Abstract
Background
We evaluated the burden of sexual- or injection drug use (IDU)-related infections in male prisoners in Karachi, Pakistan.
Methods
We administered a structured questionnaire in a cross-sectional survey of 365 randomly selected imprisoned men. We analyzed blood for human immunodeficiency virus (HIV) and Hepatitis B and C by ELISA, and for syphilis by rapid plasma reagin and Treponema pallidum hemagglutination assay confirmation. Subjects with possible tuberculosis (WHO criteria) provided sputum samples for an acid fast bacillus smear and culture.
Results
Prevalence of tuberculosis was 2.2% (95%CI: 0.71, 3.8). HIV infected 2.0% (95%CI: 0.55, 3.4) of 357 randomly selected prisoners (8 refused to give blood), with confirmed syphilis in 8.9% (95%CI: 6.0, 11.8), hepatitis B virus in 5.9% (95%CI: 3.5, 8.3), and hepatitis C virus in 15.2% (95%CI: 11.7, 18.8). By self-report, 59.0% had used any illicit drugs, among whom 11.8% (95%CI: 8.5, 15.0) had injected drugs. The median length of stay in the prison had been 3.2 (range 1-72) months.
Conclusions
All four infections were prevalent among the prisoners in Pakistan. Prisons are excellent venues for infectious disease screening and intervention given conditions of poverty and drug addiction. Collaboration with community-based health providers is vital for post-discharge planning.
Keywords: Infectious disease, substance abuse, prison, epidemiology, Pakistan
INTRODUCTION
Prisons are incubators for infectious diseases, yet are readily accessible for screening and intervention[1]. They provide a high-yield opportunity for early disease detection, intervention, and treatment that benefits not only prisoners and prison employees, but also family members and the general population due to high turnover of prisoners [1, 2]. About 9.25 million people are held in prisons worldwide, with 30 million inmates moving from prison to the community and/or back again each year[3, 4]. Prisons are typically overcrowded, offer limited access to health care, and harbor high rates of airborne and blood-borne diseases [1, 5]. Inmates often come from marginalized populations, such as injecting drug users (IDU) or persons with high risk sexual behaviors (including sex workers), who are already at an increased risk for these infections [5].
Available global data suggest a high prevalence and transmission of infectious diseases, such as tuberculosis (TB), human immunodeficiency virus (HIV), syphilis, hepatitis B virus (HBV) and hepatitis C virus (HCV) in prisons[6-9] [10-14]. Yet few research studies in Pakistan have focused on disease detection, treatment, community linkages, health education, and prevention for prison inmates[15, 16]. Pakistan is the eighth most heavily burdened country for TB cases in the world, with an estimated prevalence rate of 263 active cases per 100,000 in 2006[17]. Around 181 new cases per 100,000 are estimated to be added each year to the existing pool of TB-infected persons in Pakistan[17]. HIV patients are especially vulnerable to tuberculosis reactivation or acquisition. Tuberculosis case rates are thought to be high in Pakistani prisons, but few representative surveys have been done[18-20].
In 2003, an outbreak of HIV infection was reported among IDUs in a prison in the city of Larkana in Sindh Province, Pakistan[21, 22]. Subsequently, there has been a sudden rise in the prevalence of HIV among IDUs in other major cities. Pakistan’s largest city, Karachi, is also located in Sindh Province where HIV seroprevalence rose in IDUs from 0.4% in 2004 to 30% in 2007[22-24]. In the round III integrated behavioral and biological surveillance report, 2008 HIV prevalence for IDUs in Karachi was 23.1%[25]. Similar trends have been seen among IDUs in other major cities of Pakistan with documented increases in IDU seroprevalence to 30% in Hyderabad and 50% in Sargodha[24]. HIV is now prevalent among commercial sex workers, especially men who have sex with men (MSM) and Hijras (traditional transvestites). HIV seroprevalence in 2007 was 1.8% among Hijras and 1.5% among other MSM according to surveys conducted in 12 cities of Pakistan[24]. An increase in sexually transmitted disease (STD) prevalence has been noted among high-risk populations, especially IDUs, Hijras, and other male sex workers in Karachi and Lahore in 2005[26, 27]. Prevalence of hepatitis B and C virus in the general and high-risk population especially among IDUs is also increasing at an alarming rate[28, 29]. The number of opiate users in Pakistan was estimated in 2006 to be 0.7% (628,000) of the adult population; among these, 77% are estimated to be heroin users (484,000) and approximately 14% of heroin users are IDUs (125,000)[30].
The Sindh AIDS Control Program has developed service delivery packages for prison inmates and drug users for the prevention of HIV/AIDS in major prisons of Sindh province, including District Jail Malir[31]. However, there is no provision for screening for TB, HIV, STD, or hepatitis, nor are effective control measures in place. The objective of our study was to assess the prevalence and risk factors of TB, HIV/AIDS, syphilis, HBV, and HCV among incarcerated men in Karachi, the first such systematic study in Pakistan. We also sought to upgrade care within the prison, as well as to bridge discharged prisoners to community services.
METHODS
Study Site & Population
We conducted a cross sectional study in District Jail Malir, Karachi, Pakistan from December 2007 to January 2008. This facility is both a jail and a prison and it serves as the principal incarceration venue for adult males with illicit drug allegations, as well as for men accused of many other crimes. The maximum capacity of District Jail Malir is 893 but there are typically about 3,000 inmates[32]. The study protocol was approved by the Vanderbilt University Institutional Review Board (IRB; Nashville, TN, USA) after a special review by the Office of Human Research Protection (OHRP: Washington, D.C., USA) and the Bridge Consultants Foundation IRB (Karachi, Pakistan).
Sampling methods, study design, and sample size
District Jail Malir consists of 26 barracks of varying sizes, plus a hospital barrack; prisoner populations range from 2 to 265 inmates per barrack. We assumed that prevalence of disease would differ between prisoners placed in the hospital barrack compared to those in the other barracks. Hence we randomly sampled inmates using stratified sampling across two strata: the 26 non-hospital barracks and the 1 hospital barrack. Sampling within the non-hospital barracks stratum was done proportional to the number of inmates in each barrack. The hospital barrack was smaller in prisoner population than the average barrack and we sampled 50% of the prisoners in the hospital to obtain more precise prevalence estimates. A sample size of 350 was needed to estimate prevalence with no greater than a 5% margin of error for all diseases. Assuming a <10% refusal rate, random number tables were used for sampling 385 subjects.
Data Collection (Questionnaire)
Jail health care staff and study team were trained in data collection techniques, laboratory techniques, clinical diagnosis for tuberculosis, and ethical considerations of privacy and confidentiality. All consenting participants were interviewed by study doctors using a structured questionnaire on tuberculosis, HIV, syphilis, hepatitis B and C virus history, sociodemographic, and history of sexual behaviors, drug use, and previous incarcerations.
Recruitment Process and Informed Consent
A list containing each prisoner’s identity number and corresponding barrack was received from the prison staff. Study participants were selected according to our pregenerated randomized number list. At the prison clinic, each selected prisoner was assigned an interviewer who was not affiliated with the prison and reviewed the consent form (many prisoners were illiterate), insuring privacy. Prisoners had full authority to accept or refuse to take part in the study; each participant was explained that his acceptance or refusal to take part in the study would not affect their incarceration nor their possibility for parole. Only after the written consent was signed (all prisoners could sign their names), the questionnaire was administered by the interviewing physician.
Sputum collection for tuberculosis
Sputum samples were collected from participants suspected of having TB as per WHO screening criteria: (1) clinical symptoms such as cough >2 weeks, sputum production, and/or weight loss; (2) previous TB or treatment in the past 5 years; (3) body mass index <20 kg/m2; and/or (4) known HIV infection[33]. Three sputum samples were collected from men with any of these four criteria and examined using the Ziehl-Neelsen Carbolfuchsin (ZNCF) method, direct and concentrated sputum smears, and smear cultures using Lowenstein-Jensen (LJ) media. We defined a patient as positive for TB if they had acid-fast bacilli on smear and culture confirmation.
Serological Testing
A 5 mL blood sample was collected from willing participants for HIV, syphilis, HBV and HCV. Specimens were tested at the Sindh Institute of Urology and Transplantation (SIUT) as follows: syphilis by rapid plasma regain (RPR™, Randox, Crumlin, UK) and Treponema pallidum hemagglutination assay (TPHA™, Randox, Crumlin, UK) confirmation; antibodies for HBV by HBsAg ELISA (AXSYM™, Abbott, Chicago, IL, USA); and for HCV Ab by ELISA (Version 3.0 AXYSM™, Abbott, Chicago, IL USA). HIV antibody tests were conducted at the Sindh AIDS Control Program by HIV-1/2 ELISA (Enzygnost™, Dade Behring, Marburg, Germany; Vironostika™ or, BioMérieux, Boxtel, Netherlands). Positive HIV cases were confirmed by Western blot (Genlab Diagnostic™, Redwood City, CA, USA).
Care and Policy Intervention
Active TB cases were registered with the prison clinic for daily TB treatment. Treatment was continued outside the prison if the prisoner was released during treatment through an arrangement with a local non-government organization that has continued beyond the end of the study. HIV and syphilis-positive cases were registered with the prison voluntary counseling and testing center and followed up by Sindh AIDS Control Programme. RPR+/TPHA+ cases were treated with Benzathine penicillin in the prison, while hepatitis cases were referred to clinics at the Dow University of Health Sciences.
Statistical Analysis
Stratum-specific and overall prevalence estimates of TB, HIV, syphilis, HBV, and HCV were computed. The Wilson confidence intervals (95%CI) were calculated for the stratum-specific prevalence estimates; 95%CI using unbiased estimators of the true variance for stratified simple random samples were calculated for the overall prevalence estimates. The relationship between sociodemographic variables and a positive screening test for HIV, HBV, and/or HCV or a positive screening for syphilis were assessed using multivariable logistic regression models.
RESULTS
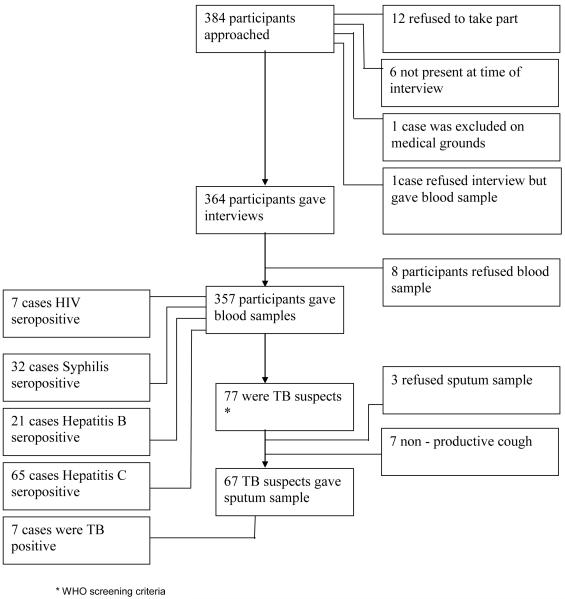
From December 2007 to January 2008, we approached 384 prisoners for enrollment in the study. Ninety-five percent (n=365) of approached prisoners provided informed consent, of whom 364 (99.7%) agreed to the interview and 357 (97.8%) agreed to a blood test. One prisoner refusing the interview agreed to the blood test (Figure 1).
Figure 1. Flow Chart of the Data Collection Process in District Jail Malir.
Sociodemographic Profile
The median age of the respondents was 27 years (range 18-81) and 50% (182) of the inmates were married (Table 1). No formal education was reported by 44% (158/361), 21% (75/361) had no more than primary school education, and 17% (63/361) had some or all of a middle school education. The monthly income of inmates at the time of arrest was <US$83 for 39% (129/329), US$83 to $333 for 50% (166/329), and >US$333 for 10% (34/329). Forty-three percent (158/361) of inmates were from Karachi, 6.6% (24/361) from Sindh province excluding Karachi, 21% (77/361) from Punjab province, 13.5% (49/361) from the Northwest Frontier Province (NWFP), 3.3% (12/361) from Baluchistan Province and 0.6% (2/361) from Azad Kashmir (Table 1). Eleven percent were foreign nationals from nine countries on three continents.
Table 1. Sociodemographic Profile and Sexual, Drug & Infectious Disease History of male prison population sample (N=364).
| Demographics | ||
|---|---|---|
| Age in years median (range) (N=364)a | 27(18-81) | |
| Length of prison stay in months Median (Range) (N=361)b | 3.2 (1-72) | |
| Region of Origin (N=362)b | N | % |
| Karachi | 158 | 43.4% |
| Sindh (Excluding Karachi) | 24 | 6.6% |
| Punjab | 77 | 21.3% |
| Baluchistan | 12 | 3.3% |
| North West Frontier Province | 49 | 13.5% |
| Azad Kashmir | 2 | 0.6% |
| Foreigners c | 40 | 11.0% |
| Prior prison term (n=364) | 150 | 41% |
| Marital status (n=364) | ||
| Married | 182 | 50% |
| Single | 168 | 46% |
| Separated, divorced or widowed | 14 | 4% |
| Educational Level (n=361) b | ||
| No Formal Education | 158 | 44% |
| Some or all Primary or Middle | 138 | 38% |
| Some or all post middle school | 64 | 18% |
| Islamic Religious Studies | 1 | 0.3% |
| Monthly Income equivalent in US $ d (n=329) b | ||
| < 83 | 129 | 39% |
| 83-333 | 166 | 51% |
| >333 | 34 | 10% |
| Sexual History b | ||
| Ever paid for sex with a female (n=362) | 166 | 46% |
| Condom use during last paid sex with a female (n=166) | 41 | 25% |
| Ever paid for sex with a male (n=362) | 77 | 21% |
| Condom use during last paid sex with a male (n=77) | 7 | 9% |
| Ever received money or drugs for sex (n=362) | 19 | 5% |
| Drug History | ||
| Illicit drug use in past six months at the time of incarceration (n=364) | 215 | 59% |
| Injection drug use, % of all drug users (n=215) | 50 | 23% |
| Needle sharing, % of injecting drug users(n=50) | 23 | 46% |
| Length of drug use, median (range) | 214 | 7.3 (1-71) |
| Length of injection drug use, median (range) | 49 | 1 (1-12) |
| History of Infectious diseases | ||
| Prior Tuberculosis diagnosis (n=364) | 23 | 6% |
| History of Tuberculosis exposure in prisoners | ||
| with prior diagnosis (n=23) | 8 | 35% |
| Ever tested for HIV (n=364) | 41 | 11% |
| Prior HIV diagnosis (n=41) | 1 | 2% |
| Prior Syphilis diagnosis (n=364) | 26 | 7% |
| Prior Hepatitis B /Hepatitis C Diagnosis e (n=364) | 16 | 4% |
| Prior knowledge of HIV/AIDS (n=364) | 242 | 66% |
Note
One of 365 prisoners (0.3%) refused the questionnaire, but provided a blood sample
Refusals to answer included: 3 for length of prison stay, 3 for education, 32 for income, 2 for original home, 2 for sexual history
India (19), Afghanistan (1), Bangladesh (4), Iran (3), Ukraine (1), United Arab Emirates (2), Myanmar (1), Uzbekistan (1), and Nigeria (8)
January 2008 exchange rate of 60 Pakistani rupees per US$1
Patients could not distinguish from hepatitis B and C, referring to both “hepatitsi”
Sexual and drug histories
By self report, 45% (166/362) of the participants had paid for sex with a female, 25% (41/166) of whom used a condom during the last paid sex (Table 1); 21% (77/362) of the total participants reported having paid for sex with a male, 9% (7/77) of whom used a condom during the last paid sex. Five percent (19/362) of the respondents reported having received money or drugs for sex at least once.
Almost 60% (215/363) of the participants gave a history of drug use excluding alcohol, of whom 11.8% (50/215; 95%CI: 8.5, 15.0) were IDUs. Of the IDUs, 46.0% (23/50) had shared a needle or syringe, 84.0% (42/50) had been previously incarcerated, and 49.0% (24/50) had a history of a surgery. The median duration of any kind of drug use was 7.3 years (range ≤1-71) and median duration of IDU was <1 year (range <1-12). Seventy-seven percent (280/364) of the study participants smoked cigarettes or used tobacco products and 52.0% (189/364) had a history of alcohol use.
Risk factors for infection
Twenty-five percent (91/364) of study participants had been skin tattooed, 21.0% (75/364) had body piercings, 39.0% (143/363) reported having a prior surgical procedure, and 28.0% (97/363) reported that their barbers did not use a new blade for a hair cut or shave. The median stay in the District Jail Malir was 3.2 months (range 1-72). Forty-one percent (150/364) of the participants had been incarcerated prior to the current incarceration.
Prevalence
Prevalence of active tuberculosis by sputum smear was 2.2% (95%CI 0.70%, 3.8%) (Table 2). HIV prevalence was 2.0% (95%CI: 0.6, 3.4). Syphilis was confirmed in 8.9% (95%CI: 6.0, 11.8), HBV Ag in 5.9% (95%CI: 3.5, 8.3), and HCV Ab in 15.2% (95%CI: 11.7, 18.8) of subjects.
Table 2. Prevalence of Tuberculosis, HIV, Syphilis, Hepatitis B & Hepatitis C in male prison population sample (N=357, 8 prisoners refused to give blood).
| Diseases | N | % | 95%CI |
|---|---|---|---|
| Tuberculosis sputum culture positive | 7 | 2.2% | (0.71%, 3.8%) |
| Hospitalized Inmates | 0 | 0% | (0%, 6.8%) |
| Non Hospitalized Inmates | 7 | 2.3 | (1.1%, 4.7%) |
| HIV, dual positive | 7 | 2.0% | (0.6%, 3.4%) |
| Hospitalized Inmates | 1 | 1.9% | (0.1%, 9.9%) |
| Non Hospitalized Inmates | 6 | 2.0% | (0.9%, 4.2%) |
| Syphilis, TPHA confirmed | 32 | 8.9% | (6.0%, 11.8%) |
| Hospitalized Inmates | 5 | 9.4% | (4.1%, 20.3%) |
| Non Hospitalized Inmates | 27 | 8.9% | (6.2%, 12.6%) |
| Hepatitis B, ELISA positive | 21 | 5.9% | (3.5%, 8.3%) |
| Hospitalized Inmates | 3 | 5.7% | (1.9%, 15.4%) |
| Non Hospitalized Inmates | 18 | 5.9% | (3.8%, 9.2%) |
| Hepatitis C, Elisa positive | 65 | 15.2% | (11.7%, 18.8%) |
| Hospitalized Inmates | 21 | 39.6% | (27.6%, 53.1%) |
| Non Hospitalized Inmates | 44 | 14.5% | (11.0%, 18.9%) |
Multivariable models
Multivariable logistic regression models elucidated the relationship between inmates’ characteristics and reported risk behaviors and positive status for the blood-borne and/or sexually transmitted infections studied. Two models were constructed, one for blood and needle-borne diseases (HIV, HBV, HCV) and one for syphilis. For both models, these covariates were included: age, marital status, IDU, paid heterosexual intercourse, paid homosexual intercourse, sex exchanged for drugs, blood transfusion, past surgery, and reporting if the barber used a clean blade. We did not construct a model for TB due to the comparatively low event frequency.
IDU (adjusted odds ratio (ORadj) =24.3; 95%CI 9.4, 63.2; P< 0.001) and a history of surgery (ORadj=2.4; 95%CI: 1.1, 5.5; P=0.03) were associated with a higher risk of HIV, HBV and/or HCV (Table 3a). Paying for heterosexual intercourse was associated with an increased risk of syphilis (ORadj=3.3; 95%CI: 1.2, 8.7; P=0.02) (Table 3b). Prevalence of HCV showed the only significant association (hospital versus barracks) of increased representation in the hospital barracks (unadjusted OR=4.3, 95% CI: 2.1, 8.4; P < 0.001).
Table 3a. Multivariable logistic regression model to identify independent predictors of HIV, HBV, or HCV.
| Covariate | OR** | 95% CI | P |
|---|---|---|---|
| Age (years) | 1.04 | (1.0, 1.08) | 0.08 |
| Marital status: Single* | 0.44 | (0.16, 1.2) | 0.09 |
| Marital status: Other* | 0.42 | (0.06, 3.12) | 0.39 |
| IDU | 24.32 | (9.35, 63.2) | < 0.001 |
| Paid heterosexual intercourse | 1.07 | (0.47, 2.46) | 0.96 |
| Paid homosexual intercourse | 1.40 | (0.54, 3.6) | 0.62 |
| Sex for drugs | 2.24 | (0.54, 9.27) | 0.24 |
| Blood transfusion | 2.09 | (0.61, 7.14) | 0.23 |
| Surgery | 2.41 | (1.05, 5.54) | 0.03 |
| Clean blade at barber | 0.48 | (0.19, 1.23) | 0.1 |
Reference category is Marital status: Married.
All odds ratios are adjusted for all other variables in the table
Table 3b. Multivariable logistic regression model to identify independent predictors of Syphilis.
| Covariate | OR** | 95% CI | P |
|---|---|---|---|
| Age (years) | 1.00 | (0.96, 1.05) | 0.92 |
| Marital status: Single* | 0.68 | (0.24, 1.91) | 0.46 |
| Marital status: Other* | 1.80 | (0.31, 10.56) | 0.51 |
| IDU | 0.66 | (0.21, 2.03) | 0.45 |
| Paid heterosexual intercourse | 3.28 | (1.24, 8.7) | 0.02 |
| Paid homosexual intercourse | 0.54 | (0.18, 1.64) | 0.29 |
| Sex for drugs | 0.99 | (0.19, 5.17) | 0.97 |
| Blood transfusion | 1.42 | (0.34, 5.97) | 0.62 |
| Surgery | 0.80 | (0.32, 1.98) | 0.61 |
| Clean blade at barber | 0.86 | (0.31, 2.38) | 0.65 |
Reference category is Marital status: Married.
All odds ratios are adjusted for all other variables in the table
DISCUSSION
We found the prevalence of TB, HIV, syphilis, HBV, and HCV to be higher among male prisoners than in reports from the general population in Pakistan, as expected[17, 23, 28, 34]. The prisoners had low literacy rates, low socioeconomic status, and many had been incarcerated previously, as seen in other prison studies[6, 7, 11]. Sexual risk in these men derived from paid sex with both women and men and with very low condom use. Substance abuse was common (60%), as was needle use (23% of users) and needle sharing (46% of needle users), compatible with findings from a large Pakistan survey of drug users in 2006-2007. Infectious risk was derived from the high proportion of drug users, their median length of drug use (7.1 years), and the high rates of body tattooing, piercing, use of old blades for haircuts and shaves, and prior surgical history. (We did not study HIV-related blood transfusion as most men were unsure as to their transfusion histories). We saw a very high turnover of inmates, similar to circumstances in other countries [2, 11, 12]. Among IDUs, 84% had been incarcerated previously, providing a vicious cycle of acquisition and transmission both outside and inside the prison. At the same time, these grim statistics underscore the opportunity and potential community benefits of screening and treatment in a high-risk, easily-accessed population[35]. The potential danger of discharging an IDU without a community treatment venue, an uneducated hepatitis patient, or an untreated TB or HIV patient can extend beyond Karachi’s metropolitan area; inmates came from all four regions of Pakistan and nine foreign countries.
The prevalence in our study for pulmonary TB was 2.2%. This is lower than seen in some prison studies[7-9, 18, 20] and about the same as seen in India prison [14], though TB diagnosis definitions differ by study. The 2.2% active TB rate is nonetheless much higher than in the general population[17]. Our definition of smear positive with culture confirmation is more specific and less sensitive than used by some studies. Although our study cannot identify whether TB was acquired in the prison, prisons are overcrowded, may have poor ventilation, and have notoriously poor health care facilities, including isolation rooms for active cases. Among seven HIV-positive participants, only one was previously diagnosed for HIV and five gave a history of IDU. Syphilis prevalence (RPR+/TPHA+) was 8.9%, not a stereotypically low prevalence rate from a Muslim country. A 1994 behavioral survey in Sindh prisons on genital ulcers and urethritis concluded that STD rates would be a serious problem in the prison population[15]. There are very limited data regarding Hepatitis B and C in prison populations in Pakistan[28]. In contrast, more work has been done in Iran, which borders Pakistan, where prison studies have focused on IDUs and their need for harm reduction programs, especially opiate substitution treatment[36].
In our multivariable model, the significance risk factors for any blood borne infection (HIV, HBV and HCV) were IDU and having had surgery. This suggests the origin of blood borne infections among IDUs and, possibly during surgery due to the poor sterilization procedures in some Pakistani venues. For syphilis, having paid for sex with a female was the only significant predictor, but this might reflect social response bias because male-to-male sex is not culturally acceptable in Pakistani society and is denied, though it is prevalent.
Incarceration in both lower and upper income countries are incubators for infectious diseases[37]. This is due to the fact that pre-incarceration prisoners are a core transmitter group with high risk sexual behaviors such as sex work, being clients of sex workers, drug use including IDUs, and low literacy levels[38].During incarceration, prisoners may acquire new infections due to overcrowding, poor medical diagnosis and treatment, insufficient infection control, an absence of harm reduction efforts like condom use or needle exchange, and sudden transfer to other facilities or discharge into the community without provisions for ongoing therapy[1]. High risk activities like tattooing, IDU, and sexual activity, although banned, nonetheless take place inside prison [37]. These factors not only instigate greater vulnerability among prisoners but also due to their frequent flow in the community can be a major concern for epidemics of infectious diseases among general population[38].
Prisons are excellent venues for screening and interrupting infectious diseases commonly prevalent in incarcerated as well as in general populations. Most inmates are from lower income backgrounds and have limited access to health care services and routine screening checkups[5]. In jails and many prisons, most inmates are incarcerated for a short period of time and if they return back to the community with undetected infections, there has been a missed opportunity to screen and treat[39]. To break this chain of transmission in resource-limited settings, routine screening and treatment in jails/prisons can be expected to benefit the communities to which prisoners are being released. While proper screening and treatment in the prison is a public health boon, confidentially of medical information of inmates who test positive does not exist in most settings such that news leaks into the prison environment[37]. HIV, for example, is still stigmatized and if the news leaks out that a given prisoner is HIV-infected, he may be abused or neglected both inside and outside the prison. If an inmate is on longer-term treatment for TB, for example, and is transferred to another prison or released, treatment is interrupted unless the other prison has a similar treatment program process or there is a bridge to community-based TB programs. Paradoxically, correction facilities may provide free shelter and food for disenfranchised, homeless persons (like IDUs), but rarely offer harm reduction or infection screening programs[37].
Strengths of our study included the representative sampling, the high response rate, and our action plan to provide improved logistic procedures for prison health care staff and improved care for diseased prisoners. This was the first study in Pakistan focusing on five major infectious diseases in a prison population. Limitations included our inability to assess incidence because of the cross-sectional study design, study of only a single facility due to budget constraints, and lack of IRB approval for X-ray screening for tuberculosis (deemed more than minimal risk by the U.S.-based IRB and the OHRP such that a review would have put our study into a >10-month queue for special review by the U.S. Secretary of Health and Human Services). We had insufficient numbers of events to examine risk factors for HIV, HBV, and HCV separately. Finances limited the extent of our workup and the number of infections that we could diagnose. We believe improvements in clinical management benefited the study volunteers, but only a small component of our protocol has been implemented prison-wide after completion of our study.
Pakistan spends a higher proportion of its governmental expenditures on the military than almost any other nation, investing comparatively little in health, education, and social services[40]. A powerful argument can be made that health, education, and social services within a prison setting can be a superb long-term investment. A prison-based screening program enables early intervention among the inmates through disease detection, treatment, and education[41]. It also benefits the general population by interrupting disease transmission when detainees return to the community, as long as bridges are built between prison discharge and available community services, as with directly observed therapy-short course (DOTS) for TB. Prison data provide epidemiological insights into a subset of high-risk populations at lower cost than comparable community surveys[39]. Our results justify investing in treatable diseases such as TB, HIV and syphilis, and they may well reflect conditions throughout the nation. HBV vaccination should be provided to all inmates. HCV prevention and care will be challenging, but health education and rehabilitation for drug users can help, especially using opiate agonist therapy, education, and job training. The urgency is augmented by the marked rise in HIV seroincidence documented among IDUs in Pakistan, surely a harbinger of worsening conditions for a variety of opportunistic infections and STDs.
ACKNOWLEDGEMENTS
We would like to thank Bridge Consultant Foundation team for their contribution and support. Drs Suleman Otho, Rashid Shaikh, Arshad Altaf, Raja Fahim, Ashraf Memon, Rana Muzzaffar, Salma Batool, A. Khalique Ghauri, Timothy Sterling, Jon Warkentin, and S. Asad Ali, and Mrs. Ellen Murray, provided assistance.
Financial Support: This work was supported in part by NIH grants D43TW001035 (AIDS International Training and Research Program), R25TW007766 (Framework Program for Global Health), and P30AI054999 (Vanderbilt-Meharry Center for AIDS Research).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Conflict of Interest: All authors: no conflicts.
REFERENCES
- [1].Bick JA. Infection control in jails and prisons. Clin Infect Dis. 2007 Oct 15;45(8):1047–55. doi: 10.1086/521910. [DOI] [PubMed] [Google Scholar]
- [2].McIntyre AF, Studzinski A, Beidinger HA, Rabins C. STD, HIV/AIDS, and Hepatitis Services in Illinois County Jails. Sex Transm Dis. 2008 Jan 28; doi: 10.1097/OLQ.0b013e31815e4167. [DOI] [PubMed] [Google Scholar]
- [3].Walmsley R. [Accessed on 8 January 2009];World Prison Population List. 2007 Available at: http://wwwkclacuk/depsta/law/research/icps/downloads/world-prison-pop-seventhpdf.
- [4].UNAIDS 2006 Report on the global AIDS epidemics; A UNAIDS 10th anniversary special edition; Geneva, Switzerland. May 2006; UNAIDS/06.20E. [Google Scholar]
- [5].Niveau G. Prevention of infectious disease transmission in correctional settings: a review. Public Health. 2006 Jan;120(1):33–41. doi: 10.1016/j.puhe.2005.03.017. [DOI] [PubMed] [Google Scholar]
- [6].Stuckler D, Basu S, McKee M, King L. Mass incarceration can explain population increases in TB and multidrug-resistant TB in European and central Asian countries. Proc Natl Acad Sci U S A. 2008 Sep 9;105(36):13280–5. doi: 10.1073/pnas.0801200105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wong MY, Leung CC, Tam CM, Kam KM, Ma CH, Au KF. TB surveillance in correctional institutions in Hong Kong, 1999-2005. Int J Tuberc Lung Dis. 2008 Jan;12(1):93–8. [PubMed] [Google Scholar]
- [8].Noeske J, Kuaban C, Amougou G, Piubello A, Pouillot R. Pulmonary tuberculosis in the Central Prison of Douala, Cameroon. East Afr Med J. 2006 Jan;83(1):25–30. doi: 10.4314/eamj.v83i1.9357. [DOI] [PubMed] [Google Scholar]
- [9].MacNeil JR, Lobato MN, Moore M. An unanswered health disparity: tuberculosis among correctional inmates, 1993 through 2003. Am J Public Health. 2005 Oct;95(10):1800–5. doi: 10.2105/AJPH.2004.055442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Verneuil L, Vidal JS, Ze Bekolo R, Vabret A, Petitjean J, Leclercq R, et al. Prevalence and risk factors of the whole spectrum of sexually transmitted diseases in male incoming prisoners in France. Eur J Clin Microbiol Infect Dis. 2008 Nov 8; doi: 10.1007/s10096-008-0642-z. [DOI] [PubMed] [Google Scholar]
- [11].Adjei AA, Armah HB, Gbagbo F, Ampofo WK, Boamah I, Adu-Gyamfi C, et al. Correlates of HIV, HBV, HCV and syphilis infections among prison inmates and officers in Ghana: A national multicenter study. BMC Infect Dis. 2008;8:33. doi: 10.1186/1471-2334-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Fialho M, Messias M, Page-Shafer K, Farre L, Schmalb M, Pedral-Sampaio D, et al. Prevalence and risk of blood-borne and sexually transmitted viral infections in incarcerated youth in Salvador, Brazil: opportunity and obligation for intervention. AIDS Behav. 2008 Jul;12(4 Suppl):S17–24. doi: 10.1007/s10461-008-9409-x. [DOI] [PubMed] [Google Scholar]
- [13].Solomon L, Flynn C, Muck K, Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and hepatitis C among entrants to Maryland correctional facilities. J Urban Health. 2004 Mar;81(1):25–37. doi: 10.1093/jurban/jth085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Singh S, Prasad R, Mohanty A. High prevalence of sexually transmitted and blood-borne infections amongst the inmates of a district jail in Northern India. Int J STD AIDS. 1999 Jul;10(7):475–8. doi: 10.1258/0956462991914357. [DOI] [PubMed] [Google Scholar]
- [15].Akhtar S, Luby SP, Rahbar MH. Risk behaviours associated with urethritis in prison inmates, Sindh. J Pak Med Assoc. 1999:268–73. [PubMed] [Google Scholar]
- [16].Baqi S, Nabi N, Hasan SN, Khan AJ, Pasha O, Kayani N, et al. HIV antibody seroprevalence and associated risk factors in sex workers, drug users, and prisoners in Sindh, Pakistan. J Acquir Immune Defic Syndr Hum Retrovirol. 1998 May 1;18(1):73–9. doi: 10.1097/00042560-199805010-00011. [DOI] [PubMed] [Google Scholar]
- [17].World Health Organization (WHO) Global tuberculosis control : surveillance, planning, financing. WHO; Geneva: 2008. [Google Scholar]
- [18].Rao NA. Prevalence of pulmonary tuberculosis in Karachi central prison. J Pak Med Assoc. 2004 Aug;54(8):413–5. [PubMed] [Google Scholar]
- [19].Hussain H, Akhtar S, Nanan D. Prevalence of and risk factors associated with Mycobacterium tuberculosis infection in prisoners, North West Frontier Province, Pakistan. Int J Epidemiol. 2003 Oct;32(5):794–9. doi: 10.1093/ije/dyg247. [DOI] [PubMed] [Google Scholar]
- [20].Shah SA, Mujeeb SA, Mirza A, Nabi KG, Siddiqui Q. Prevalence of pulmonary tuberculosis in Karachi juvenile jail, Pakistan. East Mediterr Health J. 2003 Jul;9(4):667–74. [PubMed] [Google Scholar]
- [21].Shah SA, Altaf A, Mujeeb SA, Memon A. An outbreak of HIV infection among injection drug users in a small town in Pakistan: potential for national implications. Int J STD AIDS. 2004 Mar;15(3):209. doi: 10.1258/095646204322916713. [DOI] [PubMed] [Google Scholar]
- [22].UNGASS Indicators Country Report. National AIDS Control Program Ministry of Health Government of Pakistan; Islamabad: 2006. [Google Scholar]
- [23].UNGASS Pakistan Report. National AIDS Control Program Ministry of Health Government of Pakistan; Islamabad: 2007. [Google Scholar]
- [24].Canada Pakistan HIV/AIDS Surveillance Project (CIDA) HIV Second Generation Surveillance in Pakistan: National Report Round II. National AIDS Control Program Ministry Of Health; Pakistan: 2006-07. [Google Scholar]
- [25].Canada Pakistan HIV/AIDS Surveillance Project (CIDA) HIV Second Generation Surveillance in Sindh: Round III IBBS Report. National AIDS Control Program Ministry Of Health; Pakistan: 2008. [Google Scholar]
- [26].Altaf A, Shah SA, Zaidi NA, Memon A, Nadeem ur R, Wray N. High risk behaviors of injection drug users registered with harm reduction programme in Karachi, Pakistan. Harm Reduct J. 2007;4:7. doi: 10.1186/1477-7517-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Survey of High Risk groups in Lahore and Karachi . National AIDS Control Program Ministry of Health Goverment of Pakistan; 2005. [Google Scholar]
- [28].Ali SADR, Qureshi H, Vermund SH. Prevalence and risk factors of Hepatitis B and C infections in Pakistan. Int J Infect Dis. 2008 doi: 10.1016/j.ijid.2008.06.019. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kuo I, ul-Hasan S, Galai N, Thomas DL, Zafar T, Ahmed MA, et al. High HCV seroprevalence and HIV drug use risk behaviors among injection drug users in Pakistan. Harm Reduct J. 2006;3:26. doi: 10.1186/1477-7517-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ur-Rehman DN. Problem of Drug Use In Pakistan: Results from Year 2006 National Assessment [Poster Presentations]; The First Asian Consultation on the Prevention of HIV related to Drug Use; Goa, India. 28 - 31 January, 2008. [Google Scholar]
- [31].HIV/AIDS in Pakistan. The World Bank; [Accessed 8 January 2009]. 2008. Available at http://siteresources.worldbank.org/INTSAREGTOPHIVAIDS/Resources/496350-1217345766462/HIV-AIDS-brief-Aug08-PK.pdf. [Google Scholar]
- [32].Inmate Statement of Sindh Jails. Home Department Govt of Sindh; Pakistan: [Accessed on 8 january 2009]. Available at http://www.sindh.gov.pk/dpt/Home/prisons.htm. [Google Scholar]
- [33].Angie Bone AA, Grzemska Malgosia, et al. Tuberculosis Control in Prisons: A Manual for Programme Managers. World Health Organization; 2000. [Google Scholar]
- [34].Khan EA, Khokhar N, Malik GJ. Seroprevalence of Syphilis in asymptomatic adults seeking employment abroad. Rawal Med J. 2004;29(2):65–7. [Google Scholar]
- [35].Restum ZG. Public health implications of substandard correctional health care. Am J Public Health. 2005 Oct;95(10):1689–91. doi: 10.2105/AJPH.2004.055053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Zamani S, Ichikawa S, Nassirimanesh B, Vazirian M, Ichikawa K, Gouya MM, et al. Prevalence and correlates of hepatitis C virus infection among injecting drug users in Tehran. Int J Drug Policy. 2007 Oct;18(5):359–63. doi: 10.1016/j.drugpo.2007.02.007. [DOI] [PubMed] [Google Scholar]
- [37].Comfort ML, Grinstead O. The carceral limb of the public body: jail inmates, prisoners, and infectious disease. J Int Assoc Physicians AIDS Care (Chic Ill) 2004 Apr-Jun;3(2):45–8. doi: 10.1177/154510970400300202. [DOI] [PubMed] [Google Scholar]
- [38].Clark M, Cameron DW. Health of prisoners, and the public health: no man is an island. J Int Assoc Physicians AIDS Care (Chic Ill) 2004 Apr-Jun;3(2):44. doi: 10.1177/154510970400300201. [DOI] [PubMed] [Google Scholar]
- [39].White MC. Identifying infectious diseases in prisons: surveillance, protection, and intervention. West J Med. 1999 Mar;170(3):177. [PMC free article] [PubMed] [Google Scholar]
- [40].Islam A, Tahir MZ. Health sector reform in South Asia: new challenges and constraints. Health Policy. 2002 May;60(2):151–69. doi: 10.1016/s0168-8510(01)00211-1. [DOI] [PubMed] [Google Scholar]
- [41].Weilandt C, Radun D. Prisons: health hazards, but also health opportunities. Euro Surveill. 2007 Jan 20;12(1) [Google Scholar]