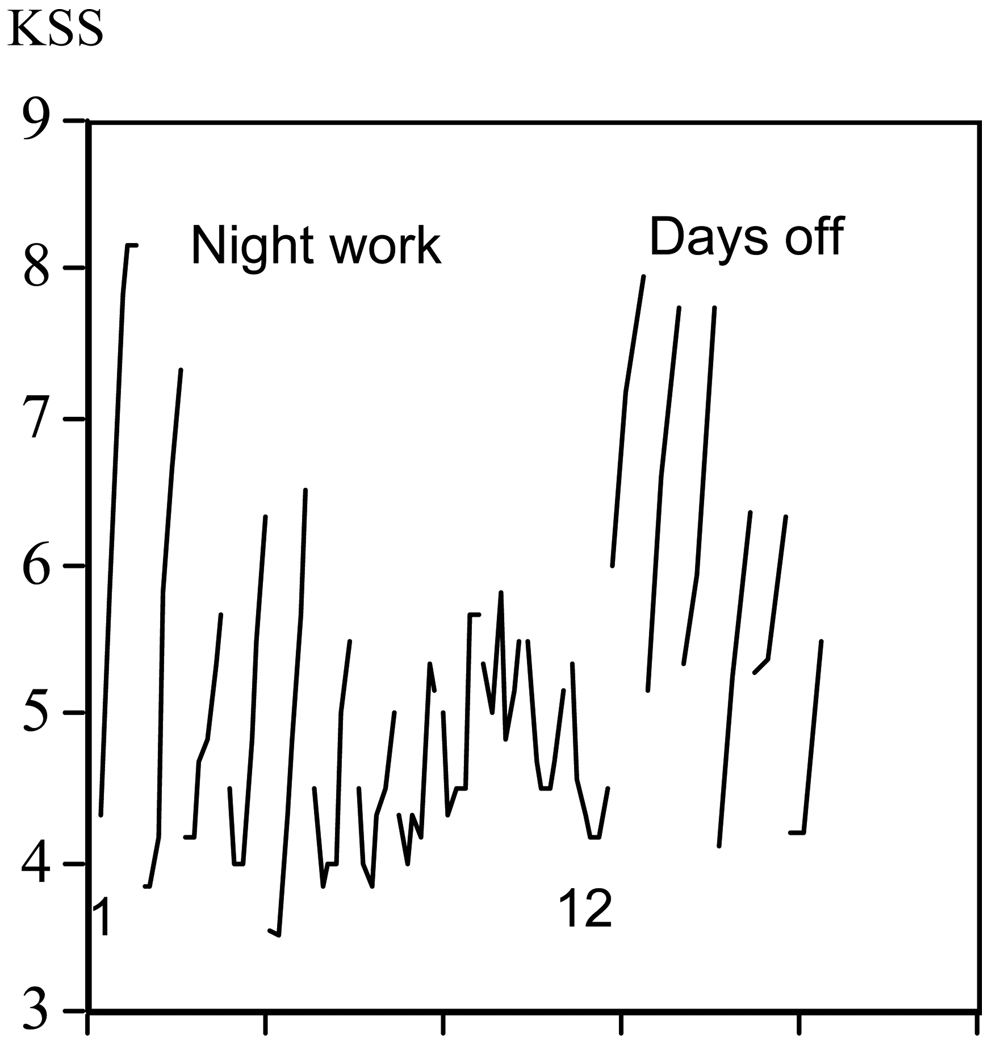
The second shift work illustration (Figure 3) concerns adjustment to night work under rather special circumstances. Adjustment to night shifts normally do not occur because shifts either alternate or because of the exposure to daylight when returning home from the night shift, which counteracts the expected delay of the circadian clock(92). However, when light is not interfering, for example, when night workers are provided with strong sunglasses for the morning commute home, partial adjustment can occur(40;92). This may also be seen in situations when no day-light is present. Figure 3 shows the results from 7 workers on an oil production platform in the North Sea(93). They worked 14 consecutive days between 1900h and 0700h. These were followed by three weeks off. The workers were not exposed to outdoor light since the platform was a self-contained work place in which all aspects of life took place indoors. Figure 3 shows the sleepiness pattern across the working days and the first six days off. Sleepiness reached extremely high levels during the first days, but the pattern gradually changed. In about the middle, the pattern and levels become similar to day work patterns, although at a level of intermediate sleepiness. On return home the pattern was strongly changed again and sleepiness levels remained high for 4–5 days. In fact, daytime levels never seem to reach normal day life levels. Since the study did not include further weeks off it is unclear whether recovery may have proceeded further.
Figure 3.
Mean subjective sleepiness in oil platform workers on 12 night shifts and 6 days off (dashed lines).
The daytime sleep data during the night work schedule showed that the bedtime gradually changed from 0800h to close to 1100h. Similarly, the time of awakening changed from 1700h to 1800h, yielding a sleep length of just below 8h. During the days off a midnight bedtime was adopted throughout, but the time of awakening changed from 0600h to 0800h on day six. Taken together, the results suggest that the circadian system adjusted strongly to night work, although not perfectly, and that the readjustment back to reasonably normal levels took around six days. Indeed, it is possible that even some days more would have been required in order to reach full recovery.
An important question is the implications of the rated sleepiness discussed above. Impaired performance will be discussed below, but is there a level of sleepiness that might be “acceptable” considering a putative right of individuals to lead their lives at reasonable levels of alertness. We suggested above that the KSS-level 5–6 characterized subjects high on burnout (91) and patients with a burnout diagnosis at slightly higher levels.(94) One might also consider the level of sleepiness in individuals with a very negative attitude to shift work in the study by Axelsson et al(7).That group reached a maximum of 7.2 on the night shift, 5.2 on the afternoon shift and 5.9 on the morning shift. The corresponding values for those with a positive attitude was 5.7, 3.9, and 4.8, respectively. Similarly, Czeisler et al. (84) showed that workers diagnosed with shift work disorder (SWD) had a mean KSS value of 7 out of 9 on the night shift. The comparisons attempted here suggest that night shift sleepiness for average shift workers are higher than acceptable and that there are some shift workers with even higher levels of night shift sleepiness.
The effects of shift work on sleepiness are obviously profound, but an important question is whether it is related to the ability to function. This seems to be the case(81;95), although the relation between subjective sleepiness and many performance tasks appears moderate(82;96–102). However, Yang et al have reported that if the self-rating is carried out after a minute of sitting quietly with closed eyes the correlation is increased(103); although it is still moderate. In most studies self-ratings are carried out without any control of the situation leading up to the rating, whereas performance tests are carried out under controlled conditions and with a task load that may unmask sleepiness.
Performance and accidents at work
As may be expected from the effects of shift work on sleepiness, performance and safety are also affected(104). Road transport is the area where the link between safety and night work sleepiness is most pronounced. Thus Harris (105) and Hamelin (106) and Langlois et al. (107) convincingly demonstrated that single vehicle truck accidents have, by far, the greatest probability of occurring at night (early morning). Single vehicle automobile highway accidents are also greatest at night(108–110). Furthermore, The (US) National Transportation Safety board (NTSB) found that 30–40% of all US truck accidents are fatigue related (and grossly underestimated in conventional reports). The latter investigation was extended to search for the immediate causes of fatigue-induced accidents (111). It was found that the most important factor was the amount of sleep obtained during the proceeding 24 hours and split-sleep patterns, whereas the length of time driven seemed to play a minor role.
The NTSB also concluded that the Exxon Valdez accident in 1989 was due to fatigue, caused by reduced sleep and extended work hours (112). The extent of fatal, fatigue-related accidents is considered to lie around 30 per cent (113). This is compared with approximately the same level of incidence in the air-traffic sector, while equivalent accidents at sea are estimated at slightly below 20 per cent.
In industry a classic study is that of Bjerner et al (114) who showed that errors in meter readings over a period of 20 years in a gas works had a pronounced peak on the night shift. There was also a secondary peak during the afternoon. Similarly, Brown (115) demonstrated that telephone operators connected calls considerably slower at night. Woyczak-Jaroszova found that the speed of spinning threads in a textile mill went down during the night(116). From conventional industrial operations less data are available(117;118)but indicate that overall accidents tend to occur, not surprisingly, when activity is at its peak. But these values do not take account of exposure. Findings from other studies show night shift dominance for accidents(119–121), but not all.
It is also believed that the (nighttime) nuclear plant meltdown at Chernobyl was due to human error related to work scheduling(122). Similar observations have been made for the Three Mile Island reactor accident and the near miss incidents at the David Beese reactor in Ohio and at the Rancho Seco reactor in California. These are all anecdotal, however, and very little other data is available.
However, the most carefully executed study, from car manufacturing, seems to indicate a 30–50% increase in accident risk on the night shift(123). Åkerstedt et al (124) showed that fatal occupational accidents were higher in shift workers in a prospective study of shift workers (controlling for physical work load, stress, and other factors). Extended duration work shifts also increase the risk of automobile accidents(125). Recently, a study of interns on call showed that improving rest conditions (maximum 16 consecutive hours of work and 60 hours per week) greatly reduced many types of medical mistakes, of which several were serious(15). The performance decrement during simulated (126) and actual shift work(127) has been compared to the effects of blood alcohol levels of 0.05% and greater.
Several studies have tried to evaluate the costs to society of alertness related accidents and loss of performance (which does not reflect only the costs of shift work). One estimate from the 1990s exceeds $40 billion per year in the United States(128).
Special cases
With regard to shift scheduling there has also been attempts to show that clockwise shift changes should be less negative for performance than counterclockwise ones, but the results are not encouraging(23;129;130). It has also been a continuous discussion of whether permanent shifts are better than rotating ones(16;131–133) This issue has not been resolved. One could also conceive of longer shifts since they would leave more days free for recuperation. This is probably not applicable to all occupation because of too high a work load, but in many studies shifts up to 12h have been shown not to affect performance negatively (79;134–136) and they seem to be very attractive to the employees Findings from other studies however, indicate that shifts 10 hours and greater increase sleepiness(137;138) and risk of accidents(125;136;139).
Shift work (sleep) disorder
As noted above, the effects of shift work are relatively pronounced, for example a reduction of sleep by 1.5–2 hours when working the night shift schedule and considerable sleepiness (reaching 2–3 minutes on average for the MSLT and average subjective sleepiness around 7 on the 1–9 level KSS scale). Clearly some individuals appear to be more negatively afflicted by shift work than others. Thus, there a diagnostic category called “Shift work sleep disorder” (SWSD), also referred to as shift work disorder or shift work type. (DSM IV)(140). SWSD is defined as the "report of difficulty falling asleep, staying asleep, or non-restorative sleep for at least one month”; and it must be associated with "a work period that occurs during the habitual sleep phase”. The International Classification of Sleep Disorders(69) defines the diagnosis of Shift Work Disorder (SWD – “sleep” has been dropped) on four criteria: (1) Complaint of insomnia or excessive sleepiness temporally associated with a recurring work schedule that overlaps the usual time for sleep, (2) symptoms must be associated with the shift work schedule over the course of at least one month, (3) circadian and sleep-time misalignment as demonstrated by sleep log or actigraphical monitoring for 7 days or more and finally (4) sleep disturbance is not explainable by another sleep disorder, a medical or neurological disorder, mental disorder, medication use or substance use disorder.
The prevalence of SWD is not clear since most studies have not used standardized diagnostic criteria of SWD (141). However, one estimate arrives at 10%, using the ICSD-2 criteria (sleep difficulties or sleepiness sometimes or often at a severity level of 6 on a 1–10 scale(77). In another study a figure of 8% were found when using “a very negative or rather negative to present work hours” as a criterion(7).
Czeisler et al. (84) used ICSD-2 SWD criteria with MSLT values <6 minutes during the night to objectively verify excessive nighttime sleepiness, and sleep efficiency of < 87.5% during day sleep (8h Time in Bed) after a night shift to objectively verify daytime insomnia. The resulting group showed a mean MSLT during the night shift of <2 minutes, an average sleepiness rating of ~7 on the Karolinska Sleepiness Scale(56) and average sleep duration of ~6h. MSLT and sleepiness ratings are clearly below what is usually found to be averages in other studies, whereas the sleep duration is similar to most other studies. However, the controlled and soporific laboratory situation may not be representative of the real life situation, at least not with respect to absolute levels of sleepiness.
Countermeasures
The most logical countermeasure of the sleep/wake problems in night work is to discontinue that activity. If that is not possible, there are a number of aspects of scheduling that have been recommended as improvements(7). Among them are clockwise rotation (the sequence of morning-night-afternoon shifts), but the empirical support is rather weak(142). There are, however, some obvious adverse types of schedules that should be avoided. One includes short rest periods between shifts. In many countries 8 hours of rest frequently appears in-between, for example, a night shift and a morning shift. This results in short sleep and sleepiness during work(7;79).
One should probably also avoid several night shifts in succession since sleepiness will accumulate, as will accidents(143). Flexibility and influence on scheduling will have positive effects on sleep(144). Strategic distribution of rest days will improve alertness(135). Rest breaks seem to be efficient barriers to increased accident risk (and presumably sleepiness/fatigue) across the night shift(145). Late changeovers seem preferable to early ones(146).
Education of shift workers is needed regarding good sleep habits and environment, the need for protected time for sleep, as well as recognition of critical times of vulnerability. Among acute countermeasures for night shift fatigue/sleepiness, naps are one possibility(147), but few real life shift work studies are available(24;26;148;149). If naps are used as a countermeasure to shift work induced sleepiness, evidence from laboratory studies suggest that prophylactic naps of 2 hours in duration prior to an overnight (e.g., late afternoon) are more effective at reducing nighttime sleepiness than are 2 hour naps during the night shift(150). The latter is likely due to the negative impact of sleep inertia(151)following a long work shift naps since such naps are likely to include deep slow wave sleep and sleep inertia is worst when awakening from deep sleep. If naps are used during shift work operations, very short naps of <1o minutes may be effective since there is less sleep inertia seen after short naps. Short 10 min naps have been reported to reduce sleepiness during the daytime(152). However, it should be noted that the effectiveness of short naps to reduce sleepiness have not been tested at night.
Sleepiness at night can also be reduced by wakefulness promoting drugs. Caffeine is perhaps the most common self-selected countermeasure used by shift workers. No operational field studies have been performed with caffeine. However, findings from laboratory studies indicate that caffeine can reduce nighttime sleepiness and improve performance(67;149;153) Prophylactic use of caffeine prior to the onset of sleepiness(67;153) appears to be more effective than use of caffeine to reverse sleepiness(154). Recent work on alertness enhancing drugs, like modafinil, is shown to improve nighttime sleepiness in patients with SWD; although clinically significant sleepiness is still present during modafinil treatment(84). Treating healthy shift workers with pharmaceutical products is questionable and the risks associated with treatment need to be weighed against the risks associated with no treatment and/or effectiveness of alternate treatments. The case is probably the same with the “chronobiotic” melatonin(155). Exogenous melatonin has been tried in an actual shift work situation but with moderate success(156). Light treatment is a third possibility, but little applied field work has been carried out, and with modest effects (40–42;153;156–158).
With respect to driving, rolling down a window, turning on the radio, stopping for exercise have been tried in simulator studies without success(159). Interestingly, a recent study by Anund et al (160) showed that hitting a so called “rumble strip” due do sleepiness only brings back alertness (physiological, behavioral) for 1–2 minutes. The sleepiness returns to pre-hit levels.
Perhaps the most effective way of promoting wakefulness at night is through the use of combined countermeasures. In laboratory studies assessing nighttime performance, it has been demonstrated that combinations of bright light and caffeine, naps and caffeine, as well as naps and modafinil improve cognitive performance and alertness at night more than either treatment alone(149;153;154;161).
CONCLUSION
Shift work that includes the night will have pronounced negative effects on sleep, sleepiness, performance and accident risk. Misalignment between internal circadian physiology and the required work schedule is thought to be a primary cause of shift work schedule induced sleepiness and sleep disruption. Wakefulness and sleep promoting countermeasures can provide some help to reduce sleepiness and improve sleep, but as of date there are no effective treatments that can counteract all of the negative impact that shift work schedules have on human physiology and behavior. Additional research is necessary to determine why some individuals have particular vulnerability to nighttime sleepiness and daytime insomnia. In addition, more research is needed to develop effective countermeasures for both sleepiness and insomnia associated with shift work, as shift work is now an important and established component of local and world economies.
Acknowledgments
KPW was funded by grants from the NIH HL081761 and National Space Biomedical Research Institute Cooperative Agreement NCC 9-58-202 with NASA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53(2):103–108. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- 2.Knauth P. Categories and parameters of shiftwork systems. In: Colquhoun WP, Costa G, Folkard S, Knauth P, editors. Shiftwork: Problems and solutions. Frankfurt am Main: Peter Lang GmbH; 1996. pp. 17–28. [Google Scholar]
- 3.Aanonsen A. Shift work and health. OSLO: Universitetsforlaget; 1964. [Google Scholar]
- 4.Tune GS. A note on the sleep of shift workers. Ergonomics. 1968;11(2):183–184. doi: 10.1080/00140136808930955. [DOI] [PubMed] [Google Scholar]
- 5.Andersen JE. Three-Shift Work. Copenhagen: Social forsknings instituet; 1970. [Google Scholar]
- 6.Åkerstedt T. Sleepiness as a consequence of shift work. Sleep. 1988;11:17–34. doi: 10.1093/sleep/11.1.17. [DOI] [PubMed] [Google Scholar]
- 7.Axelsson J, Akerstedt T, Kecklund G, Lowden A. Tolerance to shift work-how does it relate to sleep and wakefulness? Int Arch Occup Environ Health. 2004;77(2):121–129. doi: 10.1007/s00420-003-0482-1. [DOI] [PubMed] [Google Scholar]
- 8.Pilcher JJ, Schoeling SE, Prosansky CM. Self-report sleep habits as predictors of subjective sleepiness. Behav Med. 2000;25(4):161–168. doi: 10.1080/08964280009595745. [DOI] [PubMed] [Google Scholar]
- 9.Foret J, Lantin G. The sleep of train drivers: An example of the effects of irregular work schedules on sleep. In: Colquhoun WP, editor. Aspects of Human Efficiency. Diurnal Rhythm and Loss of Sleep. London: The English Universities Press Ltd; 1972. pp. 273–281. [Google Scholar]
- 10.Foret J, Benoit O. [Sleep patterns of workers on rotating shifts] Electroencephalogr Clin Neurophysiol. 1974;37(4) doi: 10.1016/0013-4694(74)90109-6. 377-44. [DOI] [PubMed] [Google Scholar]
- 11.Matsumoto K. Sleep patterns in hospital nurses due to shift work: An EEG study. Waking and Sleeping. 1978;2:169–173. [Google Scholar]
- 12.Tilley A, Wilkinson RT, Drud M. Night and Shift Work: Biological and Social Aspects. Oxford: Pergamon Press; 1981. Night and day shifts compared in terms of the quality and quantity of sleep recorded in hte home and performance measures at work: a pilot study; pp. 187–196. [Google Scholar]
- 13.Torsvall L, Akerstedt T, Gillander K, Knutsson A. Sleep on the night shift: 24-hour EEG monitoring of spontaneous sleep/wake behavior. Psychophysiol. 1989;26(3):352–358. doi: 10.1111/j.1469-8986.1989.tb01934.x. [DOI] [PubMed] [Google Scholar]
- 14.Mitler MM, Miller JC, Lipsitz JJ, Walsh JK, Wylie CD. The sleep of long-haul truck drivers. N Engl J Med. 1997;337(11):755–761. doi: 10.1056/NEJM199709113371106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lockley SW, cronin JW, Evans EE, Cade BE, lee CJ, landrigan CP, et al. Effect of Reducing Interns' Weekly Work Hours on Sleep and Attentional Failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 16.Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23(2):155–163. [PubMed] [Google Scholar]
- 17.Park YM, Matsumoto PK, Seo YJ, Cho YR, Noh TJ. Sleep-wake behavior of shift workers using wrist actigraph. Psychiatry Clin Neurosci. 2000;54(3):359–360. doi: 10.1046/j.1440-1819.2000.00714.x. [DOI] [PubMed] [Google Scholar]
- 18.Folkard S. Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm. Chronobiol Int. 2008;25(2):215–224. doi: 10.1080/07420520802106835. [DOI] [PubMed] [Google Scholar]
- 19.Signal TL, Gander PH. Rapid counterclockwise shift rotation in air traffic control: effects on sleep and night work. Aviat Space Environ Med. 2007;78(9):878–885. [PubMed] [Google Scholar]
- 20.Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284(5423):2177–2181. doi: 10.1126/science.284.5423.2177. [DOI] [PubMed] [Google Scholar]
- 21.Wright KP, Jr, Hughes RJ, Kronauer RE, Dijk D-J, Czeisler CA. Intrinsic near-24-hour pacemaker period determines limits of circadian entrainment to a weak synchronizer in humans. Proc Natl Acad Sci U S A. 2001;98(24):14027–14032. doi: 10.1073/pnas.201530198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Czeisler CA, Mooreede MC, Coleman RM. Rotating Shift Work Schedules That Disrupt Sleep Are Improved by Applying Circadian Principles. Science. 1982;217(4558):460–463. doi: 10.1126/science.7089576. [DOI] [PubMed] [Google Scholar]
- 23.Cruz C, Boquet A, Detwiler C, Nesthus T. Clockwise and counterclockwise rotating shifts: effects on vigilance and performance. Aviat Space Environ Med. 2003;74(6 Pt 1):606–614. [PubMed] [Google Scholar]
- 24.Garbarino S, Mascialino B, Antonietta M, Squarcia S, De Carli F, Nobili L, et al. Professional shiftwork drivers adopting prophylactic naps can reduce the risk of car accidents during night work. Sleep. 2004 doi: 10.1093/sleep/27.7.1295. [DOI] [PubMed] [Google Scholar]
- 25.Rosekind MR, Smith RM, Miller DL, Co EL, Gregory KB, Webbon LL, et al. Alertness management: strategic naps in operational settings. J Sleep Res. 1995;4(S2):62–66. doi: 10.1111/j.1365-2869.1995.tb00229.x. [DOI] [PubMed] [Google Scholar]
- 26.Smith-Coggins R, Howard SK, Mac DT, Wang C, Kwan S, Rosekind MR, et al. Improving alertness and performance in emergency department physicians and nurses: the use of planned naps. Ann Emerg Med. 2006;48(5):596–604. doi: 10.1016/j.annemergmed.2006.02.005. 604. [DOI] [PubMed] [Google Scholar]
- 27.Signal TL, Gander PH, Anderson H, Brash S. Scheduled napping as a countermeasure to sleepiness in air traffic controllers. J Sleep Res. 2009;18(1):11–19. doi: 10.1111/j.1365-2869.2008.00702.x. [DOI] [PubMed] [Google Scholar]
- 28.Webb WB, Agnew HW., Jr Sleep: effects of a restricted regime. Science. 1965;150:1745–1747. doi: 10.1126/science.150.3704.1745. [DOI] [PubMed] [Google Scholar]
- 29.Akerstedt T, Gillberg M. A dose-response study of sleep loss and spontaneous sleep termination. Psychophysiol. 1986;23(3):293–297. doi: 10.1111/j.1469-8986.1986.tb00635.x. [DOI] [PubMed] [Google Scholar]
- 30.Tilley AJ, Wilkinson RT, Warren PSG, Watson B, Drud M. The sleep and performance of shift workers. Hum Factors. 1982;24:629–641. doi: 10.1177/001872088202400601. [DOI] [PubMed] [Google Scholar]
- 31.Dahlgren K. Adjustment of circadian rhythms and EEG sleep functions to day and night sleep among permanent nightworkers and rotating shiftworkers. Psychophysiol. 1981;18(4):381–391. doi: 10.1111/j.1469-8986.1981.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 32.Akerstedt T, Kecklund G, Knutsson A. Spectral analysis of sleep electroencephalography in rotating three-shift work. Scand J Work Environ Health. 1991;17(5):330–336. doi: 10.5271/sjweh.1694. [DOI] [PubMed] [Google Scholar]
- 33.Kecklund G. Sleep and alertness: Effects of shift work, early rising, and the sleep environment. Stress Research Report. 1996:252. [Google Scholar]
- 34.Foret J, Benoit O. Shiftwork: The level of adjustment to schedule reversal by a sleep study. Waking and Sleeping. 1978;2:107–112. [Google Scholar]
- 35.Dahlgren K. Long-term adjustment of circadian rhythms to a rotating shiftwork schedule. Scand J Work Environ Health. 1981;7(2):141–151. doi: 10.5271/sjweh.2555. [DOI] [PubMed] [Google Scholar]
- 36.Kripke DF, Cook B, Lewis OF. Sleep of night workers: EEG recordings. Psychophysiol. 1970;7(3):377–384. doi: 10.1111/j.1469-8986.1970.tb01762.x. [DOI] [PubMed] [Google Scholar]
- 37.Bryden G, Holdstock TL. Effects of night duty on sleep patterns of nurses. Psychophysiol. 1973;10(1):36–42. doi: 10.1111/j.1469-8986.1973.tb01080.x. [DOI] [PubMed] [Google Scholar]
- 38.Tepas DI, Walsh JK, Moss PD, Armstrong D. Polysomnographic correlates of shift worker performance in the laboratory. In: Reinberg A, Vieux N, Andlauer P, editors. Night and Shift Work: Biological and Social Aspects. Oxford: Pergamon Press; 1981. pp. 179–186. [Google Scholar]
- 39.Akerstedt T. Adjustment of Physiological Circadian Rhythms and the Sleep-Wake Cycle to Shiftwork. In: Folkard S, Monk TH, editors. Hours of Work. John Wiley and Sons Ltd; 1985. pp. 185–197. [Google Scholar]
- 40.Smith MR, Eastman CI. Night shift performance is improved by a compromise circadian phase position: study 3. Circadian phase after 7 night shifts with an intervening weekend off. Sleep. 2008;31(12):1639–1645. doi: 10.1093/sleep/31.12.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Horowitz TS, Cade BE, Wolfe JM, Czeisler CA. Efficacy of bright light and sleep/darkness scheduling in alleviating circadian maladaptation to night work. American Journal of Physiology-Endocrinology and Metabolism. 2001;281(2):E384–E391. doi: 10.1152/ajpendo.2001.281.2.E384. [DOI] [PubMed] [Google Scholar]
- 42.Boivin DB, James FO. Circadian adaptation to night-shift work by judicious light and darkness exposure. J Biol Rhythms. 2002;17(6):556–567. doi: 10.1177/0748730402238238. [DOI] [PubMed] [Google Scholar]
- 43.Bjorvatn B, Stangenes K, Oyane N, Forberg K, Lowden A, Holsten F, et al. Subjective and objective measures of adaptation and readaptation to night work on an oil rig in the North Sea. Sleep. 2006;29(6):821–829. doi: 10.1093/sleep/29.6.821. [DOI] [PubMed] [Google Scholar]
- 44.Dumont M, Montplaisi J, Infante-Rivard C. Insomnia symptoms in nurses with former permanent nightwork experience. In: Koella WP, Obal F, Schultz H, Visser P, editors. Sleep '86. Stuttgart: Gustav Fischer Verlag; 1988. pp. 405–406. [Google Scholar]
- 45.Dumont M, Montplaisir J, Infante-Rivard C. Sleep Quality of Former Night-shift Workers. Int J Occup Environ Health. 1997;3 Supplement 2:S10–S14. [PubMed] [Google Scholar]
- 46.Dement WC, Hall J, Walsh JK. Tiredness versus sleepiness: semantics or a target for public education? Sleep. 2003;26(4):485–486. [PubMed] [Google Scholar]
- 47.Ingre M, Akerstedt T. Effect of accumulated night work during the working lifetime, on subjective health and sleep in monozygotic twins. J Sleep Res. 2004;13(1):45–48. doi: 10.1111/j.1365-2869.2004.00390.x. [DOI] [PubMed] [Google Scholar]
- 48.Wilkinson RT, Edwards RS, Haines E. Performance following a night of reduced sleep. Psychon.Sci. 1966;5(471):472. [Google Scholar]
- 49.Roehrs T, Burduvali E, Bonahoom A, Drake C, Roth T. Ethanol and sleep loss: A "Dose" comparison of impairing effects. Sleep. 2003;26(8):981–985. doi: 10.1093/sleep/26.8.981. [DOI] [PubMed] [Google Scholar]
- 50.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 51.Akerstedt T, Ingre M, Broman JE, Kecklund G. Disturbed sleep in shift workers, day workers, and insomniacs. Chronobiol Int. 2008;25(2):333–348. doi: 10.1080/07420520802113922. [DOI] [PubMed] [Google Scholar]
- 52.Roehrs T, Roth T. Multiple Sleep Latency Test: technical aspects and normal values. J Clin Neurophysiol. 1992;9(1):63–67. [PubMed] [Google Scholar]
- 53.Porcu S, Bellatreccia A, Ferrara M, Casagrande M. Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo. Sleep. 1997;20(7):535–541. doi: 10.1093/sleep/20.7.535. [DOI] [PubMed] [Google Scholar]
- 54.Muehlbach MJ, Walsh JK. The effects of caffeine on simulated night-shift work and subsequent daytime sleep. Sleep. 1995;18(1):22–29. doi: 10.1093/sleep/18.1.22. [DOI] [PubMed] [Google Scholar]
- 55.Santamaria J, Chiappa KH. The EEG of drowsiness in normal adults. J Clin Neurophysiol. 1987;4(4):327–382. doi: 10.1097/00004691-198710000-00002. [DOI] [PubMed] [Google Scholar]
- 56.Akerstedt T, Gillberg M. Subjective and Objective Sleepiness in the Active Individual. International Journal of Neuroscience. 1990;52(1–2):29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 57.Wierwille WW, Ellsworth LA. Evaluation of driver drowsiness by trained raters. Accid Anal Prev. 1994;26(5):571–581. doi: 10.1016/0001-4575(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 58.Ogilvie RD, McDonagh DM, Stone SN, Wilkinson RT. Eye movements and the detection of sleep onset. Psychophysiol. 1988;25(1):81–91. doi: 10.1111/j.1469-8986.1988.tb00963.x. [DOI] [PubMed] [Google Scholar]
- 59.Cajochen C, Khalsa SBS, Wyatt JK, Czeisler CA, Dijk D-J. EEG and ocular correlates of circadian melatonin phase and human performance decrements during sleep loss. Am J Physiol. 1999;277:R640–R649. doi: 10.1152/ajpregu.1999.277.3.r640. [DOI] [PubMed] [Google Scholar]
- 60.Torsvall L, Akerstedt T. Sleepiness on the job: continuously measured EEG changes in train drivers. Electroencephalogr Clin Neurophysiol. 1987;66(6):502–511. doi: 10.1016/0013-4694(87)90096-4. [DOI] [PubMed] [Google Scholar]
- 61.Kecklund G, Akerstedt T. Sleepiness in long distance truck driving: an ambulatory EEG study of night driving. Ergonomics. 1993;36(9):1007–1017. doi: 10.1080/00140139308967973. [DOI] [PubMed] [Google Scholar]
- 62.Rosekind MR, Graeber RC, Dinges DF, Connel LJ, Rountree MS, Gillen K. Crew factors in flight operations IX: Effects of planned cockpit rest on crew performance and alertness in longhaul operations. Moffett Field, CA: NASA Technical Memorandum; 1995. Technical Memorandum No. A-94134. [Google Scholar]
- 63.landrigan CP, Rothschild JW, Conin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of Reducing Interns' Work Hours on Serious Medical Errors in Intensive Care Units. N Engl J Med. 2004;351(18):1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 64.Gillberg M, Kecklund G, Akerstedt T. Sleepiness and performance of professional drivers in a truck simulator--comparisons between day and night driving. J Sleep Res. 1996;5(1):12–15. doi: 10.1046/j.1365-2869.1996.00013.x. [DOI] [PubMed] [Google Scholar]
- 65.Gillberg M, Kecklund G, Goransson B, Akerstedt T. Operator performance and signs of sleepiness during day and night work in a simulated thermal power plant. International Journal of Industrial Ergonomics. 2003;31(2):101–109. [Google Scholar]
- 66.Akerstedt T, Peters B, Anund A, Kecklund G. Impaired alertness and performance driving home from the night shift: a driving simulator study. J Sleep Res. 2005;14(1):17–20. doi: 10.1111/j.1365-2869.2004.00437.x. [DOI] [PubMed] [Google Scholar]
- 67.Walsh JK, Muehlbach MJ, Schweitzer PK. Hypnotics and caffeine as countermeasures for shiftwork-related sleepiness and sleep disturbance. J Sleep Res. 1995;4(S2):80–83. doi: 10.1111/j.1365-2869.1995.tb00233.x. [DOI] [PubMed] [Google Scholar]
- 68.Schweitzer PK, Muehlbach MJ, Walsh JK. Countermeasures for Night Work Performance Deficits -the Effect of Napping Or Caffeine on Continuous Performance at Night. Work and Stress. 1992;6(4):355–365. [Google Scholar]
- 69.American Academy of Sleep Medicine. The International Classification of Sleep Disorders (ICSD) 2nd Edition. Chicago: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 70.Dement WC, Carskadon MA. Current perspectives on daytime sleepiness: the issues. Sleep. 1982;5 Suppl 2:S56–S66. doi: 10.1093/sleep/5.s2.s56. [DOI] [PubMed] [Google Scholar]
- 71.Horne T. The semantics of sleepiness. Sleep. 2003;26(6):763. [PubMed] [Google Scholar]
- 72.Paley MJ, Tepas DI. Fatigue and the shiftworker: firefighters working on a rotating shift schedule. Hum Factors. 1994;36(2):269–284. doi: 10.1177/001872089403600208. [DOI] [PubMed] [Google Scholar]
- 73.Verhaegen P, Maasen A, Meers A. Biological Rhythms and Shift Work. New York: Spectrum; 1981. Health problems in shift workers; pp. 271–282. [Google Scholar]
- 74.Prokop O, Prokop L. Ermüdung und einschlafen am steuer {Fatigue and falling asleep in driving] Zbl.Verkehrsmed. 1955;1:19–30. [PubMed] [Google Scholar]
- 75.Coleman RM, Dement WC. Falling asleep at work: a problem for continous operations. Sleep Research. 1986;15:265. [Google Scholar]
- 76.Luna TD, French J, Mitcha JL. A study of USAF air traffic controller shiftwork: sleep, fatigue, activity, and mood analyses. Aviat Space Environ Med. 1997;68(1):18–23. [PubMed] [Google Scholar]
- 77.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27(8):1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 78.Johns MW. A New Method for Measuring Daytime Sleepiness - the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 79.Lowden A, Kecklund G, Axelsson J, Akerstedt T. Change from an 8-hour shift to a 12-hour shift, attitudes, sleep, sleepiness and performance. Scand J Work Environ Health. 1998;24 Suppl 3:69–75. [PubMed] [Google Scholar]
- 80.Harma M, Sallinen M, Ranta R, Mutanen P, Muller K. The effect of an irregular shift system on sleepiness at work in train drivers and railway traffic controllers. J Sleep Res. 2002;11(2):141–151. doi: 10.1046/j.1365-2869.2002.00294.x. [DOI] [PubMed] [Google Scholar]
- 81.Gillberg M, Kecklund G, Akerstedt T. Relations Between Performance and Subjective Ratings of Sleepiness During A Night Awake. Sleep. 1994;17(3):236–241. doi: 10.1093/sleep/17.3.236. [DOI] [PubMed] [Google Scholar]
- 82.Axelsson J, Kecklund G, Akerstedt T, Donofrio P, Lekander M, Ingre M. Sleepiness and performance in response to repeated sleep restriction and subsequent recovery during semi-laboratory conditions. Chronobiol Int. 2008;25(2):297–308. doi: 10.1080/07420520802107031. [DOI] [PubMed] [Google Scholar]
- 83.Greneche J, Krieger J, Erhardt C, Bonnefond A, Eschenlauer A, Muzet A, et al. EEG spectral power and sleepiness during 24 h of sustained wakefulness in patients with obstructive sleep apnea syndrome. Clin Neurophysiol. 2008;119(2):418–428. doi: 10.1016/j.clinph.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 84.Czeisler CA, Walsh JK, Roth T, Hughes RJ, Wright KP, Kingsbury L, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med. 2005;353(5):476–486. doi: 10.1056/NEJMoa041292. [DOI] [PubMed] [Google Scholar]
- 85.Suhner A, Schlagenhauf P, Johnson R, Tschopp A, Steffen R. Comparative study to determine the optimal melatonin dosage form for the alleviation of jet lag. Chronobiol Int. 1998;15(6):655–666. doi: 10.3109/07420529808993201. [DOI] [PubMed] [Google Scholar]
- 86.Kecklund G, Akerstedt T, Lowden A. Morning work: effects of early rising on sleep and alertness. Sleep. 1997;20(3):215–223. doi: 10.1093/sleep/20.3.215. [DOI] [PubMed] [Google Scholar]
- 87.Strogatz SH, Kronauer RE, Czeisler CA. Circadian pacemaker interferes with sleep onset at specific times each day: role in insomnia. Am J Physiol. 1987;253(1 Pt 2):R172–R178. doi: 10.1152/ajpregu.1987.253.1.R172. [DOI] [PubMed] [Google Scholar]
- 88.Knauth P, Rutenfranz J. Duration of sleep related to the type of shift work. In: Reinberg A, Vieux N, Andlauer P, editors. Night and shift work: Biological and Social Aspects. Oxford: Pergamon Press; 1981. pp. 161–168. [Google Scholar]
- 89.Tepas DI. Shiftworker sleep strategies. J Hum Ergol (Tokyo) 1982;11 Suppl:325–336. [PubMed] [Google Scholar]
- 90.Harma M, Knauth P, Ilmarinen J. Daytime Napping and Its Effects on Alertness and Short-Term-Memory Performance in Shiftworkers. International Archives of Occupational and Environmental Health. 1989;61(5):341–345. doi: 10.1007/BF00409390. [DOI] [PubMed] [Google Scholar]
- 91.Soderstrom M, Ekstedt M, Akerstedt T, Nilsson J, Axelsson J. Sleep and sleepiness in young individuals with high burnout scores. Sleep. 2004;27(7):1369–1377. doi: 10.1093/sleep/27.7.1369. [DOI] [PubMed] [Google Scholar]
- 92.Eastman CI, Stewart KT, Mahoney MP, Liu L, Fogg LF. Shiftwork: Dark goggles and bright light improve circadian rhythm adaptation to night-shift work. Sleep. 1994;17(6):535–543. doi: 10.1093/sleep/17.6.535. [DOI] [PubMed] [Google Scholar]
- 93.Bjorvatn B, Kecklund G, Akerstedt T. Rapid adaptation to night work at an oil platform, but slow readaptation after returning home. J Occup Environ Med. 1998;40(7):601–608. doi: 10.1097/00043764-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 94.Ekstedt M, Soderstrom M, Akerstedt T, Nilsson J, Sondergaard HP, Aleksander P. Disturbed sleep and fatigue in occupational burnout. Scand J Work Environ Health. 2006;32(2):121–131. doi: 10.5271/sjweh.987. [DOI] [PubMed] [Google Scholar]
- 95.Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: a new approach. Psychophysiol. 1973;10(4):431–436. doi: 10.1111/j.1469-8986.1973.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 96.Dorrian J, Lamond N, Holmes AL, Burgess HJ, Roach GD, Fletcher A, et al. The ability to self-monitor performance during a week of simulated night shifts. Sleep. 2003;26(7):871–877. doi: 10.1093/sleep/26.7.871. [DOI] [PubMed] [Google Scholar]
- 97.Dorrian J, Lamond N, Dawson D. The ability to self-monitor performance when fatigued. J Sleep Res. 2000;9(2):137–144. doi: 10.1046/j.1365-2869.2000.00195.x. [DOI] [PubMed] [Google Scholar]
- 98.Ingre M, Akerstedt T, Peters B, Anund A, Kecklund G. Subjective sleepiness, simulated driving performance and blink duration: examining individual differences. J Sleep Res. 2006;15(1):47–53. doi: 10.1111/j.1365-2869.2006.00504.x. [DOI] [PubMed] [Google Scholar]
- 99.Johnson LC, Spinweber CL, Gomez SA, Matteson LT. Daytime sleepiness, performance, mood, nocturnal sleep: the effect of benzodiazepine and caffeine on their relationship. Sleep. 1990;13(2):121–135. doi: 10.1093/sleep/13.2.121. [DOI] [PubMed] [Google Scholar]
- 100.Kaida K, Akerstedt T, Kecklund G, Nilsson JP, Axelsson J. Use of subjective and physiological indicators of sleepiness to predict performance during a vigilance task. Ind Health. 2007;45(4):520–526. doi: 10.2486/indhealth.45.520. [DOI] [PubMed] [Google Scholar]
- 101.Kaida K, Takahashi M, Akerstedt T, Nakata A, Otsuka Y, Haratani T, et al. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin Neurophysiol. 2006;117(7):1574–1581. doi: 10.1016/j.clinph.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 102.Rogers NL, Dinges DF. Subjective surrogates of performance during night work. Sleep. 2003;26(7):790–791. [PubMed] [Google Scholar]
- 103.Yang CM, Lin FW, Spielman AJ. A standard procedure enhances the correlation between subjective and objective measures of sleepiness. Sleep. 2004;27(2):329–332. doi: 10.1093/sleep/27.2.329. [DOI] [PubMed] [Google Scholar]
- 104.Folkard S, Akerstedt T. Trends in the risk of accidents and injuries and their implications for models of fatigue and performance. Aviat Space Environ Med. 2004;75(3 Suppl):A161–A167. [PubMed] [Google Scholar]
- 105.Harris W. Fatigue, circadian rhythm and truck accidents. In: Mackie RR, editor. Vigilance. New York: Plenum Press; 1977. pp. 133–146. [Google Scholar]
- 106.Hamelin P. Lorry driver's time habits in work and their involvement in traffic accidents. Ergonomics. 1987;30(9):1323–1333. doi: 10.1080/00140138708966026. [DOI] [PubMed] [Google Scholar]
- 107.Langlois PH, Smolensky MH, Hsi BP, Weir FW. Temporal patterns of reported single-vehicle car and truck accidents in Texas, U.S.A. during 1980–1983. Chronobiol Int. 1985;2(2):131–140. doi: 10.3109/07420528509055552. [DOI] [PubMed] [Google Scholar]
- 108.Horne JA, Reyner LA. Sleep related vehicle accidents. BMJ. 1995;310(6979):565–567. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27(6):769–775. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 110.Akerstedt T, Kecklund G, Horte LG. Night driving, season, and the risk of highway accidents. Sleep. 2001;24(4):401–406. doi: 10.1093/sleep/24.4.401. [DOI] [PubMed] [Google Scholar]
- 111.National Transportation Safety Board. Factors that affect fatigue in heavy truck accidents. Washington, D.C: National Transportation Safety Board; 1995. NTSB/SS-95/01. [Google Scholar]
- 112.National Transportation Safety Board. Grounding of the US tankship Exxon Valdez on Bligh Reef, Prince William Sound near Valdez, Alaska, March 24, 1989. Washington, D.C: National Transportation Safety Board. Maritime Accident Report; 1990. NTSB/MAR-90/04. [Google Scholar]
- 113.National Transportation Safety Board. Evaluation of U.S. Department of Transportation: efforts in the 1990s to address operation fatigue. Washington, D.C: National Transportation Safety Board; 1999. NTSB/SR-99/01. [Google Scholar]
- 114.Bjerner B, Holm A, Swensson A. Diurnal variation in mental performance; a study of three-shift workers. Br J Ind Med. 1955;12(2):103–110. doi: 10.1136/oem.12.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brown RC. The day and night performance of teleprinter switchboard operators. J Occup.Psychol. 1949;23:121–126. [Google Scholar]
- 116.Wojtczak-Jaroszowa J, Pawlowska=Skyga K. Night and shift work I: Circadian variations in work. Med.Pr. 1967;18:1–10. [PubMed] [Google Scholar]
- 117.Ong CN, Phoon WO, Iskandar N, Chia KS. Shiftwork and work injuries in an iron and steel mill. Appl Ergon. 1987;18(1):51–56. doi: 10.1016/0003-6870(87)90070-6. [DOI] [PubMed] [Google Scholar]
- 118.Wojtczak-Jaroszowa J, Jarosz D. Chronohygienic and chronosocial aspects of industrial accidents. Prog Clin Biol Res. 1987;227B:415–426. [PubMed] [Google Scholar]
- 119.Andlauer P. TU Information Bulletin. European Productivity Agency; 1960. The effect of shift working on the workers' health; p. 29. [Google Scholar]
- 120.Gold DR, Rogacz S, Bock N, Tosteson TD, Baum TM, Speizer FE, et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82(7):1011–1014. doi: 10.2105/ajph.82.7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Smith P. Study of Weekly and Rapidly Rotating Shift Workers. Ergonomics. 1978;21(10):874. [Google Scholar]
- 122.Mitler MM, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep, and public policy: consensus report. Sleep. 1988;11(1):100–109. doi: 10.1093/sleep/11.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Smith L, Folkard S, Poole CJ. Increased injuries on night shift. Lancet. 1994;344(8930):1137–1139. doi: 10.1016/s0140-6736(94)90636-x. [DOI] [PubMed] [Google Scholar]
- 124.Akerstedt T, Fredlund P, Gillberg M, Jansson B. A prospective study of fatal occupational accidents --relationship to sleeping difficulties and occupational factors. J Sleep Res. 2002;11(1):69–71. doi: 10.1046/j.1365-2869.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- 125.Barger LK, Cade BE, Ayas NT, cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 126.Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388(6639):235. doi: 10.1038/40775. [DOI] [PubMed] [Google Scholar]
- 127.Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294(9):1025–1033. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 128.Leger D. The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research. Sleep. 1994;17(1):84–93. doi: 10.1093/sleep/17.1.84. [DOI] [PubMed] [Google Scholar]
- 129.Knauth P. Speed and direction of shift totation. J Sleep Res. 1995;4 suppl 2:41–46. doi: 10.1111/j.1365-2869.1995.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 130.van Amelsvoort LG, Jansen NW, Swaen GM, van den Brandt PA, Kant I. Direction of shift rotation among three-shift workers in relation to psychological health and work-family conflict. Scand J Work Environ Health. 2004;30(2):149–156. doi: 10.5271/sjweh.772. [DOI] [PubMed] [Google Scholar]
- 131.Wilkinson RT. How Fast Should the Night-Shift Rotate. Ergonomics. 1992;35(12):1425–1446. doi: 10.1080/00140139208967412. [DOI] [PubMed] [Google Scholar]
- 132.Wedderburn AAI. How Fast Should the Night-Shift Rotate - A Rejoinder. Ergonomics. 1992;35(12):1447–1451. doi: 10.1080/00140139208967413. [DOI] [PubMed] [Google Scholar]
- 133.Folkard S. Is There A Best Compromise Shift System. Ergonomics. 1992;35(12):1453–1463. doi: 10.1080/00140139208967414. [DOI] [PubMed] [Google Scholar]
- 134.Smith L, Folkard S, Tucker P, Macdonald I. Work shift duration: a review comparing eight hour and 12 hour shift systems. Occup Environ Med. 1998;55(4):217–229. doi: 10.1136/oem.55.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tucker P, Smith L, Macdonald I, Folkard S. Distribution of rest days in 12 hour shift systems: impacts on health, wellbeing, and on shift alertness. Occup Environ Med. 1999;56(3):206–214. doi: 10.1136/oem.56.3.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occupational and Environmental Medicine. 2005;62(9):588–597. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gundel A, Drescher J, Maass H, Samel A, Vejvoda M. Sleepiness of Civil Airline Pilots During 2 Consecutive Night Flights of Extended Duration. Biol Psychol. 1995;40(1–2):131–141. doi: 10.1016/0301-0511(95)05107-4. [DOI] [PubMed] [Google Scholar]
- 138.Son M, Kong JO, Koh SB, Kim J, Harma M. Effects of long working hours and the night shift on severe sleepiness among workers with 12-hour shift systems for 5 to 7 consecutive days in the automobile factories of Korea. J Sleep Res. 2008;17(4):385–394. doi: 10.1111/j.1365-2869.2008.00675.x. [DOI] [PubMed] [Google Scholar]
- 139.Scott LD, Hwang WT, Rogers AE, Nysse T, Dean GE, Dinges DF. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep. 2007;30(12):1801–1807. doi: 10.1093/sleep/30.12.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C: American Psychiatric Association; 2000. [Google Scholar]
- 141.Sack RL, Auckley D, Auger R, Carskadon MA, Wright KP, Jr, Vitiello MV, et al. Circadian Rhythm Sleep Disorders: Part I, Basic Principles, Shift Work and Jet Lag Disorders: An American Academy of Sleep Medicine Review. Sleep. 2007;30(11):1456–1479. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tucker P, Smith L, Macdonald I, Folkard S. Effects of direction of rotation in continuous and discontinuous 8 hour shift systems. Occup Environ Med. 2000;57(10):678–684. doi: 10.1136/oem.57.10.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Folkard S, Lombardi DA, Tucker PT. Shiftwork: Safety, sleepiness and sleep. Industrial Health. 2005;43(1):20–23. doi: 10.2486/indhealth.43.20. [DOI] [PubMed] [Google Scholar]
- 144.Costa G, Sartori S, Akerstedt T. Influence of flexibility and variability of working hours on health and well-being. Chronobiol Int. 2006;23(6):1125–1137. doi: 10.1080/07420520601087491. [DOI] [PubMed] [Google Scholar]
- 145.Tucker P, Folkard S, Macdonald I. Rest breaks and accident risk. Lancet. 2003;361(9358):680. doi: 10.1016/S0140-6736(03)12566-4. [DOI] [PubMed] [Google Scholar]
- 146.Tucker P, Smith L, Macdonald I, Folkard S. The impact of early and late shift changeovers on sleep, health, and well-being in 8- and 12-hour shift systems. J Occup Health Psychol. 1998;3(3):265–275. doi: 10.1037//1076-8998.3.3.265. [DOI] [PubMed] [Google Scholar]
- 147.Akerstedt T, Torsvall L, Gillberg M. Shift Work and Napping. In: Dinges DF, Broughton RJ, editors. Sleep and Alertness: Chronobiological, Behavioral, and Medical Aspects of Napping. New York: Raven Press; 1989. pp. 205–220. [Google Scholar]
- 148.Purnell MT, Feyer AM, Herbison GP. The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res. 2002;11(3):219–227. doi: 10.1046/j.1365-2869.2002.00309.x. [DOI] [PubMed] [Google Scholar]
- 149.Schweitzer PK, Randazzo AC, Stone K, Erman M, Walsh JK. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep. 2006;29(1):39–50. doi: 10.1093/sleep/29.1.39. [DOI] [PubMed] [Google Scholar]
- 150.Dinges DF, Orne MT, Whitehouse WG, Orne EC. Temporal placement of a nap for alertness: contributions of circadian phase and prior wakefulness. Sleep. 1987;10(4):313–329. [PubMed] [Google Scholar]
- 151.Wertz AT, Ronda JM, Czeisler CA, Wright KP., Jr Effects of sleep inertia on cognition. JAMA. 2006;295(2):163–164. doi: 10.1001/jama.295.2.163. [DOI] [PubMed] [Google Scholar]
- 152.Tietzel AJ, Lack LC. The short-term benefits of brief and long naps following nocturnal sleep restriction. Sleep. 2001;24(3):293–300. doi: 10.1093/sleep/24.3.293. [DOI] [PubMed] [Google Scholar]
- 153.Wright KP, Jr, Badia P, Myers BL, Plenzler SC. Combination of bright light and caffeine as a countermeasure for impaired alertness and performance during extended sleep deprivation. J Sleep Res. 1997;6(1):26–35. doi: 10.1046/j.1365-2869.1997.00022.x. [DOI] [PubMed] [Google Scholar]
- 154.Bonnet MH, Arand DL. The use of prophylactic naps and caffeine to maintain performance during a continuous operation. Ergonomics. 1994;37(6):1009–1020. doi: 10.1080/00140139408963714. [DOI] [PubMed] [Google Scholar]
- 155.Smith MR, Lee C, Crowley SJ, Fogg LF, Eastman CI. Morning melatonin has limited benefit as a soporific for daytime sleep after night work. Chronobiol Int. 2005;22(5):873–888. doi: 10.1080/09636410500292861. [DOI] [PubMed] [Google Scholar]
- 156.Bjorvatn B, Stangenes K, Oyane N, Forberg K, Lowden A, Holsten F, et al. Randomized placebo-controlled field study of the effects of bright light and melatonin in adaptation to night work. Scand J Work Environ Health. 2007;33(3):204–214. doi: 10.5271/sjweh.1129. [DOI] [PubMed] [Google Scholar]
- 157.Lowden A, Akerstedt T, Wibom R. Suppression of sleepiness and melatonin by bright light exposure during breaks in night work. J Sleep Res. 2004;13(1):37–43. doi: 10.1046/j.1365-2869.2003.00381.x. [DOI] [PubMed] [Google Scholar]
- 158.Santhi N, Aeschbach D, Horowitz TS, Czeisler CA. The impact of sleep timing and bright light exposure on attentional impairment during night work. J Biol Rhythms. 2008;23(4):341–352. doi: 10.1177/0748730408319863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Reyner LA, Horne JA. Evaluation "in-car" countermeasures to sleepiness: cold air and radio. Sleep. 1998;21(1):46–50. [PubMed] [Google Scholar]
- 160.Anund A, Kecklund G, Vadeby A, Hjalmdahl M, Akerstedt T. The alerting effect of hitting a rumble strip--a simulator study with sleepy drivers. Accid Anal Prev. 2008;40(6):1970–1976. doi: 10.1016/j.aap.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 161.Batejat DM, Lagarde DP. Naps and modafinil as countermeasures for the effects of sleep deprivation on cognitive performance. Aviat Space Environ Med. 1999;70(5):493–498. [PubMed] [Google Scholar]