Abstract
Objective
Fatigue is a common and distressing complaint among people with diabetes, and likely to hinder the ability to perform daily diabetes self-management tasks. A review of the literature about diabetes-related fatigue was conducted with an eye toward creating a framework for beginning to conduct more focused studies on this subject.
Methods
A literature search containing the terms diabetes, fatigue, tiredness, and symptoms was conducted to search for literature that addressed diabetes-related fatigue.
Results
Diabetes presents many potential pathways for fatigue, but focused studies on this symptom are rare. Furthermore, research on diabetes-related fatigue is limited by fatigue's non-specific symptoms and because fatigue researchers have yet to agree on standardized definition, measurement or diagnostic criteria. Additionally, few diabetes randomized clinical trials included measurement of patient-reported outcomes, such as symptoms or health-related quality of life in their study designs, though one that did provided some the meaningful finding that symptom-focused education improved self-management practices, HbA1c levels, quality of life and symptom distress.
Conclusion
There is a need to standardized definition, measurement and diagnostic criteria of fatigue in diabetes. We present a model that can guide focused studies on fatigue in diabetes. The model capitalizes on the multidimensional phenomena (physiological, psychological, and lifestyle) associated with fatigue in diabetes.
Keywords: Diabetes, fatigue, review
Introduction
Diabetes mellitus, a major public health problem, affects approximately 6% of the world's adult population, and is increasing in epidemic proportions.1, 2 Among people with diabetes, fatigue is a pervasive and distressing complaint. Although fatigue also occurs in other medical disorders, the importance of fatigue may be greater in individuals with diabetes. Clinicians who work with patients affected by diabetes have noted anecdotally the considerable toll that fatigue takes on their patients, yet there is little empirical research describing the severity of the problem. Fatigue in diabetes may be associated with physiological phenomena, such as hypo- or hyperglycemia or wide swings between the two. Fatigue may also be related to psychological factors, such as depression or emotional distress related to the diagnosis or to the intensity of diabetes self-management regimens. Fatigue may also be related to such lifestyle issues as lack of physical activity or being overweight--especially common in people with type 2 diabetes. Research is needed to clarify these relationships in order to help people with diabetes manage this symptom.
Purpose
Herein, we review the existing literature about diabetes-related fatigue with an eye toward creating a framework for beginning to conduct more focused studies on this subject.
Definitions of Fatigue
Fatigue is a word commonly used in everyday conversations, with subjective meanings as varied as the individuals using it. Terms including fatigue, sleepiness, tiredness, lacking energy, and exhaustion are used interchangeably. Within the scientific literature, definitions of fatigue vary greatly, and defining fatigue becomes more challenging because there is poor differentiation among causes, indicators, and effects 1, 2. Fatigue has largely been defined as either a subjective symptom or an objective performance decrement 3, but has also been identified as a syndrome unto itself (chronic fatigue syndrome). Fatigue is generally acknowledged to be complex and/or multifaceted 4-6, encompassing physiological, psychological, and situational components, such as life or work events 4-13.
While fatigue is considered a normal occurrence in daily life, it is also a symptom associated with a variety of physiological and psychological conditions. Fatigue normally occurs after mental or physical exertion, inadequate sleep, or other temporary phenomena. Sometimes called acute or healthy, such fatigue is usually temporary and alleviated with rest. Acute fatigue serves as a protective mechanism by signaling the body's need for rest. Chronic, or pathologic fatigue, however, occurs after modest effort and continues despite rest.10, 16, 17 Terms such as “unrefreshed by sleep” or “unresponsive to rest” have been used by some authors to differentiate chronic fatigue from acute.7-9, 13, 18 This type of8, 14, 15 fatigue is most notably associated with diseases such as cancer, chronic obstructive pulmonary disease, rheumatoid arthritis, depression, and fibromyalgia, but it may also play a significant role in diabetes.
A common view is that fatigue results from one or a combination of peripheral physiologic processes--alone or in combination with the brain and/or its neurological systems. Fatigue has been distinguished as “peripheral” and “central” depending on which processes and systems are involved. Peripheral fatigue has been described as a purely physiologic phenomenon, involving an end organ such as skeletal or cardiac muscle and has been defined as “the decline in muscle tension (force) capacity with repeated stimulation” (p. 400).19 Peripheral fatigue, such as that seen in skeletal muscle, occurs from a combination of neurological, musculoskeletal, and metabolic aberrations, such as reductions in hepatic or muscular glycogen stores, reduced oxygen consumption during activity, and muscle fiber changes resulting from physical inactivity or aging.
Central fatigue is thought to result from disturbances to the complex neurological circuitry connecting the brain's motor coordination centers (basal ganglia) with the executive center (frontal lobe) and internal motivational center (hypothalamus and limbic system).20 These neuroregulatory mechanisms are vulnerable to episodes of hypoxia, inflammatory processes, alterations in neurotransmitter release (e.g., serotonin or dopamine), and other central nervous system (CNS) disturbances. Central fatigue differs from peripheral fatigue in that it occurs in the absence of clinically detectable motor weaknesses. Central fatigue has been defined as the “failure to initiate and/or sustain attentional tasks (mental fatigue) and physical activities (physical fatigue) requiring self motivation (as opposed to external stimulation)” (p. 35).20 Episodes of central fatigue may be of short duration, such as those following viral illnesses or sleep disturbances, but may also persist for many months, as seen in neurological disorders, including Parkinson's disease or multiple sclerosis.
Some believe that fatigue is psychological in origins. However, psychological fatigue has not been adequately defined in the literature. Psychological fatigue symptoms may originate from emotional phenomena or may arise from alterations in neurotransmitter release such as is seen in clinical depression. A recent study of fatigue in primary care patients suggested that psychological disorders were more predictive of fatigue than were physical illnesses.21 Psychological phenomena not usually treated clinically, including stress and burnout phenomena, have also been associated with increased levels of fatigue.
Fatigue is one of the most common somatic symptoms associated with depression22-26 and is among the nine diagnostic criteria for major depressive disorder as outlined in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV).27 Recently, semi-structured interviews were conducted with 1,523 psychiatric outpatients to reevaluate each of the symptoms for their appropriateness for continued inclusion in the current DSM-IV diagnostic criteria for major depression.28 The authors predicted that somatic symptoms such as fatigue, insomnia, and impaired concentration would not retain a high enough degree of specificity for diagnosing depression since they are also diagnostic criteria for other illnesses. Contrary to prediction, 87.2% of the subjects reported being fatigued, suggesting that fatigue is a highly sensitive marker of depression. In further logistic regression analyses, fatigue was as strong a predictor of depression as those symptoms considered to be unique to depression.28
Consequences of Fatigue
Among healthy individuals without diabetes, self-reported symptoms such as fatigue have been found to negatively affect self-rated health and quality of life 28. Fatigue has also been associated with decreased physical functioning and decreased ability to manage routine daily activities 26, 29. While few studies have examined the relationship between fatigue and daily functioning in individuals with diabetes, fatigue is likely a barrier to their health-promoting behaviors, such as participating in diabetes self-care regimens, following a healthy eating plan or participating in regular exercise.
Despite the consequences, fatigue remains a challenging problem for treatment by health care providers. Wessely suggests that because fatigue is a non-specific and universal symptom, clinicians are hindered in appropriately diagnosing or treating the problem 3. In addition, fatigue researchers have yet to agree on standardized definition, measurement or diagnostic criteria, further hindering our understanding of this symptom. Thus, we undertook this review to move toward creating a framework for beginning to conduct focused studies on fatigue in diabetes.
Fatigue in Diabetes
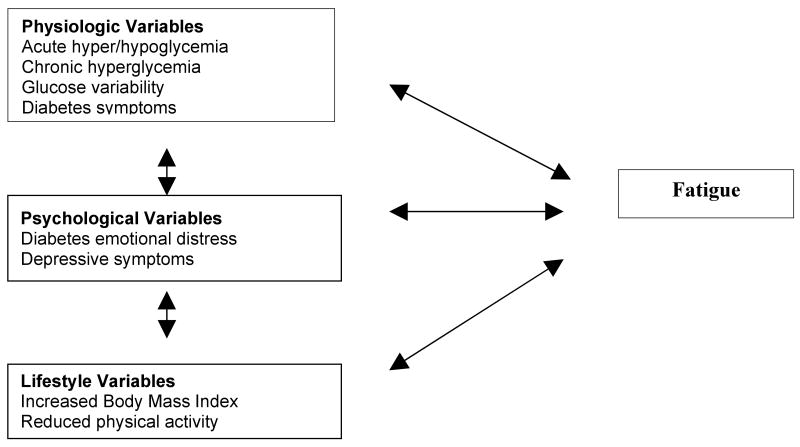
As in other conditions, fatigue in people with diabetes is likely to be multidimensional, encompassing physiological, psychological, and lifestyle factors (Figure 1).
Figure 1.
Exploratory Framework of Fatigue in Diabetes
Physiologic Diabetes-Specific Factors Relating to Fatigue
One likely reason for fatigue in diabetes (uncomplicated by severe comorbidities) is alterations in blood glucose levels. Altered blood glucose metabolism may result in acute and chronic hyperglycemic episodes, hypoglycemia, or blood glucose fluctuations. These alterations may affect fatigue separately or in tandem. The presence of short- and long-term complications of diabetes and their symptoms, including symptoms of hypo- or hyperglycemia, cardiac disease, neuropathy, or retinopathy, has also been associated with increased fatigue 30-32.
Glucose Metabolism
Acute hyper/hypoglycemia
Some evidence suggests that acute glycemic excursions are associated with fatigue. During an in-depth analysis of common hyperglycemic symptoms, 361 insulin-treated diabetics were asked to list their most common symptoms and report the blood glucose level at which those symptoms occurred 33. Tiredness was ranked fifth of the 16 most commonly reported symptoms. A mean symptom inventory score was computed for each subject based on the 16 symptoms. There was only a slight association between mean symptom inventory score and chronic glucose control measured by hemoglobin A1c (r = 0.149, p < 0.003). However 85% of the subjects were able to estimate a hyperglycemic threshold for the onset of their symptoms (including tiredness). The mean blood glucose threshold was 274 mg/dl, suggesting that acute elevations of blood glucose were more predictive of symptoms, including tiredness. Subjects also reported tiredness during lower levels of hyperglycemia, prior to osmotic symptoms such as thirst or increased urination 33.
More recently, the effects of acute hyperglycemia on cognition and mood were examined in a group of 20 subjects with type 2 diabetes 34, and the study concluded that acute episodes of hyperglycemia were significantly associated with diminished cognitive function and altered mood states, including heightened fatigue 34.
Findings from an epidemiological study of 1,137 general practice patients with newly diagnosed type 2 diabetes revealed that fatigue was present in approximately 61% of patients at the time of diagnosis and was significantly associated with fasting plasma glucose (FPG) levels, but not hemoglobin A1c 35. It is possible that the average hemoglobin A1c may be falsely low in this group because their blood glucose level may not have been elevated the full three months. Similar findings were reported in 430 adults with newly diagnosed type 2 diabetes, prior to enrolling in the United Kingdom Prospective Diabetes Study (UKPDS) 36. A high number of symptom complaints (including fatigue) was significantly associated with FPG, body mass index (BMI), and female gender. There was no association between symptom complaints and hemoglobin A1c, again suggesting a stronger association between fatigue and acute, rather than chronic, hyperglycemia.
Acute episodes of hypoglycemia have also been associated with higher levels of fatigue. In a controlled study of adults with type 1 diabetes, the effects of a nocturnal hypoglycemic episode on subsequent subjective well-being and physical fatigue were examined 37. In this study, blood glucose levels were lowered to hypoglycemic levels (42-59 mg/dl) during one overnight visit, and maintained within a higher range (90-216 mg/dl) during a second overnight visit. The morning following the hypoglycemia visit, subjects reported more fatigue symptoms, decreased well-being, and were more likely to fatigue faster during an exercise bout than when blood glucose levels were maintained within the higher range.
Chronic hyperglycemia
Chronic hyperglycemia has long been assumed to cause fatigue; however, few data support this relationship. One cross-sectional study examined the relationship between glucose control and physical symptoms, moods, and well-being. The study included 188 Dutch patients with type 2 diabetes 38, and fatigue was measured using two different instruments: the Diabetes Symptom Checklist-Type 2 (DSC-Type 2) 39 and the Profile of Mood States (POMS) 40. Slight, but statistically significant, correlations between HbA1c and fatigue were noted using both instruments (DSC-Type 2 r = 0.14, p < 0.05; POMS r = 14, p < 0.05), suggesting that chronic hyperglycemia may contribute to fatigue.
In contrast, there was no association between hemoglobin A1c and fatigue symptoms as measured by the DSC-Type 2 during a two-year prospective study examining the initiation of insulin therapy in Dutch adults with type 2 diabetes 41. The authors reported a significant relationship of every unit increase of insulin dose with DSC-Type 2 total symptom complaint scores (which included a fatigue subscale) and POMS anger, displeasure, and fatigue scores, suggesting increased emotional fatigue possibly related to increased hypoglycemic events and the burden of daily injections 41.
In a study of patients with type 2 diabetes and restless leg syndrome, hemoglobin A1c was associated with sleepiness (as measured by the Epworth Sleepiness Scale), but not fatigue (as measured by the Fatigue Severity Scale) 42.
Glucose variability (blood glucose fluctuations)
Glucose variability can be defined as the fluctuations in glucose levels that may occur rapidly over minutes or over hours. In the clinical setting, glucose variability may be missed, since glucose fluctuations will not be revealed through a single measure of blood glucose or with a hemoglobin A1c test. Fluctuations in blood glucose levels, regardless of overall blood glucose control as measured by hemoglobin A1c, may contribute to fatigue.
There is evidence to suggest that the frequency and magnitude of blood glucose fluctuations may be greater in individuals with type 1 diabetes, who are more sensitive to the effects of exogenous insulin, have altered glucagon and norepinephrine responses to hypoglycemia, and may overcompensate by overtreating hypoglycemia. These factors place them at higher risk for hypoglycemia and hyperglycemia excursions than patients with type 2 diabetes.45 However, a growing body of literature suggests that individuals with type 2 diabetes may also experience blood glucose fluctuations.46-48 A study of non-insulin-treated adults with type 2 diabetes (n = 856), revealed exaggerated postprandial glucose excursions (in excess of 40 mg/dl) from pre-meal blood glucose values in the majority of subjects. These findings were consistent, even in subjects with hemoglobin A1c values in the satisfactory range (< 7.0%).46 Recent evidence suggests that these glucose fluctuations during the postprandial period may be strong triggers for inflammatory markers and oxidative stress, thought to play a key role in the development of diabetic vascular complications 43. Oxidative stress and fatigue were studied in patients with chronic fatigue syndrome. In a control-matched, cross-sectional study of 47 adults with chronic fatigue syndrome, increased markers of oxidative stress, including isoprostanes and oxidized low-density lipoproteins, were associated with chronic fatigue symptoms 44
Glucose variability may also cause psychological fatigue. Patients who frequently experience wide swings in blood glucose levels are likely to feel that they are failing at maintaining good diabetes control. They may feel “worn out” or “burned out” from the daily tasks of diabetes self-management and disengage from performing those tasks. Over a long period of time, this neglect could result in worsening of blood glucose control, thus increasing the risk for long-term complications.
Diabetes-Related Long-Term Complications/Symptoms
Many of the chronic complications associated with diabetes are associated with fatigue. Diabetes is the leading cause of end-stage renal disease (ESRD) in the United States 45. Anemia, the major side effect of impaired kidney function, results in increased fatigue. Among patients undergoing dialysis for treatment of ESRD, symptoms (including fatigue) negatively affected quality of life and were significantly worse among the patients with diabetes than those without diabetes 30. Additionally, investigators have suggested that anemia is more prevalent in patients with diabetes than without 46 and occurs during the earliest stages of kidney disease, when only microscopic amounts of urinary protein are present 47.
Some form of neuropathy (nerve damage) will affect 60%-70% of all people with type 1 or type 2 diabetes 45. Peripheral neuropathy, which predominantly affects the hands and the feet, is the most common form of diabetic neuropathy. In a study of adults with type 1 and 2 diabetes, foot pain was positively correlated with symptoms of general fatigue (r = 0.63, p < 0.001), physical fatigue (r = 0.48, p < 01) and reduced activity (r = 0.48, p < 01) 32.
Peripheral vascular disease is often present in patients with diabetic peripheral neuropathy, and causes deep, aching pain in the calves. Inadequate perfusion to the lower extremities deprives the tissues of oxygen, nutrients, and antibiotics, and impairs waste removal, thus placing the limb at risk for impaired wound healing and gangrene. Treatment for lower extremity infections and ulcerations usually includes reduced ambulation or bearing no weight on the affected limb. The combination of poor substrate utilization, infection risk, and reduced physical activity may all contribute to fatigue.
Diabetes-related symptoms, whether or not a comorbid condition has been diagnosed, have also been associated with fatigue. Findings from a study addressing workplace fatigue in 292 individuals with insulin-treated diabetes reported that diabetes symptoms and the burden of adjusting insulin dosages accounted for 29% of the variance in fatigue scores 48. In a later paper, these authors found that individuals with diabetes and a comorbid condition reported more prolonged fatigue than did either healthy persons or individuals with diabetes and no comorbid condition 31. Neither paper described the specific diabetes symptoms that were associated with the increased fatigue, nor did either study distinguish between subjects with type 1 or 2 diabetes. Both studies, however, offered additional support that diabetes fatigue may have deleterious effects on job or work roles.
Psychological Factors Associated with Fatigue in Diabetes
The proposed fatigue research framework (Figure 1) suggests that there are two key psychological variables that are most likely associated with diabetes-related fatigue: diabetes emotional distress and depressive symptoms.
Diabetes emotional distress
Mental fatigue associated with managing diabetes's chronic and complicated medical regimen has been termed “Diabetes Overwhelmus” in the lay press 49. A new term has evolved called “diabetes emotional distress” which represents a sub-clinical field of psychological disturbances 50, 51. This term is related to the work of managing and living with diabetes. Diabetes emotional distress, frequently called “diabetes burnout,” has been eloquently described:
Burnout is what happens when you feel overwhelmed by diabetes and by the frustrating burden of diabetes self-care. People who have burned out realize that good diabetes care is important for their health, but they just don't have the motivation to do it. At a fundamental level, they are at war with their diabetes--and they are losing 52.
Little research has directly linked diabetes emotional distress or burnout to fatigue; however, “lack of energy” and “feeling that diabetes is taking up too much of my mental and physical energy everyday” are measurement items in the instruments most widely used to measure diabetes emotional distress 50, 53. From data collected on 87 adults with type 1 and type 2 diabetes, Casalenuovo reported that the stress of living with diabetes was disruptive to well-being and led to energy depletion and fatigue 54. Multiple regression analysis revealed that stress accounted for 23% of the variance in fatigue (p < 0.01) 54. In a study evaluating the influence of initiating insulin therapy on physical symptoms, mood states, general well-being (including fatigue), and treatment satisfaction in adults with type 2 diabetes, subjects reported no changes in physiological fatigue symptoms with improved glucose control 41. However, psychological fatigue symptoms such as feeling “burned out” increased significantly. The subjects in the intervention group, who were started on insulin therapy, reported more frequent insulin reactions and weight gain. These findings support the relationship between the increased burden of diabetes management and psychological/emotional fatigue, despite improved physiologic blood glucose control.
The concept of burnout has been strongly associated with workplace fatigue. Maslach has conceptualized three key dimensions associated with job burnout: overwhelming exhaustion, feeling of cynicism and detachment from job, and sense of ineffectiveness and lack of accomplishment 55. These dimensions may be seen in a non-workplace context in patients who experience “diabetes burnout.” When patients with diabetes do not experience positive results from their efforts at diabetes self-management, or when they experience unanticipated or negative results, they may experience a sense of ineffectiveness or lack of accomplishment. Over time, they may experience emotional fatigue, cynicism, and resultant detachment from their health care provider's recommendations. These factors may play a role in exacerbating physiologic fatigue, or adding a psychological dimension to it. This has special implications for individuals with diabetes. There is a growing body of evidence that working-age adults with diabetes are more likely to be unemployed or unable to work, miss work days, or have severe difficulty with work tasks compared to those without diabetes 56, 57.
Depression
Research has suggested that individuals with diabetes are twice as likely to suffer from depression as the general population 58. A recent meta-analysis reported that elevated depressive symptoms were present in 11% and major depression was present in 31% of individuals with diabetes 58. In addition, diabetes has been associated with an increased risk for developing depression or depressive symptoms 58-60, while clinical depression and depressive symptoms have been associated with increased risk for diabetes 61, 62. These findings underscore the importance of and challenges to clinical measurement of fatigue in people with diabetes.
Lifestyle Factors Associated with Fatigue in Diabetes
Although numerous lifestyle factors may affect fatigue, being overweight and engaging in low levels of habitual physical activity have been strongly associated with fatigue and have special clinical relevance for many patients with diabetes.
Body mass index
Most people with insulin-resistant type 2 diabetes are overweight or obese 63. Obesity and overweight have been associated with higher levels of fatigue in the general population 64-66, and were independently associated with fatigue levels in women 65. The physiological and psychological phenomena that mediate the relationship between obesity and fatigue have not been fully elucidated; however, there is a growing body of literature suggesting that increased levels of pro-inflammatory cytokines (as seen in obese individuals) may be significant factors in fatigue levels 67-69
Physical activity
There is growing interest in the relationship between self-reported feelings of fatigue and physical activity. Much evidence supports the positive effects of regular physical activity on alleviating symptoms of fatigue 70-73. Physical activity has been inversely associated with reported fatigue levels in diverse populations, including patients with cancer 74, rheumatoid arthritis 75 and chronic diseases, including diabetes and hypertension 76. A secondary analysis of data collected from the Third National Health and Nutrition Survey revealed that adults aged 20-59 years who reported low levels of physical activity were more likely to feel “tired” or “exhausted” despite a usual night's sleep 64. In healthy, physically fit individuals who were exercising approximately six hours per week, cessation of usual exercise routines resulted in increased levels of fatigue 77
There are several etiological mechanisms that might explain the relationship between physical activity and fatigue in individuals with type 2 diabetes. Regular physical activity, especially vigorous physical activity, has been shown to improve aerobic capacity and muscle mass, enhance metabolic substrate use for energy, and improve mood. It has been noted that individuals with diabetes engage in low levels of physical activity 78-82, which may lead to reductions in aerobic capacity.
The Effects of Fatigue in People with Diabetes
Fatigue was among the top four symptoms found to interfere with self-reported quality of life in women with type 2 diabetes who rated their health poorer than women without symptoms 83. In children with type 1 diabetes, self-reported fatigue was comparable to fatigue in children with cancer and significantly higher than in healthy, age-matched controls 84.
Qualitative research has been the primary source of recurring themes about the deleterious effects of fatigue in adults with diabetes 85-90. For example, African-American women with type 2 diabetes participating in a qualitative study of problem-solving in diabetes self-management noted that fatigue limited their ability to exercise 85. Phrases such as “overwhelming tiredness,” “sleeping through most days,” and “I can't do what I want, I feel weak…I am lonely” were expressed by women with type 2 diabetes living in Australia who participated in a qualitative study about the experience of living with a chronic illness 86. Fatigue was among the predominant concerns in the Australian women, who also reported that they had limited their social activities and/or confined their activities to only those deemed necessary 86. In a focus group about the barriers to diabetes self-management, feelings of being betrayed by the body were common among rural-dwelling African American adults with type 2 diabetes. A male participant in the focus group described himself as “so tired it was like my muscles weren't working properly” 88. In community-dwelling adults with type 2 diabetes, both sleepiness and being tired were associated with lack of motivation and ability to perform such diabetes self-care activities as preparing healthy meals, participating in exercise, and monitoring blood glucose levels 90. In all of the above-referenced studies, the participants noted feeling that they were no longer able to participate in activities and attributed their fatigue to their diabetes 85-89.
Such findings suggest that fatigue has far-reaching and serious consequences for patients with diabetes because it is largely a self-managed disease, requiring both physical and mental energy to accomplish the daily self-management tasks necessary for maintaining optimal health.
The Need for Studies on Fatigue in Diabetes
A recent review of diabetes randomized clinical trials revealed that only 18% of studies included measurement of patient-important outcomes, such as symptoms or health-related quality of life in their study designs 91. One study that did include such patient-important outcomes provided us with some of the most directly applicable findings on this subject to date. Skelly reported that symptom-focused education improved self-management practices and HbA1c levels. The subjects also had higher perceived quality of life and reduced symptom distress 92. Further studies such as this can only increase the much-needed understanding of fatigue in diabetes.
A Working Model for Research in Fatigue in Diabetes
Based on the review of the above studies related to fatigue in diabetes and the identified need for more studies and a more directed approach, we propose a model (Figure 1) for more focused research on this important symptom and its meaning for people with diabetes. Fatigue in people with diabetes is likely multidimensional, incorporating any combination of physiological phenomena such as altered blood glucose levels and diabetes complications; psychological phenomena, such as depression or diabetes-related emotional distress; or lifestyle factors, such as being overweight or physically inactive.
Conclusion
Patients with diabetes who neglect their health because of symptoms such as fatigue put themselves at greater risk for both the acute and chronic complications associated with diabetes. The successful self-management of diabetes requires physical, psychological and cognitive tasks (e.g., exercise participation, management of hypoglycemia and hyperglycemia, and calculation of insulin doses) that are likely to be affected by fatigue. Fatigue in diabetes is likely caused from the interplay of physiological, psychological, and lifestyle-related factors. Fatigue is also likely to be both a cause and a result of poor diabetes self-management. Diabetes and its related effects represent a potential archetype for fatigue, with abundant potential for future research.
Acknowledgments
This research was funded in part by the National Institutes of Health/National Institute for Nursing Research F31 NR009751. The authors thank Kevin Grandfield for editorial assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bartley SH. What do we call fatigue. In: Simonson E, Weiser PC, editors. Psychological and Physiological Aspectss of Work and Fatigue. Springfield, IL: Charles C. Thomas; 1976. pp. 409–414. [Google Scholar]
- 2.Winningham ML, Nail LM, Burke MB, et al. Fatigue and the cancer experience: The state of the knowledge. Oncol Nurs Forum. 1994;21(1):23–36. [PubMed] [Google Scholar]
- 3.Wessely S. The epidemiology of chronic fatigue syndrome. Epidemiol Psichiatr Soc. 1998;7(1):10–24. doi: 10.1017/s1121189x00007089. [DOI] [PubMed] [Google Scholar]
- 4.Aistars J. Fatigue in the cancer patient: A conceptual approach to a clinical problem. Oncol Nurs Forum. 1987;14(6):25–30. [PubMed] [Google Scholar]
- 5.Ream E, Richardson A. Fatigue: A concept analysis. Int J Nurs Stud. 1996;33(5):519–529. doi: 10.1016/0020-7489(96)00004-1. [DOI] [PubMed] [Google Scholar]
- 6.NANDA. Nursing Diagnoses: Definitions and Classification 2001-2002. Philadelphia: North American Nursing Diagnosis Association; 2001. [Google Scholar]
- 7.Aaronson LS, Teel CS, Cassmeyer V, et al. Defining and measuring fatigue. Image: the journal of nursing scholarship. 1999;31(1):45–50. doi: 10.1111/j.1547-5069.1999.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 8.Hart LK, Freel MI. Fatigue. In: Norris CM, editor. Concept Clarification in Nursing. Rockville, MD: Aspen Systems Corporation; 1982. [Google Scholar]
- 9.Lewis G, Wessely S. The epidemiology of fatigue: More questions than answers. J Epidemiol Community Health. 1992;46(2):92–97. doi: 10.1136/jech.46.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rose L, Pugh LC, Lears K, Gordon DL. The fatigue experience: Persons with HIV infection. J Adv Nurs. 1998;28(2):295–304. doi: 10.1046/j.1365-2648.1998.00789.x. [DOI] [PubMed] [Google Scholar]
- 11.Trendall J. Concept analysis: Chronic fatigue. J Adv Nurs. 2000;32(5):1126–1131. doi: 10.1046/j.1365-2648.2000.01583.x. [DOI] [PubMed] [Google Scholar]
- 12.Magnusson K, Moller A, Ekman T, Wallgren A. A qualitative study to explore the experience of fatigue in cancer patients. Eur J Cancer Care (Engl) 1999;8(4):224–232. doi: 10.1046/j.1365-2354.1999.00168.x. [DOI] [PubMed] [Google Scholar]
- 13.Mosso A. Fatigue. London: Swan Sonnenschein & Company; 1904. [Google Scholar]
- 14.Kant IJ, Bultmann U, Schroer KA, Beurskens AJ, Van Amelsvoort LG, Swaen GM. An epidemiological approach to study fatigue in the working population: The maastricht cohort study. Occup Environ Med. 2003;60(Suppl 1):i32–9. doi: 10.1136/oem.60.suppl_1.i32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ream E, Richardson A. Fatigue in patients with cancer and chronic obstructive airways disease: A phenomenological enquiry. Int J Nurs Stud. 1997;34(1):44–53. doi: 10.1016/s0020-7489(96)00032-6. [DOI] [PubMed] [Google Scholar]
- 16.McArdle WD, Katch FI, Katch VL. Neural control of human movement. In: McArdle WD, editor. Exercise Physiology. Philadelphia: Lippincott, Williams and Wilkins; 2001. [Google Scholar]
- 17.Chaudhuri A, Behan PO. Fatigue and basal ganglia. J Neurol Sci. 2000;179(S 1-2):34–42. doi: 10.1016/s0022-510x(00)00411-1. [DOI] [PubMed] [Google Scholar]
- 18.Drayer RA, Mulsant BH, Lenze EJ, et al. Somatic symptoms of depression in elderly patients with medical comorbidities. Int J Geriatr Psychiatry. 2005;20(10):973–982. doi: 10.1002/gps.1389. [DOI] [PubMed] [Google Scholar]
- 19.Sugahara H, Akamine M, Kondo T, et al. Somatic symptoms most often associated with depression in an urban hospital medical setting in japan. Psychiatry Res. 2004;128(3):305–311. doi: 10.1016/j.psychres.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Lavidor M, Weller A, Babkoff H. Multidimensional fatigue, somatic symptoms and depression. Br J Health Psychol. 2002;7(Pt 1):67–75. doi: 10.1348/135910702169367. [DOI] [PubMed] [Google Scholar]
- 21.Vaccarino AL, Sills TL, Evans KR, Kalali AH. Prevalence and association of somatic symptoms in patients with major depressive disorder. J Affect Disord. 2008 doi: 10.1016/j.jad.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Price RK. Symptoms in the community. prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153(21):2474–2480. [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- 24.Wijeratne C, Hickie I, Brodaty H. The characteristics of fatigue in an older primary care sample. J Psychosom Res. 2007;62(2):153–158. doi: 10.1016/j.jpsychores.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Leone SS, Huibers MJ, Knottnerus JA, Kant IJ. Similarities, overlap and differences between burnout and prolonged fatigue in the working population. QJM. 2007;100(10):617–627. doi: 10.1093/qjmed/hcm073. [DOI] [PubMed] [Google Scholar]
- 26.Nijrolder I, van der Windt DA, van der Horst HE. Prognosis of fatigue and functioning in primary care: A 1-year follow-up study. Ann Fam Med. 2008;6(6):519–527. doi: 10.1370/afm.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Craig A, Tran Y, Wijesuriya N, Boord P. A controlled investigation into the psychological determinants of fatigue. Biol Psychol. 2006;72(1):78–87. doi: 10.1016/j.biopsycho.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Stewart ST, Woodward RM, Rosen AB, Cutler DM. The impact of symptoms and impairments on overall health in US national health data. Med Care. 2008;46(9):954–962. doi: 10.1097/MLR.0b013e318179199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Avlund K, Mehlsen MY, Thomsen DK, Viidik A, Zachariae R. Physical functioning and use of health services in a young and old sample. the influence of fatigue. Dan Med Bull. 2008;55(3):147–151. [PubMed] [Google Scholar]
- 30.Morsch CM, Goncalves LF, Barros E. Health-related quality of life among haemodialysis patients--relationship with clinical indicators, morbidity and mortality. J Clin Nurs. 2006;15(4):498–504. doi: 10.1111/j.1365-2702.2006.01349.x. [DOI] [PubMed] [Google Scholar]
- 31.Weijman I, Kant I, Swaen GM, et al. Diabetes, employment and fatigue-related complaints: A comparison between diabetic employees, “healthy” employees, and employees with other chronic diseases. J Occup Environ Med. 2004;46(8):828–836. doi: 10.1097/01.jom.0000135605.62330.ca. [DOI] [PubMed] [Google Scholar]
- 32.Rijken PM, Dekker J, Dekker E, et al. Clinical and functional correlates of foot pain in diabetic patients. Disabil Rehabil. 1998;20(9):330–336. doi: 10.3109/09638289809166090. [DOI] [PubMed] [Google Scholar]
- 33.Warren RE, Deary IJ, Frier BM. The symptoms of hyperglycaemia in people with insulin-treated diabetes: Classification using principal components analysis. Diabetes Metab Res. 2003;19(5):408–414. doi: 10.1002/dmrr.396. [DOI] [PubMed] [Google Scholar]
- 34.Sommerfield AJ, Deary IJ, Frier BM. Acute hyperglycemia alters mood state and impairs cognitive performance in people with type 2 diabetes. Diabetes Care. 2004;27(10):2335–2340. doi: 10.2337/diacare.27.10.2335. [DOI] [PubMed] [Google Scholar]
- 35.Drivsholm T, de Fine Olivarius N, Nielsen AB, Siersma V. Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycaemia, blood pressure and weight. Diabetologia. 2005 doi: 10.1007/s00125-004-1625-y. [DOI] [PubMed] [Google Scholar]
- 36.Bulpitt CJ, Palmer AJ, Battersby C, Fletcher AE. Association of symptoms of type 2 diabetic patients with severity of disease, obesity, and blood pressure. Diabetes Care. 1998;21(1):111–115. doi: 10.2337/diacare.21.1.111. [DOI] [PubMed] [Google Scholar]
- 37.King P, Kong MF, Parkin H, Macdonald IA, Tattersall RB. Well-being, cerebral function, and physical fatigue after nocturnal hypoglycemia in IDDM. Diabetes Care. 1998;21(3):341–345. doi: 10.2337/diacare.21.3.341. [DOI] [PubMed] [Google Scholar]
- 38.Van der Does FE, De Neeling JN, Snoek FJ, et al. Symptoms and well-being in relation to glycemic control in type II diabetes. Diabetes Care. 1996;19(3):204–210. doi: 10.2337/diacare.19.3.204. [DOI] [PubMed] [Google Scholar]
- 39.Grootenhuis PA, Snoek FJ, Heine RJ, Bouter LM. Development of a type 2 diabetes symptom checklist: A measure of symptom severity. Diabet Med. 1994;11(3):253–261. doi: 10.1111/j.1464-5491.1994.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 40.McNair D, Heuchert JW. Profile of mood states: Technical update. Toronta, Canada: Multi-Health Systems Inc.; 2003. [Google Scholar]
- 41.de Sonnaville JJ, Snoek FJ, Colly LP, Deville W, Wijkel D, Heine RJ. Well-being and symptoms in relation to insulin therapy in type 2 diabetes. Diabetes Care. 1998;21(6):919–924. doi: 10.2337/diacare.21.6.919. [DOI] [PubMed] [Google Scholar]
- 42.Cuellar NG, Ratcliffe SJ. A comparison of glycemic control, sleep, fatigue, and depression in type 2 diabetes with and without restless legs syndrome. J Clin Sleep Med. 2008;4(1):50–56. [PMC free article] [PubMed] [Google Scholar]
- 43.Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295(14):1681–1687. doi: 10.1001/jama.295.14.1681. [DOI] [PubMed] [Google Scholar]
- 44.Kennedy G, Spence VA, McLaren M, Hill A, Underwood C, Belch JJ. Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms. Free Radic Biol Med. 2005;39(5):584–589. doi: 10.1016/j.freeradbiomed.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 45.American Diabetes Association. Diabetes statistics [Google Scholar]
- 46.Deray G, Heurtier A, Grimaldi A, Launay Vacher V, Isnard Bagnis C. Anemia and diabetes. Am J Nephrol. 2004;24(5):522–526. doi: 10.1159/000081058. [DOI] [PubMed] [Google Scholar]
- 47.Thomas MC, MacIsaac RJ, Tsalamandris C, Power D, Jerums G. Unrecognized anemia in patients with diabetes: A cross-sectional survey. Diabetes Care. 2003;26(4):1164–1169. doi: 10.2337/diacare.26.4.1164. [DOI] [PubMed] [Google Scholar]
- 48.Weijman I, Ros WJ, Rutten GE, Schaufeli WB, Schabracq MJ, Winnubst JA. Fatigue in employees with diabetes: Its relation with work characteristics and diabetes related burden. Occup Environ Med. 2003;60(Suppl 1):i93–8. doi: 10.1136/oem.60.suppl_1.i93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rubin RR. Dealing with “diabetes overwhelmus”. [9/10/2008]; http/www.diabetesselfmanagement.com.
- 50.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 51.Polonsky WH. Emotional and quality-of-life aspects of diabetes management. Curr Diab Rep. 2002;2(2):153–159. doi: 10.1007/s11892-002-0075-5. [DOI] [PubMed] [Google Scholar]
- 52.Polonsky WH. Diabetes Burnout : What to do when You can't Take it Anymore. Alexandria, Va.: American Diabetes Association; 1999. [Google Scholar]
- 53.Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 54.Casalenuovo GA. Fatigue in diabetes mellitus: Testing a middle range theory of well-being derived from neuman's theory of optimal client system stability and the neuman systems model. knoxville, TN: University of TennesseeEditor; 2002. [Google Scholar]
- 55.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 56.Von Korff M, Katon W, Lin EH, et al. Work disability among individuals with diabetes. Diabetes Care. 2005;28(6):1326–1332. doi: 10.2337/diacare.28.6.1326. [DOI] [PubMed] [Google Scholar]
- 57.American Diabetes Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 58.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 59.Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Jonge P, Roy JF, Saz P, Marcos G, Lobo A, ZARADEMP Investigators Prevalent and incident depression in community-dwelling elderly persons with diabetes mellitus: Results from the ZARADEMP project. Diabetologia. 2006;49(11):2627–2633. doi: 10.1007/s00125-006-0442-x. [DOI] [PubMed] [Google Scholar]
- 61.Golden SH, Williams JE, Ford DE, et al. Depressive symptoms and the risk of type 2 diabetes: The atherosclerosis risk in communities study. Diabetes Care. 2004;27(2):429–435. doi: 10.2337/diacare.27.2.429. [DOI] [PubMed] [Google Scholar]
- 62.Palinkas LA, Lee PP, Barrett-Connor E. A prospective study of type 2 diabetes and depressive symptoms in the elderly: The rancho bernardo study. Diabet Med. 2004;21(11):1185–1191. doi: 10.1111/j.1464-5491.2004.01315.x. [DOI] [PubMed] [Google Scholar]
- 63.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31 Suppl 1:S55–60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- 64.Resnick HE, Carter EA, Aloia M, Phillips B. Cross-sectional relationship of reported fatigue to obesity, diet, and physical activity: Results from the third national health and nutritional examination survey. JCSM. 2006;2(2):163–169. [PubMed] [Google Scholar]
- 65.Theorell-Haglow J, Lindberg E, Janson C. What are the important risk factors for daytime sleepiness and fatigue in women? Sleep. 2006;29(6):751–757. doi: 10.1093/sleep/29.6.751. [DOI] [PubMed] [Google Scholar]
- 66.Lim W, Hong S, Nelesen R, Dimsdale JE. The association of obesity, cytokine levels, and depressive symptoms with diverse measures of fatigue in healthy subjects. Arch Intern Med. 2005;165(8):910–915. doi: 10.1001/archinte.165.8.910. [DOI] [PubMed] [Google Scholar]
- 67.Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004;27(3):813–23. doi: 10.2337/diacare.27.3.813. 2004 Mar. [DOI] [PubMed] [Google Scholar]
- 68.Miller MA, Cappuccio FP. Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol. 2007;5(2):93–102. doi: 10.2174/157016107780368280. [DOI] [PubMed] [Google Scholar]
- 69.Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: The role of the stress system and cytokines. Ann N Y Acad Sci. 2006;1083:329–344. doi: 10.1196/annals.1367.023. [DOI] [PubMed] [Google Scholar]
- 70.Puetz TW. Physical activity and feelings of energy and fatigue: Epidemiological evidence. Sports Med. 2006;36(9):767–780. doi: 10.2165/00007256-200636090-00004. [DOI] [PubMed] [Google Scholar]
- 71.Puetz TW, Beasman KM, O'Connor PJ. The effect of cardiac rehabilitation exercise programs on feelings of energy and fatigue: A meta-analysis of research from 1945 to 2005. Eur J Cardiovasc Prev Rehabil. 2006;13(6):886–893. doi: 10.1097/01.hjr.0000230102.55653.0b. [DOI] [PubMed] [Google Scholar]
- 72.Puetz TW, O'Connor PJ, Dishman RK. Effects of chronic exercise on feelings of energy and fatigue: A quantitative synthesis. Psychol Bull. 2006;132(6):866–876. doi: 10.1037/0033-2909.132.6.866. [DOI] [PubMed] [Google Scholar]
- 73.O'Connor PJ, Puetz TW. Chronic physical activity and feelings of energy and fatigue. Med Sci Sports Exerc. 2005;37(2):299–305. doi: 10.1249/01.mss.0000152802.89770.cf. [DOI] [PubMed] [Google Scholar]
- 74.Mock V, Frangakis C, Davidson NE, et al. Exercise manages fatigue during breast cancer treatment: A randomized controlled trial. Psychooncology. 2004 doi: 10.1002/pon.863. [DOI] [PubMed] [Google Scholar]
- 75.Neuberger GB, Press AN, Lindsley HB, et al. Effects of exercise on fatigue, aerobic fitness, and disease activity measures in persons with rheumatoid arthritis. Res Nurs Health. 1997:195–204. doi: 10.1002/(sici)1098-240x(199706)20:3<195::aid-nur3>3.0.co;2-d. 1997 Jun. [DOI] [PubMed] [Google Scholar]
- 76.Stewart AL, Hays RD, Wells KB, Rogers WH, Spritzer KL, Greenfield S. Long-term functioning and well-being outcomes associated with physical activity and exercise in patients with chronic conditions in the medical outcomes study. J Clin Epidemiol. 1994;47(7):719–730. doi: 10.1016/0895-4356(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 77.Glass JM, Lyden AK, Petzke F, et al. The effect of brief exercise cessation on pain, fatigue, and mood symptom development in healthy, fit individuals. J Psychosom Res. 2004;57(4):391–398. doi: 10.1016/j.jpsychores.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 78.Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW. Physical activity in u.s. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care. 2007;30(2):203–209. doi: 10.2337/dc06-1128. [DOI] [PubMed] [Google Scholar]
- 79.Lim K, Taylor L. Factors associated with physical activity among older people--a population-based study. Prev Med. 2005;40(1):33–40. doi: 10.1016/j.ypmed.2004.04.046. [DOI] [PubMed] [Google Scholar]
- 80.Hays LM, Clark DO. Correlates of physical activity in a sample of older adults with type 2 diabetes. Diabetes Care. 1999;22(5):706–712. doi: 10.2337/diacare.22.5.706. [DOI] [PubMed] [Google Scholar]
- 81.Wood FG. Leisure time activity of mexican americans with diabetes. J Adv Nurs. 2004;45(2):190–196. doi: 10.1046/j.1365-2648.2003.02880.x. [DOI] [PubMed] [Google Scholar]
- 82.Ford ES, Herman WH. Leisure-time physical activity patterns in the U.S. diabetic population. findings from the 1990 national health interview survey--health promotion and disease prevention supplement. Diabetes Care. 1995;18(1):27–33. doi: 10.2337/diacare.18.1.27. [DOI] [PubMed] [Google Scholar]
- 83.Stover JC, Skelly AH, Holditch-Davis D, Dunn PF. Perceptions of health and their relationship to symptoms in african american women with type 2 diabetes. Appl Nurs Res. 2001;14(2):72–80. doi: 10.1053/apnr.2001.22372. [DOI] [PubMed] [Google Scholar]
- 84.Varni JW, Limbers CA, Bryant WP, Wilson DP. The PedsQLtrade mark multidimensional fatigue scale in type 1 diabetes: Feasibility, reliability, and validity. Pediatr Diabetes. 2008 doi: 10.1111/j.1399-5448.2008.00482.x. [DOI] [PubMed] [Google Scholar]
- 85.Hill-Briggs F, Cooper DC, Loman K, Brancati FL, Cooper LA. A qualitative study of problem solving and diabetes control in type 2 diabetes self-management. Diabetes Educ. 2003;29(6):1018–1028. doi: 10.1177/014572170302900612. [DOI] [PubMed] [Google Scholar]
- 86.Koch T, Kralik D, Sonnack D. Women living with type II diabetes: The intrusion of illness. J Clin Nurs. 1999;8(6):712–722. doi: 10.1046/j.1365-2702.1999.00320.x. [DOI] [PubMed] [Google Scholar]
- 87.Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among african-american women: Spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23(7):928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 88.Wenzel J, Utz SW, Steeves R, Hinton I, Jones R. “Plenty of sickness” descriptions by african americans living in rursal areas with type 2 diabetes. Diabetes Educ. 2005;31(1):98–107. doi: 10.1177/0145721704273242. [DOI] [PubMed] [Google Scholar]
- 89.Samuel-Hodge CD, Skelly AH, Headen S, Carter-Edwards L. Familial roles of older african-american women with type 2 diabetes: Testing of a new multiple caregiving measure. Ethn Dis. 2005;15(3):436–443. [PubMed] [Google Scholar]
- 90.Chasens ER, Olshansky E. Daytime sleepiness, diabetes, and psychological well-being. Issues Ment Health Nurs. 2008;29(10):1134–1150. doi: 10.1080/01612840802319878. [DOI] [PubMed] [Google Scholar]
- 91.Gandhi GY, Murad MH, Fujiyoshi A, et al. Patient-important outcomes in registered diabetes trials. JAMA. 2008;299(21):2543–2549. doi: 10.1001/jama.299.21.2543. [DOI] [PubMed] [Google Scholar]
- 92.Skelly AH, Carlson JR, Leeman J, Holditch-Davis D, Soward AC. Symptom-focused management for african american women with type 2 diabetes: A pilot study. Appl Nurs Res. 2005;18(4):213–220. doi: 10.1016/j.apnr.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 93.International Diabetes Federation. Diabetes atlas. [08/05, 2009]; http://www.eatlas.idf.org/