Abstract
Background
Restricting the dietary intake of sodium chloride is associated with a reduction of the arterial blood pressure by approximately 4/2 mm Hg in hypertensive patients and by approximately 1/0.6 mm Hg in normotensive persons. As the cardiovascular risk is known to rise steadily with systolic blood pressure values starting from 115 mm Hg, lowering the mean blood pressure of the general population by dietary salt restriction would seem to be a practicable form of primary prevention of cardiovascular disease.
Method
Selective literature search and review.
Results
Multiple studies have shown dietary salt restriction to be associated with lower cardiovascular morbidity and mortality. The reduction of adjusted relative risk in controlled observational studies ranges from 25% over 15 years to 41% over three years.
Conclusion
On the basis of the available studies, it seems likely that a moderate lowering of the daily intake of sodium chloride by the general population from 8 to 12 grams per day (the current value) to 5 to 6 grams per day would be a useful public health measure, with economic benefits as well. The potential risks for certain groups of individuals are foreseeable and controllable. A general reduction of dietary salt intake can only be achieved by reducing the sodium chloride content of industrially processed foods, as these account for 75% to 80% of the sodium chloride consumed daily. Aside from a general reduction of dietary salt intake, further important primary prevention measures for the general population include changes in lifestyle and in dietary habits.
Cardiovascular disorders continue to be responsible for more than half of all deaths in western industrialized nations (e1). Primary prevention of these disorders aims to reduce their premature occurrence and the economic burden they place on society. This review article is based on a selective literature search and an earlier review article (4) investigating the relation between dietary salt intake, blood pressure, incidence of hypertension, and cardiovascular sequelae. We review whether reducing dietary salt intake is a promising measure for the primary prevention of cardiovascular morbidities in the long term. Unfortunately, in spite of large-scale information campaigns to the public, attempts to change the eating habits of Germany’s population in the past 10 years, and to thus reduce the rates of overweight and obesity, have failed, as is obvious from the data collected in the German National Consumption Study II (Nationale Verzehrsstudie II [1]). Education campaigns targeting selected groups of patients have yielded some impressive successes, as evidenced by DASH (Dietary Approach to Stop Hypertension), a diet that resembles the Mediterranean diet and has led to notable reductions in blood pressure in hypertensive and normotensive persons (2, e2). The risk of coronary heart disease (CHD) and stroke was also lowered, as shown by a 24 year study of 18 497 nurses that had followed the DASH diet closely (e3). Adherence to these measures has, however, been low since the studies were concluded (3). Similarly, studies of dietary salt reduction have shown that a mere 25% of participants reached the desired objective (e4). A general change of dietary habits in the sense of Mediterranean food has also failed because a change in individual dietary habits has been notably less accepted by socioeconomically weaker strata of society—presumably for reasons of cost—than by the higher social classes (1).
Dietary salt intake, cardiovascular risk, and incidence of hypertension
The publications cited by us reported and discussed mostly only the adjusted relative risks. We calculated changes in absolute risks from the raw data provided in some studies. An increase in the intake of dietary salt of 100 mmol (approximately 5.8 g NaCl) is associated with an increase in cardiovascular events of 51% and in overall mortality of 26%, as was shown by a 7 year prospective study from Finland, which included 1173 men and 1263 women whose salt intake was determined by measuring their renal excretion of sodium (e5).
In a recently published meta-analysis of 13 studies with 177 025 participants and study periods ranging from 5 to 19 years, an increase in the intake of dietary salt of 5 g/day was associated with an increase in the rate of strokes of 23% and of cardiovascular morbidities of 17% (6). A high intake of salt leads to greater mortality due to stroke independently of a rise of blood pressure (e6, e7).
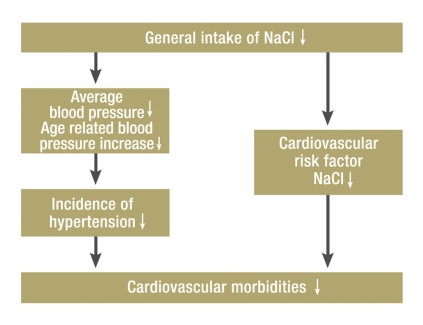
A high dietary intake of salt thus constitutes a cardiovascular risk factor independent of blood pressure (figure), a fact that has also been confirmed in numerous other clinical and experimental studies (4, 5) (box 1).
Figure.
Mechanisms for a fall in cardiovascular morbidities by reducing dietary salt intake in the general population
Box 1.
Independently of blood pressure, a high intake of NaCl has been associated with the following findings in clinical studies:
Increases in left ventricular muscle mass (e37)
Reduction in arterial compliance and raised pulse pressure (e38)
Weakened baroreceptor reflex (e39)
Initially increased glomerular filtration rate, later glomerulosclerosis (e40)
Increased microalbuminuria (e41)
Experimentally in rats: myocardial and renal fibrosis (e42)
Conversely, restricting dietary salt intake is associated with a decrease in the rate of cardiovascular events. In the TOHP-I (Trial of Hypertension Prevention) study of slightly overweight persons with high normal blood pressure (7), 744 participants reduced their dietary salt intake by 2.6 g/d for a year and a half; in the TOHP-II study, 2382 participants reduced their dietary salt intake by 2 g/d for 4 years. After adjusting for various biases, the relative risk for cardiovascular events 15 and 10 years later was significantly (25%) lower in participants with restricted dietary salt intake than in the control groups on whom no dietary salt restriction was imposed in the earlier study periods (absolute risk reduction [ARR] 1.4%). Total mortality fell by 20% (ARR 0.3%), but did not reach significance. Titze and Ritz (e8) pointed out that the reduced rate of cardiovascular events in this study can be explained primarily with the intensive dietary and behavioral advice with the objective of achieving a reduction in daily salt intake.
In Taiwan, 2 of 5 large-scale catering establishments in old people’s homes substituted salt with sodium-reduced, potassium-enriched mineral salt (49% NaCl, 49% KCl), which meant a reduction in dietary salt intake in 768 elderly people from 13.1 g/d to 9.6 g/d. After 31 months, the adjusted cardiovascular mortality in the group with restricted salt intake was 41% lower than in the control group whose salt intake had remained unchanged (raw data: 27 events per 2057 person years in the intervention group versus 66 events per 3218 person years in the control group [8]). This equates to an absolute risk reduction of 0.74%.
In Finland in 1972 to 2002, the relative risk for annual mortality due to myocardial infarction fell by 77% and due to stroke by 71% in the age group under 65, and the average life expectancy rose by 6 years in both men and women (9). The relative risk reductions are compared with the general annual risk of Finish people younger than 65 of dying from stroke, which was about 1 in 1000 in 1972 (10). The authors (9) explain this success to a large part with a reduction in dietary salt in processed foods, in which sodium chloride was partly substituted by mineral salt that consisted of only 50% sodium chloride and 50% potassium chloride, magnesium sulfate, and lysine hydrochloride. The average daily intake of dietary salt fell from 14 g/d to 9 g/d and the average systolic blood pressure by 15 mm Hg. The observed fall in mortality due to stroke was 52% and the fall in CHD rates 15%, which was explained with the lower blood pressure resulting from NaCl reduction (10, 11). Other crucial influences on the successful results included the fall in total cholesterol measurements from 7.0 mmol/L to 5.7 mmol/L (e9), the fall in the rate of smokers from 53% to 37%, and better treatments for hypertension and CHD (10, 11).
In Japan, mortality due to stroke between 1970 and 1990 fell by 43.5% (raw data: 99/100 000 versus 175/100 000), which was associated with a reduction in the average salt intake from 14.5 g/d to 12.5 g/d (12, e10).
A reduced dietary intake of salt is accompanied by a lowering of blood pressure in the population. Restricting the daily salt intake by 0.9 g, which was monitored by measuring sodium excretion, and increasing the amount of fruit and vegetables in people’s diets in a Japanese village of 550 inhabitants was associated with a fall in average systolic blood pressure of 2.7 mm Hg within a year, compared with a control village where the dietary salt intake increased by 0.7 g/d during the same time period. The diastolic blood pressure remained the same (13).
Lowering the average blood pressure is also associated with a decrease in hypertension (e11). In North Karelia, between 1982 and 1997, reductions in the average blood pressure of 6/3 mm Hg in men and 7/3 mm Hg in women were associated with a fall in the prevalence of hypertension in men from 35.1% to 28.7% and in women from 28.4% to 20.8% (e12).
Some studies have shown no relation (14, 15) or an inverse relation (16) between the amount of dietary salt intake and cardiovascular morbidities. However, these studies either had short observational periods of merely a few years (such as the Scottish Heart Health Study [14] or the Rotterdam Study [15]) or were methodologically controversial (16, e13).
One of the criticisms of the data from the NHANES-I survey published by Alderman in 1992 (16) has to be that the daily dietary intake if sodium chloride for 19 years was extrapolated from a single day’s intake (one-day recall). In the 9-year NHANES-III survey of 2000 (e14), the raised incidence of cardiovascular morbidities in people with low salt intake did not reach significance (as it had in NHANES-I) but was noticeable only as a trend. Alderman (17) discusses the possibility of a J curve between sodium intake and cardiovascular morbidity and mortality, which seems to be borne out by experimental findings (e15).
Critical assessment of benefits and possible risks
Hopper et al. (18) are of the opinion that the achieved reduction in average blood pressure by 1/0.6 mm Hg is too low to reduce risk of cardiovascular morbidities. They base their opinion on a comprehensive Cochrane Review of 11 randomized controlled trials (RCTs) including 3514 normotensive and hypertensive individuals in whom the average daily dietary salt intake was reduced by 2 g. Similar to McCarron (19), they call for RCTs to confirm a reduction in overall mortality, which was not proven in TOHP-I and TOHP-II (7). However, RCTs to answer this question are hardly possible because, in addition to exorbitant costs, several thousand participants would have to be recruited who, in the intervention group, would have to reduce their salt intake permanently for 10–15 years (6). The question of whether the effects of dietary salt reduction are also attributable to changes in the intake of other minerals as a result of the dietary modification remains unanswered (18, 19). Overall, in persons restricting salt intake, a trend exists to increase the dietary intake of potassium and magnesium and to decrease the intake of calcium, iron, some B vitamins, and saturated fats (18). This argument is not valid if the salt content is reduced only in industrially processed foods.
Investigators in some short term trials have observed activation of the renin-angiotensin-aldosterone system and the sympathetic nervous system, a decrease in insulin sensitivity, and increases in LDL cholesterol concentrations, triglycerides, and uric acid (box 2). Jürgens and Graudal (20) interpret the increase in LDL cholesterol by 5% as a possible risk factor for an increase in cardiovascular morbidities. However, such increases in LDL cholesterol were observed only under the extreme conditions of a short-term drastic restriction of dietary salt intake to 1 g/d for 5–7 days. For the primary prevention of cardiovascular morbidities, a moderate salt restriction to 5–6 g/d is recommended. In the TOMHS study, participants with mild hypertension whose only therapeutic measure was salt reduction by 1.5 g/d, lowered LDL cholesterol measurements of 7.5 mg/dL and of triglycerides of 19.2 mg/dL were observed after 4.4 years (e16).
Box 2.
Possible adverse effects of a general reduction in dietary salt to 5–6 g/d
Sodium deficiency in extreme situations (heat, diarrhea)
Sodium loss in renal morbidities
Sodium deficiency in adrenal insufficiency
Hyponatremia in elderly people (?)
Hypovolemia in pregnancy (?)
Iodine deficiency
Adverse effects of drastic salt restriction to 1 g/d
Activation of renin-angiotensin-aldosterone system
Activation of sympathetic nervous system (only noradrenaline)
Increase of LDL cholesterol levels and triglycerides in blood
Increased blood concentrations of uric acid
Lowered insulin sensitivity
Jürgens and Graudal (20) interpret the trebling of plasma renin and aldosterone concentrations as a physiological counter-reaction. Recent studies have shown that raised plasma renin levels do not result in a higher incidence of cardiovascular morbidities (e17). In Yanomamo Indians who consume only 0.4 g/d of NaCl, plasma renin levels are also increased to similar concentrations and aldosterone to about 10 times the normal level; however, no increase in cardiovascular morbidities has been reported for this population (e18).
With a moderate restriction of salt intake to 5–6 g/d, which vastly exceeds the minimum requirement of 1 g/d, short episodes of severe diarrhea or longer episodes of vomiting are not likely to cause sodium deficiency, and are likely to be manageable in the same way as sodium loss subsequent to renal disease or adrenal insufficiency. Geriatricians (21) warn of restricting dietary salt intake in elderly patients for fear of causing sodium deficiency. Most elderly people would, however, benefit from restricting dietary salt intake because 60% to 70% of those older than 70 have systolic hypertension of old age, for which restricting salt intake is as beneficial as for systolic-diastolic hypertension (e19).
A moderately restricted salt intake is not believed to be dangerous for pregnant women. The upper limit of 5.8 g/d of salt that was decided by the US Food and Nutrition Board in 2004 also applies to pregnant women (22, e20). Controlled studies in pregnant women who restricted their salt intake to 3.5 g/d did not show any effects on maternal blood pressure and neonatal weight (e21).
In regions with endemic struma, a general restriction of dietary salt may result in iodine deficiency; iodine supplementation is required for pregnant women in such areas even now (e22). Iodine deficiency, which is a possible side effect of lower salt intake, can be balanced by increasing iodine concentrations in the salt (23).
Putting salt restrictions into practice
The minimum salt requirement is about 1 g/d, as has been shown in indigenous populations (e23). Restricting salt intake in the industrialized countries from 8–12 g/d to 5–6 g/d has been recommended for hypertensive individuals for many years by the World Health Organization (23) and guidelines from and numerous medical societies (e24, e25); nowadays this is recommended even for the general population (22). This will be difficult to achieve in everyday life because people in Western industrialized countries ingest 75% to 80% of their daily amounts of dietary salt in industrially processed foods (sausages, cheeses, tinned foods, ready meals, fast food, restaurant food, and canteen food) and especially in bread (box 3). It therefore seems to make sense to lower the salt content of foods gradually by 40% to 50%.
Box 3. Dietary salt consumption per day.
Average amount of dietary salt in average daily amounts consumed in Germany (e43)
| • | 1 g: | basic foodstuffs, unprocessed: vegetables, potatoes, grains, milk, meat |
| • | 2–3 g: | bread, all sorts |
| • | 3–5 g: | cold cuts: sausages, ham/bacon, salt-cured foods, cheeses, marinades for fish |
| • | 4–5 g: | industrially processed foods, tinned foods, fish dishes, home made foods |
| • | 1–2 g: | putting extra salt on food and using seasonings that contain salt |
Expected successes
The extent of salt reduction and targeted fall in blood pressure determine the success of restricting the salt intake in the general population. If the dietary salt intake is moderately reduced by 3 g/d, the systolic blood pressure reduction in normotensive individuals is expected to be 1.8 to 3.5 mm Hg (24, e28). Lowering systolic pressure is associated with a relative risk reduction for ischemic heart disease and cardiovascular mortality of 4% to 5% and a fall in overall mortality of 3% (25). In the US, a reduction of salt intake to an average of 5.8 g/d is expected to result in an annual reduction of hypertension cases by 11 million and annual cost savings of 18 billion dollars in the healthcare system (e29). A decreased incidence of hypertension as a result of salt restriction would thus counteract the increased rates in overweight, diabetes, and terminal renal failure that have been seen in the US and Europe in recent years (e30).
A general reduction in salt is also beneficial in children because the salt intake during childhood determines blood pressure in children and adolescents, and a high salt intake is likely to increase the appetite for salt (e31). Increasing consumption of soft drinks also leads to an increase in salt intake in children and adolescents. Restricting salt would therefore also contribute to combating the increasing problem of overweight in young people (e32).
Conclusion
In the context of this review article it is not possible to consider all studies of interventions (medical treatment, changes of lifestyle) that influence cardiovascular morbidities (e33, e34) and their beneficial effects (5, e13) or the whole subject of salt sensitivity (e35). The main task for the planned task force “Less salt for all” (e36) should be to critically assess the risks and benefits of a general restriction of dietary sodium chloride. We cannot expect rapid successes for a stepwise, gradual reduction of the salt content of processed foods. Patience is required, as is the provision of non-dogmatic and consistent information to the public. We cannot emphasize enough that lifestyle modifications and dietary modifications as the established measures for the primary prevention of cardiovascular morbidities should not only be retained but should even be intensified because a high intake of dietary salt and raised blood pressure are merely two of many cardiovascular risk factors.
Key Messages.
A dietary sodium chloride intake of more than 6 g per day is associated with increased blood pressure and thus cardiovascular risk.
Excessive dietary sodium chloride intake is not only associated with raised blood pressure and resultant organ damage but is also a risk factor independently of blood pressure.
Restricting the daily salt intake to 5–6 g in the general population is associated with an average reduction in blood pressure and a lowered incidence of hypertension and a lower cardiovascular risk.
Lowering the daily amount of salt ingested in food in the general population is possible only by means of reducing the sodium chloride content of processed foods.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Hauner H. Ernährungsmedizin 2009. Dtsch Med Wochenschr. 2009;134:1349–1353. doi: 10.1055/s-0029-1225289. [DOI] [PubMed] [Google Scholar]
- 2.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure: DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 3.Mellen P, Gao SK, Vitolius SZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168:308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 4.Klaus D, Böhm M, Halle M, et al. Die Beschränkung der Kochsalzaufnahme in der Gesamtbevölkerung verspricht langfristig großen Nutzen. Dtsch Med Wochenschr. 2009;134:108–118. doi: 10.1055/s-0029-1222573. [DOI] [PubMed] [Google Scholar]
- 5.Cailar G, Mimram A. Non-pressure related effects of dietary sodium. Curr Hypertens Rep. 2007;9:154–159. doi: 10.1007/s11906-007-0027-1. [DOI] [PubMed] [Google Scholar]
- 6.Strazullo P, D’Elia L, Kandala N, Cappuccio FP. Salkt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339 doi: 10.1136/bmj.b4567. b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–892. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang HY, Hu YW, Yue CS, et al. Effect of potassium-enriched salt on cardiovascular mortality and medial expenses of elderly men. Am J Clin Nutr. 2006;83:1289–1296. doi: 10.1093/ajcn/83.6.1289. [DOI] [PubMed] [Google Scholar]
- 9.Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006;49:59–75. doi: 10.1016/j.pcad.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Vartiainen E, Sarti C, Tuomilehto J, Kuulasmaa K. Do changes in cardiovascular risk factors explain changes in mortality from stroke in Finland? BMJ. 1995;310:901–904. doi: 10.1136/bmj.310.6984.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vartiainen E, Puska P, Pekkanen J, Tuomilehto J, Jousilahti P. Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. BMJ. 1994;309:23–27. doi: 10.1136/bmj.309.6946.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ueshima H, Tatara K, Asakura S, Okamoto M. Declining trends in blood pressure level and the prevalence of hypertension, and changes in related factors in Japan 1956-1980. J Chron Dis. 1987;40:137–147. doi: 10.1016/0021-9681(87)90065-8. [DOI] [PubMed] [Google Scholar]
- 13.Takahashi Y, Sasaki, Okubo S, Hayashi M, Tsugane S. Blood pressure change in a free-living population-based dietary modification study in Japan. J Hypertens. 2006;24:451–458. doi: 10.1097/01.hjh.0000209980.36359.16. [DOI] [PubMed] [Google Scholar]
- 14.Tunstall-Pedoe H, Woodward M, Travendale R, Brook RA, McCluskey MK. Comparison of the prediction by 27 different factors of coro-nary heart disease and death in men and women of the Scottish heart health study: cohort study. BMJ. 1997;315:722–729. doi: 10.1136/bmj.315.7110.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geleijnse JM, Witteman JC, Stijnen T, Kloos MW, Hofman A, Grobbee DE. Sodium and potassium intake and risk of cardiovascular events and all-cause mortality: the Rotterdam Study. Eur J Epidemiol. 2007;22:763–770. doi: 10.1007/s10654-007-9186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alderman MH, Cohen H, Madhavan S. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I) Lancet. 1998;351:781–785. doi: 10.1016/S0140-6736(97)09092-2. [DOI] [PubMed] [Google Scholar]
- 17.Alderman MH. Dietary sodium and cardiovascular disease: the ’J’-shaped relation. J Hypertension. 2007;25:903–907. doi: 10.1097/HJH.0b013e3280c14394. [DOI] [PubMed] [Google Scholar]
- 18.Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane -Database of Systematic Reviews. 2004;(Issue 1) doi: 10.1002/14651858.CD003656.pub2. [DOI] [PubMed] [Google Scholar]
- 19.McCarron DA. Dietary sodium and cardiovascular and renal disease risk factors: dark horse or phantom entry? Nephrol Dial Transplant. 2008;23:2133–2137. doi: 10.1093/ndt/gfn312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jürgens G, Graudal NA. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride. Cochrane Database Syst Rev. 2004;(1) doi: 10.1002/14651858.CD004022.pub2. CD004022. [DOI] [PubMed] [Google Scholar]
- 21.Füsgen I. Hyponatriämie durch unnötige Salzangst. Therapiewoche. 1992;42:2304–2310. [Google Scholar]
- 22.Dickinson BD, Havas S. Council on Science and Public Health, American Medical Association. Reducing the population burden of cardiovascular disease by reducing sodium intake: a report of the Council on Science and Public Health. Arch Intern Med. 2007;167:1460–1468. doi: 10.1001/archinte.167.14.1460. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Reducing salt intake in populations. Report of a WHO Forum. 2006 [Google Scholar]
- 24.He FJ, MacGregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2004;(3) doi: 10.1002/14651858.CD004937. CD004937. [DOI] [PubMed] [Google Scholar]
- 25.Stamler J. The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr. 1997;65(suppl):626–642. doi: 10.1093/ajcn/65.2.626S. [DOI] [PubMed] [Google Scholar]
- e1.Statistisches Bundesamt Deutschland, Pressemitteilung Nr. 344 vom 15. 9. 2009. [Google Scholar]
- e2.Sacks FM, Svetkey LP, Vollmer WM, et al. for the DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet: DASH Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- e3.Fung TT, Chiuve SE, McCullough ML, et al. Adhaerence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- e4.Kumanyika SK, Cook NR, Cutler JA, et al. Sodium reduction for hypertension prevention in overweight adults: further results from the Trials of Hypertension Prevention Phase II. J Hum Hypertens. 2005;19:33–45. doi: 10.1038/sj.jhh.1001774. [DOI] [PubMed] [Google Scholar]
- e5.Tuomilehto J, Jousilahti P, Rastenvte D, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001;357:848–851. doi: 10.1016/S0140-6736(00)04199-4. [DOI] [PubMed] [Google Scholar]
- e6.Nagata C, Takatsuka N, Shimizu N, Shimizu H. Sodium intake and risk of death from stroke in Japanese men and women. Stroke. 2004;35:1543–1547. doi: 10.1161/01.STR.0000130425.50441.b0. [DOI] [PubMed] [Google Scholar]
- e7.Yamori Y, Nara Y, Mizumisha S, et al. Nutritional factors for stroke and major cardiovascular diseases: international epidemiological comparison of dietary prevention. Health Rep. 1994;6:22–27. [PubMed] [Google Scholar]
- e8.Titze J, Ritz E. Salt and its effect on blood pressure and target organ damage: new pieces in an old puzzle. J Nephrol. 2009;22:177–189. [PubMed] [Google Scholar]
- e9.Pietinen P, Vartiainen E, Seppänen R, et al. Changes in diet in Finland from 1972 to 1992: impact on coronary heart disease risk. Prev Med. 1996;25:243–250. doi: 10.1006/pmed.1996.0053. [DOI] [PubMed] [Google Scholar]
- e10.Vital and Health Statistics Division, Statistics and Information Department, Ministry of Health, Labour and Welfare, Japan. [Google Scholar]
- e11.Stamler J, Rose G, Stamler R, et al. INTESALT study findings. Public health and medical care implications. Hypertension. 1989;14:570–577. doi: 10.1161/01.hyp.14.5.570. [DOI] [PubMed] [Google Scholar]
- e12.Kastarinen MJ, Salomaa VV, Vartiainen EA, et al. Trends in blood pressure levels and control of hypertension in Finland from 1982-1997. J Hypertens. 1998;16:1379–1387. doi: 10.1097/00004872-199816090-00019. [DOI] [PubMed] [Google Scholar]
- e13.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Human Hypertens. 2009;23:363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- e14.Cohen HW, Halpern SM, Alderman MH. Sodium intake and Mortality follow-up in the third national health and nutrition examination Survey (NHANES III) J Gen Intern Med. 2008;231:297–302. doi: 10.1007/s11606-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e15.Ritz E. Salt - friend or foe? Nephrol Dial Transplant. 2006;21:2052–2056. doi: 10.1093/ndt/gfi256. [DOI] [PubMed] [Google Scholar]
- e16.Grimm RH, Flack JM, Grandits GA, et al. Long-term effects on plasma lipids of diet and drugs to treat hypertension. JAMA. 1996;275:1549–1556. doi: 10.1001/jama.1996.03530440029033. [DOI] [PubMed] [Google Scholar]
- e17.Parikh NI, Gona P, Larson MG, et al. Plasma renin and risk of cardiovascular disease and mortality: the Framingham Heart Study. Eur Heart J. 2007;282:644–652. doi: 10.1093/eurheartj/ehm399. [DOI] [PubMed] [Google Scholar]
- e18.Oliver JW, Cohen EL, Neel JV. Blood pressure, sodium intake, and sodium related hormones on the Yanomamo Indians, a “no salt” culture. Circulation. 1975;52:146–151. doi: 10.1161/01.cir.52.1.146. [DOI] [PubMed] [Google Scholar]
- e19.He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure in isolated systolic hypertension and combined hypertension. Hypertension. 2005;46:66–70. doi: 10.1161/01.HYP.0000171474.84969.7a. [DOI] [PubMed] [Google Scholar]
- e20.Institute of Medicine. Water, Potassium, Sodium Chloride, and Sulfate. 1st edition. Washington, DC: National Academy Press; 2004. Dietary Reference Intakes. [Google Scholar]
- e21.van der Maten GD, Van Raaij JM, Visman L, et al. Low-sodium diet in pregnancy: effects on blood pressure and maternal nutritional status. Br J Nutr. 1997;77:703–720. doi: 10.1079/bjn19970069. [DOI] [PubMed] [Google Scholar]
- e22.Maberly GF, Haxton DP, van der Haar F. Iodine deficiency: consequences and progress toward elimination. Food Nutr Bull. 2003;24(Suppl 4):91–98. doi: 10.1177/15648265030244S205. [DOI] [PubMed] [Google Scholar]
- e23.Carvalho JJ, Baruzzi RG, Howard PF, et al. Blood pressure in four remote populations in the Intersalt study. Hypertension. 1989;14:238–246. doi: 10.1161/01.hyp.14.3.238. [DOI] [PubMed] [Google Scholar]
- e24.Chobanian AV, Bakris GL, Black HR, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;43:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- e25.Guidelines Committee. 2003 European Society of Hypertension - European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- e26.Cohen HW, Hailpern SM, Fang J, Alderman MH. Sodium intake and mortality in the NHANES II follow-up study. Am J Med. 2006;119:275e7–275e14. doi: 10.1016/j.amjmed.2005.10.042. [DOI] [PubMed] [Google Scholar]
- e27.Food labelling. Health claims and label statements: sodium/hypertension. Federal Register. 1991;56:60825–60855. [Google Scholar]
- e28.Law MR, Frost CD, Wald NY. By how much does dietary salt reduction lower blood pressure. BMJ. 1991;302:811–824. doi: 10.1136/bmj.302.6780.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e29.Palar K, Sturm R. Potential societal savings from reduced sodium consumption in the U.S. adult population. Am J Health Promot. 2009;24:49–57. doi: 10.4278/ajhp.080826-QUAN-164. [DOI] [PubMed] [Google Scholar]
- e30.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics - 2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 Jan 29;117(4):e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- e31.Geleijnse JM, Grobbee DE. High salt intake early in life: does it increase the risk of hypertension? Hypertension. 2002;20:2121–2124. doi: 10.1097/00004872-200211000-00003. [DOI] [PubMed] [Google Scholar]
- e32.He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension. 2008;51:629–634. doi: 10.1161/HYPERTENSIONAHA.107.100990. [DOI] [PubMed] [Google Scholar]
- e33.He J, Ogden LG, Vupputuri S, Bazzano LA, Loria C, Whelton PK. Dietary sodium intake and subsequent risk of cardiovascular disease in overweight adults. JAMA. 1999;282:2027–2034. doi: 10.1001/jama.282.21.2027. [DOI] [PubMed] [Google Scholar]
- e34.He J, Ogden LG, Bazzano LA, et al. Dietary sodium intake and incidence of congestive heart failure in overweight US men and women. Arch Intern Med. 2002;162:1619–1624. doi: 10.1001/archinte.162.14.1619. [DOI] [PubMed] [Google Scholar]
- e35.Franco V, Oparil S. Salt sensitivity, a determinant of blood pressure, cardiovascular disease and survival. J Am Coll Nutr. 2006;25(3 Suppl):247–255. doi: 10.1080/07315724.2006.10719574. [DOI] [PubMed] [Google Scholar]
- e36.Klaus D, Middeke M, Hoyer J. Beschränkung der Kochsalzaufnahme für die Gesamtbevölkerung? Aufruf zur Gründung einer Task Force „Weniger Salz für alle“. Dtsch Med Wochenschr. 2008;133:1317–1319. doi: 10.1055/s-2008-1077261. [DOI] [PubMed] [Google Scholar]
- e37.Schmieder RE, Messerli FH, Garavaglia GE, Nunez BD. Dietary salt intake: a determinant of cardiac involvement in essential hypertension. Circulation. 1988;78:951–961. doi: 10.1161/01.cir.78.4.951. [DOI] [PubMed] [Google Scholar]
- e38.Cailar G, Mimran A, Fesler P, et al. Dietary sodium and pulse pressure in normotensive and essential hypertensive subjects. J Hypertens. 2004;22:697–703. doi: 10.1097/00004872-200404000-00011. [DOI] [PubMed] [Google Scholar]
- e39.Creager MA, Roddy M, Holland KM, et al. Sodium depresses arterial baroreceptor reflex function in normotensive humans. Hypertension. 1991;17:989–996. doi: 10.1161/01.hyp.17.6.989. [DOI] [PubMed] [Google Scholar]
- e40.Mallamaci F, Lonardis D, Billizzi V, Zoccali C. Does high salt intake cause hyperfiltration in patients with essential hypertension? J Hum Hypertens. 1996;10:157–161. [PubMed] [Google Scholar]
- e41.Cailar G, Ribstein J, Mimran A. Dietary sodium and target organ damage in essential hypertension. Am J Hypertens. 2002;15:222–229. doi: 10.1016/s0895-7061(01)02287-7. [DOI] [PubMed] [Google Scholar]
- e42.Yu HCM, Burrell LM, Black MJ, et al. Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation. 1998;98:2621–2628. doi: 10.1161/01.cir.98.23.2621. [DOI] [PubMed] [Google Scholar]
- e43.Klaus D, Gleichmann S. Bluthochdruck und kardiovaskuläre Risikofaktoren, ein Leitfaden für Arzt-Patientenseminare. 3rd Edition. Heidelberg: Deutsche Hochdruckliga; 1998. [Google Scholar]