Abstract
Introduction
Cardiovascular disease (CVD) is a burden for developing countries, yet few CVD intervention studies have been conducted in developing countries such as Indonesia. This paper outlines the process of designing a community intervention programme to reduce CVD risk factors, and discusses experiences with regard to design issues for a small-scale intervention.
Design process
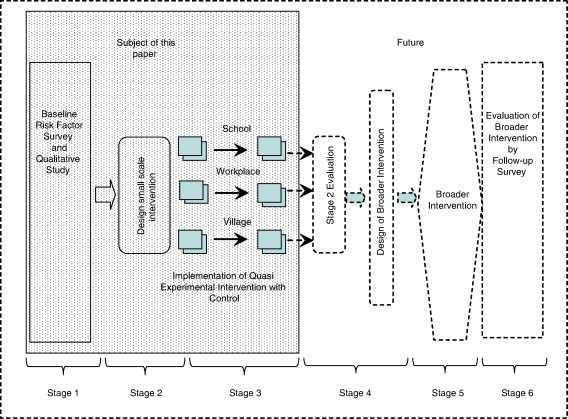
The design process for the present community intervention consisted of six stages: (1) a baseline risk factor survey, (2) design of a small-scale intervention by using both baseline survey and qualitative data, (3) implementation of the small-scale intervention, (4) evaluation of the small-scale intervention and design of a broader CVD intervention in the Yogyakarta municipality, (5) implementation of the broader intervention and (6) evaluation of the broader CVD intervention. According to the baseline survey, 60% of the men were smokers, more than 30% of the population had insufficient fruit and vegetable intake and more than 30% of the population were physically inactive, this is why a small-scale population intervention approach was chosen, guided both by the findings in the quantitative and the qualitative study.
Experiences
A quasi-experimental study was designed with a control group and pre- and post-testing. In the small-scale intervention, two sub-districts were selected and randomly assigned as intervention and control areas. Within them, six intervention settings (two sub-villages, two schools and two workplaces) and three control settings (a sub-village, a school and a workplace) were selected. Health promotion activities targeting the whole community were implemented in the intervention area. During the evaluation, more activities were performed in the low socioeconomic status sub-village and at the civil workplace.
Keywords: cardiovascular disease, design intervention, community intervention, urban community, developing countries
Cardiovascular disease (CVD) has recently become the leading cause of death in developing countries, where 60% of all CVD currently occurs (1). In Indonesia, CVD ranked 11th in 1972, 2nd in 1986 and became the leading cause of death in 1992 (2). In 2002, it was estimated that chronic disease was the cause of 68% of all deaths and almost half were caused by CVD (3).
The burden of CVD in Indonesia varies in terms of location and sex. CVD mortality is higher in the more populated provinces of Java and Bali (16.2%) than in Sumatra (5.3%) (4), for example, and risk factor prevalence is higher in the more populated areas (5). The most common CVD risk factors are smoking, physical inactivity and high blood pressure. Prevalence of smoking (men 58%, women 3%) and hypertension (men 27%, women 11%) are higher among men, while physical inactivity is more prevalent among women (men 59%, women 71%) (S. Soemantri et al., unpublished).
CVD risk factors are closely related to the daily lifestyle of an individual, which is often beyond that person's control; personal behaviour is influenced not only by individual choice, but also by the preferences of surrounding people and other environmental factors (6). A programme is needed that enables people to take control of their health, not only at an individual level, but also at organisational and community levels. As such, an intervention to reduce CVD, based on community empowerment, may be an effective approach (7, 8) considering the limited budget in the health sector and the importance of sustainability for any programme. A literature search in PubMed, however, identified only four publications regarding CVD community interventions using empowerment principles, all of which were conducted in developed countries (9).
The Yogyakarta province, a densely populated area in Java Island, has the highest life expectancy in Indonesia, and can therefore be expected to bear the greatest burden of CVD (10). The PRORIVA programme (Programme to Reduce Cardiovascular Disease Risk Factors in Yogyakarta City, or PROJABAR in local language) involves six planned stages: (1) a baseline risk factor survey and a baseline qualitative study, (2) design of a small-scale intervention based on baseline data and data from the qualitative study, (3) implementation of a small-scale intervention, (4) evaluation of the small-scale intervention and design of a broader CVD intervention, (5) implementation of the broader intervention and (6) evaluation of the broader CVD intervention (Fig. 1).
Fig. 1.
PRORIVA study framework.
This paper outlines the process of designing a small-scale community intervention programme to reduce CVD risk factors in Yogyakarta, and discusses experiences with regard to design issues. The paper reports results from a quantitative baseline survey, and integrates these finding with those from a qualitative study, published in the first paper (Maintaining balance and harmony: Javanese perceptions on health and CVD) (11).
Process of designing a community intervention
Study setting
Yogyakarta is the main city of Yogyakarta province and was selected because urban populations typically show a higher prevalence of CVD risk factors. Yogyakarta extends over an area of 32.5 km2, has a population of almost half a million and a population density of 15,197 people/km2 (12). It is a well-known tourist destination with historical sites such as Borobudur temple, Prambanan temple and Yogyakarta Palace (13). In 2005, life expectancy of the population in Yogyakarta city was longer (72.9 year) than in Indonesia (68.1 year) as a whole (14). The risk of chronic disease is increasing for older people; consequently, people in Yogyakarta city have a relatively higher risk for chronic diseases, including CVD.
The existence of Yogyakarta Palace in Yogyakarta city maintains a degree of Javanese culture. Historically, Yogyakarta Palace was one of the cultural cores of Javanese ancient heritage, and this tradition has continued so that today the city still represents the centre of Javanese culture.
Ethical approval for the study was given by the Gadjah Mada University, governmental permission by the provincial government, and individual informed consent by each respondent.
Stage 1. Baseline risk factor survey
Baseline screening was performed to evaluate the prevalence of CVD risk factors in the Yogyakarta population as such information is scarce. The survey was based on the WHO framework for surveillance of non-communicable diseases (NCD) (15).
The STEPS instrument (core and expanded version 1.4) was used to monitor NCD risk factors, which incorporates self-reported habits and physical measurements (16); a questionnaire on knowledge and attitude about CVD risk factors was also added. Daily habits surveyed included smoking habits, alcohol consumption, daily intake of fruit and vegetables, physical activity and history of hypertension and diabetes. Physical measurements were taken for height, weight, waist and hip circumference and blood pressure.
Sampling frames containing individual age and sex lists are scarce in developing countries. One feasible solution is to conduct multistage random sampling that utilises available sampling frames (17). The available sampling frame in this study was block censuses (BC), with no individual age and sex list for each building within each BC. To overcome this problem, a procedure was decided before data collection to substitute respondents from nearby buildings in a certain order.
The sample size was determined using the WHO manual (18), and resulted in a sample size of 3,205 respondents. Respondents were selected using a multistage random sampling design. First, 150 out of 1,217 BC were randomly selected. Within each BC, buildings were systematically selected. Next, all individuals aged 15–75 years were selected from each building. An equal number of respondents in each age and sex group were selected from each BC. In selected buildings, 2,147 respondents met the age and sex criteria, while 1,058 respondents were recruited from nearby buildings.
The respondent substitutions were due to non-response 82 and failure to meet age and sex criteria 976. There were no statistically significant differences between selected respondents and substituted respondents with regard to risk factors or demographic characteristics (sex, age group, income and education level).
Respondents were classified as smokers if they reported smoking at least one cigarette per day; as having low fruit and vegetable intake if they ate <4.5 portions per day of fruit and vegetables (one portion is equal to 100 ml of fruit or vegetables); as being physically inactive if their average total activity time was less than 105 min per week (the mean of total activity time); as having elevated blood pressure if systolic blood pressure was ≥140 mmHg and/or diastolic blood pressure was ≥90 mmHg or was taking antihypertensive medication; as overweight if their BMI was ≥25, and as obese if their BMI was ≥30 (19). Respondents were classified as low socioeconomic status (SES) if they had a monthly household income lower than the mean of household income, and as high SES if their monthly income was equal to or higher than the mean. Finally, participants were characterised according to gender and age groups (15–34, 35–54 and 55–75 year). Cases of elevated blood pressure, overweight and obesity in need of medical treatment were referred to the local health service.
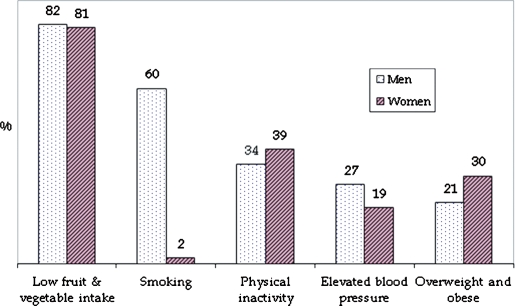
The baseline risk factor prevalence differed according to gender (Fig. 2). Fruit and vegetable intake was low for both genders, and, furthermore, people ate more vegetables than fruit, with an average of 2.1±0.03 and 1.2±0.03 portions per day, respectively. Smoking prevalence was much higher among men; while physical inactivity was more common among women. Prevalence of elevated blood pressure was higher among men, and obesity and overweight were more common among women.
Fig. 2.
The prevalance of CVD risk factors among men and women.
The prevalence of CVD risk factors differed according to SES and age group (Table 1). Smoking was more common among middle-aged men and among low SES respondents. By contrast, in women, smoking was more common among the younger age groups and high SES groups. Low fruit and vegetable intake was higher in low SES groups, while physical inactivity was higher in high SES groups. Finally, elevated blood pressure was higher among the elderly, and overweight and obesity were common among the middle-aged in all SES groups.
Table 1.
Prevalence of CVD risk factors with regard to age groups, sex and SES
| Prevalence among age groupsa | ||||||
|---|---|---|---|---|---|---|
| Men | Women | |||||
| Risk factors and SES | 15–34 | 35–54 | 55–75 | 15–34 | 35–54 | 55–75 |
| Smokingb | ||||||
| SES lowc | 62 | 72 | 65 | 2 | 0 | 3 |
| SES highd | 52 | 67 | 50 | 4 | 1 | 2 |
| Low fruit and vegetable intakee | ||||||
| SES low | 85 | 83 | 85 | 84 | 84 | 83 |
| SES high | 78 | 79 | 76 | 76 | 75 | 78 |
| Physical inactivityf | ||||||
| SES low | 38 | 23 | 29 | 33 | 27 | 38 |
| SES high | 37 | 36 | 33 | 43 | 42 | 31 |
| Elevated blood pressureg | ||||||
| SES low | 17 | 38 | 55 | 7 | 30 | 54 |
| SES high | 16 | 38 | 58 | 5 | 21 | 59 |
| Overweighth | ||||||
| SES low | 13 | 26 | 22 | 22 | 47 | 31 |
| SES high | 22 | 36 | 29 | 22 | 43 | 42 |
aValues are percentages.
bSmoking was defined if they smoked at least one cigarette per day.
cLow SES was defined if the household income less than the mean.
dHigh SES was defined if the household income greater than or equal to the mean.
eFruit and vegetable intake was defined low if they ate <4.5 portion per day.
fPhysical inactivity was defined if their total activity time <105 min per week (the mean of total activity time).
gElevated blood pressure was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg or taking antihypertensive medication.
hOverweight was defined if BMI ≥25.
Based on the baseline survey, it was considered important to develop a health promotion programme for the primary prevention of CVD before pathologic conditions appear.
Stage 2. Design of a small-scale intervention by using both quantitative baseline survey data and qualitative data
The qualitative study that is reported in parallel to this paper (unpublished observations) shows existing social activities that could be used to deliver health information to the community and contribute to developing a culturally sensitive intervention.
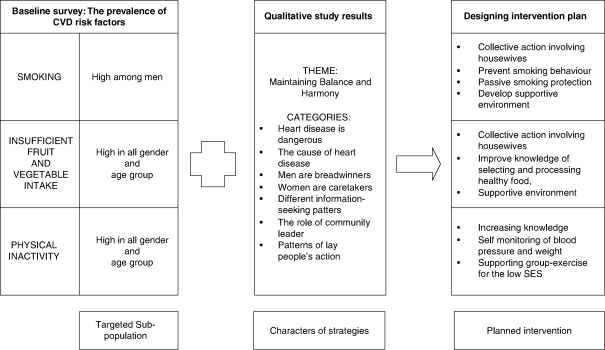
The process of combining baseline and qualitative data into an intervention plan is described in Fig. 3. The result of the qualitative study was directed towards the suitability of the intervention to local culture, while the risk factor survey addressed the particular target of the intervention.
Fig. 3.
The Stage 2 intervention plan developed from baseline and qualitative study data.
As all the CVD risk factors (smoking, low fruit and vegetable intake and physical inactivity) were common among the population, the CVD prevention programme needed to target both genders and all SES and age groups, even if particular attention was given to the groups at higher risk. Because smoking is high among men and they consider smoking to be a necessity (20), smoking cessation has to be carefully designed. Another way may be to focus on protection against passive smoking as an introductory activity, thereby encouraging measures to reduce opportunities to smoke before a more strict smoking ban could be applied. In addition, an education programme tailored towards the prevention of smoking behaviour among youth could also be beneficial in the long run. Low fruit and vegetable intake among low SES groups (especially fruit intake) was interpreted as an indication of reduced ability to purchase fruit. As there are abundant high fruit and vegetable foods that are cheap, an education programme is needed that seeks to improve knowledge of high fruit and vegetable yet low price food, and cooking of healthy food that is rich in fruit and vegetables, but low in salt, sugar and oil. Based on the findings of the survey, the programme to promote physical activity should be targeted at high SES populations, especially women. High SES groups were found to be more self-reliant, to act individually and to be better able to find information. Consequently, the intervention programme should encourage this group to be more physically active through specific group exercise, to self-monitor their health condition and to provide more detailed health information. For the low SES group, it may be sufficient to promote collective exercise.
Overall, the intervention should seek to maintain balance and harmony at the individual, household and population levels of society, which may be easier through a community empowerment approach that enables community members to participate in decision making (7). In this study, we use Beeker's definition of community empowerment (7):
A community empowerment intervention seeks to effect community-wide change in health-related behaviors by organizing communities to define their health problems, to identify the determinants of those problems and to engage in effective individual and collective action to change those determinants.
According to the community empowerment approach (7, 8, 21), the community is the main actor, while programme representatives mainly act as facilitators. This approach identifies five stages: (1) building trust with the community, describing the goals of the project and clarifying the role of the programme facilitator and the community; (2) raising community awareness to identify their problems and ways to solve them; (3) community programme development; (4) organisational work that aims to encourage the community to organise themselves to run the programme; and (5) a maintenance period to keep the programme sustainable by identifying internal community motivators and encouraging the authorities to provide supportive environments (21). A maintenance period was not included in this small-scale study.
Stage 3. Implementation of the small-scale intervention
The small-scale intervention was carried out as a model, with the intention being to apply the intervention to the whole municipality. The study design was quasi-experimental. Two sub-districts with demographic characteristics similar to Yogyakarta, but geographically separated, were selected and assigned as intervention (Tegalrejo sub-district) and control (Mantrijeron sub-district). In the intervention sub-district, six settings (two schools, two workplaces and two sub-villages) were selected as intervention sites. The selection of the sites was based on purposive sampling strategies (22). One of the intervention schools represented a high-rank school and one was a low-rank school according to national standards. The high-rank school will reach more high SES youths and vice versa. Of the two intervention sub-villages, one was characterised as having high SES and one as low SES. The two workplaces also differed: one was a civil workplace targeting high SES groups and the other was private, targeting the low SES working population. The total population in the intervention area was 4,237. Three reference settings were selected in the Mantrijeron sub-district, which represented a middle-rank school, a private workplace with middle SES workers, and a middle SES sub-village.
Study context
The social activities and communication networks varied in each site. In the low SES sub-village, people had more time for social activities compared to the high SES sub-village. The informal communication network in the low SES sub-village was mainly through regular public meetings. In the high SES sub-village, people communicated mainly through printed media, electronic media or door-to-door information.
At the schools, the activities were similar between the high-rank and low-rank schools and mainly consisted of compulsory courses including biology, life skills, sports and a few optional activities. No food was provided by the schools, and smoking was strictly prohibited for students. The main communication networks were top-down and between-peer communication.
At the civil office, staff shared moderate time for social activities, which was in contrast to the private office where there was no time for social activities. The informal communication network in the civil office was top-down and between-workers, whereas the private office was mainly top-down.
The PRORIVA small-scale intervention
The small-scale intervention lasted 8 months, from September 2006 to May 2007. Two different SES groups and three risk factors (smoking, physical inactivity and low fruit and vegetable intake) were targeted at the community level of the three different settings (schools, workplaces and sub-villages). In the control sites, a leaflet about CVD, its risk factors and how to prevent CVD was distributed after the intervention had ended.
Meetings were held with leaders of each setting to obtain permission and raise awareness of the danger of CVD. The intervention was then developed based on an agreement between an internal team consisting of local people, and the programme representatives. During the intervention process, local voluntary health workers were identified, trained and enlisted in each activity and setting. Coordination meetings were held with community members as part of existing meetings.
Health education sessions were organised to help people understand CVD. The topics and strategy of these sessions were adjusted according to the communities' needs. Health education topics typically included CVD manifestations, causes, prevention and how to practice healthy behaviours. The high SES settings demanded more detailed information regarding CVD compared with the low SES settings. Health education in the sub-villages was practiced in small group lectures during community meetings and speeches after group exercise. Health education was added to related academic sessions at schools, and was delivered as workshops in the civil workplace. In all settings, printed materials were provided by the programme representative to assist with self-education. The printed materials were developed based on target group preferences (23). For example, people in working places requested more written materials, whereas people in sub-villages chose more picture-based materials. Further, the printed material raised the benefit of adopting healthy behaviour, which is the exchange concept of social marketing techniques (24).
To encourage the practice of healthy behaviours in the two sub-village settings, we decided that the public meetings should be conducted as non-smoking meetings and that regular group exercise should be performed. Anti-smoking activities were emphasised in low SES sub-villages with more health education provided during public meetings and through informal discussion with local voluntary health workers. Non-smoking classes were held at the schools, additional exercise classes were organised with both students and teachers, and workshops were set up about choosing and cooking healthy food, involving the teacher, student representatives and food retailers near to the schools. At the civil workplaces, non-smoking policies were implemented. Friday morning group exercise was revived, and fruit was promoted instead of snacks at each meeting. Due to concern regarding lost of work time, there was no-practice agreement to preform health education during and after working hours at the private workplace site. The number of intervention activities was highest in sub-villages followed by schools and the civil workplace. The private workplace had the fewest activities (Table 2).
Table 2.
The PRORIVA intervention activities in different settings
| Activities | |||
|---|---|---|---|
| Community intervention phases | Sub-village setting | School setting | Workplace setting |
| Building trust | Meetings with sub-village and community leaders | Informal meetings with principals and some teachers | Formal meetings with workplace directors |
| Raising awareness | Public meetings with community members | Announcements to the students | Public meetings with workers |
| Identification of local CVD risk factor problems | Identification of local CVD risk factor problems | ||
| Programme development | Select an internal team at each sub-village, consisting of community leaders and volunteer health workers | Assign internal team consisting of teachers and students | Assigning one contact person |
Agree on activities:
|
Agree on activities:
|
Agree on activities b:
|
|
| Community organisation | Community team obtained the agreements | Schools team obtained the agreements | Workplace team obtained the agreements |
Programme supported:
|
Programme supported:
|
Programme supported:
|
|
| Initiation of maintenance | Internal teams trained to deliver message and continue the programme | Internal teams trained to continue the programme | Trained contact persons to operate risk factor measurement kits |
The community team conducted:
|
The school teams conducted:
|
||
aIncluded: blood pressure, body weight and waist circumference measurement kit.
bNo agreement at private workplace.
Discussion
Despite the emerging global CVD epidemic, few community intervention studies have been conducted in developing countries, and almost no studies based in urban settings in a developing country have been reported. This makes the PRORIVA study unique. Being a developing country means coping with limited resources that only allow small studies and short intervention periods. Thus, it is even more important to model an intervention before scaling up (25, 26). A small-scale study provides opportunities to increase the intensity of the intervention, while short-term interventions carry the advantage of differentiating ‘intentional’ from ‘unintentional’ interventions.
The small-scale PRORIVA intervention was developed based on a quantitative study (baseline survey) and a qualitative study that enriched information on behaviour risk factors in the population and the local culture. This allows for greater understanding of personal behaviours that are rooted in the local culture (25–27).
Our baseline survey showed that the population prevalence of unhealthy lifestyles was above 30%. This was one reason for using a population approach when designing the small-scale intervention. A population approach might be more appropriate than a high-risk strategy, as a small shift in the risk factors in the majority of a population is believed to be more effective than a substantial shift among a smaller high-risk group. A population approach concerns to change the risk factors in population-wide, whereas high-risk approach only among high-risk individuals (28–30).
The small-scale PRORIVA intervention uses a community empowerment strategy. A cornerstone of this strategy is community perception that the programme belongs to them and that they are the main actors. As such, it may be possible to mobilise community resources and ensure sustainability of the programme (21). This is crucial if a programme is to reinforce long-term behaviour changes, thereby reducing the risk of CVD (26, 31).
The first phase of PRORIVA intervention is building trust with the targeted community, a trust of working together to control the CVD problem. Trust was built in all settings except for the private workplace. As building trust is a prerequisite for the phases that follow, the number of activities in the private workplace was the smallest (Table 2).
To illustrate how the different activities were received in different settings, three supporting factors were assessed by two researchers. The extent of support for each factor differed between the intervention settings. Intervention activities in the low SES sub-villages received strong support, while none of the supporting factors were present in the private workplace (Table 3).
Table 3.
Presence in six intervention settings of supporting factors in the implementation of health promotion activities in a small-scale community intervention
| Sub-village | Schools | Workplace | ||||
|---|---|---|---|---|---|---|
| Factors | Low SES | High SES | Low academic achievement | High academic achievement | Civil | Private |
| Existing social activities | + | – | – | – | – | – |
| Support from community leaders | + | + | + | + | + | – |
| Internal site team activity | + | – | – | – | – | – |
Note: + = exist; – = not exist.
Conditions that support or hinder community interventions are often beyond an individual's control, and depend more on networking between members of the community (32). In this small-scale intervention, the low SES sub-village received more support than in other settings, thus the community intervention included more activities. School-based interventions might be useful as the setting for CVD prevention programmes that support healthy behaviours from an early age (32, 33).
The study showed promising findings for many activities. The low SES sub-village developed more preventive activities than the high SES sub-village, which suggests possible opportunities to prevent CVD in low SES sub-villages where the predicted burden of CVD is high (33). Community interventions to reduce CVD risk factors in developed countries are usually externally tailored programmes, developed and managed by authorities (34–37), and only a few are implemented as bottom-up programmes. Many of the programmes have reported success with regard to different risk factors, but all have abundant external resources. In developing countries, a top-down strategy has also been applied. An externally tailored community intervention programme in India (27) showed promising short-term results, however this study differed from the PRORIVA small-scale interventions, in that PRORIVA aimed to develop a bottom-up intervention. This community empowerment approach was selected because it enables behaviour change at individual, organisational and social levels, and results in more sustainable behaviour change (7). Only long-term and continuous CVD intervention can show significant results in terms of the outcome (38, 39), thus the sustainability of an intervention is important. Furthermore, the community empowerment approach is suitable for disadvantaged populations (8), such as in Indonesia, where the health sector budget is limited.
There are many challenges for a large-scale PRORIVA study in the future. As local communities have different needs and requests, the intervention components will vary. Consequently, programme management must be flexible in order to accommodate this (40). Financing is another problem in settings with few supporting conditions for community mobilisation. Local resources will take longer to mobilise. Joint ventures with top-down resources are needed to back-up the lack of financial resources in certain settings. There are potential conflicts of interests in the process of combining top-down and bottom-up approaches; top-down approaches rely heavily on the government, while bottom-up approaches need to accommodate local demands. Other important challenges include making the programme sustainable and keeping the importance of CVD risk factor reduction on the community agenda.
Successful chronic disease management requires comprehensive care at the patient level as well as at health service, community and policy maker levels. The healthcare system has to provide necessary medical treatment, counselling for the chronic disease patient and establish adequate surveillance systems. Accordingly, relevant conditions to improve the skills of health workers and provide financing are demanded from the policy and decision makers (41). In summary, the small-scale PRORIVA study illustrates a way to design a CVD prevention programme that integrates the results of scientific studies as well as the needs expressed by the community. The small-scale study focused on the intervention target and identified ways to develop culturally sensitive programmes in accordance with the community demands and potentials. However, further study on cost-effectiveness analysis is needed before scaling-up the programme (42).
Acknowledgements
We are grateful to the Health Promotion Coordination Board of Yogyakarta, Indonesia, who supported community mobilisation.
Conflict of interest and funding
This study was supported by a grant from the Provincial Health Office of Yogyakarta Special Regency, Indonesia, by a scholarship based on a donation from the Swedish Centre Party to Umeå International School of Public Health, Umeå, Sweden and Umeå Centre for Global Health Research.
References
- 1.Mackay J, Mensah GA, Mendis S, Greenlund K. The atlas of heart disease and stroke. Brighton: Myriad EditionLimited; 2004. [Google Scholar]
- 2.Muhilal Transitions in diet and health: implication of modern lifestyles in Indonesia. Asia Pacific J Clin Nutr. 1996;5:132–34. [PubMed] [Google Scholar]
- 3.WHO Global Infobase Online. 2006. Available from: http://www.who.int/ncd_surveillance/infobase/web/InfoBaseCommon/Shared/print.aspx?printpage=%2fInfoBasePolicyMaker%2freports%2freportViewer.aspx%3fUN_Code%3d360%26rptCode%3dMOR%26dm%3d10%26GraphDisplayType_DDL%3dPie2D [cited 23 September 2006]
- 4.Sumartono RW, Aryastami NK. Penyakit jantung dan pembuluh darah pada usia 55 tahun menurut Survei Kesehatan Rumah Tangga 1992. [Heart and cardiovascular disease on men 55 year based on Household Health Survey 1992]. The Mirror of Medical WorldCermin Dunia Kedokteran. 1999;123:5–8. [Google Scholar]
- 5.Kristanti CM, Hapsari D, Pradono J, Soemantri S. Behavior risk factors in Indonesia: National Household Health Survey 2001. Buletin Penelitian Kesehatan [Health Res Bull] 2002;30:21–8. [Google Scholar]
- 6.Thomas AG, editor. New York: Oxford University Press; 2000. Psychosocial intervention. [Google Scholar]
- 7.Beeker C, Guenther-Grey C, Raj A. Community empowerment paradigm drift and the primary prevention of HIV/AIDS. Soc Sci Med. 1998;46:831–42. doi: 10.1016/s0277-9536(97)00208-6. [DOI] [PubMed] [Google Scholar]
- 8.Secret M, Jordan A, Ford J. Empowerment evaluation as a social work strategy. Health Soc Work. 1999;24:120–7. doi: 10.1093/hsw/24.2.120. [DOI] [PubMed] [Google Scholar]
- 9.US NLM N. Available from: http://www.ncbi.nlm.nih.gov/sites/entrez [cited 20 December 2007]
- 10.Badan Pusat Statistik [Central Board of Statistics] (Indonesia) Profil populasi daerah istimewa yogyakarta. 2000. [updated 2000]. Jakarta; Available from: http://www.bps.go.id/index.sthml [cited 23 September 2006]
- 11.Dewi STD, Weinehall L, Öhman A. ‘Maintaining balance and harmony’: Javanese perceptions of health and cardiovascular disease. Global Health Action. 2010;3:4660. doi: 10.3402/gha.v3i0.4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Situs resmi pemerintah kota Yogyakarta [Jogja Government Online] Kondisi Geografis Kota Yogyakarta. 2006. Yogyakarta; [updated 2006]. Available from: http://www.jogja.co.id/jogjaku/geografis.asp [cited 20 October 2006]
- 13.Dahles H, Bras K. Entrepreneurs in romance tourism in Indonesia. Ann Tourism Res. 1999;26:267–93. [Google Scholar]
- 14.Badan Pusat Statistik [Central Board of Statistics] (Indonesia) Human Development Index 1999–2005. 2005. Jakarta; [updated 2005]. Available from: http://www.bps.go.id/sector/ipm/table1.shtml [cited 16 September 2008]
- 15.World Health Organization. Non communicable diseases and mental health. STEPS: a framework for surveillance. World Health Organization. 2003. Available from: http://www.who.int/ncd_surveillance [cited 10 May 2004]
- 16.World Health Organization. Noncommunicable diseases and mental health. STEP instrument for NCD risk factors (core and expanded version 1.4). The WHO STEPwise approach to surveillance of non communicable diseases (STEPS) [electronic book] WHO. 2004. Available from: http://www.who.int/ncd_surveillance [cited 19 March 2004]
- 17.Levy PS, Lemeshow S. Sampling of populations. Methods and applications. 3rd ed. New York: John Wiley; 1999. [Google Scholar]
- 18.World Health Organization. Non communicable diseases and mental health. STEPS: planning and implementation in the WHO STEPwise approach to surveillance of noncommunicable diseases (STEPS) [electronic book] World Health Organization. 2004. Available from: http://www.who.int/ncd_surveillance [cited 19 March 2004]
- 19.World Health Organization. Geneva: WHO; 2005. The WHO STEPwise approach to chronic disease risk factor surveillance. [Google Scholar]
- 20.Ng N, Weinehall L, Ohman A. ‘If I don't smoke, I'm not a real man’ – Indonesian teenage boys' views about smoking. Health Educ Res. 2007;22:794–804. doi: 10.1093/her/cyl104. [DOI] [PubMed] [Google Scholar]
- 21.Bartle P. Community empowerment: handbook for mobilizers [electronic book] UN. 1998. Available from: http://www.scn.org/cmp/hbmob.htm [cited 10 April 2006]
- 22.Hudelson PM. Qualitative research for health programs. Geneva: World Health Organization; 1994. [Google Scholar]
- 23.Neiger BL, Thackeray R, Barnes MD, McKenzie JF. Positioning social marketing as a planning process for health education. Am J Health Stud. 2003;18:75–81. [Google Scholar]
- 24.Donovan RJ, Henley N. Social marketing, principles and practice. Melbourne: IP Communication; 2003. [Google Scholar]
- 25.Weinehall L, Hellsten G, Boman K, Hallmans G. Prevention of cardiovascular disease in Sweden: the Norsjö community intervention programme-motives, methods and intervention components. Scand J Public Health Suppl. 2001;56:13–20. [PubMed] [Google Scholar]
- 26.Nissinen A, Berrios X, Pekka P. Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. Bull World Health Org. 2001;79:963–70. [PMC free article] [PubMed] [Google Scholar]
- 27.Krishnan A, Pandav CS, Kapoor SK, Leowski J. Integrated community-based intervention against the risk factors for noncommunicable diseases – early lessons from demonstration project undertaken at Ballabgarh, India. Regional Health Forum. 2006;10:11–21. [Google Scholar]
- 28.Emberson J, Whincup P, Morris R, Walker M, Ebrahim S. Evaluation the impact of population and high-risk strategies for the primary prevention of CVD. Eur Heart J. 2004;25:484–91. doi: 10.1016/j.ehj.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 29.Pearson TA, Lewis C, Wall S, Jenkins PL, Nafziger A, Weinehall L. Dissecting the “black box” of community intervention: background and rationale. Scand J Public Health. 2001;29:5–12. [PubMed] [Google Scholar]
- 30.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–8. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 31.Pearson TA, Wall S, Lewis C, Jenkins PL, Nafziger A, Weinehall L. Dissecting the “black box” of community intervention: lesson from community-wide cardiovascular disease prevention programs in the US and Sweden. Scand J Public Health. 2001;29(Suppl 56):69–78. [PubMed] [Google Scholar]
- 32.Hawe P, Shiell A. Social capital and health promotion: a review. Soc Sci Med. 2000;51:871–85. doi: 10.1016/s0277-9536(00)00067-8. [DOI] [PubMed] [Google Scholar]
- 33.Ng N, Stenlund H, Bonita R, Hakimi M, Wall S, Weinehall L. Preventable risk factors for noncommunicable diseases in rural Indonesia: prevalence study using WHO STEPS approach. Bull World Health Org. 2006;84:305–13. doi: 10.2471/blt.05.023721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brannstrom I, Emmelin M, Dahlgren L, Johansson M, Wall S. Co-operation, participation and conflicts faced in public health: lessons learned from a long-term prevention programme in Sweden. Health Educ Res. 1994;9:317–29. doi: 10.1093/her/9.3.317. [DOI] [PubMed] [Google Scholar]
- 35.Farquhar JW, Fortmann SP, Maccoby N, Haskell WL, Williams PT, Flora JA, et al. The Stanford five-city project: design and methods. Am J Epidemiol. 1985;122:323–34. doi: 10.1093/oxfordjournals.aje.a114104. [DOI] [PubMed] [Google Scholar]
- 36.Shea S, Basch CE, Wechsler H, Lantigua R. The Washington Heights-Inwood healthy heart program: a 6-year report from a disadvantaged urban setting. Am J Public Health. 1996;86:166–71. doi: 10.2105/ajph.86.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacobs DR, Jr, Luepker RV, Mittelmark MB, Folsom AR, Pirie PL, Mascioli SR, et al. Community-wide prevention strategies: evaluation design of the Minnesota heart health program. J Chronic Dis. 1986;39:775–88. doi: 10.1016/0021-9681(86)90080-9. [DOI] [PubMed] [Google Scholar]
- 38.Puska P, Vartiainen E, Tuomilehto J, Salomaa V, Nissinen A. Changes in premature deaths in Finland: successful long-term prevention of cardiovascular diseases. Bull World Health Org. 1998;76:419–25. [PMC free article] [PubMed] [Google Scholar]
- 39.Farquhar JW, Fortmann SP, Flora JA, Taylor CB, Haskell WL, Williams PT, et al. Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. J Am Med Assoc. 1990;264:359–65. [PubMed] [Google Scholar]
- 40.O'Loughlin J, Renaud L, Richard L, Gomez LS, Paradis G. Correlates of the sustainability of community-based heart health promotion interventions. Prev Med. 1998;27:702–12. doi: 10.1006/pmed.1998.0348. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Geneva: World Health Organization; 2002. Noncommunicable diseases and mental health cluster. Innovative care for chronic conditions: building blocks for actions: global report. [Google Scholar]
- 42.Gaziano TA, Galea G, Reddy KS. Scaling up interventions for chronic disease prevention: the evidence. Lancet. 2007;370:1939–46. doi: 10.1016/S0140-6736(07)61697-3. [DOI] [PubMed] [Google Scholar]