Abstract
When using the laryngeal tube and the intubating laryngeal mask airway (ILMA), the medium-size (maximum volume 1100 ml) versus adult (maximum volume 1500 ml) self-inflating bags resulted in significantly lower lung tidal volumes. No gastric inflation occurred when using both devices with either ventilation bag. The newly developed medium-size self-inflating bag may be an option to further reduce the risk of gastric inflation while maintaining sufficient lung ventilation. Both the ILMA and laryngeal tube proved to be valid alternatives for emergency airway management in the experimental model used.
Keywords: emergency airway management, gastric regurgitation, intubating laryngeal mask airway, laryngeal tube, tidal volume
Synopsis
Introduction:
In-hospital cardiopulmonary resuscitation (CPR) response teams may include nurses because of shortages of physicians. Hence, ventilation-associated complications may occur if nurses who are involved in such teams have no extensive experience in emergency airway management.
Rescuers who are unable or untrained to intubate may perform bag-valve-mask ventilation during CPR [1]. In order to reduce the risk of stomach inflation, the European Resuscitation Council recommends a tidal volume of 0.5 l for bag-valve-mask ventilation of a nonintubated cardiac arrest victim, as compared with the 0.8-1.2 l as previously recommended by the American Heart Association [1,2].
It was shown [3,4,5,6,7,8] that a LMA and combitube (Tyco Healthcare, Argyle, NY, USA) may be an alternative to bag-valve-mask ventilation. However, a possible limiting feature of the laryngeal mask is the risk of aspiration [9], and the complex combitube requires extensive instruction and training to ensure correct placement within an acceptable time [10]. Therefore, the ILMA and the laryngeal tube (Fig. 1) have recently been developed [11,12].
Figure 1.
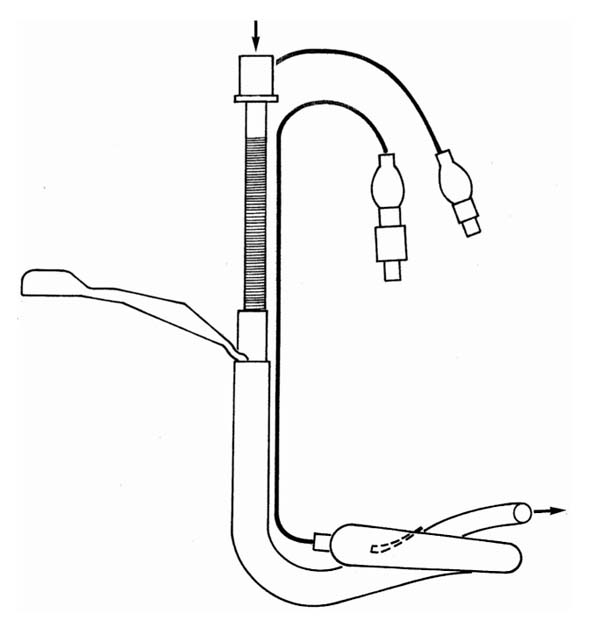
Intubating laryngeal mask airway.
The present study assesses lung ventilation and gastric inflation with the ILMA and the laryngeal tube in a bench model, when performed by intensive care unit (ICU) nurses. Furthermore, it was investigated whether a tidal volume of 0.5 l, rather than 0.8-1.2 l, is beneficial in reducing the risk of gastric inflation.
Methods:
A previously described bench model (lung compliance 50 ml/cmH2O [13]; airway resistance 16 cmH2O/l per s [14]; lower oesophageal sphincter pressure 6 cmH2O [15]) simulating an unintubated cardiac arrest patient [3,4] was used to compare the effects of ventilation using ILMA and laryngeal tube.
All 20 nurses were instructed in the use of the ILMA and the laryngeal tube before the study. The participants then used each ventilatory device with two self-inflating bags (maximum volume 1500 and 1100 ml, respectively; Dräger, Lübeck, Germany) in a randomized order for a 2-min attempt to achieve adequate ventilation. The time to attain a tidal lung volume exceeding 200 ml was recorded. If this volume could not be achieved within 180 s, then it was deemed that the attempt at ventilation had failed. The time to insertion of the endotracheal tube when using the ILMA was recorded, which was followed by another 2-min attempt to achieve adequate ventilation. Standard respiratory monitoring was performed.
The Mann-Whitney U-test was used to compare performance with the two self-inflating bags. Comparison by pairs of the ventilatory devices was performed using the Wilcoxon test; α was set at 0.05.
Results:
The time to deliver the first adequate tidal volume ranged from 26 to 111 s (median 37 s) for the ILMA, and 28-77 s (median 55 s) for the laryngeal tube, resulting in an overall success rate of 100% for both devices. All participants successfully performed `blind' tracheal intubation (median 31 s; range 19-57 s) with the ILMA. When using the medium-sized self-inflating bag (1100 ml), tidal volumes with both ILMA and laryngeal tube were significantly lower (P < 0.05) than those achieved with the adult self-inflating bag (1500 ml; Table 1). Lung tidal volumes and peak airway pressures were not significantly different between the ILMA and the laryngeal tube. No gastric inflation occurred with either airway device (Table 1).
Table 1.
Tidal lung and tidal oesophageal volume, airway and oesophageal peak pressure for the intubating laryngeal mask and laryngeal tube and both self inflating bags
| Laryngeal tube/ | ||||
| mask characteristics | Peak Paw (cmH2O) | Peak Poesoph (cmH2O) | VT lung (ml) | VT oesophagus (ml) |
| ILMA (before endotracheal intubation) | ||||
| 1100 ml bag | 18 ± 2 | 0 | 674 ± 27 | 0 |
| 1500 ml bag | 21 ± 2 | 0 | 790 ± 33* | 0 |
| ILMA (after endotracheal intubation) | ||||
| 1100 ml bag | 25 ± 2* | 0 | 623 ± 26 | 0 |
| 1500 ml bag | 30 ± 3 | 0 | 741 ± 33* | 0 |
| Laryngeal tube | ||||
| 1100 ml bag | 25 ± 2 | 0.1 ± 0.1 | 666 ± 31 | 0 |
| 1500 ml bag | 27 ± 2 | 0.4 ± 0.4 | 752 ± 46 | 0 |
Data are expressed as mean ± standard error of the mean. Paw, airway pressure; Poesoph, oesophageal pressure; VT, tidal volume. *P < 0.05, versus 1100 ml self-inflating bag.
Discussion:
Tracheal intubation is the `gold standard' device for securing the airway during CPR, but it requires excellent skills and experience. Hence, particularly during basic life support management of a cardiac arrest victim, the standard recommendation for ventilation has been to use the bag-valve-face mask while waiting for a professional rescuer who is able to perform tracheal intubation [1]. Airway management with the bag-valve-mask may not provide sufficient ventilation [3,4] or may have adverse consequences such as gastric inflation, with subsequent regurgitation and pulmonary aspiration [6,16,17,18]. The data from the present study suggest that use of the ILMA and the laryngeal tube may be beneficial in ensuring adequate lung ventilation, and may minimize the risk of gastric inflation. Both devices prevented gastric inflation in the bench model used in the present study, even when using the ILMA before securing the airway by performing `blind' endotracheal intubation. Similar to a previous, large clinical study that employed the ILMA [11], the volunteers studied here had cumulative insertion success rates with the first, second and third attempts of 60, 90 and 100%, respectively. This indicates that the ILMA ensures immediate and rapid ventilation and oxygenation, allowing the airway to be secured definitively by a professional rescuer at a later time.
Interestingly, use of both airway devices resulted in comparable tidal volumes of approximately 750 ml, which is significantly higher than tidal volumes achieved with the bag-valve-mask, which resulted in extensive gastric inflation and insufficient pulmonary tidal volumes in earlier studies [3,4].
One approach to achieve proper ventilation may be to choose the best ventilatory device; another strategy may be to employ a smaller tidal volume [1,19]. However, when using the 1100 ml and 1500 ml ventilation bag with the bag-valve-face mask in a historical study [4], only approximately 50-60% of the recommended lung tidal volumes were achieved. It should be pointed out that application of small tidal volumes with the newly developed medium-size self-inflating bag (maximum volume 1100 ml) with both airway devices resulted in lung tidal volumes of approximately 650 ml, which is close to the 500 ml recommended by the European Resuscitation Council and the American Heart Association [1]. This is particularly important, because either ≥ 50% oxygen has to be used when administering tidal lung volumes of 400 ml or less, or larger tidal volumes of 600 ml or more should be applied when room air has to be used in order to maintain both sufficient oxygenation and ventilation [20,21,22].
Limitations include the inability to simulate changing respiratory system compliance, such as during CPR, and the nonsignificant (37 s versus 55 s) difference in insertion time between the LMA and the combitube.
In conclusion, the newly developed medium-size self-inflating bag may be an option for maintaining sufficient ventilation and for reducing the risk of gastric inflation when ventilating an unprotected airway. Both the ILMA and laryngeal tube proved to be valid alternatives for emergency airway management in the experimental model studied here.
Introduction
In-hospital CPR response teams may often include an ICU nurse, because of shortages in physicians who are experienced in CPR. Also, it is quite common that hospital departments are spread over different buildings, or over different floors within the same building. As such, many hospitals may not be able to dispatch experienced physicians to remote locations for prolonged periods of time in order to administer CPR, because this would leave ICU or even operation room patients unattended. Thus, ICU nurses who are in charge of an in-hospital attempt at CPR may be less clinically experienced than an anaesthesiologist, but have to carry full responsibility with regard to pharmacological interventions, and especially airway management. Hence, if such ICU nurses have, for whatever reason, either no extensive theoretical or practical experience in emergency airway management, then the CPR outcome may be jeopardized, for example because of ventilation-associated complications. Thus, if an airway device can be identified that is easy to handle for this group of carers, efforts at CPR may be more successful.
Endotracheal intubation remains the `gold standard' technique for securing the airway, and for protecting the patient from aspiration during CPR [1]. For rescuers who do not have adequate skills in endotracheal intubation, the most common means of providing rapid ventilatory support in nonintubated patients during CPR is the bag-valve-face mask system [1]. Bag-valve-face mask ventilation has a number of well-known disadvantages, including loss of tidal volume via dead-space ventilation, leakage around the face mask and gastric inflation [14,16,17,23,24]. Gastric inflation and subsequent aspiration of stomach contents is a major hazard of bag-valve-mask ventilation during the basic life support phase of CPR [17].
The European Resuscitation Council now recommends a decreased tidal volume of 0.5 l for positive pressure ventilation of a nonintubated cardiac arrest victim, as compared with the 0.8-1.2 l that was previously recommended by the American Heart Association [1,2]. The Airway and Ventilation Management Working Group of the European Resuscitation Council pointed out that a smaller tidal volume may provide reasonable lung ventilation, while avoiding massive stomach inflation, which might result in ventilation-associated complications such as aspiration.
The principal components of the gas distribution in an unprotected airway with positive pressure ventilation are lower esophageal sphincter pressure, peak airway pressure, respiratory system compliance, inspiratory flow rate and airway resistance [25]. Recent clinical investigations and laboratory studies described a significant change in respiratory mechanics during cardiac arrest [14,26,27]. Furthermore, a decrease in the lower esophageal sphincter pressure during cardiac arrest [15] may render gastric inflation even more likely.
It was shown [3,4,5,6,7,8,28,29] that the LMA and the combitube may provide an alternative to bag-valve-mask ventilation. In some studies [3,7], use of the LMA was preferred by student nurses, whereas the combitube was preferred when used by health care professionals who were more experienced in airway management, such as intensive care nursing staff [4]. Nevertheless, a possible limiting feature of the laryngeal mask may be the risk of aspiration of gastric contents [9], because fibreoptic studies have found 6-9% visualization of the oesophagus [30,31]. Although the combitube was developed as an alternative to endotracheal intubation to secure the airway in an emergency setting, its complex structure requires extensive instruction and training to ensure correct placement within an acceptable time [10].
Two other ventilatory devices have recently been developed to provide rapid ventilation and to secure the airway. The ILMA was developed as an additional method of endotracheal intubation, with a specially designed endotracheal tube (Fig. 1) [11,32]. The newly developed laryngeal tube, which is a single-lumen, shortened combitube with an oropharyngeal and oesophageal low-pressure cuff, and a ventilation outlet between these cuffs (Fig. 2), seals the oesophagus and pharynx in a way that enables ventilation of the trachea and lungs. It can be inserted without additional equipment, and in a preliminary clinical trial [12] it was proved to effectively ventilate patients with respiratory arrest.
Figure 2.
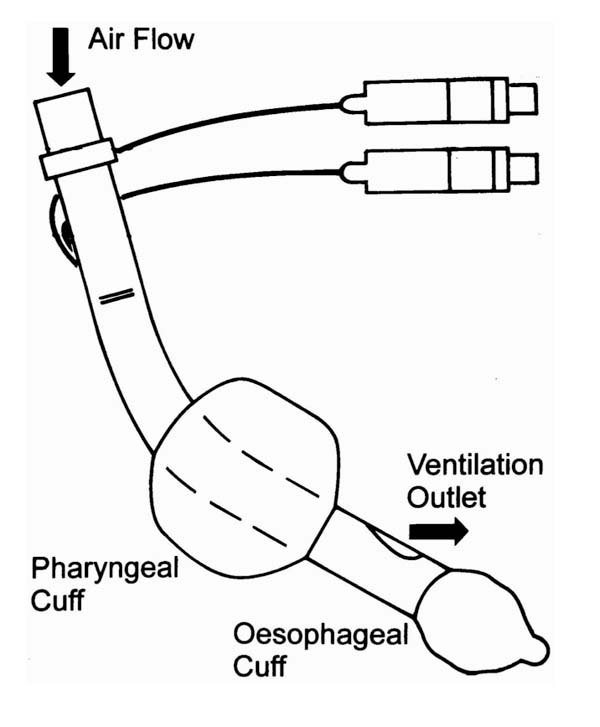
Laryngeal tube.
The purpose of the present study was to assess lung ventilation and gastric inflation when ICU nurses perform ventilation with the ILMA and the laryngeal tube, in a bench model. Furthermore, it was investigated whether smaller tidal volumes, as recommended by the European Resuscitation Council [1], but not previously by the American Heart Association [2], are beneficial in reducing the risk of gastric inflation, as suggested by some previous bench models that simulate a cardiac arrest patient [27,33].
Materials and methods
Experimental model
A previously described bench model [3,4] that simulates an unintubated cardiac arrest patient was used to compare the effects of ventilation using the ILMA and the laryngeal tube (Fig. 3). It consists of an manikin head that is suitable for intubation (Bill I; VBM Medizintechnik, Sulz, Germany) and a lung simulator that allows the compliance and resistance to be adjusted (LS 800; Dräger, Lübeck, Germany). Lung compliance was adjusted to 50 ml/cmH2O [13,26, 34] and airway resistance to 16 cmH2O/l per s [14,26], in order to simulate the respiratory mechanics of a cardiac arrest patient. Respiratory parameters were recorded using the AS3 compact monitor (Datex Ohmeda, Helsinki, Finland). According to the physiology of a cardiac arrest laboratory study, the lower oesophageal sphincter pressure of the simulated stomach was calibrated at 6 cmH2O with an adjustable positive end-expiratory pressure (PEEP) valve [15]. This was then connected to a paediatric pneumotachometer in order to record oesophageal peak pressure and gastric inflation.
Figure 3.
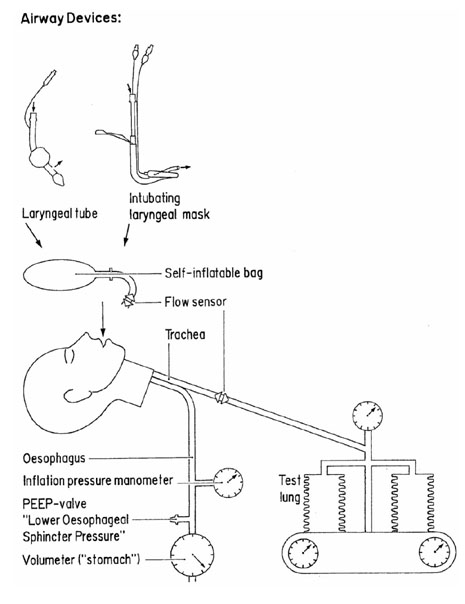
Modification of a previously described bench model of positive-pressure ventilation with an unprotected airway [3,33]. The upper airway was provided by a new intubation manikin head. The tracheal outlet of the manikin head was connected to a mechanical test lung (lung compliance 50 ml/cmH2O; airway resistance 16 cmH2O/l per s). The oesophageal outlet of the manikin head was connected to an adjustable PEEP valve, which represented lower oesophageal sphincter pressure. A second outlet from the PEEP valve was connected to a paediatric pneumotachometer in order to record oesophageal peak pressure and gastric inflation. A flow sensor was inserted between the self-inflating bag and the airway device under investigation; another flow sensor was inserted into the simulated trachea. The flow sensors were connected to respiratory monitors in order to measure ventilation variables.
Experimental protocol
The present study was performed in a research laboratory of a University hospital. Twenty ICU nurses, who were experienced in airway management, but who self-reported no previous experience in ventilation using the ILMA and the laryngeal tube, volunteered to take part in the study.
All volunteers were given theoretical and practical instruction in the use of a size 4 ILMA (LMA International Services Ltd, Hanley, UK) and a size 5 laryngeal tube (VBM, Sulz, Germany) before the study. Using a calibrated syringe, the ILMA required 60 ml inflation volume to achieve a tight seal, which is significantly more than the 30-35 ml that is required in a human. We believe that this was due to the design of the manikin's pharynx. Both cuffs of the laryngeal tube were inflated to 80 mmHg with a cuff pressure manometer. Inflation of the oropharyngeal cuff closes the oropharynx; the esophageal inlet is closed by inflating the lower cuff. For ventilation, we chose an adult and a newly developed self-inflating bag (maximum volumes 1500 and 1100 ml, respectively; Dräger, Lübeck, Germany). The participants then used each ventilatory device with both self-inflating bags in a random order for a 2-min attempt to achieve adequate ventilation of the simulated cardiac arrest patient.
The time to attain a tidal volume exceeding 200 ml was recorded. If this volume could not be achieved within 180 s, it was deemed that the ventilation attempt had failed. Additionally, when using the ILMA, the insertion time of the endotracheal tube was recorded. This was followed by another 2-min attempt to achieve adequate ventilation. Peak airway pressures at the pharynx level and in the oesophagus were recorded, as were lung and gastric tidal volumes during each attempt.
Statistical methods
Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS, Chicago, Illinois, USA). P <0.05 was considered statistically significant. A Kolmogorov-Smirnov adjustment test was performed to assess the distribution of the data. The Mann-Whitney U-test was used to compare the two self-inflating bags. Comparison by pairs of the ventilatory devices was performed using a Wilcoxon test.
Results
Twenty trained ICU nurses (13 female and seven male; age 27-41 years) participated in the present study, and ventilated the experimental model with an adult and a medium-size self-inflating bag. All were able to deliver a tidal volume greater than 200 ml within 180 s on the first attempt at ventilation, resulting in an overall success rate of 100% for the ILMA and laryngeal tube.
The time to deliver the first adequate tidal volume ranged from 26 to 111 s (median 37 s) for the ILMA and from 28 to 77 s (median 55 s) for the laryngeal tube. Additionally, when using the ILMA, all participants successfully performed `blind' endotracheal intubation (median 31 s; range 19-57 s).
When the participants used the medium-size self-inflating bag (1100 ml), tidal volumes but not peak airway pressures with both ILMA and laryngeal tube were significantly lower (P < 0.05) than with the adult (1500 ml) self-inflating bag (Table 1).
Lung tidal volumes and peak airway pressures were not significantly different between the ILMA and the laryngeal tube. Also, statistical analysis of the medium-size self-inflating bag performance revealed no significant differences in peak airway pressures and lung tidal volumes. No gastric inflation occurred with either airway device (Table 1).
Discussion
Ventilation-associated complications were more related to training efforts than to the airway devices themselves, when paramedics in a US Emergency Medical Service were trained to administer advanced airway management [35]. Accordingly, when this experience is extrapolated to ICU nurses providing in-hospital advanced cardiac life support, two pragmatic solutions are possible: extensive, continuous training; and use of an airway device that is simple to handle with little training. Paramedics, emergency physicians and anaesthesiologists perform basic and advanced cardiac life support on a daily basis. ICU registered nurses, however, may spend a larger portion of their working hours caring for patients, without the need to handle respiratory and/or cardiac emergencies on a daily basis. Also, training and maintaining advanced airway skills in all or at least some ICU nurses may be costly, with limited resources available for such proposes.
Without doubt, endotracheal intubation remains the `gold standard' in securing the airway during CPR. However, endotracheal intubation requires excellent skills and experience, and is therefore usually performed by professional rescuers. Hence, particularly during basic life support management of a cardiac arrest victim, the standard recommendation for ventilation has been to use the bag-valve-face mask while waiting for a professional rescuer who is trained and experienced in advanced airway management techniques, such as endotracheal intubation [1].
Earlier studies [3,4] showed that airway management with the bag-valve-face mask performed by both untrained health care personnel and health care personnel such as ICU nurses may not be sufficient. For example, only a few participants of those studies achieved a tidal lung volume in excess of 400 ml using the bag-valve-face mask. Thus, in over 80% of cases, ventilation was not sufficient, which may lead to hypoxaemia and/or hypercapnic acidosis; in turn, this may adversely affect the outcome of CPR. This is in agreement with previous studies [36,37] that indicated that ventilation with the bag-valve-mask may result in ineffective ventilation. The reasons may be an ineffective seal between mask and face, hand fatigue and lack of experience in mask ventilation.
Ventilation of an unprotected airway during the basic life support phase of CPR carries the risk of gastric inflation, with subsequent regurgitation and pulmonary aspiration [6,16,17,18,38]. Also, the change in lower esophageal sphincter pressure and respiratory mechanics during cardiac arrest and CPR may affect the distribution of gas between the lungs and stomach, and direct larger volumes of gas to the stomach rather than to the lungs [33]. In order to determine the distribution of gas between lungs and stomach, we used a previously described experimental model of an unprotected airway [3]. Respiratory system compliance and airway resistance were adjusted in accordance with real-life resuscitation situations [14,34]. The lower esophageal sphincter pressure was set at 6 cmH2O, which is in agreement with a recent investigation that demonstrated a fundamental reduction in lower esophageal sphincter pressure in an animal model within 5 min of cardiac arrest [15].
If the best ventilation strategy can be identified that ensures proper ventilation during CPR when performed by an individual with inconsistent experience in emergency airway management, then improvements in outcome after CPR may result. This has fundamental practical implications. Although services such as helicopter emergency medical service programs or emergency departments are always staffed with individuals who have an extensive and continuous background in emergency airway management, in-hospital CPR response teams often include nurses [39] and some small hospitals may not even have a CPR response team at all. Therefore, ICU nurses may have to perform CPR in an emergency, and may have to carry full responsibility with regard to pharmacological interventions, and especially emergency airway management. Accordingly, there is a good chance that a health care professional without extensive skills in advanced life support may be required to perform emergency airway management. For example, small hospitals may not have an anaesthesiologist on duty 24 h a day. In addition, some hospitals are large and have been built, over decades, into extremely complex structures. This may result in CPR response times of the local emergency medical service that are shorter than in the hospital itself, which further suggests that nurses will be at the scene before the cardiac arrest team arrives. In such cases, if the response time of the cardiac arrest team is greater than 5 min, then by the time they arrive the initial airway management will have determined whether the stomach is inflated, whether the patient remains hypoxic and/or hypercapnic, or whether the patient is adequately ventilated and oxygenated.
In the present study ICU nurses performed emergency airway management of a simulated cardiac arrest patient. The results suggest that use of ILMA and laryngeal tube may be beneficial in ensuring adequate lung ventilation and in minimizing the risk of gastric inflation. Both devices prevented gastric inflation in this bench model, even when using the ILMA before securing the airway by performing `blind' endotracheal intubation, which, interestingly, was successful in all cases. Similar to a previous large clinical study that employed the ILMA [11], these volunteers had cumulative insertion success rates with the first, second and third attempts of 60, 90 and 100%, respectively. This indicates that the ILMA ensures immediate and rapid ventilation and oxygenation, allowing the airway to be secured definitively by a professional rescuer at a later time. As such, use of the ILMA may add flexibility in securing the airway by allowing several options for rescuers with different airway management skills. Namely, rescuers with some airway skills could immediately insert the ILMA and provide ventilation and oxygenation, whereas prolonged intubation efforts may prolong the hypoxic and hypercapnic interval. Subsequently, advanced cardiac life support personnel could then take over with endotracheal intubation via the ILMA.
Although the bag-valve-face mask is the simplest airway device, it resulted in the most gastric inflation and in insufficient pulmonary tidal volumes in historical studies [3,4]. In those studies, the combitube was the only device that safely prevented gastric inflation in a bench model, but it needed extensive and continuous training, which may not be possible. The LMA, however, was easier to handle and faster to insert, but carried a risk of gastric inflation.
The present positive findings are in contrast to those of a previous study [39], which reported that the LMA cannot be recommended as a resuscitation device for use by inexperienced operators. Our data are in agreement with previous reports that showed that use of the LMA during CPR by nurses served as an alternative when intubation was not possible [7,28,40,41].
Interestingly, use of both the ILMA and laryngeal tube resulted in comparable tidal volumes of approximately 750 ml. This is significantly higher than tidal volumes achieved with the bag-valve-mask, which resulted in extensive gastric inflation and insufficient pulmonary tidal volumes in a previous study [4]. Relatively high tidal volumes using the ILMA before endotracheal intubation compared with tidal volumes recommended by the European Resuscitation Council suggest that this airway device may not prevent gastric inflation in all cases.
Accordingly, one approach to achieve proper ventilation may be to choose the best ventilatory device; another strategy may be a smaller tidal volume, as recently recommended by the European Resuscitation Council in order to minimize gastric inflation during ventilation of an unprotected airway [1,19]. Thus, the best combination of the right `hardware' and the right tidal volume may contribute to sufficient oxygenation and ventilation, and might avoid gastric inflation. However, when using the 1100 ml and 1500 ml ventilation bag with the bag-valve-face mask in a historical study, only about 50-60% of the recommended lung tidal volumes were achieved [4]. It has to be pointed out that application of small tidal volumes using the newly developed medium-size self-inflating bag (maximum volume 1100 ml) with ILMA and laryngeal tube in our bench model resulted in lung tidal volumes of approximately 650 ml. This is close to the 500 ml recommended by the European Resuscitation Council and the American Heart Association [1]. This is particularly important, because either ≥ 50% oxygen has to be used when administering tidal lung volumes of 400 ml or less, or larger tidal volumes of 600 ml or more should be applied when room air has to be used in order to maintain both sufficient oxygenation and ventilation [20,21,22].
Some limitations of the present study should be noted. First, the value of experimental models in simulating cardiac arrest situations is always debatable. One advantage of the experimental model is that respiratory variables can be carefully controlled, and a certain hypothesis may be fully investigated. Furthermore, because of ethical and design limitations, it is impossible to perform such a study in human cardiac arrest patients. We suggest that, because of the careful design of the model, the bench model used here closely simulates the respiratory mechanics of a human cardiac arrest patient. We chose this established experimental model in order to control respiratory mechanics and lower esophageal sphincter pressure, and to secure stable conditions for all participating volunteer health care professionals. A second limitation is that it is impossible to simulate changing respiratory system compliance, such as occurs during CPR, which was demonstrated in a laboratory model [27]. Third, although the manikin used here was unable to simulate the upper airway of a human perfectly with regard to sealing conditions, we suggest that peak airway pressure values in both the ILMA and laryngeal tube group indicated an adequate seal. Fourth, although there was a difference in insertion time between the LMA and the combitube (37 s versus 55 s), this difference was not statistically significant. This suggests that the present study is underpowered in terms of determining differences in insertion time; therefore, no statistical analysis or commentary is given with regard to this end-point.
Finally, we acknowledge that converting a scientific observation into routine clinical practice may be a challenge. Topics that may be raised are as follows. How will teaching of these techniques be organized for nursing personnel, and will all members of the nursing staff be trained, or only certain nurses? Will training be solely manikin-based or will this include work in the operating theatre with anaesthetized patients, and how long will it last? Which devices will be chosen, what criteria will be used to choose between the devices, and how will the nurse decide what size to use for a given patient?
In conclusion, the newly developed medium-size self-inflating bag may be an option to maintain sufficient ventilation and reduce the risk of gastric inflation when ventilating an unprotected airway. Both the ILMA and laryngeal tube proved to be valid alternatives for emergency airway management in the experimental model studied here.
Acknowledgments
Acknowledgement
No author has a potential conflict of interest that relate to the present report. This project was supported, in part, by the Department of Anaesthesiology, the Medical University of Lübeck, Germany.
References
- The European Resuscitation Council (ERC), and the American Heart Association (AHA) in Collaboration with the International Liaison Committee on Resuscitation (ILCOR): International Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiac Care -- An International Consensus on Science. Circulation. 2000;102(suppl 1):22–59. [Google Scholar]
- Emergency Cardiac Care Committee and Subcommittees American Heart Association: Guideline for cardiopulmonary resuscitation and emergency cardiac care. Part II: adult basic life support. JAMA . 1992;268:2184–2198. [PubMed] [Google Scholar]
- Doerges V, Sauer C, Ocker H, Wenzel V, Schmucker P. Airway management during cardiopulmonary resuscitation. A comparison of bag-valve-mask, laryngeal mask and combitube. Resuscitation. 1999;41:63–69. doi: 10.1016/s0300-9572(99)00036-2. [DOI] [PubMed] [Google Scholar]
- Dörges V, Sauer C, Ocker H, Wenzel V, Schmucker P. Smaller tidal volumes during cardiopulmonary resuscitation: comparison of adult and paediatric self-inflatable bags with three different ventilatory devices. . Resuscitation. 1999;43:31–37. doi: 10.1016/s0300-9572(99)00117-3. [DOI] [PubMed] [Google Scholar]
- Frass M, Frenzer R, Rauscha F, Weber H, Pacher R, Leithner C. Evaluation of the esophageal tracheal combitube in cardiopulmonary resuscitation. Crit Care Med. 1987;15:609–611. doi: 10.1097/00003246-198706000-00015. [DOI] [PubMed] [Google Scholar]
- Ho-Tai LM, Devitt JH, Noel AG, O'Donnell MP. Gas leak and gastric insufflation during controlled ventilation: face mask versus laryngeal mask airway. Can J Anaesth. 1998;45:206–211. doi: 10.1007/BF03012903. [DOI] [PubMed] [Google Scholar]
- Anonymous: The use of the laryngeal mask airway by nurses during cardiopulmonary resuscitation. Results of a multicentre trial. . Anaesthesia. 1994;49:3–7. doi: 10.1111/j.1365-2044.1994.tb03302.x. [DOI] [PubMed] [Google Scholar]
- Stone BJ, Chantler PJ, Baskett PJF. The incidence of regurgitation during cardiopulmonary resuscitation: a comparison between the bag valve mask and laryngeal mask airway. Resuscitation. 1998;38:3–6. doi: 10.1016/s0300-9572(98)00068-9. [DOI] [PubMed] [Google Scholar]
- Weiler N, Latorre F, Eberle B, Goedecke R, Heinrichs W. Respiratory mechanics, gastric insufflation pressure, and air leakage of the laryngeal mask airway. Anesth Analg. 1997;84:1025–1028. doi: 10.1097/00000539-199705000-00013. [DOI] [PubMed] [Google Scholar]
- Atherton GL, Johnson JC. Ability of paramedics to use the combitube in prehospital cardiac arrest. Ann Emerg Med. 1993;22:27–32. doi: 10.1016/s0196-0644(05)80104-0. [DOI] [PubMed] [Google Scholar]
- Baskett PJF, Parr MJA, Nolan JP. The intubating laryngeal mask. Results of a multicentre trial with experience in 500 cases. . Anaesthesia. 1998;53:1174–1179. doi: 10.1046/j.1365-2044.1998.00614.x. [DOI] [PubMed] [Google Scholar]
- Dörges V, Ocker H, Wenzel V, Schmucker P. The laryngeal tube: a new simple airway device. Anesth Analg. 2000. [DOI] [PubMed]
- Safar P, Agusto-Escarraga L. Compliance in anesthetized adults. . Anesthesiology. 1959;20:283–289. doi: 10.1097/00000542-195905000-00005. [DOI] [PubMed] [Google Scholar]
- Weiler N, Heinrichs W, Dick W. Assessment of pulmonary mechanics and gastric inflation pressure during mask ventilation. Prehosp Disaster Med. 1995;10:101–105. doi: 10.1017/s1049023x00041807. [DOI] [PubMed] [Google Scholar]
- Bowman FP, Menegazzi JJ, Check BD, Duckett TM. Lower esophageal sphincter pressure during prolonged cardiac arrest and resuscitation. . Ann Emerg Med. 1995;26:215–219. doi: 10.1016/s0196-0644(95)70154-0. [DOI] [PubMed] [Google Scholar]
- Lawes EG, Baskett PJ. Pulmonary aspiration during unsuccessful cardiopulmonary resuscitation. Intensive Care Med. 1987;3:379–382. doi: 10.1007/BF00257678. [DOI] [PubMed] [Google Scholar]
- Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987;92:287–291. doi: 10.1378/chest.92.2.287. [DOI] [PubMed] [Google Scholar]
- Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. Am J Obstet Gynecol. 1946;52:191–194. doi: 10.1016/s0002-9378(16)39829-5. [DOI] [PubMed] [Google Scholar]
- Baskett P, Nolan J, Parr M. Tidal volumes which are perceived to be adequate for resuscitation. Resuscitation. 1996;31:231–234. doi: 10.1016/0300-9572(96)00994-x. [DOI] [PubMed] [Google Scholar]
- Dörges V, Ocker H, Hagelberg S, Wenzel V, Schmucker P. Smaller tidal volumes with room-air are not sufficient to ensure adequate oxygenation during bag-valve-mask ventilation. Resuscitation. 2000;44:37–41. doi: 10.1016/s0300-9572(99)00161-6. [DOI] [PubMed] [Google Scholar]
- Dörges V, Ocker H, Hagelberg S, Wenzel V, Schmucker P. Optimisation of tidal volumes given with self-inflatable bags without additional oxygen during simulated basic life support. . Resuscitation. 2000;43:195–199. doi: 10.1016/s0300-9572(99)00148-3. [DOI] [PubMed] [Google Scholar]
- Wenzel V, Keller C, Idris AH, Doerges V, Lindner KH, Brimacombe JR. Effects of smaller tidal volumes during basic life support ventilation in patients with respiratory arrest: good ventilation, less risk? Resuscitation. 1999;43:25–29. doi: 10.1016/s0300-9572(99)00118-5. [DOI] [PubMed] [Google Scholar]
- Ruben H, Knudsen EJ, Carugati G. Gastric insufflation in relation to airway pressure. Acta Anaesthesiol Scand. 1961;5:107–114. doi: 10.1111/j.1399-6576.1961.tb00089.x. [DOI] [PubMed] [Google Scholar]
- Wenzel V, Idris AH, Lindner KH. Ventilation with an unprotected airway during cardiac arrest. Yearbook of Intensive Care and Emergency Medicine. Edited by Vincent JL. Berlin, Heidelberg: Springer; 1997. pp. 483–492.
- Wenzel V, Idris AH. The current status of ventilation strategies during cardiopulmonary resuscitation (CPR). Curr Opin Crit Care . 1997;3:206–213. doi: 10.1097/00075198-200206000-00002. [DOI] [PubMed] [Google Scholar]
- Ornato JP, Bryson BL, Donovan PJ, Faquharson RR, Jaeger C. Measurement of ventilation during cardiopulmonary resuscitation. . Crit Care Med. 1983;11:79–82. doi: 10.1097/00003246-198302000-00004. [DOI] [PubMed] [Google Scholar]
- Wenzel V, Idris AH, Banner MJ, Kubilis PS, Band R, Williams JL, Jr, Lindner KH. Respiratory system compliance decreases after cardiopulmonary resuscitation and stomach inflation: Impact of large and small tidal volumes on calculated peak airway pressure. . Resuscitation. 1998;38:113–118. doi: 10.1016/s0300-9572(98)00095-1. [DOI] [PubMed] [Google Scholar]
- Martin PD, Cyna AM, Hunter WAH, Henry J, Ramayya GP. Training nursing staff in airway management: a clinical comparison of the face mask and the laryngeal mask. Anaesthesia. 1993;48:33–37. [PubMed] [Google Scholar]
- Frass M, Frenzer R, Zdrahal F, Hoflehner G, Porges P, Lackner F. The esophageal tracheal combitube: preliminary results with a new airway for CPR. Ann Emerg Med. 1987;16:768–772. doi: 10.1016/s0196-0644(87)80571-1. [DOI] [PubMed] [Google Scholar]
- Barker P, Langton JA, Murphy PJ, Rowbotham DJ. Regurgitation of gastric contents during general anaesthesia using the laryngeal mask airway. . Br J Anaesth. 1992;69:358–360. doi: 10.1093/bja/69.3.314. [DOI] [PubMed] [Google Scholar]
- Payne J. The use of the fibreoptic laryngoscope to confirm the position of the laryngeal mask [letter]. Anaesthesia. 1989;44:865. [Google Scholar]
- Chan YW, Kong CF, Kong CS, Hwang NC, Ip-Yam PC. The intubating laryngeal mask airway (ILMA): initial experience in Singapore. Br J Anaesth. 1998;81:610–611. doi: 10.1093/bja/81.4.610. [DOI] [PubMed] [Google Scholar]
- Wenzel V, Idris AH, Banner MJ, Kubilis PS, Williams JL. Influence of tidal volume on the distribution of gas between the lungs and the stomach in the nonintubated patient receiving positive pressure ventilation. Crit Care Med. 1998;26:364–368. doi: 10.1097/00003246-199802000-00042. [DOI] [PubMed] [Google Scholar]
- Davies K, Jr, Johannigman JA, Johnson RC, Jr, Branson RD. Lung compliance following cardiac arrest. Acad Emerg Med. 1995;10:855–856. doi: 10.1111/j.1553-2712.1995.tb03100.x. [DOI] [PubMed] [Google Scholar]
- Pepe PE, Zachariah BS, Chandra NC. Invasive airway techniques in resuscitation. . Ann Emerg Med. 1993;22:393–403. doi: 10.1016/s0196-0644(05)80470-6. [DOI] [PubMed] [Google Scholar]
- Alexander R, Hodgson P, Lomax D, Bullen C. A comparison of the laryngeal mask airway and Guedel airway for manual ventilation following formal training. Anaesthesia. 1993;48:231–234. doi: 10.1111/j.1365-2044.1993.tb06909.x. [DOI] [PubMed] [Google Scholar]
- Elling R, Politis J. An evaluation of emergency medical technicians' ability to use manual ventilation devices. Ann Emerg Med. 1983;12:765–768. doi: 10.1016/s0196-0644(83)80254-6. [DOI] [PubMed] [Google Scholar]
- Osterwalder JJ, Schuhwerk W. Effectiveness of mask ventilation in a training manikin. A comparison of the Oxylator EM100 and the bag-valve device. Resuscitation. 1998;36:23–27. doi: 10.1016/s0300-9572(97)00091-9. [DOI] [PubMed] [Google Scholar]
- Tolley PM, Watts AD, Hickman JA. Comparison of the use of the laryngeal mask and face mask by inexperienced personnel. Br J Anaesth. 1992;69:320–321. doi: 10.1093/bja/69.3.320. [DOI] [PubMed] [Google Scholar]
- Brimacombe J. The advantage of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anaesth. 1995;42:1017–1023. doi: 10.1007/BF03011075. [DOI] [PubMed] [Google Scholar]
- Yardy N, Hancox D, Strang T. A comparison of two airway aids for emergency use by unskilled personnel. Anaesthesia. 1999;54:172–197. doi: 10.1046/j.1365-2044.1999.00651.x. [DOI] [PubMed] [Google Scholar]


