Abstract
Objective
Assess the long-term effect of sensory re-training exercises, age, gender, type of surgery, and pre-surgical psychological distress on patients' perception of the interference related to altered sensation two years after orthognathic surgery.
Setting and Sample Population
186 subjects with a developmental dentofacial disharmony were enrolled in a multicenter randomized clinical trial: one center was a community based practice and the other a university-based center.
Methods and Materials
Subjects were randomly allocated to two groups: standard of care mouth opening exercises after BSSO or a progressive series of sensory retraining facial exercises in addition to the opening exercises. At 1, 3, 6, 12, and 24 months after surgery, subjects scored unusual feelings on the face, numbness, and loss of lip sensitivity from “no problem(1)” to “serious problem(7)”. A marginal proportional odds model was fit for each of the ordinal outcomes.
Results
Up to two years after surgery, the opening exercise only group had a higher likelihood of reporting interference in daily activities related to numbness and loss of lip sensitivity than the sensory retraining exercise group. The difference between the two groups was relatively constant. Older subjects and those with elevated psychological distress before surgery reported higher burdens related to unusual facial feelings, numbness, and loss of lip sensitivity (P<0.02).
Conclusion
The positive effect of sensory retraining facial exercises observed after surgery is maintained over time. Clinicians should consider the patient's age and psychological well-being prior to providing pre-surgical counseling regarding the impact on daily life of persistent altered sensation following a mandibular osteotomy.
Keywords: age, altered sensation, orthognathic surgery, psychological well-being, sensory retraining
Introduction
Patients who have orthognathic surgery routinely accept short-term risks and discomforts, such as changes in facial sensation, with the expectation of long-term benefits in quality of life. Although the proportion of patients who experience altered sensations decreases over time after surgery, greater than 60% of patients who have a bilateral sagittal split osteotomy report some form of persistent altered sensation (1) defined as an altered sensation that persists for at least six months after surgery (2), or a difference from the sensation experienced before surgery.(3) The lack of treatment options to enhance nerve recovery or to promote accommodation to a sensory deficit is unfortunate because patients with persistent altered sensation tend to report more difficulties with orofacial function and with daily activities long-term after surgery.(4,5,6,7)
Recently, we have shown that sensory retraining or sensory reeducation, consisting of a set of simple facial exercises performed daily, is an effective cognitive behavioral therapy for reducing subjects' perceptions of the burden associated with negative altered sensations in the short term after mandibular ostetomy.(8) At six months after surgery, subjects who performed the sensory retraining exercises reported less problem related to residual numbness and loss of lip sensitivity than those subjects who performed only the standard of care mouth opening exercises.(8) This difference between the two exercise groups appears to be related to the difference in how the “retrained” individual experiences or interprets tactile stimuli rather than any difference in nerve recovery or repair.(9) The positive effect of the sensory retraining persisted even after the exercises were stopped. At two years after surgery, patients who performed only the opening exercises were significantly more likely to report the presence of an altered facial sensation than those who used both the sensory retraining exercises and the opening exercises.(10)
Other factors may also affect how a patient perceives an alteration in sensation. Older patients are more likely to report persistent neurosensory deficit(10,11,12) and to experience functional deficits than younger patients.(13) Psychological distress, particularly depression and anxiety, has been associated with elevated pain and decreased satisfaction following a diverse variety of surgical procedures.(14) For orthognathic surgery patients, psychological distress prior to surgery has been shown to negatively influence patients' perceptions of their recovery after surgery(15) and their perception of their oral health and quality of life in the longer term (2 yrs) after orthognathic surgery(16)
The aims of this analysis were twofold: first, to assess whether sensory retraining exercises, performed only for the first six months after surgery, have a long-term effect on patient self-report of daily life interference related to altered sensation; and second, to assess whether age, gender, the type of surgery, or pre-surgical psychological distress may affect patients' perception of daily life interference long-term.
Methods
Subjects
Subjects were recruited from the Oral and Maxillofacial Surgery Clinic at the University of North Carolina at Chapel Hill (UNC) or from University Oral Maxillofacial Surgery in Charlotte, NC, a community based practice. Consecutive patients, age 13 to 50, who were scheduled for a bilateral sagittal split osteotomy alone or with LeFort I osteotomy to correct a severe malocclusion and/or a developmental disharmony between December 2001 and April 2005 were enrolled in a multi-center, double blind, two-arm parallel group, stratified block randomized controlled clinical trial. The clinical trial was designed to evaluate the effects of sensory retraining, a non-invasive rehabilitative therapy, on nerve recovery and patients' perception of altered sensation following orthognathic surgery. Within the stratification factors (number of jaws and genioplasty), subjects were randomized to receive either instruction on standard opening exercises only after surgery or the opening exercises plus a 3-level progressive series of sensory re-training facial exercises. The progressive series of facial exercises was designed to increasingly challenge patients to discriminate moving from non-moving touch (1 week post-surgery); the orientation of moving touch (~1 month post); and the direction of moving touch (3 months post). Subjects were instructed to perform the exercises first in front of a mirror and then to practice visualization with their eyes closed. The opening-only exercise program was based on current clinical practice at our institution. Details of the sensory retraining trial and exercise protocol are described in Phillips et al.(8)
Outcome Measures
Prior to surgery and at 1, 3, 6, 12, and 24 months following surgery, participants were instructed to report the interference (problem) that unusual feelings on the face, numbness in facial areas, and loss of lip sensitivity had had on their daily life during the past two weeks.. These three items, theorized to be linked to the hypothesized effect of sensory retraining, were identified prior to the initiation of the trial as primary efficacy outcomes.
For each item, the response could range from “no problem(1)” to “serious problem(7)”. The percentage of patients who reported moderate to severe problem decreased over time creating a highly skewed distribution of responses at 12 and 24 months. For this reason, the responses to each item at each visit were re-scaled reducing the 7 point scale to 3, with 1 =no problem, 2 = original 2,3,4, little to somewhat of a problem, and 3 = original 5,6,7 moderate to serious problem.
Explanatory Variables
Exercise, time, and the exercise x time interaction were included in all final models. Demographic characteristics of interest were gender and the age at the time of surgery. Age was centered at the overall mean and standardized so that 1 unit represented a decade. Surgical characteristics of interest were type of procedure (BSSO only vs 2 jaw) and presence of genioplasty.
Assessment of Psychological Well-Being
Prior to surgery, psychological distress, optimism, and expected discomfort were assessed and examined to determine if these factors were associated with the patient reported burden from altered sensation. Psychological distress was assessed using the Symptom Checklist-90 Revised (SCL-90R).(17) The global severity index, an overall measure that combines information on both the number of symptoms and the intensity of the perceived distress, was calculated and converted, using the non-psychiatric gender and age-specific patient norms, to a standardized T-score (TSGSI).
Optimistic style was measured using the Life Orientation Test, a 10 item questionnaire with each item scored on a 4 point scale from “strongly agree” to “strongly disagree”. An overall score was calculated as the sum of all items after reversal of negatively worded items.(18)
The Post-surgical Sequelae Expectations subscale of the Short-term Expectations Questionnaire has 7 items rated on a seven-point scale reflecting the patient's expected discomfort during the first month after surgery. The 7-point scale for each item ranged from “expect no discomfort”(1) to “expect much discomfort” (7).(19)
Statistical Analysis
In an intent-to-treat framework, marginal proportional odds models with generalized estimating equations and a working independence correlation structure were performed separately for each outcome. As preliminary analyses, models were fit separately for the demographic factors (age and gender), psychological well-being factors (psychological distress, optimism, and expected discomfort before surgery), and clinical factors (surgical procedure and presence of genioplasty). Time was included in all of the preliminary models. If the global generalized score test was statistically significant (p<0.05), those explanatory variables in the set for which the generalized score test was statistically significant after adjusting for all other covariates were included in the final model. In addition, the final model included visit (1, 3, 6, 12 and 24 months), exercise group (the primary explanatory variable) and the time-by-exercise group interaction. The interaction was not statistically significant for any of the outcomes (P>0.05) and the models were reduced. Model results are given for the final models only.
Results
Of the 186 subjects enrolled, 94 were in the Opening Exercise Only group and 92 in the Sensory Retraining with Opening Exercises group. The subjects were young adults (x=25.1yrs, sd=11.9). The majority were female (71%) and almost all (93%) were Caucasian. Sixty-one percent had a BSSO only and 30% had a genioplasty. As expected, based on randomization, the percent of subjects who had a BSSO only or a genioplasty were very similar for the two exercise groups (P>0.22). The two exercise groups were also similar in terms of average age and percentages of females and Caucasians (P>0.58). Details of the pre-surgery comparisons of the exercise groups and the two centers were presented previously in Phillips et al. (8)
Unusual Feelings
At six months after surgery, approximately half of the subjects in both exercise groups continued to report at least mild interference in everyday life related to unusual feelings in the face or mouth. At two years after surgery, those reporting interference had decreased to roughly one third (Table 1). In the preliminary analyses, the global test for the surgical characteristics was not statistically significant (P= 0.14) while the global tests for the demographic characteristics and psychological well-being were significant (P <0.0001). Age (P <0.0001), psychological distress (P<0.0001), and optimism(P=0.002) contributed to the variability in the subject's perception of problems with unusual feelings after adjusting for other factors in the respective preliminary models. The pattern of responses for the two exercise groups over time was similar. (Fig. 1) In the final model, the two exercise groups did not differ significantly in the overall likelihood of reporting no problem associated with unusual feelings (P =0.94). Age, psychological well-being, and time were statistically significant (Table 2). Older patients and those who had elevated psychological distress before surgery were more likely to report interference related to unusual feelings (Fig 2,3).
Table 1.
Percent of subjects in each exercise group reporting no, little to somewhat, or moderate to serious problem related to altered sensation
| 1 mo. | 3 mo. | 6 mo. | 1 year | 2 years | |
|---|---|---|---|---|---|
| Unusual Feeling | |||||
|
| |||||
| % No Problem | |||||
| Opening | 22 | 30 | 51 | 60 | 66 |
| Sensory | 16 | 43 | 57 | 59 | 67 |
|
| |||||
| % Little to Somewhat | |||||
| Opening | 55 | 58 | 47 | 35 | 27 |
| Sensory | 53 | 47 | 37 | 39 | 28 |
|
| |||||
| % Moderate to Serious | |||||
| Opening | 22 | 12 | 2 | 5 | 7 |
| Sensory | 30 | 10 | 5 | 2 | 6 |
|
| |||||
| Numbness | |||||
|
| |||||
| % No Problem | |||||
| Opening | 6 | 12 | 23 | 32 | 36 |
| Sensory | 4 | 19 | 36 | 38 | 44 |
|
| |||||
| % Little to Somewhat | |||||
| Opening | 46 | 63 | 68 | 53 | 51 |
| Sensory | 42 | 62 | 51 | 54 | 45 |
|
| |||||
| % Moderate to Serious | |||||
| Opening | 48 | 25 | 9 | 15 | 13 |
| Sensory | 53 | 19 | 13 | 8 | 10 |
|
| |||||
| Loss of Lip Sensitivity | |||||
|
| |||||
| % No Problem | |||||
| Opening | 21 | 33 | 38 | 55 | 58 |
| Sensory | 21 | 39 | 56 | 66 | 67 |
|
| |||||
| % Little to Somewhat | |||||
| Opening | 48 | 49 | 55 | 36 | 32 |
| Sensory | 46 | 46 | 34 | 27 | 24 |
|
| |||||
| % Moderate to Serious | |||||
| Opening | 31 | 18 | 7 | 9 | 10 |
| Sensory | 34 | 16 | 10 | 8 | 9 |
Figure 1.
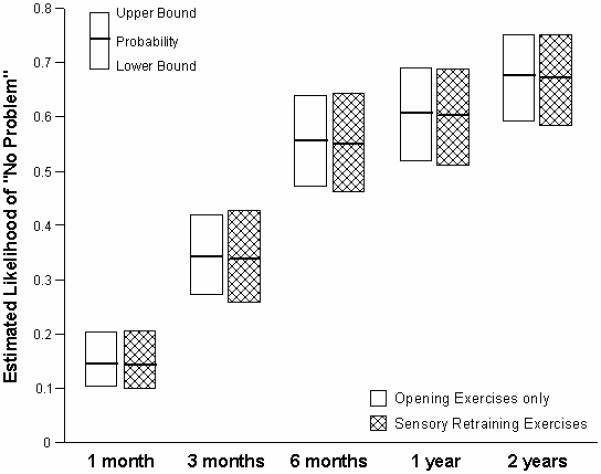
Estimated Likelihood of “No Problem” related to Unusual Feelings by Exercise Group
Table 2.
The generalized score test results from the final model examining interference in daily life associated with unusual feelings
| Effect | DF | Chi-Square | P-value |
|---|---|---|---|
| Age | 1 | 18.02 | <.0001 |
| Global severity index | 1 | 17.33 | <.0001 |
| Optimism | 1 | 2.98 | 0.0844 |
| Sensory Retraining | 1 | 0.01 | 0.9353 |
| Time | 4 | 101.43 | <.0001 |
Figure 2.
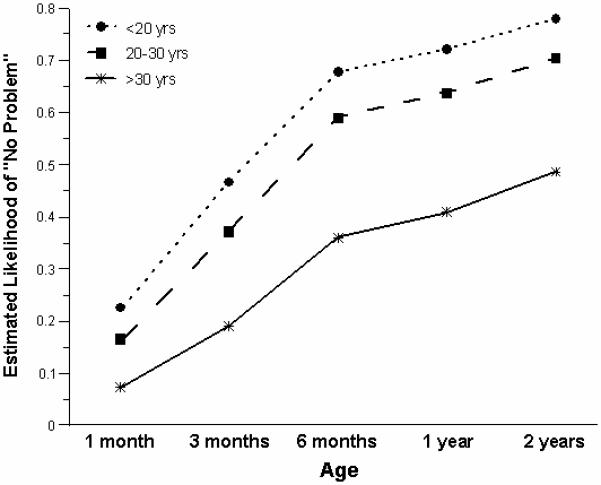
Estimated Likelihood of “No Problem” related to Unusual Feelings for Three Age Groups
Figure 3.
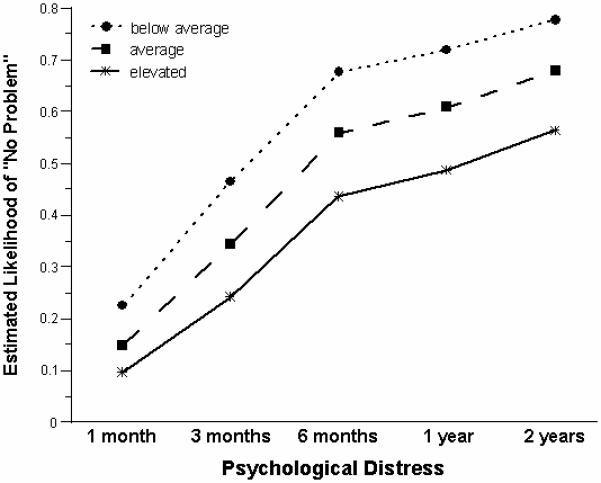
Estimated Likelihood of No “Problem” related to Unusual Feelings for Subjects who self-reported Below Average, Average, and Elevated Psychological Distress before Surgery
Numbness
By two years after surgery, 36% of the Opening only group reported no problem related to numbness in facial areas or around the mouth compared to 23% at six months after surgery. For the Sensory Retraining group, 44% reported no problems with numbness at 2 years after surgery, compared to 36% at six months (Table 1). In the preliminary analyses, the global test was statistically significant for all three sets of explanatory factors (demographic, P<0.0001; psychological, P<0.0001; clinical, P= 0.05). Although optimism (P= 0.002), expected discomfort (P= 0.03), and the presence of a genioplasty(P=0.04) were significant contributors to the explanation of the subject's perception of problems with numbness in the respective preliminary analyses, they were not statistically significant contributors in the final model (P>0.06; Table 3). The group by time interaction was not statistically significant (P = 0.30) indicating that the relative difference between the groups was consistent over time (Fig 4). The sensory retraining group was more likely to report less interference in daily life associated with numbness than the opening only group but this overall difference was not statistically significant after controlling for the other explanatory variables (P = .35). Age, psychological well-being, and time were significantly associated with the level of interference from numbness (Table 3). Older patients and those who reported elevated psychological distress were more likely to report interference from numbness. (Figures 5, 6).
Table 3.
The generalized score test results from the final model examining interference in daily life associated with numbness
| Effect | DF | Chi-Square | P-value |
|---|---|---|---|
| Age | 1 | 11.55 | 0.0007 |
| Global severity index | 1 | 9.45 | 0.0021 |
| Optimism | 1 | 3.32 | 0.0684 |
| Expectations | 1 | 3.50 | 0.0615 |
| Genioplasty | 1 | 2.84 | 0.0919 |
| Sensory Retraining | 1 | 0.87 | 0.3507 |
| Time | 4 | 99.26 | <.0001 |
Figure 4.
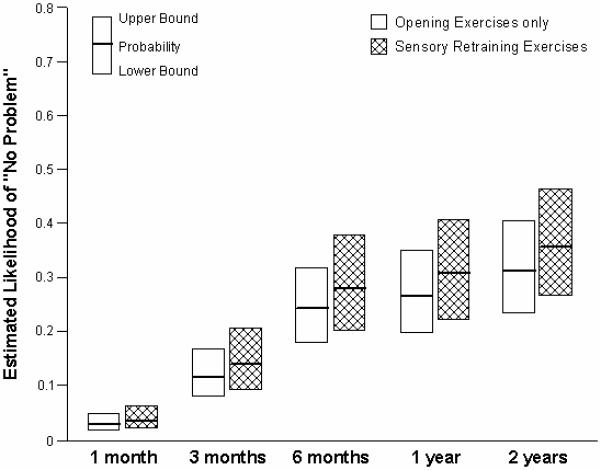
Estimated Likelihood of “No Problem” related to Numbness by Exercise Group
Figure 5.
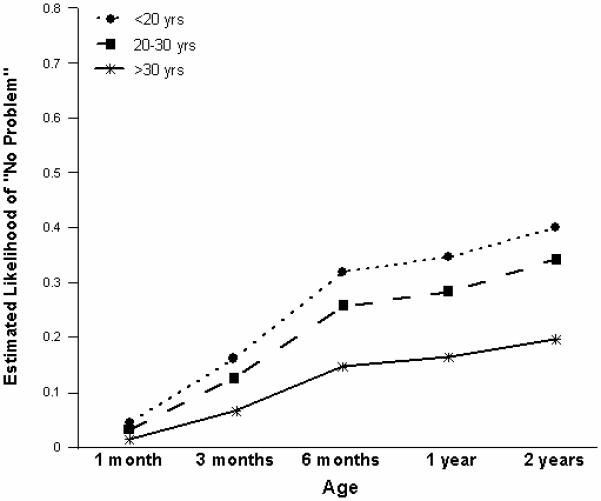
Estimated Likelihood of “No Problem” related to Numbness for Three Age Groups
Figure 6.
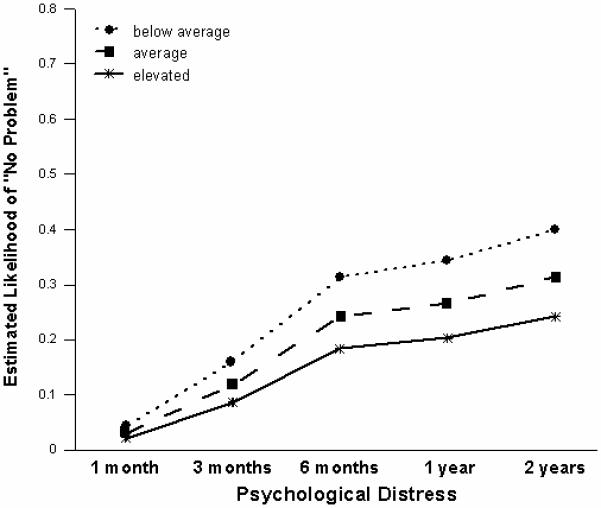
Estimated Likelihood of “No Problem” related to Numbness for Subjects who self-reported Below Average, Average, and Elevated Psychological Distress before Surgery
Loss of Lip Sensitivity
At six months after surgery, 38% of the Opening only group and 56% of the Sensory retraining group reported no problem associated with loss of lip sensitivity. At two years after surgery, those reporting no problem increased to 58% and 67%, respectively (Table 1). In the preliminary analyses, the global test was not statistically significant for clinical factors (P=.14) but was for both demographic and psychological factors (P<0.0001). Although optimism (P=.003) and expected discomfort (P=0.02) were statistically significant contributors in the preliminary models, they were not in the final model (P>.06). The exercise group by time interaction was not statistically significant (P =0.64) indicating that the difference between the exercise groups was consistent over time (Fig 7). Over the long-term recovery period, the sensory retraining group was more likely to report less interference associated with loss of lip sensitivity than the opening only group although this difference was not statistically significant (P=0.16) after adjustment for age and psychological distress. Consistent with unusual feelings and numbness, only age, psychological well-being, and time were statistically significant contributors to the explanation of the overall variability in the subject's perception of problems or interference in daily life related to loss of lip sensitivity (Table 4). Older patients and those who reported elevated psychological distress before surgery were more likely to report interference (Figures 8, 9).
Figure 7.

Estimated Likelihood of “No Problem” related to Loss of Lip Sensitivity by Exercise Group
Table 4.
The generalized score test results from the final model examining interference in daily life associated with loss of lip sensitivity
| Effect | DF | Chi-Square | P-value |
|---|---|---|---|
| Age | 1 | 20.92 | <.0001 |
| Global severity index | 1 | 5.28 | 0.0215 |
| Optimism | 1 | 1.13 | 0.2877 |
| Expectations | 1 | 3.49 | 0.0619 |
| Sensory Retraining | 1 | 2.00 | 0.1571 |
| Time | 4 | 84.93 | <.0001 |
Figure 8.
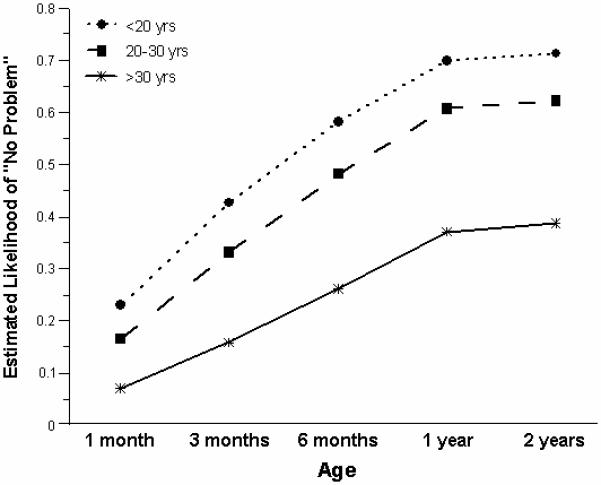
Estimated Likelihood of “No Problem” related to Loss of Lip Sensitivity for Three Age Groups
Figure 9.
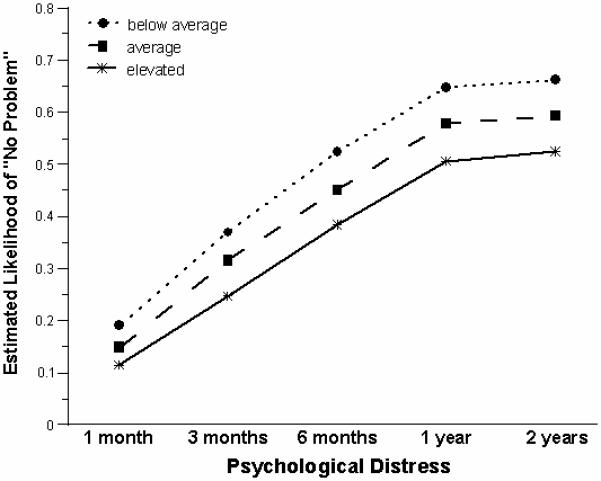
Estimated Likelihood of “No Problem” related to Loss of Lip Sensitivity for Subjects who self-reported Below Average, Average, and Elevated Psychological Distress before Surgery
Discussion
The demographic characteristics of the patients who participated in this study were representative of patients who have orthognathic surgery in the “Standard Metropolitan Areas” of the university and community-based practices that participated in this study. The generalizations, though, may not apply to non-Caucasians.
The sensory branches of the trigeminal nerve carry information about facial movements, pressures, and expressions to those areas of the cerebral cortex that underlie recognition and discrimination of skin stimuli i.e. “how the face feels”. The primary efficacy results at 6 months (8) and these longer term recovery analyses at 24 months after orthognathic surgery indicate that for patients who experience an acute nerve injury, as is highly likely during a mandibular osteotomy, the simple, non-invasive sensory retraining facial exercises, which require only an inexpensive cosmetic brush and a mirror, are an effective cognitive behavioral therapy to promote accommodation to a sensory deficit on the face. At six months after surgery, patients who participated in the sensory retraining exercise protocol reported less objectionable impression or burden associated with altered sensation on the face,(8) and were more adept at perceiving touch (accommodation) even though there was no improvement in the ability to discriminate two distinct points of contact from one (nerve recovery).(20) The two year follow-up results indicated that the overall effect of the sensory retraining exercises continued even after the exercises had been discontinued. The proportion of patients who reported the presence of altered sensation decreased over time in both exercise groups, but the proportion who reported residual deficit was significantly lower for those patients who participated in the sensory retraining protocol.(10) This result does not necessarily reflect a difference in actual nerve recovery but more likely reflects the sensory retraining patients' accommodation to any residual sensory deficit and desensitization to the altered sensation.21) Whether this positive benefit is generalizable to individuals who experience facial altered sensation from sources other than acute nerve injury is not known.
An important component of the retraining exercises is the visual feedback provided by performing the exercises in front of a mirror. This elicits two different sensory events, the sensation of the brush on the facial skin and the sight of the brush on the face. Recent experimental studies have shown that viewing a body surface can directly enhance tactile perception and detection(22,23) even when the “touch” is not physical but a mirrored reflection.(24,25) It may be that encouraging patients to perform the sensory retraining exercises with a small handheld mirror for a short period of time, perhaps 1 minute, 6 to 10 times per day would be as or more effective than the exercise protocol used in the clinical trial (~ 10 minutes three times per day)(8)
Younger patients were more likely to report less interference related to altered sensation regardless of the exercise program used. In general, younger patients are more likely to report better postsurgical oral health(26) and less functional deficit associated with altered sensation than older patients.(13) Whether these findings are a result of cognitive or physiological differences between younger and older patients is not known. These results suggest that pre-surgical counseling regarding the likelihood of a persistent altered sensation should be modified depending on the subject's age.
Patients who did not report elevated psychological distress prior to surgery were more likely to report less interference. Psychological status as indicated by the GSI score on the SCL-90-R, the same measure used in this study, was reported as having a direct influence on oral health with elevated distress scores associated with poorer postsurgical oral health even at two years after surgery.(27) The findings from this and previous studies(15) including patients who were psychologically distressed prior to orthognathic surgery are congruent with the findings from studies on diverse surgical procedures.(28,29) Patients who are psychologically distressed prior to surgery tend to report more discomfort or difficulty with symptoms, general health, and overall recovery in the first few months after surgery than those who are not distressed. A recent evidence-based literature review(14) on clinical recovery concluded that the “preoperative consideration of attitudinal (expectations, optimism) and mood (anxiety, depression) factors will assist the surgeon in estimating both the speed and extent of recovery.” These findings highlight the importance of improving patient management strategies for orthognathic surgery patients who report symptoms of psychological distress before surgery.
Everyone is faced with daily stressors that can influence mood and psychological well-being. Add for patients the anxiety of a surgical procedure with general anesthesia, concerns about recovery and finances and it is not surprising that in general, orthognathic surgery patients tend to exhibit higher levels of anxiety than non-patients (30) and elevated interpersonal sensitivity.(31,32) Orthodontists and oral and maxillofacial surgeons should expect that approximately 15 to 20% of orthognathic surgery patients will be psychologically distressed prior to surgery. These percentages have been reported previously in clinical studies(31, 33) and mirror that in the general population.(34,35) For these reasons, standardized screening is recommended as a routine part of the presurgical evaluation of a patient who is a candidate for orthognathic surgery. Psychological distress, as indicated on a self-report assessment such as the SCL-90R, can alert the orthodontist or the surgeon to explore those areas that may complicate or interfere with a patient's treatment and recovery from surgery.
During the post-surgical orthodontic treatment phase, the orthodontist will have the most frequent clinical contact with the patient and may be asked for advice and counsel regarding the resolution of altered sensation. Orthodontists and oral and maxillofacial surgeons are encouraged to provide orthognathic surgery patients, particularly those who have a mandibular osteotomy, with these simple facial exercises, which require only an inexpensive cosmetic brush and a mirror. The exercises could be explained to patients before surgery and a reminder included in a letter or telephone call after surgery.
Conclusion
The findings from this randomized clinical trial indicate that
Sensory retraining exercises provide an overall long-term benefit following mandibular osteotomy.
Older patients and patients who report elevated psychological distress prior to surgery have a greater likelihood of reporting that persistent altered sensation has a negative effect on daily life activities.
Clinical Relevance.
For patients who experience an acute injury to the inferior alveolar nerve, sensory retraining exercises, a non-invasive set of cognitively based facial exercises, provide an overall long-term benefit in terms of accommodation to altered sensation, particularly hypoesthesia. Older patients and patients who report elevated psychological distress prior to mandibular osteotomy have a greater likelihood of reporting that persistent altered sensation two years after surgery has a negative effect on daily life activities.
Acknowledgement
As a Phase III clinical trial, a Data Safety and Monitoring Board was required by NIDCR to monitor the project. This project was supported in part by NIH grant DE013967.
References
- 1.Phillips C, Essick G, Zuniga J, Tucker M, Blakey GH., III Qualitative Descriptors Used by Patients following Orthognathic Surgery to Portray Altered Sensation. J Oral Maxillofac Surg. 2006;64:1751–1760. doi: 10.1016/j.joms.2005.11.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merskey H, Bogduk N. Classification of chronic pain:descriptions of chronic pain syndromes and definitions of pain terms. IASP Press; Seattle: 1994. [Google Scholar]
- 3.Ylikontiola L, Kinnunen J, Oikarinen K. Factors affecting neurosensory disturbance after mandibular bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 2000;58:1234–1239. doi: 10.1053/joms.2000.16621. discussion 1239-1240. [DOI] [PubMed] [Google Scholar]
- 4.Westermark A, Englesson L, Bongenhielm U. Neurosensory function after sagittal split osteotomy of the mandible: A comparison between subjective evaluation and objective assessment. Int J Adult Orthodon Orthognath Surg. 1999;14:268–275. [PubMed] [Google Scholar]
- 5.Phillips C, Essick G, Blakey GH, III, Tucker M. Relationship between Patients' Perceptions of Post-surgical Sequelae and Altered Sensation following BSSO. J Oral Maxillofac Surg. 2007;65:597–607. doi: 10.1016/j.joms.2005.12.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey WS, Phillips CL, Essick GK. Neurosensory impairment and patient perception of recovery following orthognathic surgery. J Dent Res. 2001;80(Special Issue):187. [Google Scholar]
- 7.Lemke RR, Clark GM, Bays RA, Tiner BD, Rugh JD. Effects of hypesthesia on oral behaviors of the orthognathic surgery patient. J Oral Maxillofac Surg. 1998;56:153–157. doi: 10.1016/s0278-2391(98)90856-4. discussion 158-60. [DOI] [PubMed] [Google Scholar]
- 8.Phillips C, Essick G, Preisser JS, Turvey TA, Tucker M, Lin D. Sensory Retraining following orthognathic surgery: effect on patient perception of altered sensation. J Oral Maxillofac Surg. 2007;65:1162–1173. doi: 10.1016/j.joms.2006.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Essick GK, Phillips C, Turvey TA, Tucker M. Facial altered sensation and sensory impairment after orthognathic surgery. Int. J Oral Maxillofac Surg. 2007;36:577–582. doi: 10.1016/j.ijom.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips C, Kim S, Essick G, Tucker M, Turvey TA. Sensory retraining following orthognathic surgery: Effect on Patient Report of the Presence of Altered Sensation. Am J Ortho Dentofac Orthop. 2009;136:788–794. doi: 10.1016/j.ajodo.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Westermark A, Bystedt H, von Konow L. Inferior alveolar nerve function after sagittal split osteotomy of the mandible: Correlation with degree of intraoperative nerve encounter and other variables in 496 operations. Br J Oral Maxillofac Surg. 1998;36:429–433. doi: 10.1016/s0266-4356(98)90458-2. [DOI] [PubMed] [Google Scholar]
- 12.Van Sickels JE, Hatch JP, Dolce C, Bays RA, Rugh JD. Effects of age, amount of advancement, and genioplasty on neurosensory disturbance after a bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 2002;60:1012–1017. doi: 10.1053/joms.2002.34411. [DOI] [PubMed] [Google Scholar]
- 13.August M, Marchena J, Donady J, Kaban L. Neurosensory deficit andfunctional impairment after sagittal ramus osteotomy: a long-term follow-upstudy. J Oral Maxillofac Surg. 1998;56:1231–1235. doi: 10.1016/s0278-2391(98)90595-x. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberger PH, Jokl P, Ickovics J. Psychosocial factors and surgical outcomes: an evidence-based literature review. J Am Acad Orthop Surg. 2006;14:397–405. doi: 10.5435/00124635-200607000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Phillips C, Kiyak HA, Bloomquist D, Turvey TA. Perceptions of recovery and satisfaction in the short term after orthognathic surgery. J Oral Maxillofac Surg. 2004;62:535–544. doi: 10.1016/j.joms.2003.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatch JP, Rugh JD, Clark GM, Keeling SD, Tiner BD, Bays RA. Health-related quality of life following orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1998;13:67–77. [PubMed] [Google Scholar]
- 17.Derogatis LR. The SCL-90-R administration, scoring, and procedures. NCS Pearson; Eagle, MN: 1994. [Google Scholar]
- 18.Scheier MF, Carver CS. Optimism, coping and health: assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 19.Phillips C, Bailey L, Kiyak HA, Bloomquist D. Effects of a computerized treatment simulation on patient expectations for orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 2001;16:87–98. [PMC free article] [PubMed] [Google Scholar]
- 20.Essick G, Phillips C, Zuniga J. Effect of Facial Sensory Retraining on Sensory Thresholds. J Dent Res. 2007;86:571–575. doi: 10.1177/154405910708600616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Essick GK, Phillips C, Kim SK, Zuniga J. Sensory retraining following orthognathic surgery: Effect on threshold measures of sensory function. J Oral Rehabilitation. 2009;36:415–426. doi: 10.1111/j.1365-2842.2009.01954.x. [DOI] [PubMed] [Google Scholar]
- 22.Fiorio M, Haggard P. Viewing the body prepares the brain for touch: effects of TMS over somatosensory cortex. European Journal of Neuroscience. 2005;22:773–777. doi: 10.1111/j.1460-9568.2005.04267.x. [DOI] [PubMed] [Google Scholar]
- 23.Taylor-Clarke M, Kennett S, Haggard P. Vision modulates somatosensory cortical processing. Current Biology. 2002;12:233–236. doi: 10.1016/s0960-9822(01)00681-9. [DOI] [PubMed] [Google Scholar]
- 24.Ro T, Wallace R, Hagedorn J, Farne A, Pienkos E. Visual enhancing of tactile perception in the posterior parietal cortex. J Cogn Neurosci. 2004;16:24–30. doi: 10.1162/089892904322755520. [DOI] [PubMed] [Google Scholar]
- 25.Sathian K, Greenspan AI, Wolf SL. Doing it with mirrors: a case study of a novel approach to neurorehabilitation. Neurorehabil and Neural Repair. 2000;14:73–76. doi: 10.1177/154596830001400109. [DOI] [PubMed] [Google Scholar]
- 26.Scott AA, Hatch JP, Rugh JD, Rivera SM, Hoffman TJ, Dolce C, Bays RA. Psychosocial predictors of high-risk patients undergoing orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999;14:113–124. [PubMed] [Google Scholar]
- 27.Scott AA, Hatch JP, Rugh JD, Rivera SM, Hoffman TJ, Dolce C, Bays RA. Psychosocial predictors of high-risk patients undergoing orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999;14:113–124. [PubMed] [Google Scholar]
- 28.Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine. 2000;25:2616–2621. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 29.Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery. Perspectives from Psychoneuroimmunology. Am Psychol. 1998;53:1209–1218. doi: 10.1037//0003-066x.53.11.1209. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham Sj, Gilthorpe MS, Hunt NP. Are orthognathic patients different? Eur J Orthod. 2000;22:195–202. doi: 10.1093/ejo/22.2.195. [DOI] [PubMed] [Google Scholar]
- 31.Phillips C, Bennett ME, Broder HL. Dentofacial disharmony: psychological status of patients seeking a treatment consultation. Angle Orthod. 1998;68:547–556. doi: 10.1043/0003-3219(1998)068<0547:DDPSOP>2.3.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen B, Zhang ZK, Wang X. Factors influencing postoperative satisfaction of orthognathic surgery patients. Int J Adult Orthodon Orthognath Surg. 2002;17:217–222. [PubMed] [Google Scholar]
- 33.Hatch JP, Rugh JD, Bays RA, Van Sickels JE, Keeling SD, Clark GM. Psychological function in orthognathic surgical patients before and after bilateral sagittal split osteotomy with rigid and wire fixation. Am J Orthodon Dentofacial Orthop. 1999;115:536–543. doi: 10.1016/s0889-5406(99)70276-3. [DOI] [PubMed] [Google Scholar]
- 34.Shih M, Hootman JM, Strine T, Chapman DP, Brady TJ. Serious psychological distress in US adults with arthritis. J Gen Intern Med. 2006;21:1160–1166. doi: 10.1111/j.1525-1497.2006.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Center for Health Statistics . Serious Psychological Distress. Early Release of Selected Estimates Based on Data from the January-June 2004 National Health Interview Survey. U.S. Department of Health and Human Services – Center for Disease Control and Prevention; Hyattsville, MD: [Google Scholar]


