Abstract
Objective
The purpose of this study was to empirically derive eating disorder phenotypes in a clinical sample of children and adolescents using latent profile analysis (LPA) and compare these latent profile (LP) groups to the DSM-IV-TR eating disorder categories.
Method
Eating disorder symptom data collected from 401 youth (ages 7–19; mean 15.14 ± 2.35y) seeking eating disorder treatment were included in LPA; general linear models were used to compare LP groups to DSM-IV-TR eating disorder categories on pre-treatment and outcome indices.
Results
Three LP groups were identified: LP1 (n=144), characterized binge eating and purging (“Binge/purge”); LP2 (n=126), characterized by excessive exercise and extreme eating disorder cognitions (“Exercise-extreme cognitions”); and LP3 (n=131), characterized by minimal eating disorder behaviors and cognitions (“Minimal behaviors/cognitions”). Identified LPs imperfectly resembled DSM-IV-TR eating disorders. LP1 resembled bulimia nervosa; LP2 and LP3 broadly resembled anorexia nervosa with a relaxed weight criterion, differentiated by excessive exercise and severity of eating disorder cognitions. LP groups were more differentiated than the DSM-IV-TR categories across pre-treatment eating disorder and general psychopathology indices, as well as weight change at follow-up. Neither LP nor DSM-IV-TR categories predicted change in binge/purge behaviors. Validation analyses suggest these empirically-derived groups improve upon the current DSM-IV-TR categories.
Conclusions
In children and adolescents, revisions for DSM-V should consider recognition of patients with minimal cognitive eating disorder symptoms.
Key Terms: Eating disorders, diagnosis, classification, latent profile analysis
Introduction
The phenomenology of eating disorders in children and adolescents is understudied and poorly understood. The current classification system of eating disorders (Diagnostic and Statistical Manual of Mental Disorders [DSM-IV-TR])1 recognizes three diagnoses: anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (EDNOS). AN and BN are defined by specific physical, cognitive, and behavioral criteria; EDNOS is defined instead by eating disorder symptoms that do not meet full criteria for either AN or BN. The DSM-IV-TR does not make specific provisions for the diagnosis of eating disorders in children and adolescents. To inform DSM-V, research is needed to determine whether the same symptom clusters and diagnostic presentations observed in adults can be found in children and adolescents.
Indeed, limited empirical work has examined the appropriateness and applicability of the DSM-IV-TR categories to youth but it has been suggested that different diagnostic thresholds or categories may be needed for younger populations. The Workgroup for Classification of Eating Disorders in Children and Adolescents reviewed the literature relevant to nosology in children and adolescents, identifying potential problems with the diagnostic criteria as they are applied to youth.2–3 For example, growth and weight gain are expected in children and adolescents, which can challenge application of a strict weight criterion required for the AN diagnosis. Similarly, children and adolescents may be premenarcheal or have not yet established regular menstrual cycles, which makes the AN amenorrhea criterion irrelevant. Importantly, the cognitive eating disorder criteria – extreme fear of weight gain, body image disturbance, and overvaluation of weight and shape – are also difficult to assess and apply in younger patients who may have limited insight into their motives for eating disorder behaviors due in part to an underdeveloped capacity for abstract reasoning.4–5 Further, in both adults and youth alike, the twice weekly frequency criteria for binge eating and purging required for the diagnosis of BN is not empirically-based and may be too strict a threshold.6
Perhaps secondary to these challenges in applying the current eating disorder diagnoses to younger patients, descriptive clinical studies indicate that EDNOS is the most common eating disorder in clinical settings.7–10 This diagnosis is problematic due to its heterogeneity, rendering the amount of specific information conveyed by the EDNOS label to be minimal. This problem is not unique to youth – as EDNOS similarly predominates in adult clinical samples11 – but the reasons younger patients are assigned this diagnosis may be distinct as suggested by the Workgroup.2
Preliminary studies have suggested a lack of clinically meaningful differences between youth with AN and BN and those with EDNOS who narrowly miss criteria for either of the other two disorders. 7,9 These study findings support the Workgroup’s position that the current thresholds for AN and BN may be overly narrow and that relaxing the criteria would allow a subset of youth with EDNOS to be meaningfully reclassified within broadened forms of AN or BN. However, research from our group also demonstrated that a subset of youth with EDNOS did not resemble either AN or BN.7 Indeed, youth with eating problems may present with a distinct set of symptoms including selective or picky eating, for example, which are not currently included within DSM-IV-TR examples of EDNOS. 2 Taken together, the literature suggests that the current classification system of eating disorders may be inadequate for categorizing eating pathology in youth.
Empirical approaches can be used to investigate nosology. One such approach utilizes the statistical technique of latent class or latent profile analysis (LCA or LPA). LCA and LPA identify underlying (or latent) groups of individuals on the basis of their patterned responses across a set of eating disorder features.12 LPA has the advantage of allowing for the inclusion of continuous indicators while LCA is limited to categorical indicators. To date, this empirical classification research has been limited to adult samples,13–20 with the exception of one recent report combining adolescents and young adults.21 In adult samples, this research has demonstrated that LCA/LPA reliably identify clinically meaningful subgroups of individuals with eating disorders including those that resemble AN, BN, and one particular type of EDNOS characterized by binge eating without purging (binge eating disorder [BED]).13,15–16,18 However, the resemblance is imperfect and subthreshold presentations cluster with similar full syndrome disorders.13,16,18
As developmental differences between children, adolescents, and adults may result in unique sets of challenges related to the fit of the DSM-IV-TR eating disorders criteria,2–3,7 empirical studies are needed to characterize the full range of individuals who seek treatment for eating disorders. While it is possible that similar eating disorder phenotypes will be identified in younger samples as have been identified in adults, unique child or adolescent phenotypes may emerge. Because the onset of eating disorders most often occurs in adolescence, failure to characterize younger patients with eating disorders (and to examine them separately from adults) is problematic.
Given that the diagnostic classification system plays a critical role in guiding clinical practice and research, ensuring that this system accurately organizes and includes the full range of psychopathology in individuals of all ages is imperative. This study was designed to examine diagnostic classification in children and adolescents using an empirical approach that has been useful in nosological studies of adult samples. Specifically, we sought (1) to determine whether an empirical classification system of eating disorders in adolescents could be derived using LPA, (2) to examine the concordance of latent profile (LP) group membership with DSM-IV-TR eating disorder diagnoses, and (3) to compare the validity of the two classification systems across cross-sectional and outcome indices. On the basis of the descriptive child and adolescent literature and the adult LCA/LPA studies, we hypothesized that LPA would successfully identify eating disorder phenotypes in youth and that these would resemble the DSM-IV-TR diagnoses imperfectly.
Method
Participants
Data were collected from 401 consecutive children and adolescents evaluated through the Eating Disorders Program at the University of Chicago Medical Center between October 2001 and April 2009. The Eating Disorders Program is a specialist outpatient treatment setting at a tertiary medical institution. Three hundred and sixty-three girls (90.5%) and 38 boys (9.5%) participated. The mean age of participants was 15.14 ± 2.35 years. The majority (73.9%) were Caucasian, 12.4% were Hispanic, 8.9% were Black, and 2.0% were Asian; 2.8% identified as another race/ethnicity.
Follow-up data were available for a subset of these participants who had completed >3 months of treatment (n=229; 57.1%). The mean duration elapsed between pre-treatment and follow-up was 11.19 ± 5.59 months.
Procedure
This study was approved by the Institutional Review Board at The University of Chicago Medical Center. Data were collected at baseline, prior to the initiation of treatment, as well as at the end of treatment or the last available follow-up point for a subset. Each child/adolescent gave written assent, and a parent/guardian gave written consent for protocol participation. Fewer than 10% of youth presenting for treatment during this time period did not consent/assent to have their data included in this research database; non-participants did not differ from participants with regard to demographics.
Measures
Intake (Pre-treatment)
Eating Disorder Examination (EDE) version 12.0D/C.2 or version adapted for children.22–23
Both the adult and child versions of the EDE assess eating-related behaviors and cognitions to diagnose specific DSM-IV-TR eating disorders and yield four dimensional scales: dietary restraint, eating concern, shape concern, and weight concern; a global scale is calculated as the average of the four scales. For each of the scales, scores range from 0 to 6, with higher scores indicating increased eating disorder pathology. The presence and frequency of specific eating and compensatory behaviors during the three months before the assessment are collected, including objective binge eating, subjective binge eating (collected only one month before the assessment), self-induced vomiting, misuse of laxatives or diuretics, excessive exercising, and fasting. The EDE has shown excellent reliability and validity,22,24 and studies indicate that the child interview also demonstrates good reliability and validity.23,25–26 Interviewers were trained in the administration of both the adult and child versions of the interview – which capture the same sets of symptoms – and were able to use the more simple language in the child version to ensure comprehension by children and younger adolescents.
DSM-IV-TR diagnoses of AN and BN were assigned based on EDE-generated behavioral and cognitive symptoms. Eating disorder presentations that did not meet DSM-IV-TR criteria for AN or BN were categorized as EDNOS. Due to its heterogeneity, we divided EDNOS into clinically meaningful categories of subthreshold AN, subthreshold BN, BED, and purge disorder, along with an EDNOS “other” category that included individuals who could not be classified elsewhere.7
Beck Depression Inventory.(BDI).27
The BDI is a self-report measure of depressive symptoms; scores range from 0 to 63; 10 to 18 suggests mild/moderate depressive symptoms and >18 indicates moderate/severe depressive symptoms. This measure is widely used and has demonstrated good psychometric properties and strong associations with clinical depression; it has recently been used in two randomized, controlled clinical trials of adolescent AN28 and BN.29
Rosenberg Self-Esteem Scale (RSE).30
The RSE is a self-report measure of overall self-esteem; scores range from 0 to 30; scores <15 suggest low self-esteem. This measure has demonstrated adequate reliability and validity in adolescents.31
Follow-up
Self-reported frequency of objective binge eating and purging (by self-induced vomiting, misuse of laxatives or diuretics) during the past four weeks was ascertained.
Physical Assessment. At both pre-treatment and follow-up, participants were weighed on a calibrated digital or balance-beam scale in light indoor clothing; height was obtained using a calibrated stadiometer.
Statistical Analysis
Latent Profile Analysis
Four hundred and one cases were included in the LPA.32 The analyses were also run excluding male participants and the results were unchanged. LPA posits that a heterogeneous group can be broken down to a finite number of homogeneous subgroups through minimizing associations among responses across multiple indicators. In doing so, LPA identifies the number and composition of unobserved latent groups, which themselves are mutually exclusive. The number of LPs was determined by three information criterion indices: the Bayesian information criteria (BIC) parsimony index,33 the sample-size adjusted BIC (aBIC),34 and the Consistent Akaike information criterion (cAIC), which was suggested by Bozdogman.35 The BIC expresses model fit as a function of log-likelihood, sample size, and number of model parameters. The cAIC is derived from the Akaike information criterion,36 which determines model fit on the basis of log-likelihood of the model and number of estimated parameters; the advantage of using the cAIC is that it includes a penalty for models having larger numbers of parameters. The BIC, the aBIC, and the cAIC were used for comparing plausible models, where the lowest value of a given index indicates the best fitting model.
Analysis was performed using Latent Gold version 4.5 software.37 Eight indicators of eating disorder pathology were selected from the EDE to represent the DSM-IV-TR eating disorder criteria sets for AN and BN. Indicators included percent ideal body weight (%IBW [defined as current BMI/50th centile BMI for age and gender using Centers for Disease Control and Prevention growth charts: http://www.cdc.gov/growthcharts/percentile_data_files.htm]38) (≤85% IBW; >85% IBW and <95% IBW; ≥95% IBW and <105% IBW; ≥105% IBW); objective binge eating episodes, subjective binge eating episodes, self-induced vomiting, laxative or diuretic abuse (combined as a summary variable due to their non-independence), excessive exercising, (all rated in clinically relevant ordered categories: never or <1x/month; 1-7x/month; ≥8x/month); fear of weight gain, weight and shape overvaluation (both rated: not at all or slightly; moderately; very much or extremely). Missing values were estimated with full information maximum-likelihood estimation.
Validation Analyses
Cross-sectional validators included the EDE scales, depressive symptoms measured by the BDI, and self-esteem measured by the RSE. Outcome variables relevant to eating disorders were measured as %IBW, binge frequency, and purge frequency at follow-up. Validation analyses were run using general linear models for cross-sectional and outcome indices; age and gender were controlled in all analyses. Note that for the outcome variables, only participants for whom the variable was relevant were included (i.e., for %IBW only those who were <95% at intake were included; for binge eating only those who reported objective binge eating >1x/month at intake were included; and for purging only those who reported purging >1x/month at intake were included). For outcome analyses, both relevant pre-treatment variables (e.g., %IBW, binge frequency, purge frequency) and duration of treatment were additionally included as covariates. Post-hoc comparisons were made using Bonferroni-corrected significance levels (i.e., for each of the 10 validators we made 3 between-group comparisons and significance levels were adjusted to reflect multiple comparisons). Direct comparisons of the LPs to the DSM-IV-TR diagnoses were made based on the size of partial eta-squared (η2), representing the unique portion of variance in the dependent variable accounted for by group membership (i.e., DSM-IV-TR or LP). All validation analyses were conducted using SPSS version 17.0.
Results
Latent Profile Analysis
LPA models varying the number of latent profiles from 1–7 were evaluated. Fit indices were lowest for a 3-profile solution (χ2[362]=11171.17, p>.99) with 39 parameters, indicating that a 3-profile solution was the best-fitting model (see Table 1). Of the total sample, 144 (35.9%) were members of LP1, 126 (31.4%) members of LP2, and 131 (32.7%) members of LP3. Table 2 presents the frequency and severity of the indicators by LP.
Table 1.
Fit indices for Latent Profile Analysis
| Classes | Parameters | BIC | aBIC | cAIC | LL |
|---|---|---|---|---|---|
| 1 | 17 | 5618.65 | 5564.70 | 5635.65 | −2758.37 |
| 2 | 28 | 5300.49 | 5211.64 | 5328.49 | −2566.33 |
| 3 | 39 | 5246.79 | 5123.03 | 5285.79 | −2506.51 |
| 4 | 50 | 5282.46 | 5123.80 | 5332.46 | −2491.38 |
| 5 | 61 | 5325.62 | 5216.70 | 5386.62 | −2480.00 |
| 6 | 72 | 5366.59 | 5138.12 | 5438.59 | −2467.51 |
| 7 | 83 | 5411.34 | 5147.97 | 5484.34 | −2456.92 |
Note: BIC = Bayesian information criteria (BIC) parsimony index; aBIC = sample-size adjusted BIC; cAIC = consistent Akaike information criterion; LL = log likelihood. Lower BIC, aBIC, and cAIC indicate better model fit.
Table 2.
Frequency of eating disorder pathology in latent profiles
| LP1 (n=144) | LP2 (n=126) | LP3 (n=131) | ||
|---|---|---|---|---|
| % Ideal Body Weight | < 86% | 1.6% | 36.5% | 47.7% |
| ≥ 86% and < 95% | 20.7% | 27.3% | 20.1% | |
| ≥ 95% and < 105% | 22.3% | 21.4% | 8.7% | |
| ≥ 105% | 55.32% | 14.7% | 23.5% | |
| OBEs | 0 (<1x/month) | 22.6% | 91.4% | 93.9% |
| 1 (1-7x/month) | 35.0% | 8.1% | 5.8% | |
| 2 (≥ 8x/month) | 42.4% | 0% | 0% | |
| SBEs | 0 (<1x/month) | 41.4% | 61.2% | 80.3% |
| 1 (1-7x/month) | 23.6% | 20.6% | 13.6% | |
| 2 (≥ 8x/month) | 35.0% | 18.2% | 6.1% | |
| Vomiting | 0 (<1x/month) | 13.9% | 78.7% | 85.6% |
| 1 (1-7x/month) | 16.3% | 12.7% | 9.7% | |
| 2 (≥ 8x/month) | 70.8% | 8.6% | 4.7% | |
| Laxatives/Diuretics | 0 (<1x/month) | 80.2% | 89.7% | 100% |
| 1 (1-7x/month) | 12.4% | 7.7% | 0% | |
| 2 (≥ 8x/month) | 7.5% | 2.6% | 0% | |
| Exercise | 0 (<1x/month) | 46.7% | 24.3% | 87.2% |
| 1 (1-7x/month) | 19.1% | 17.9% | 8.9% | |
| 2 (≥ 8x/month) | 34.2% | 57.8% | 3.9% | |
| Fear | 0 (none/slight) | 12.6% | 15.0% | 86.0% |
| 1 (moderate) | 15.9% | 16.9% | 9.9% | |
| 2 (severe) | 71.5% | 68.2% | 4.1% | |
| Shape/Weight | 0 (none/slight) | 2.6% | 3.3% | 57.3% |
| Concerns | 1 (moderate) | 11.9% | 13.1% | 25.2% |
| 2 (severe) | 85.5% | 83.6% | 17.5% |
Note: BMI=body mass index; OBEs=objective binge episodes; SBEs=subjective binge episodes; LP1 = latent profile group 1; LP2 = latent profile group 2; LP3 = latent profile group 3
LP1 resembled BN, wherein patients were mostly in the healthy weight range and endorsed objective binge eating, purging by self-induced vomiting, and high levels of eating disorder cognitions; we labeled LP1, “Binge/purge.” In contrast, LP2 and LP3 were both characterized by low frequencies of objective binge eating and purge behaviors. LP2 was low to normal weight and endorsed excessive exercise and extreme eating disorder cognitions while LP3 included individuals of all weights who generally endorsed minimal eating disorder behaviors and cognitions. Accordingly, we labeled LP2, “Exercise-extreme cognitions,” and LP3, “Minimal behaviors/cognitions.”
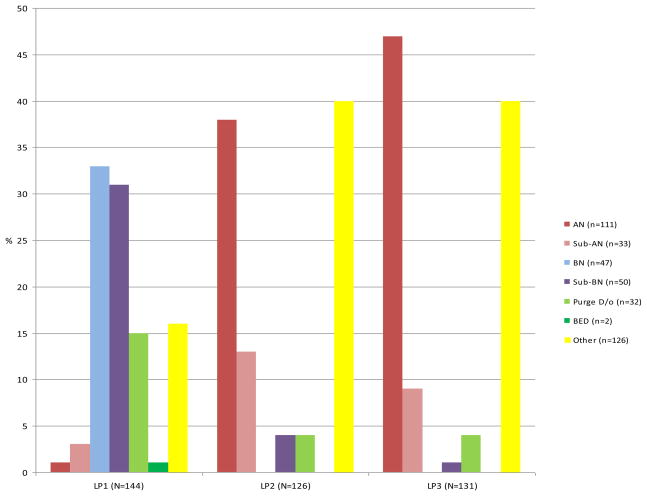
Figure 1 demonstrates the distribution of the DSM-IV-TR diagnoses by LPs. Chi-square analyses indicated an association between eating disorder diagnosis and LP (χ2[12]=246.36, p<.001). Notably, 100% of those with BN and BED along with the majority of those with EDNOS characterized by binge eating and/or purging (subthreshold BN, purge disorder) were included in LP1. The diagnostic breakdowns for LP2 and LP3 were similar to one another with each including nearly half of those with AN or subthreshold AN, and nearly half of those with EDNOS “other”.
Figure 1.
Distribution of DSM-IV diagnoses across latent profile groups (Latent Profile 1= “Binge/purge”, Latent Profile 2= “Exercise-extreme cognitions”, and Latent Profile 3= “Minimal behaviors/cognitions”)
Note: AN=Anorexia nervosa, Sub-AN=Subthreshold anorexia nervosa, BN=Bulimia nervosa, Sub-BN=Subthreshold bulimia nervosa, Purge D/o=Purging disorder, BED=Binge eating disorder, Other=Eating disorder not otherwise specified, Other type
Note: Percent of individuals with a given diagnosis within each LP group.
Validation Analyses
LPs differed in age (F[2, 398]=20.0, p<.001), gender (χ2[2]=6.46, p=.04), and current %IBW (F[2, 394]=15.82, p<.001). Post-hoc contrasts indicated that compared to LP2 and LP3, LP1 was older (16.10 ± 1.80 years, versus 14.82 ± 2.17 years in LP2 and 14.44 ± 2.72 in LP3). All three groups differed in %IBW (111.31 ± 21.17% in LP1; 91.35 ± 15.19% in LP2; 102.44 ± 42.98% in LP3). While all groups were within a healthy weight range on average, individuals who were below the 5th centile for age/gender (representing 20.2% of the entire sample) were more likely to be included in LP2 and LP3 (representing 28.0% and 33.1% of LP2 and LP3, respectively) than LP1 (1.4% of LP1). Those who were overweight (≥95th centile for age/gender; 5.5% of the entire sample) or at risk for overweight (≥85th centile and <95th centile for age/gender; 7.1% of the entire sample) were represented across all groups but least likely in LP2 (1.6% overweight, 1.6% at risk for overweight) compared to LP1 (4.9% overweight, 12.6% at risk for overweight) and LP3 (10.0% overweight, 6.2% at risk for overweight). While females predominated across groups, males were most likely to be classified in LP3, comprising 13.7% of LP3, compared to 10.3% in LP2 and only 4.9% in LP1.
Pre-treatment
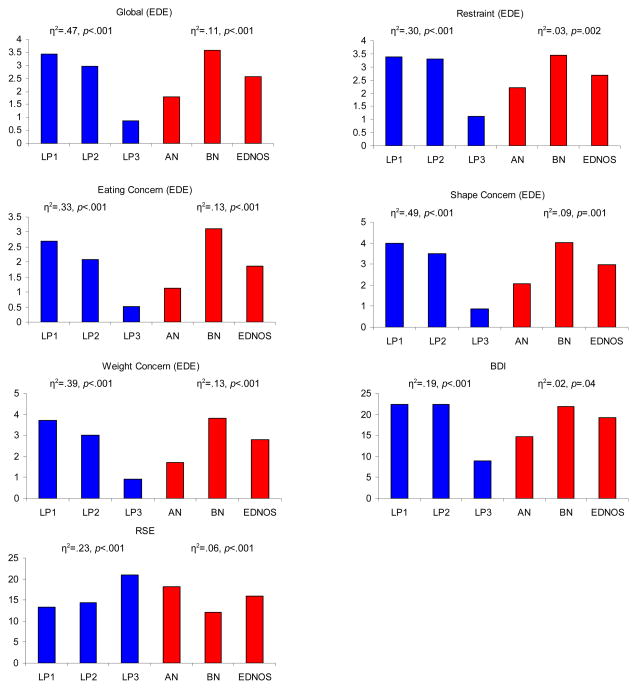
General linear models demonstrated that both the identified LP groups and the DSM-IV-TR groups were differentiated on all pre-treatment validators including eating disorder psychopathology measured by the EDE scores, depressive symptoms, and self-esteem (Figure 2). Across the EDE scales, BDI, and RSE, the LP groups were more differentiated than the DSM-IV-TR groups. Among the LP groups, LP3 reported less severe or fewer symptoms compared to LP1 and LP2 (all ps<.01). LP1 reported significantly greater pathology than LP2 on EDE Eating Concern, Weight Concern, and Global score.
Figure 2.
Validation analyses comparing latent profile groups (denoted in blue) to DSM-IV-TR diagnoses (denoted in red) on pre-treatment assessments
Note: LP=Latent profile, AN=Anorexia nervosa, BN=Bulimia nervosa, EDNOS=Eating disorder not otherwise specified, EDE=Eating Disorder Examination, RSE=Rosenberg Self Esteem Scale, BDI=Beck Depression Inventory
Follow-up
General linear models indicated that the LP groups were differentiated on %IBW at follow-up (controlling for pre-treatment %IBW, duration of treatment, age, and gender) (η2=0.068, F=4.29, df=123, p=.016). Compared to LP2, LP3 gained less weight between pre-treatment and follow-up and was less likely to be in a healthy weight range at follow-up (p<.01); LP1 did not differ significantly from either group. DSM-IV-TR diagnoses were not differentiated on %IBW at follow-up. Neither the LP groups nor the DSM-IV-TR categories were differentiated on binge eating or purging at follow-up.
Discussion
LPA identified three groups of children and adolescents presenting for treatment through a specialty eating disorders clinic. We labeled these groups, “Binge/purge,” “Exercise-extreme cognitions,” and “Minimal behaviors/cognitions.” These empirically derived groups bore resemblance to the DSM-IV-TR categories – as well as to latent groups identified in the adult eating disorders literature – yet important differences emerged.
The largest group identified (“Binge/purge”) resembled BN: all youth with BN were included in this group, along with the majority of those with EDNOS characterized by bingeing and/or purging. This empirical work suggested that these EDNOS types including subthreshold BN, purge disorder, and BED can be grouped together with BN. Both of the remaining LP groups resembled AN in terms of their inclusion of low weight individuals, however, neither group included predominantly low weight individuals. Further, only the “Exercise-extreme” group was characterized by the hallmark fear of weight gain that defines DSM-IV-TR AN, while the “Minimal behaviors/cognitions” group, instead, was marked by a relative absence of the cognitive eating disorder symptoms. These latter two latent groups were further differentiated from one another by the presence of excessive exercise, endorsed by three-quarters of those in the group with the characteristic eating disorder cognitions, compared to a small minority in the minimal cognitions group. Similar to the way in which full syndrome BN clustered with similar EDNOS presentations, individuals with AN and subthreshold AN clustered together and were likely to be included in one of these two latent groups. These findings are consistent with the descriptive child and adolescent literature that suggests few differences between full syndrome AN or BN and similar EDNOS presentations,7,9 which may support the notion of relaxing the current thresholds for AN and BN in youth.2
It is noteworthy, however, that in contrast to those with BN and similar EDNOS variants who were organized into a single latent group, those youth with AN and EDNOS resembling AN were organized into two groups. DSM-IV-TR distinguishes two types of individuals with AN on the basis of binge/purge symptoms. In this sample, two groups that included low weight individuals emerged but were, instead, distinguished by severity of eating disorder related cognitions and excessive exercise. Further, in addition to including AN and subthreshold AN, these two latent groups included individuals in a truly residual EDNOS “other” diagnosis, which could not be described as any of the other EDNOS types.
The three LP groups were differentiated in clinically meaningful ways at treatment presentation. Consistent with the descriptive literature, youth in the “Binge/purge” group tended to be older and were less likely to be in the low weight range compared to the other two groups. Interestingly, while there were a minority of boys in this sample, they were relatively more common in the group with the fewest typical eating disorder symptoms (“Minimal behaviors/cognitions”). This finding raises the possibility that boys with eating disorders may be more likely to exhibit atypical presentations than girls. Significant eating disorder pathology, depressive symptoms, and problems with self-esteem were evident in the “Binge/purge” and the “Exercise-extreme cognitions” latent groups. In contrast, the “Minimal behaviors/cognitions” group endorsed little eating disorder or general psychopathology. A striking finding was that across these clinical indices at treatment presentation, the empirically-derived groups were more differentiated than the DSM-IV-TR groups, suggesting that these empirical groupings may have more clinical utility. In individuals with eating disorders it is clinically useful to note the presence of symptoms such as binge eating, purging, and low weight; these findings suggest that in youth, it may also be particularly meaningful to note the presence of cognitive symptoms and excessive exercise.
In this sample, we examined a subset of youth for whom pre-treatment and follow-up data were available. Providing further support for the validity of the identified groups, outcome analyses demonstrated that low weight youth in the “Minimal behaviors/cognitions” group gained less weight at follow-up compared to low weight youth in either of the other two groups. Latent profile group membership – but not DSM-IV-TR diagnosis – was associated with change in %IBW at follow-up. While individuals with low weight eating disorders are – by definition – resistant to weight gain, these low weight youth with minimal eating disorder cognitions and non-depressed mood may be particularly reluctant to gain weight as they deny or minimize their experience of psychopathology/distress.
Our identified LP groups were somewhat similar to those reliably found in the adult literature. However, rather than identifying several different bulimic spectrum latent groups (e.g., BN-like, purge disorder, BED-like), we found that youth with a predominance of any of these symptoms (binge eating and/or purging) clustered in a single latent group. The separation of our groups containing low weight patients into two non-binge eating or purging latent groups is consistent with some of the adult findings.15–16 Two of the adult studies identified latent groups resembling AN that were distinguished by level of psychopathology, 15–16 with one of these being a group that endorsed low levels of both eating disorder cognitions as well as depression and anxiety, but at the same time reporting treatment-seeking and medical concerns at levels that were comparable to the other latent groups. 15
Yet, even if the groups identified in this youth sample resemble those empirically-derived in adults, they may not be the same. In youth, in particular, it can be difficult to parse out denial from inability to comprehend. It is possible that the “Minimal behaviors/cognitions” group is heterogeneous including youth who have minimal psychopathology or who lack the developmental capacity to endorse psychopathology, along with youth who deny or minimize their symptoms for other reasons.39 More sensitive assessment tools are needed to parse out denial/minimization, limited insight due to cognitive development, and absence of symptoms. One such recommendation is the collection of collateral reports, particularly by parents. Preliminary reports suggest that the addition of a parent-report component to the EDE can be clinically useful in addressing minimization of eating disorder psychopathology in youth. 40 Further, given the preliminary findings herein that these youth may gain less weight during treatment, increased attention to understanding and describing this group is needed.
Study strengths include the application of LPA to investigate nosology in a child and adolescent clinical sample of girls and boys with the full range of eating disorders. To our knowledge, no published studies have utilized this statistical method in a child and adolescent eating disorders sample. Further, this is the first LPA study to include longitudinal data, allowing for the consideration of the predictive validity of identified phenotypes. However, important limitations warrant acknowledgement. First, the identified eating disorder phenotypes were defined by the indicators of eating disorder pathology included in the analyses. The measurement of eating disorder symptoms (e.g., delineation of weight status, cognitive criteria) is challenging in youth. Although a study strength was the assessment of eating disorder pathology through a gold standard clinical interview, it is possible that this measure did not assess the full range of clinical signs and symptoms of eating disorder pathology specific to youth. It is possible that different subtypes of youth with eating disorders would have been identified if other types of indicators (e.g., picky/selective eating, taste/tactile sensitivities) had been included. Second, this study included a limited range of pre-treatment and follow-up clinical validators, and outcome data were not available for all youth. Third, this sample included treatment-seeking youth collected through a single clinical site, which may limit external validity of findings. Finally, while LPA identified the optimal number and composition of classes, it does not address whether the relationship between classes was taxonic versus dimensional.12 It is possible that some of the identified groups (e.g., LP2 and LP3) differ along a continuum rather than existing as distinct categories. Taxometric analyses would address this question and may be an approach utilized in future research.41–42
This study suggests that LPA can be used to identify meaningful eating disorder phenotypes in a clinical sample of children and adolescents. Youth who regularly engage in binge eating and/or purging are distinguished from those who do not; those who do not are more likely to be low weight and are organized into two groups distinguished by the presence of typical eating disorder cognitions and excessive exercise. These empirically-derived groups demonstrate both concurrent and predictive validity, supporting their candidacy as clinically meaningful groups. Our findings are consistent with the recommendations of the Workgroup for Classification of Eating Disorders in Children and Adolescents in which there is a focus on the need for diagnostic criteria to recognize that symptom expression – both cognitive and behavioral – may differ on the basis of development, and that comprehensive eating disorder assessment and diagnosis should include collateral (e.g., parent) report.2–3 Further, the empirical groupings of full syndrome AN or BN with similar EDNOS presentations is consistent with the Workgroup’s recommendations that strict thresholds be relaxed.2–3 Ongoing research focused on the nosology of eating disorders in children and adolescents utilizing developmentally-sensitive assessment tools and a broad range of clinical indicators and both cross-sectional and treatment outcome validators is needed to replicate and extend these findings in preparation for DSM-V.
Acknowledgments
Support for this research was provided by grants to the first author through NIMH (F32MH084396), Harvard Medical School (Livingston Fellowship Award), and the Harris Center at Massachusetts General Hospital.
The authors wish to acknowledge Leanna Delhey for her assistance with data compilation and entry.
Footnotes
This work was presented at the Conference on the Classification and Diagnosis of Eating Disorders, Washington DC, March 2009 (NIMH R13MH081447 [Wonderlich]) and at the Eating Disorders Research Society Meeting, Brooklyn, NY, September 2009.
Disclosure: The authors report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington: American Psychiatric Association Press; 2000. [Google Scholar]
- 2.Bravender T, Bryant-Waugh R, Herzog D, et al. Classification of child and adolescent eating disturbances. Workgroup for Classification of Eating Disorders in Children and Adolescents (WCEDCA) Int J Eat Disord. 2007;40:S117–S122. doi: 10.1002/eat.20458. [DOI] [PubMed] [Google Scholar]
- 3.Bravender T, Bryant-Waugh R, Herzog D, et al. Classification of eating disturbance in children and adolescents: Proposed changes for the DSM-V. Workgroup for Classification of Eating Disorders in Children and Adolescents (WCEDCA); 2009. Unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosso IM, Young AD, Femia LA, Yurgelun-Todd DA. Cognitive and emotional components of frontal lobe functioning in childhood and adolescence. Ann N Y Acad Sci. 2004;1021:355–362. doi: 10.1196/annals.1308.045. [DOI] [PubMed] [Google Scholar]
- 5.Yurgelun-Todd D. Emotional and cognitive changes during adolescence. Curr Opin Neurobiol. 2007;17:251–257. doi: 10.1016/j.conb.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Thomas JJ, Vartanian LR, Brownell KD. The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: Meta-analysis and implications for DSM-V. Psychol Bull. 2009;135:407–433. doi: 10.1037/a0015326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eddy KT, Celio Doyle A, Hoste RR, Herzog DB, Le Grange D. Eating disorder not otherwise specified (EDNOS): An examination of EDNOS presentations in adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47:156–164. doi: 10.1097/chi.0b013e31815cd9cf. [DOI] [PubMed] [Google Scholar]
- 8.Nicholls D, Chater R, Lask B. Children into DSM don’t go: a comparison of classification systems for eating disorders in childhood and early adolescence. Int J Eat Disord. 2000;28:317–324. doi: 10.1002/1098-108x(200011)28:3<317::aid-eat9>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 9.Peebles R, Wilson JL, Lock JD. How do children with eating disorders differ from adolescents with eating disorders at initial evaluation? J Adolesc Health. 2006;39:800–805. doi: 10.1016/j.jadohealth.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Turner H, Bryant-Waugh R. Eating disorder not otherwise specified (EDNOS): Profiles of clients presenting at a community eating disorders service. Eur Eat Disord Rev. 2004;12:18–26. [Google Scholar]
- 11.Fairburn CG, Cooper Z, Bohn K, O’Connor ME, Doll HA, Palmer RL. The severity and status of eating disorder NOS: Implications for DSM-V. Behav Res Ther. 2007;45:1705–1715. doi: 10.1016/j.brat.2007.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wonderlich SA, Joiner TE, Keel PK, Williamson DA, Crosby RD. Eating disorder diagnoses: Empirical approaches to classification. Am Psychol. 2007;62:167–180. doi: 10.1037/0003-066X.62.3.167. [DOI] [PubMed] [Google Scholar]
- 13.Bulik CM, Sullivan PF, Kendler KS. An empirical study of the classification of eating disorders. Am J Psychiatry. 2000;157:886–895. doi: 10.1176/appi.ajp.157.6.886. [DOI] [PubMed] [Google Scholar]
- 14.Duncan AE, Bucholz KK, Neuman RJ, Agrawal A, Madden PAF, Heath AC. Clustering of eating disorder symptoms in a general population female twin sample: A latent class analysis. Psychol Med. 2007;37:1097–1107. doi: 10.1017/S0033291707000505. [DOI] [PubMed] [Google Scholar]
- 15.Eddy KT, Crosby RD, Keel PK, et al. Empirical identification and validation of eating disorder phenotypes in a multisite clinical sample. J Nerv Ment Dis. 2009;197:41–49. doi: 10.1097/NMD.0b013e3181927389. [DOI] [PubMed] [Google Scholar]
- 16.Keel PK, Fichter M, Quadflieg N, et al. Application of a latent class analysis to empirically define eating disorder phenotypes. Arch Gen Psychiatry. 2004;61:192–200. doi: 10.1001/archpsyc.61.2.192. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell JE, Crosby RD, Wonderlich SA, et al. Latent profile analysis of a cohort of patients with eating disorder not otherwise specified. Int J Eat Disord. 2007;40:S95–S98. doi: 10.1002/eat.20459. [DOI] [PubMed] [Google Scholar]
- 18.Striegel-Moore RH, Franko DL, Thompson D, Barton B, Schreiber GB, Daniels SR. An empirical study of the typology of bulimia nervosa and its spectrum variants. Psychol Med. 2005;35:1563–1572. doi: 10.1017/S0033291705006057. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan PF, Bulik CM, Kendler KS. The epidemiology and classification of bulimia nervosa. Psychol Med. 1998;28:599–610. doi: 10.1017/s0033291798006576. [DOI] [PubMed] [Google Scholar]
- 20.Wade TD, Crosby RD, Martin NG. Use of latent profile analysis to identify eating disorder phenotypes in an adult Australian twin cohort. Arch Gen Psychiatry. 2006;63:1377–1384. doi: 10.1001/archpsyc.63.12.1377. [DOI] [PubMed] [Google Scholar]
- 21.Pinheiro AP, Bulik CM, Sullivan PF, Machado PP. An empirical study of the typology of bulimic symptoms in young Portuguese women. Int J Eat Disord. 2008;41:251–258. doi: 10.1002/eat.20497. [DOI] [PubMed] [Google Scholar]
- 22.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, assessment and treatment. 12. New York: Guilford Press; 1993. pp. 333–360. [Google Scholar]
- 23.Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the Eating Disorder Examination with children: A pilot investigation. Int J Eat Disord. 1996;19:391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 24.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 25.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal weight children. J Consult Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watkins B, Frampton I, Lask B, Bryant-Waugh R. Reliability and validity of the child version of the Eating Disorder Examination: A preliminary investigation. Int J Eat Disord. 2005;38:183–197. doi: 10.1002/eat.20165. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT. Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- 28.Lock J, Agras WS, Bryson S, Kraemer H. A comparison of short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2005;44:632–639. doi: 10.1097/01.chi.0000161647.82775.0a. [DOI] [PubMed] [Google Scholar]
- 29.Le Grange D, Crosby RD, Rathouz PJ, Leventhal BL. A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch Gen Psychiatry. 2007;64:1049–1056. doi: 10.1001/archpsyc.64.9.1049. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 31.Hagborg WJ. Scores of middle-school-age students on the Rosenberg Self-Esteem Scale. Psychological Reports. 1996;78:1071–1074. [Google Scholar]
- 32.Lazarsfeld PF, Henry NW. Latent structure analysis. Boston: Houghton Mifflin; 1968. [Google Scholar]
- 33.Sclove S. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 34.Croudace TJ, Jarvelin M-R, Wadsworth MEJ, Jones PB. Developmental typology of trajectories to nighttime bladder control: Epidemiologic application of longitudinal latent class analysis. Am J Epidem. 2003;157:834–842. doi: 10.1093/aje/kwg049. [DOI] [PubMed] [Google Scholar]
- 35.Bozdogman H. Model selection and Akaike’s information criterion: The general theory and its analytical extensions. Psychometrika. 1987;52:345–370. [Google Scholar]
- 36.Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- 37.Vermunt JK, Magidson J. Latent GOLD User’s Guide. Belmont: Statistical Innovations Inc; 2000. [Google Scholar]
- 38.Center for Disease Control. CDC Growth Charts for the United States: Development and Methods. Center for Disease Control; 2002. [Google Scholar]
- 39.Becker AE, Eddy KT, Perloe A. Clarifying criteria for cognitive signs and symptoms for eating disorders in DSM-V. Int J Eat Disord. 2009;42:611–619. doi: 10.1002/eat.20723. [DOI] [PubMed] [Google Scholar]
- 40.Couturier J, Lock J, Forsberg S, Vanderheyden D, Yen HL. The addition of a parent and clinician component to the EDE for children and adolescents. Int J Eat Disord. 2006;40:472–475. doi: 10.1002/eat.20379. [DOI] [PubMed] [Google Scholar]
- 41.Beauchaine TP. Taxometrics and developmental psychopathology. Dev Psychopathol. 2003;15:501–527. doi: 10.1017/s0954579403000270. [DOI] [PubMed] [Google Scholar]
- 42.Meehl P. Bootstraps taxometrics: Solving the classification problem in psychopathology. Am Psychol. 1995;50:266–275. doi: 10.1037//0003-066x.50.4.266. [DOI] [PubMed] [Google Scholar]