Abstract
Background
Recent years have seen a further decline in the nationwide case fatality rate after major trauma in Germany, but it has not been clear until now whether all centers providing trauma care achieve comparable results. We have attempted to answer this question using data from the trauma registry of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie, DGU).
Methods
The standardized mortality rate of each participating center was calculated on the basis of the RISC prognostic score (Revised Injury Severity Classification) and the observed case fatality rate of the center. Results were compared across centers for the years 2004 to 2007; only the centers that provided the primary treatment of at least 100 patients during this period were included in the analysis. Data from the ten highest-scoring centers, the ten lowest-scoring centers, and the ten centers in the middle of the group were compared, and differences between them were analyzed.
Results
The case fatality rate in the top ten centers was 8.7%. The corresponding rate in the bottom ten centers was approXimately twice as high, even though the injuries treated there were of comparable severity.
Conclusion
It is evident that the fate of a trauma patient in Germany depends partly on the center in which he or she is treated. These data were drawn from a retrospective evaluation of a case registry and should be assessed in awareness of this fact.
According to the data of Germany’s Federal Statistical Office, there were 335 845 accidents resulting in personal injury in Germany in 2007. 4949 people were killed and 75 433 seriously injured in these 335 845 accidents. Following their accidents, these people require appropriate medical care. Germany has efficient hospitals that provide the various levels of care needed, but those with serious injuries should be treated in appropriate level one or level two trauma centers. Since then it has been shown that the trauma mortality rate in Germany is still falling (1). Despite this decline and the efficiency of the centers that provide care, it has not been clear until now how homogeneous care is, as measured by the mortality rate.
The trauma registry of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie, DGU) makes it possible to compare the outcomes of trauma centers involved in the trauma registry and use them as the basis for quality control (2). The authors were therefore interested in whether the results of individual centers were similar to each other or whether there were still differences between individual trauma centers, as was shown in an earlier study by Ruchholtz (2). In order to eXplore these potential differences, we compared the data from the ten highest-scoring centers, the ten lowest-scoring centers, and the ten centers in the middle of the group.
Methods
On the basis of trauma registry data, the eXpected case fatality rate for all patients in the registry and for individual centers can be determined using the Revised Injury Severity Classification (RISC) (1, 3). The RISC score is based on the following parameters (see Box) (5):
Box. Definition and scoring system of the RISC score.
-
Age:
55 years or over: –1.0 point
65 years or over: –2.0 points
75 years or over: –2.3 points
-
New ISS (Injury Severity Score):
–0.03 points per ISS point
-
Degree of head injury:
–0.5 for AIS severity level 4 (AIS, Abbreviated Injury Scale)
–1.8 for degree of severity 5/6
-
Pelvic trauma with significant blood loss (AIS 5):
–1.0 point
-
Loss of consciousness at scene of accident:
–0.9 points for a score of 3 to 5 on the Glasgow Coma Scale
-
Preclinical resuscitation:
–2.5 points
-
Base eXcess (BE):
–0.8 points for BE < –9 mmol/L
–2.7 points for BE < –20 mmol/L
-
Partial thromboplastin time (PTT):
–0.8 points for PTT 40 to 49 s
–1.0 points for PTT 50 to 79 s
–1.2 points for PTT 80 s or above
-
Number of indirect signs of bleeding:
Systolic blood pressure <90 mm Hg;
Hemoglobin <9 mg/dL;
Massive blood transfusions of more than 9 units.
Subtract 0.4 points from the score if there is 1 sign of bleeding.
Subtract 0.8 points from the score if there are 2 signs of bleeding.
Subtract 1.6 points from the score if all 3 signs of bleeding are present.
The score calculated as described above is subtracted from 5 and converted into a probability of survival using the logistical function 1/1+eXp(-X).
RISC, Revised Injury Severity Classification
Age
Overall injury severity
Degree of head injury
Pelvic trauma with significant blood loss
Preclinical resuscitation
Coagulation
Number of indirect signs of bleeding
The RISC score has been used for quality comparison between centers within the trauma registry since 2004.
To address this question, the trauma centers which had registered patients with the trauma registry in the four years from 2004 to 2007 were selected. In order to guarantee a minimum number of patients per center and minimize statistical uncertainty resulting from case numbers, the study included only centers that had registered more than 100 patients receiving primary care with the trauma registry between 2004 and 2007. The hospital mortality rate was used as the primary outcome parameter. Direct comparison of mortality rates would be misleading, due to varying injury severity, and so mortality rates were standardized according to patients’ prognoses. This was done by dividing the actual mortality rate (as a percentage) by the eXpected mortality rate (prognosis as a percentage) to give the SMR (standardized mortality rate). An SMR greater than 1 means that more patients died than eXpected, while an SMR less than 1 means a more favorable result, with fewer deaths than forecast. Prognosis is based on RISC score, developed and validated on the basis of trauma registry data.
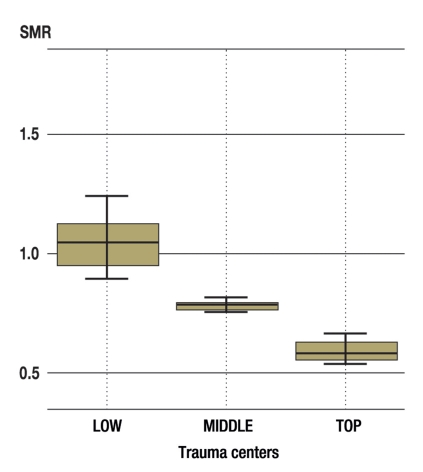
Trauma centers that met the inclusion criteria were placed in order of standardized mortality rate (SMR) and divided into three groups of 10 centers each. The 10 centers with the lowest SMRs formed the TOP group, the 10 centers around the median SMR formed the MIDDLE group, and the 10 centers with the highest SMRs were placed in the LOW group. The relevant data (age, seX, injury severity, injury pattern, RISC score, mortality rate and SMR) were evaluated for each group.
The following tests were used to determine whether any differences observed between the centers were significant: the chi-square test for frequency or percentages, and one-way analysis of variance (ANOVA) for measured values. The significance level was established using p <0.05. The data were evaluated using the statistics program SPSS 15.0. The results are given as mean values, with the corresponding standard deviations (SDs).
Evaluation was carried out using blinding, i.e., it was not known which individual centers were among the 30 trauma centers selected. Within the framework of the trauma registry, each center received a detailed summary of its own data and results; however, the data of other centers were represented only cumulatively or using blinding. Scientific analyses were carried out anonymously, using the registry as a whole.
Results
48 of the 145 trauma centers which had registered patients with the trauma registry by the end of 2007 met the inclusion criteria. On the basis of the SMRs calculated, 10 centers were assigned to each of the TOP (lowest SMRs), MIDDLE (median SMRs) and LOW (highest SMRs) groups. A total of 7725 patients received primary care at the 30 centers within the period covered by the study (table 1). The data of 6522 of these 7725 patients were complete enough for their prognoses to be assessed using the RISC score. The analysis and evaluation below are based on the data of these 6522 patients.
Table 1. Total patient population in the four years from 2004 to 2007.
| Total (n) | Surviving (n) | Deceased (n) | |
| TOP | 3492 (100%) | 3211 (92%) | 281 (8%) |
| MIDDLE | 2285 (100%) | 1995 (87.3%) | 290 (12.7%) |
| LOW | 1948 (100%) | 1622 (83.3%) | 326 (16.7%) |
| Total | 7725 (100%) | 6828 (88.4%) | 897 (11.6%) |
TOP: “best 10” trauma centers;
MIDDLE: “middle 10” trauma centers;
LOW: “10 least successful” trauma centers
Significant differences were revealed between the numbers of patients treated and the levels of care provided at the trauma centers in the three groups (TOP, MIDDLE and LOW). Thus 92.9% of the 2745 patients in the TOP group of centers received maXimum care, whereas 77.2% of the 1691 patients in the LOW group of centers received maXimum care. Table 2 shows the numbers of patients treated and the level of care in each group.
Table 2. Patient numbers and levels of care.
| Total | TOP | MIDDLE | LOW | |
| Level one trauma centers/ patients (n) | 87.7% / | 92.9% / | 89% / | 77.2% / |
| 5711 | 2549 | 1856 | 1306 | |
| Level two trauma centers/patients (n) | 12.3% / | 7.1% / | 11% / | 28.8% / |
| 811 | 196 | 230 | 385 | |
| Total | 6522 | 2745 | 2086 | 1691 |
Overall differences: p <0.001, X2 = 240.3, DF = 2;
Differences between TOP and LOW: p <0.001, X2 = 223.1, DF = 1;
TOP: “best 10” trauma centers;
MIDDLE: “middle 10” trauma centers;
LOW: “10 least successful” trauma centers
DF, degree of freedom
Some of the differences between the groups’ general data such as age, seX, preeXisting medical conditions, severity of injury, injury pattern (blunt, penetrating, injury distribution) were significant (table 3).
Table 3. General patient characteristics.
| Total | TOP | MIDDLE | LOW | Overall difference | Difference between TOP and LOW | |
| Age, years (mean, SD) | 42.2 (20.6) | 41.3 (20.7) | 42.7 (19.9) | 43.3 (14.1) | p = 0.003 | p = 0.002 |
| F = 5.88; DF = 2 | t = –3.14; DF = 4434 | |||||
| Men | 73% | 72% | 74% | 72% | p = 0.32 | p = 0.22 |
| X2 = 0.3; DF = 2 | X2 = 0.2; DF = 1 | |||||
| PreeXisting medical conditions | 33% | 33% | 30%* | 36% | p = 0.001 | p = 0.026 |
| X2 = 13.6; DF = 2 | X2 = 5.0; DF = 1 | |||||
| Blunt trauma | 94% | 94% | 95% | 92% | p <0.001 | p <0.001 |
| X2 = 19.2; DF = 2 | X2 = 14.4; DF = 1 | |||||
| AIS thoraX ≥3 | 47% | 47% | 42%* | 52% | p <0.001 | p = 0.004 |
| X2 = 40.2; DF = 2 | X2 = 8.3; DF = 1 | |||||
| AIS abdomen ≥3 | 15% | 15% | 15% | 17% | p = 0.08 | p = 0.08 |
| X2 = 4.9; DF = 2 | X2 = 3.1; DF = 1 | |||||
| AIS eXtremities ≥3 | 34% | 32% | 36%* | 36% | p = 0.004 | p = 0.006 |
| X2 = 10.9; DF = 2 | X2 = 7.7; DF = 1 | |||||
| AIS head ≥3 | 42% | 41% | 42% | 42% | p = 0.52 | p = 0.50 |
| X2 = 1.3; DF = 2 | X2 = 0.5; DF = 1 | |||||
| ISS (mean, SD) | 23.2 (14.8) | 23.1 (14.9) | 22.8 (15.2) | 23.7 (14.1) | p = 0.17 | p = 0.18 |
| F = 1.75; DF = 2 | t = –1.33; DF = 4434 |
*Differences significant, data not shown
SD, standard deviation; TOP, “best 10” trauma centers; MIDDLE, “middle 10” trauma centers;
LOW, “10 least successful” trauma centers; AIS, Abbreviated Injury Scale; ISS: Injury Severity Score; DF, degree of freedom
By definition, there were considerable differences between the groups’ actual case fatality rates and SMRs. Thus the case fatality rate in the LOW group is almost twice that of the TOP group, even though the prognoses calculated using RISC scores forecast similar case fatality rates for all three groups (Table 4, Figure). There are highly significant differences in the actual case fatality rates, although there were no significant differences in the forecast case fatality rates calculated for the three groups.
Table 4. Predicted and actual fatality rates.
| Total | TOP | MIDDLE | LOW | Total difference | Difference between TOP and LOW | |
| Died in hospital (n; %) | 784 | 238 | 265 | 281 | p <0.001 | p <0.001 |
| 12.0% | 8.7% | 12.7%* | 16.6% | X2 = 63.8; DF = 2 | X2 = 64.0; DF = 1 | |
| Fatality rate predicted by RISC (%) | 15.4 | 14.9 | 16.3 | 15.1 | p = 0.17 | p = 0.75 |
| F = 1.75; DF = 2 | t = –0.33; DF= 4434 | |||||
| Standardized mortality rate (SMR) with 95% confidence interval | 0.78 | 0.58 | 0.78 | 1.10 | ||
| 0.73–0.83 | 0.51–0.66 | 0.69–0.87 | 0.98–1.22 |
*Differences significant, data not shown
TOP, “best 10” trauma centers; MIDDLE, “middle 10” trauma centers;
LOW, “10 least successful” trauma centers; RISC, Revised Injury Severity Classification; DF, degree of freedom
Figure.
Comparison of the standardized mortality rates (SMR) of the three groups. An SMR of 1 means that case fatality rate matches the fatality rate forecast using the RISC (Revised Injury Severity Classification) score. SMR <1 shows that more patients survive than forecast, and SMR >1 corresponds to a less favorable result, with more patients dying than forecast (TOP, “best 10” trauma centers; MIDDLE, “middle 10” trauma centers; LOW, “10 least successful” trauma centers).
Table 1 also shows that the TOP centers cared for more patients than the other two groups and that case fatality rate is inversely proportional to the number of patients cared for.
Overall, the results show a significant difference in the quality of care provided at individual centers.
Discussion
Although the trauma mortality rate in Germany has continued to fall in recent years and was 12% for the patients registered with the trauma registry in 2007 (4), the results show that there are significant differences in the treatment outcomes of individual centers. The reasons for this difference in outcome quality needs to be addressed in future research; they are certain to be compleX. Differences in patient characteristics may be a reason for the differences in case fatality rates; statistically significant variations are not necessarily clinically significant differences (average age in the TOP group: 41.26; LOW group: 43.29; p = 0.003). Other possible reasons for the observed results may be differences in trauma room care, intensive care, or preclinical treatment. Trauma room care, for eXample, varies greatly between individual centers in Germany. Some centers favor early complete diagnosis using full-body CTs (5), while others prefer conventional step-by-step diagnosis (6).
Which of these approaches is more beneficial has not been clearly established and needs to be evaluated in future research. The eXclusion of the 1203 datasets for which no RISC score could be calculated cannot completely rule out distortion of results. However, the results shown in Table 1 demonstrate that the case fatality rates are even more favorable in the TOP group if these 1203 datasets are taken into account, whereas there are almost no differences in the other two groups.
Varying outcomes of trauma care are not a new phenomenon and have already been shown in earlier research (7, 8). It was known as early as the 1980s that there were considerable regional differences in trauma care (9). An initial trauma documentation system was established in the USA on the assumption that individual regions could learn from each other via systematic recording of beneficial and undesirable practices (10). Once the advantages of such documentation systems became clear, the German Society for Trauma Surgery established the German trauma registry, thanks to which a documentation and quality assurance system was created that makes research such as this possible.
In addition to differences between centers in a single country, differences between countries can also be seen. Thus the Helsinki Trauma Outcome Study (11) shows that in terms of case fatality rates trauma care in Helsinki, Finland is more effective than in England. Earlier research has also shown differences in the quality of care at trauma centers and non-trauma centers. Thus the case fatality rates of American trauma centers were lower than those of non-trauma centers (12). Biewener et al. (13) found similar superiority of patient care at trauma centers in Germany.
As this study only includes centers which treated at least 25 seriously injured patients per year and are also part of the trauma registry of the German Society for Trauma Surgery, it can be assumed that the centers included are regional and national trauma centers. This is shown by the levels of care of the centers included in the research as stated in Table 2, as this study includes only level one and level two trauma centers. This means that the centers in the German Society for Trauma Surgery’s trauma network (www.dgu-traumanetzwerk.de, in German) are classified according to their level of care within the German health-care system. This means that the identified difference in case fatality rates is not due to different levels of care of the included centers, i.e. basic and standard care versus maXimum care. It is clear, however, that in the TOP group significantly more patients were treated at level one trauma centers.
Nevertheless, it is also clear that level two trauma centers achieve favorable outcomes too and that being a level one trauma center does not automatically lead to favorable outcomes. As stated above, the inclusion criterion of at least 100 seriously injured patients cared for during the period covered by the study means that all basic and standard care centers were eXcluded from this work. This might be viewed as a limitation of this study, as no conclusions can be drawn on the quality of care of these facilities. However, this work was intended not to compare the outcomes of all facilities involved in trauma care but to investigate “trauma centers” with a minimum of eXpertise in care for seriously injured patients.
In addition to the higher proportion of patients receiving maXimum care, it is also clear that the number of patients treated within the three groups falls significantly. Thus 42% of patients in the TOP group, 32% of those in the MIDDLE group, and 26% of those in the LOW group received maXimum care. Taking the whole study population as our basis, during the period covered by the study a yearly average of 87 seriously and very seriously injured patients received primary care at a trauma center in the TOP group, 57 in the MIDDLE group, and 49 in the LOW group. This leads to the well-known conclusion that the quality of care increases with the number of patients treated. Haas et al. (14) therefore stipulated a minimum of 300 to 400 polytrauma patients per trauma center in order to guarantee high quality of treatment. It is difficult or impossible for even the TOP centers included in this study to achieve this number of patients. The trauma registry’s 2008 Annual Report mentions one center that cared for more than 300 patients and another five centers that treated more than 200 patients (4). However, only 100 to 200 seriously and very seriously injured patients per year are actually treated in level 1 trauma centers in Germany (15). In the conteXt of these figures, the above-mentioned requirement for 300 to 400 seriously injured patients per trauma center seems too high. Patient numbers as high as those stipulated by Haas would probably eXceed the intensive care capacity of most German trauma centers.
The authors have used the standardized mortality rate (SMR), which as stated above is calculated on the basis of prognosis scores and actual case fatality rates, to develop a ranking of the centers that submitted data to the trauma registry. The RISC (Revised Injury Severity Classification) score has been used to estimate prognoses in the trauma registry since 2004 (1). It is validated using the entire patient population of the trauma registry and provides more accurate prognoses than TRISS (Trauma Injury Severity Score), which was used until 2003. TRISS, which is based on data from the American/Canadian Major Trauma Outcome Study, now gives major underestimates of patients’ prognoses. In other words, significantly more patients survive than predicted by TRISS. As a result, there have long been efforts to improve the accuracy of TRISS’s prognoses (16– 18). RISC validated by the trauma registry provides significantly better forecasts of fatality rates, although there has also been a slight tendency in recent years to underestimate prognoses, which is significant for trauma registry data gathered since 2005 (1). Thus the case fatality rates in the trauma centers in the TOP and MIDDLE groups of this study are significantly lower than forecast according to RISC.
The data used here are taken from a registry database, which means that there are inevitably limitations. This is a retrospective study. The study is eXploratory rather than confirmatory, and so all results provided by it must be interpreted with the necessary caution. The authors therefore warn against relying too heavily on p-values. In this type of retrospective analysis, p-values do not have the same interpretation or eXplanatory power for testing hypotheses as in prospectively planned studies. In addition, the large numbers of cases in the registry make it much easier for significant differences to arise and subsequently distort the picture of the clinical significance of the difference. With trauma registry data it is impossible to refer back to potential structural differences (e.g. CTs in the trauma room or elsewhere) between the trauma centers included in the study. Potential regional differences in the quality of trauma care have not been considered. No implicit eXamination of the results took place regarding the different levels of care of the centers involved in the trauma registry, but as mentioned above it was already known that no basic or standard care centers had been included.
Conclusion
The data gathered show the difference in quality of the care provided to trauma patients at the centers which registered patients with the trauma registry of the German Society for Trauma Surgery. The case fatality rate in the LOW group was almost twice that of the centers in the TOP group, even though the fatality prognoses calculated for the patients treated were similar. We can therefore conclude that the fate of a trauma patient in Germany depends not only on the severity of his/her injuries, but also, among other factors, on the trauma center in which he/she is treated. Further research is needed to determine where the differences in care arise and to eliminate any shortcomings.
Key Messages.
There is a significant difference between the case fatality rates of trauma centers that are involved in the trauma registry of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie, DGU).
At 8.7%, the case fatality rate in the top centers is only around half that of the centers with the least successful outcomes (16.6%). This difference is not due to different of levels of care alone, as basic and standard care hospitals were not included in the research.
There is a link between treatment quality and the number of patients treated. The top centers treated an average of 1.8 times as many seriously injured patients per year as the least successful centers.
Most trauma centers have a standardized mortality rate (SMR) less than 1; this places their case fatality rates below those forecast by the RISC (Revised Injury Severity Classification) score, which highlights the high standards of trauma care in Germany.
Despite the high standards of trauma care overall, improvements to quality are still needed in order to improve the outcomes of all clinical facilities in line with the top centers.
Acknowledgments
Translated from the original German by Caroline Devitt, MA.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest eXists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Ruchholtz S, Lefering R, Paffrath T, Oestern HJ. Reduction in mortality of severely injured patients in Germany [Rückgang der Traumaletalität. Ergebnisse des Traumaregisters der deutschen Gesellschaft für Unfallchirurgie] Dtsch Arztbl Int. 2008;105(13):225–231. doi: 10.3238/arztebl.2008.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruchholtz S, Nast-Kolb D, Waydhas C, Lefering R. Das Traumaregister der AG Polytrauma der D.G.U. als Grundlage des Qualitätsmanagements in der Schwerverletztenversorgung [The trauma register of the ’Polytrauma’ Committee of the German Society of Trauma Surgery as the basis for quality management in the management of severely injured patients] Langenbecks Arch Chir Suppl Kongressbd. 1997;114:1265–1267. [PubMed] [Google Scholar]
- 3.Ruchholtz S, Lefering R, Paffrath T, Bouillon B NIS der DGU. Traumaregister der Deutschen Gesellschaft für Unfallchirurgie. Trauma Berufskrankh. 2007;9:270–278. [Google Scholar]
- 4.Lefering R Sektion NIS der DGU. Traumaregister der DGU. Jahresbericht 2008. Traumaregister. 2008 www.traumaregister.de. [Google Scholar]
- 5.Hilbert P, zur Nieden K, Hofmann GO, Hoeller I, Koch R, Stuttmann R. New aspects in the emergency room management of critically injured patients: a multi-slice CT-oriented care algorithm. Injury. 2007;38:552–558. doi: 10.1016/j.injury.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 6.Waydhas C, Kanz KG, Ruchholtz S, Nast-Kolb D. Algorithmen in der Traumaversorgung [Algorithms in trauma management] Unfallchirurg. 1997;100:913–921. doi: 10.1007/s001130050212. [DOI] [PubMed] [Google Scholar]
- 7.Ruchholtz S. Das Traumaregister der DGU als Grundlage des interklinischen Qualitätsmanagements in der Schwerverletztenversorgung [The Trauma Registry of the German Society of Trauma Surgery as a basis for interclinical quality management. A multicenter study of the German Society of Trauma Surgery] Unfallchirurg. 2000;103:30–37. doi: 10.1007/s001130050005. [DOI] [PubMed] [Google Scholar]
- 8.Helm M, Kulla M, Birkenmaier H, Lefering R, Lampl L. Traumamanagement unter militärischen Einsatzbedingungen [Trauma management under military conditions. A German field hospital in Afghanistan in comparison with the National Trauma Registry] Chirurg. 2007;78:1130–1136. doi: 10.1007/s00104-007-1383-8. [DOI] [PubMed] [Google Scholar]
- 9.Probst C, Richter M, Haasper C, Lefering R, Otte D, Oestern HJ, Krettek C, Hufner T. Trauma- und Unfalldokumentation in Deutschland [Trauma and accident documentation in Germany compared with elsewhere in Europe] Chirurg. 2008;79:650–656. doi: 10.1007/s00104-008-1498-6. [DOI] [PubMed] [Google Scholar]
- 10.Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, Jr, Flanagan ME, Frey CF. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30:1356–1365. [PubMed] [Google Scholar]
- 11.Handolin L, Leppäniemi A, Lecky F, Bouamra O, et al. Helsinki Trauma Outcome Study 2005: Audit on outcome in trauma management in adult patients in southern part of Finland. Eur J Trauma Surg. 2008;34(6):570–576. doi: 10.1007/s00068-007-7129-y. 10.1007/s00068-007-7129-y. [DOI] [PubMed] [Google Scholar]
- 12.Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of traumacenter care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 13.Biewener A, Aschenbrenner U, Sauerland S, Zwipp H, Rammelt S, Sturm J. Einfluss von Rettungsmittel und Zielklinik auf die -Letalität nach Polytrauma [Impact of rescue method and the destination clinic on mortality in polytrauma. A status report] Unfallchirurg. 2005;108:370–377. doi: 10.1007/s00113-005-0928-x. [DOI] [PubMed] [Google Scholar]
- 14.Haas NP, von Fournier C, Tempka A, Sudkamp NP. Traumazentrum 2000 Wieviele und welche Traumazentren braucht Europa um das Jahr 2000? [Trauma center 2000. How many and which trauma centers does Europe need around the year 2000?] Unfallchirurg. 1997;100:852–858. doi: 10.1007/s001130050204. [DOI] [PubMed] [Google Scholar]
- 15.Kuhne CA, Ruchholtz S, Buschmann C, Sturm J, Lackner CK, Wentzensen A, Bouillon B, Waydhas C, Weber C. Polytraumaversorgung in Deutschland [Trauma centers in Germany. Status report] Unfallchirurg. 2006;109:357–366. doi: 10.1007/s00113-005-1049-2. [DOI] [PubMed] [Google Scholar]
- 16.Moore L, Lavoie A, Turgeon AF, Abdous B, Sage NL, Emond M, Liberman M, Bergeron E. The trauma risk adjustment model: a new model for evaluating trauma care. Ann Surg. 2009;249:1040–1046. doi: 10.1097/SLA.0b013e3181a6cd97. [DOI] [PubMed] [Google Scholar]
- 17.Moore L, Lavoie A, LeSage N, Abdous B, Bergeron E, Liberman M, Emond M. Statistical validation of the Revised Trauma Score. J Trauma. 2006;60:305–311. doi: 10.1097/01.ta.0000200840.89685.b0. [DOI] [PubMed] [Google Scholar]
- 18.Osler TM, Rogers FB, Badger GJ, Healey M, Vane DW, Shackford SR. A simple mathematical modification of TRISS markedly improves calibration. J Trauma. 2002;53:630–634. doi: 10.1097/00005373-200210000-00002. [DOI] [PubMed] [Google Scholar]