Decades of research in psychiatry have shown that anxiety disorders and substance use disorders co-occur at greater rates than would be expected by chance alone. This co-occurrence, or comorbidity, between anxiety and substance use disorders has generated considerable interest among researchers and clinicians, due to its relatively high prevalence, developmental and maintenance characteristics, clinical impact, and unique treatment factors. It is also notable that while these disorders are commonly found in a comorbid state and have generated a great deal of focused research attention, further studies are necessary before critical questions about how to best treat comorbid anxiety and substance use disorders are resolved through empirical inquiry rather than expert opinion.
Prevalence of Comorbid Anxiety and Substance Use Disorders
Anxiety and substance use disorders are among the most frequent psychiatric problems in the United States, with lifetime rates of 28.8% and 14.6%, respectively.1 The presence of an anxiety or substance use disorder is also a risk factor for the presence of the other disorder, as shown in both epidemiological and clinical samples.2,3 Recent analyses from an epidemiological survey focused on comorbidity, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; N=43,093), offered a compelling demonstration of this shared risk, revealing striking rates of co-occurring anxiety and substance use disorders.4,5
Examination of the results of these studies, listed in the Table, shows that anxiety disorders, when considered together, were significantly related to both alcohol and drug use disorders. The pattern of results also shows that anxiety disorders were more strongly related to substance dependence (odds ratio [OR] = 3.0-6.0) than substance abuse (OR = 1.2-1.6).4 Generalized anxiety disorder (GAD) and panic disorder (PD) with and without agoraphobia had the highest associations with substance use disorders.4 The comorbidity rates between posttraumatic stress disorder and obsessive-compulsive disorder with substance use disorders were not evaluated in the first wave of NESARC data collection. However, in the National Comorbidity Survey Replication, Kessler and colleagues1 examined these associations and found that PTSD and OCD were each associated with alcohol use disorders, but not drug use disorders.
Table 1. Comorbidity of Anxiety and Substance Use Disordersa.
| Alcohol Use Disordersb,c | Drug Use Disordersb,c | |||
|---|---|---|---|---|
| Anxiety Disorder | Alcohol Abuse | Alcohol Dependence | Drug Abuse | Drug Dependence |
| Specific Phobia | 1.2 | 2.7 | 1.6 | 3.8 |
| Social Phobia | 1.2 | 2.7 | 1.7 | 4.5 |
| Generalized Anxiety Disorder | 1.1 | 2.8 | 2.0 | 9.5 |
| Panic Disorder w/ Agoraphobia | 1.0 | 3.5 | 3.2 | 9.2 |
| Panic Disorder w/o Agoraphobia | 1.2 | 2.9 | 1.4 | 6.4 |
| Any Anxiety Disorder | 1.2 | 3.0 | 1.6 | 6.0 |
Development and Maintenance of Comorbid Anxiety and Substance Use Disorders
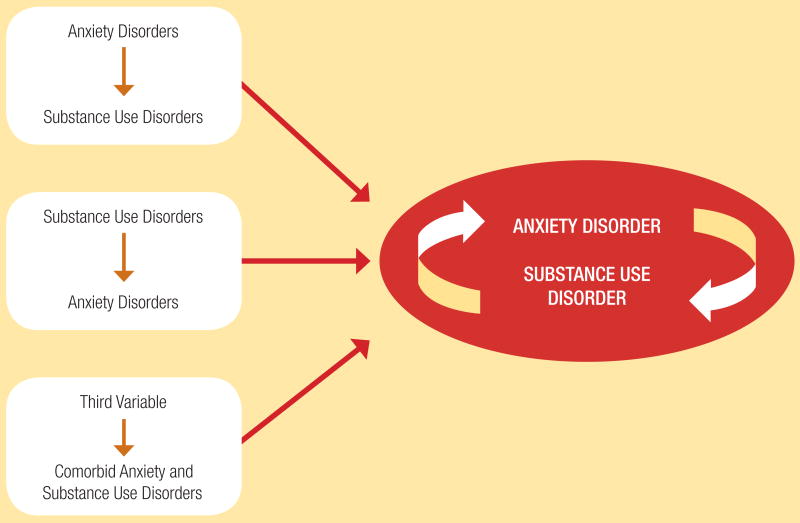
Research and clinical experience also reveals that when anxiety and substance use disorders co-occur, these disorders are functionally intertwined in both the development and maintenance of comorbidity. As detailed in the Figure, 3 primary pathways to comorbidity have been suggested from the culmination of studies to date.6 These pathways include: 1) a self-medication pathway wherein an anxiety disorder leads to a substance use disorder; 2) a substance-induced anxiety disorder pathway; and 3) a third variable pathway (e.g., genetics or anxiety sensitivity).
Figure 1. Development and Mutual Maintenance of Comorbid Anxiety and Substance Use Disorders.
Evidence from the NESARC study indicated that substance-induced anxiety disorders are quite rare, occurring in only 0.2% of comorbid cases.7 Also, a recent review of the available empirical literature showed that anxiety disorders predate substance use disorders in at least 75% of cases, further supporting the increased prevalence of the self-medication pathway compared to the alternative mechanisms.2 More research is necessary before the third variables (e.g., genetics or anxiety sensitivity) are more fully evaluated as explanatory models of anxiety disorder-substance use disorder comorbidity. Regardless of the course through which the comorbidity between anxiety and substance use disorders coalesce, the pathways together lead to a mutual maintenance pattern wherein each disorder perpetuates the other.6 This mutual maintenance pattern has implications for both the clinical impact and treatment of comorbid anxiety and substance use disorders.
Clinical Impact of Comorbidity on Anxiety and Substance Use Disorders
The importance of high comorbidity rates, developmental patterns, and mutual maintenance between co-occurring anxiety and substance use disorders is underscored by the clinical impact of these disorder pairings. Considering the mutual maintenance pattern of this comorbidity, it is not surprising that both anxiety disorders and substance use disorders impact the course and treatment outcome for the counterpart condition. For example, studies have shown that anxiety disorders are related to an increased severity of lifetime alcohol use disorders, increased lifetime service utilization among individuals with a substance use disorder, increased severity of alcohol withdrawal, and higher relapse rates following substance abuse treatment.8-12
Alternatively, the presence of a substance use disorder can impact the course of anxiety disorders. Along these lines, a 12-year prospective study showed that the presence of a substance use disorder decreased the recovery rate and increased the likelihood of recurrence of GAD.13 Of particular concern are epidemiological data showing that the presence of a substance use disorder is associated with an elevated risk of suicide in patients with PD when compared to patients with PD and no comorbid substance use disorder.14 Taken together, these collective findings highlight the importance of finding new and innovative approaches to treating co-occurring anxiety and substance use disorders.
Novel Approaches to Treatment
Several investigators have evaluated novel treatments of anxiety disorders comorbid with substance use disorders. Based on the mutual maintenance pattern previously described, most studies have attempted to find treatments addressing both psychiatric concerns. Research in this area continues to develop, and includes both pharmacotherapy and psychotherapy as primary treatment approaches for these dual diagnoses. The current state of the science has illuminated important treatment considerations unique to patients who suffer from comorbid anxiety and substance use disorders.
Pharmacotherapy
A variety of medications have been targeted and tested as potentially efficacious agents. For example, the serotonin reuptake inhibitor paroxetine (Paxil) has been evaluated as a treatment for both social anxiety disorder (SAD) and an alcohol use disorder when they occur concurrently.15 Paroxetine improved SAD as compared to placebo and, although alcohol quantity and frequency were not significantly changed, those participants randomized to paroxetine did have lower clinician global ratings of alcohol use severity.
This study was followed with a larger trial of longer duration replicating the finding that SAD was effectively reduced by the SSRI.16 Although the participants in the paroxetine group did not drink less than those in the placebo group, the authors reported that paroxetine reduced “reliance on alcohol to engage in social situations, and may change the reasons why one drinks (such that drinking occurs for other reasons besides coping with anxiety).”17 Although paroxetine did not decrease alcohol use, at least in this group of social anxiety treatment seekers, perhaps it made the therapeutic ground fertile for an additional alcohol intervention.
The SSRI sertraline (Zoloft) has also been evaluated in alcoholics with a comorbid anxiety disorder. Brady and colleagues18 randomized 94 people with alcohol dependence and comorbid PTSD to either sertraline 150 mg/day or placebo for 12 weeks. Although no overall medication effect was found on either symptoms of PTSD or on alcohol quantity and frequency, a post hoc cluster analysis revealed a subset of participants for whom sertraline decreased their drinking. The cluster for which sertraline was more effective than placebo at decreasing alcohol quantity and frequency consisted of those individuals who at baseline had less severe alcohol dependence, lower alcohol craving scores, and less alcohol consumption. In contrast, the cluster for which sertraline actually had worse alcohol outcomes than placebo included those individuals with more severe alcohol dependence and higher alcohol consumption at baseline.
Studies have also looked at the effect of medications on anxiety symptoms for individuals with substance use disorders. In a 12-week, double-blind, placebo-controlled trial of 61 alcohol-dependent individuals with high anxiety scores evaluating the efficacy of buspirone (BuSpar), the drug-treated group had greater retention in treatment and reduced anxiety, resulting in slower return to heavy drinking and fewer drinking days during the follow-up period.19
There are also several other agents that may prove fruitful in future studies. Topiramate (Topamax) has been shown to have promise in the treatment of alcohol dependence20,21 and has been considered as a treatment for cocaine dependence.22 In addition, it has some demonstrated efficacy in the treatment of anxiety disorders including PTSD,23 SAD,24 and OCD.25 Additionally, tiagabine (Gabitril), which has been shown to be helpful for anxiety disorders,26,27 has also been shown to have some efficacy at decreasing cocaine use, as shown in one study that measured urine drug screens of cocaine-dependent individuals with opiate dependence who are on methadone maintenance.28 However, another subsequent double-blind trial was not able to find efficacy of tiagabine over placebo at decreasing cocaine use.29 Although both of these GABA-ergic anticonvulsants have shown promise as treatments of anxiety disorders with comorbid substance use disorders, more work will need to be done to determine the details of their clinical usefulness.
Psychotherapy
The psychotherapies are also a critical component of the treatment of substance use disorders comorbid with anxiety disorders. However, traditional therapies, like those relying on the 12 steps, may be less palatable for some individuals with anxiety disorders. A recent study evaluating individuals with alcohol dependence entering 12-step treatment suggested that women with comorbid SAD had worse alcohol outcomes and worse scores on 12-step affiliation as compared to women without SAD.30 Cognitive-behavioral therapy (CBT), which has been shown to be effective for the treatment of substance dependence and for the treatment of anxiety disorders, may be a more successful platform on which to develop specialized treatments for individuals with both disorders.
Examples of treatments using CBT as a platform to treat comorbid anxiety and substance use disorders include a vulnerability-targeted CBT for smoking and PD comorbidity31 and concurrent treatment of PTSD and cocaine dependence.32 While there is some evidence that CBT-based treatments can be effective in this population,32 researchers have speculated that exposure, an active ingredient in traditional CBT for anxiety, may be compromised by the potentially avoidant properties of substance use.33
It is also possible that exposure-based treatments could hinder or worsen progress on substance abuse outcome goals. Randall and colleagues34 randomized 93 individuals with alcohol dependence with comorbid SAD to CBT for alcohol disorder with or without CBT for SAD concurrently. The authors hypothesized that better alcohol and anxiety outcomes would result from the additional treatment of the anxiety disorder. However, contrary to this hypothesis, both groups did equally well on anxiety outcomes and the group with the additional CBT for SAD actually had worse alcohol outcomes than the group receiving only CBT for alcohol dependence. The authors considered whether encouraging exposure to feared situations may have resulted in participants drinking more to cope with their anxiety, and the alcohol, in turn, may have interfered in the anxiety being extinguished by exposure.
Treatment considerations
Those studies that do evaluate treatments of anxiety disorders with comorbid substance use disorders bring important considerations to light. When an anxiety disorder and substance use disorder occur concurrently, should both disorders be treated simultaneously, either in an integrated treatment or in parallel, or should one disorder be addressed initially, and the other disorder treated subsequently? The answer to this is largely based on expert opinion rather than on experimental data. Stewart and Conrod6 suggested that consideration be given to the individual patient's readiness to change35 each presenting disorder. Specifically, if the patient is significantly more ready to change one of the disorders as compared to the other, they recommend starting treatment on the disorder that the patient is ready to address while simultaneously using motivational interviewing36 to improve readiness to change the concurrent problem.
The approach of treating both disorders when an anxiety disorder and substance use disorder co-occur makes intuitive sense and is consistent with the mutual maintenance pattern of dual disorders, and it has the support of expert opinion. Unfortunately very few studies have been done to validate the need for an integrated approach. Hien and colleagues37 compared the efficacy of a manualized integrated treatment of PTSD with comorbid substance use disorder to a manualized treatment aimed only at preventing relapse of the substance use disorder, largely ignoring symptoms of PTSD. The authors found that both treatments resulted in significant improvement in both PTSD symptoms and addiction severity. So, although it makes sense from a mechanistic perspective that both disorders should be addressed specifically in treatment, more studies will need to be done before clear treatment guidelines can be recommended. Until then, treatment approach to substance use disorders with comorbid anxiety disorders will be largely driven by expert opinion.
Summary and Conclusions
The current accumulated research and clinical focus on comorbid anxiety and substance use disorders has provided important insights into the prevalence, development and maintenance patterns, clinical impact, and treatment considerations for these intertwined psychiatric problems. However, further research is imperative to further spur the field toward solidifying the empirical foundations for state-of-the-art, standard clinical care. Additionally, future studies exploring the uniqueness of the associations between specific disorder pairings (e.g., comorbid SAD and alcohol dependence versus comorbid GAD and sedative dependence) are necessary to yield information on optimizing tailored treatments. Fortunately, research in these areas is ongoing and primed to advance psychiatric care for individuals experiencing comorbid anxiety and substance use disorders.
Acknowledgments
Supported by an educational grant from Forest Research Institute, Inc. a wholly-owned subsidiary of Forest Laboratories Inc.
References
- 1.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [see comments] Published erratum in. [DOI] [PubMed] [Google Scholar]; Arch Gen Psychiatry. 62(7):768. [Google Scholar]
- 2.Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. pp. 3–17. [Google Scholar]
- 3.Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. Am J Psychiatry. 1990;147(6):685–695. doi: 10.1176/ajp.147.6.685. comment. [DOI] [PubMed] [Google Scholar]
- 4.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 5.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 6.Stewart SH, Conrod PJ. Anxiety disorders and substance use disorders co-morbidity: common themes and future directions. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. pp. 239–257. [Google Scholar]
- 7.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 8.Driessen M, Meier S, Hill A, et al. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol. 2001;36(3):249–255. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- 9.Johnston AL, Thevos AK, Randall CL, Anton RF. Increased severity of alcohol withdrawal in in-patient alcoholics with a co-existing anxiety diagnosis. Br J Addict. 1991;86(6):719–725. doi: 10.1111/j.1360-0443.1991.tb03098.x. [DOI] [PubMed] [Google Scholar]
- 10.Sannibale C, Hall W. Gender-related symptoms and correlates of alcohol dependence among men and women with a lifetime diagnosis of alcohol use disorders. Drug Alcohol Rev. 2001;20(4):369–383. [Google Scholar]
- 11.Perkonigg A, Settele A, Pfister H, et al. Where have they been? Service use of regular substance users with and without abuse and dependence. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):470–479. doi: 10.1007/s00127-006-0044-4. [DOI] [PubMed] [Google Scholar]
- 12.Thomas SE, Thevos AK, Randall CL. Alcoholics with and without social phobia: a comparison of substance use and psychiatric variables. J Stud Alcohol. 1999;60(4):472–479. doi: 10.15288/jsa.1999.60.472. [DOI] [PubMed] [Google Scholar]
- 13.Bruce SE, Yonkers KA, Otto MW, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162(6):1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hornig CD, McNally RJ. Panic disorder and suicide attempt. A reanalysis of data from the Epidemiologic Catchment Area study. Br J Psychiatry. 1995;167(1):76–79. doi: 10.1192/bjp.167.1.76. [DOI] [PubMed] [Google Scholar]
- 15.Randall CL, Johnson MR, Thevos AK, et al. Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Depress Anxiety. 2001;14(4):255–262. doi: 10.1002/da.1077. [DOI] [PubMed] [Google Scholar]
- 16.Book SW, Thomas SE, Randall PK, Randall CL. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. J Anxiety Disord. 2008;22(2):310–318. doi: 10.1016/j.janxdis.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas SE, Randall PK, Book SW, Randall CL. A complex relationship between co-occurring social anxiety and alcohol use disorders: what effect does treating social anxiety have on drinking? Alcohol Clin Exp Res. 2008;32(1):77–84. doi: 10.1111/j.1530-0277.2007.00546.x. [DOI] [PubMed] [Google Scholar]
- 18.Brady KT, Sonne S, Anton RF, et al. Sertraline in the treatment of co-occurring alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res. 2005;29(3):395–401. doi: 10.1097/01.alc.0000156129.98265.57. [DOI] [PubMed] [Google Scholar]
- 19.Kranzler HR, Burleson JA, Del Boca FK, et al. Buspirone treatment of anxious alcoholics. A placebo-controlled trial. Arch Gen Psychiatry. 1994;51(9):720–731. doi: 10.1001/archpsyc.1994.03950090052008. [DOI] [PubMed] [Google Scholar]
- 20.Johnson BA, Ait-Daoud N, Bowden CL, et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet. 2003;361(9370):1677–1685. doi: 10.1016/S0140-6736(03)13370-3. see comments. [DOI] [PubMed] [Google Scholar]
- 21.Johnson BA, Rosenthal N, Capece JA, et al. Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298(14):1641–1651. doi: 10.1001/jama.298.14.1641. see comments. [DOI] [PubMed] [Google Scholar]
- 22.Johnson BA. Recent advances in the development of treatments for alcohol and cocaine dependence: focus on topiramate and other modulators of GABA or glutamate function. CNS Drugs. 2005;19(10):873–896. doi: 10.2165/00023210-200519100-00005. [DOI] [PubMed] [Google Scholar]
- 23.Tucker P, Trautman RP, Wyatt DB, et al. Efficacy and safety of topiramate monotherapy in civilian posttraumatic stress disorder: a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 68(2):201–206. doi: 10.4088/jcp.v68n0204. [DOI] [PubMed] [Google Scholar]
- 24.Van Ameringen M, Mancini C, Pipe B, et al. An open trial of topiramate in the treatment of generalized social phobia. J Clin Psychiatry. 2004;65(12):1674–1678. doi: 10.4088/jcp.v65n1213. [DOI] [PubMed] [Google Scholar]
- 25.Rubio G, Jimenez-Arriero MA, Martinez-Gras I, et al. The effects of topiramate adjunctive treatment added to antidepressants in patients with resistant obsessive-compulsive disorder. J Clin Psychopharmacol. 2006;26(3):341–344. doi: 10.1097/01.jcp.0000220524.44905.9f. letter. [DOI] [PubMed] [Google Scholar]
- 26.Dunlop BW, Papp L, Garlow SJ, et al. Tiagabine for social anxiety disorder. Hum Psychopharmacol. 2007;22(4):241–244. doi: 10.1002/hup.846. [DOI] [PubMed] [Google Scholar]
- 27.Mula M, Pini S, Cassano GB. The role of anticonvulsant drugs in anxiety disorders: a critical review of the evidence. J Clin Psychopharmacol. 2007;27(3):263–272. doi: 10.1097/jcp.0b013e318059361a. [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez G, Desai R, Sofuoglu M, et al. Clinical efficacy of gabapentin versus tiagabine for reducing cocaine use among cocaine dependent methadone-treated patients. Drug Alcohol Depend. 2007;87(1):1–9. doi: 10.1016/j.drugalcdep.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Winhusen T, Somoza E, Ciraulo DA, et al. A double-blind, placebo-controlled trial of tiagabine for the treatment of cocaine dependence. Drug Alcohol Depend. 2007;91(2-3):141–148. doi: 10.1016/j.drugalcdep.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 30.Pagano ME, Book SW, Onder CC, et al. Alcoholics seeking treatment: does co-occurring social anxiety disorder interfere with AA affiliation?. Poster presented at the 2008 RSA/ISBRA Joint Scientific Meeting; Washington, D.C.. June 28-July 2, 2008. [Google Scholar]
- 31.Zvolensky MJ, Bernstein A, Yartz AR, et al. Cognitive-behavioral treatment of co-morbid panic psychopathology and tobacco use and dependence. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. [Google Scholar]
- 32.Brady KT, Dansky BS, Back SE, et al. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: preliminary findings. J Subst Abuse Treat. 2001;21(1):47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 33.Riggs DS, Foa EB. Treatment for co-morbid posttraumatic stress disorder and substance use disorders. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. [Google Scholar]
- 34.Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: a first step toward developing effective treatments. Alcohol Clin Exp Res. 2001;25(2):210–220. [PubMed] [Google Scholar]
- 35.Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of Psychotherapy Integration. New York: Basic Books; 1992. pp. 300–334. [Google Scholar]
- 36.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- 37.Hien DA, Cohen LR, Miele GM, et al. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161(8):1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]