Abstract
Background
Diseases of the pituitary gland can lead to the dysfunction of individual hormonal axes and to the corresponding clinical manifestations. The diagnostic assessment of pituitary function has not yet been standardized.
Methods
The members of the Neuroendocrinology Section and the Pituitary Study Group of the German Society for Endocrinology (Deutsche Gesellschaft für Endokrinologie) prepared outlines of diagnostic methods for the evaluation of each of the pituitary hormonal axes. These outlines were discussed in open session in recent annual meetings of the Section and the Study Group.
Results
For the evaluation of the thyrotropic axis, basal TSH and free T4 usually suffice. For the evaluation of the gonadotropic axis in men, the testosterone level should be measured; if the overall testosterone level is near normal, then calculating the free testosterone level may be additionally useful. In women, an intact menstrual cycle is sufficient proof of normal function. In the absence of regular menstruation, measurement of the basal estradiol and gonadotropin levels aids in the diagnosis of the disturbance. For the evaluation of the adrenocorticotropic axis, the basal cortisol level may be helpful; provocative testing is in many cases necessary for precise characterization. The evaluation of the somato-tropic axis requires provocative testing. Aside from the insulin tolerance test, the GHRH-arginine test has become well established. Reference ranges normed to the body mass index (BMI) are available.
Conclusion
The diagnostic evaluation of pituitary insufficiency should proceed in stepwise fashion, depending on the patient’s clinical manifestations and underlying disease. For some pituitary axes, measurement of basal hormone levels suffices; for others, stimulation tests are required. In general, the performance of combined pituitary tests should be viewed with caution.
Pituitary dysfunction can be caused by a wide variety of diseases affecting the hypothalamus and pituitary gland and can produce major clinical manifestations, including pituitary coma. Pituitary adenomas are probably much more common than previously assumed; their prevalence is roughly 1 per 1000 people (1). The known causes of pituitary dysfunction include tumor, hemorrhage, surgery, and radiotherapy. In recent years, deficits of individual pituitary axes after head trauma have come to be recognized as a clinically relevant problem. Because of this newly appreciated entity, the prevalence of pituitary dysfunction is likely to be much higher than the previous estimate of 0.5 per 1000 people (2). Once hormonal deficits have been diagnosed, they can be treated by supplementation (figure 1), so that the patient’s quality of life becomes nearly normal. The performance of pituitary function tests is erratic in current clinical practice. Pitfalls to be avoided include not just false-positive test results leading to unnecessary (and costly) hormone supplementation, but also false-negative test results leading to the inadequate supplementation of vitally important hormones. There are no published guidelines in this field, with the sole exception of guidelines for the diagnosis of growth hormone deficiency (e1, e2). The publications that are available mostly provide a low level of evidence (grade III). In the present article, which consists of expert opinion (evidence level IV), we point out difficulties and sources of error in the performance and interpretation of endocrinological tests of pituitary function. This discussion explicitly concerns patients for whom abnormal function of the hypothalamus and pituitary gland is considered to be highly probable.
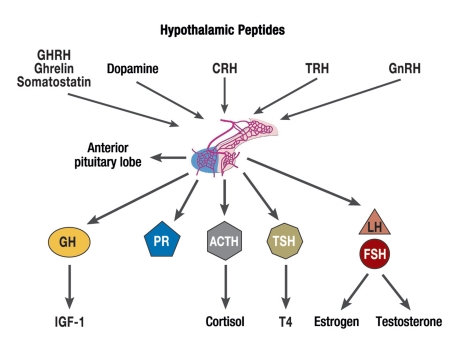
Figure 1.
Hormones of the anterior pituitary lobe, their regulation by hypothalamic peptides, and the hormones of the peripheral endocrine glands that are under their control
GHRH, growth-hormone-releasing hormone;
CRH, corticotropin-releasing hormone;
TRH, thyrotropin-releasing hormone;
GnRH, gonadotropin-releasing hormone;
GH, growth hormone;
IGF-1, insulin-like growth factor 1;
PR, prolactin;
ACTH, adrenocorticotropic hormone;
TSH, thyroid-stimulating hormone;
T4, thyroxine;
LH, luteinizing hormone;
FSH, follicle-stimulating hormone
Methods
Outlines of testing procedures for the individual pituitary axes were prepared by members of the Neuroendocrinology Section and the Pituitary Working Group of the German Society for Endocrinology (Deutsche Gesellschaft für Endokrinologie). These experts made use of relevant sources in the literature that were retrieved by a search of the PubMed database. The drafts that they submitted were discussed in open session at the annual meetings of the Neuroendocrinology Section and the Pituitary Working Group. The resulting expert opinions are summarized here. It should be noted that this work does not represent a comprehensive review of the literature.
Results
Testing of the thyrotropic axis
The clinical presentation of central hypothyroidism resembles that of primary hypothyroidism due to loss of function of the thyroid gland itself. Current, sensitive testing methods generally enable a diagnosis by measurement of the basal thyroid-stimulating hormone (TSH) and free thyroxin (fT4) levels. The fT3 level should not be measured, as its precise determination remains problematic. In unambiguous cases of central hypothyroidism, the fT4 level is low and the TSH level is either low or inappropriately normal, in contrast to the elevated TSH level seen in primary hypothyroidism. Problems of interpretation can arise when the fT4 and TSH levels are both in the low normal range. The secretion of immunogenic, but less biologically active TSH can be reflected in a measurement of high-normal or mildly elevated TSH levels (3), mimicking the findings of incipient (subclinical) primary hypothyroidism. In case of doubt, follow-up studies can help clarify the situation (e3). A comparison with thyroid values obtained earlier, when the patient’s thyroid function was still normal, can also help, because there is normally little intra-individual variation in thyroid values (4). This fact is especially useful when the patient’s thyrotropic function was normal before a surgical procedure and requires diagnostic assessment afterward.
The thyrotropin-releasing hormone (TRH) test (Table 1) normally produces an absolute rise of the TSH level by roughly 1.5 to 45 mU/L, and a relative rise to a value that is 2.8 to 23 times higher than baseline (e4). This test is not recommended for routine use (5, 6), because its results vary widely among both normal and ill subjects and can be influenced by many extraneous factors (e3, e5), yet it can provide helpful additional information in individual cases where the basal TSH and fT4 levels are difficult to interpret. It is also generally well tolerated, with few and mild side effects. Transient nausea, headache, dizziness, mild hypertension, gustatory sensations, flushing, and urinary urgency have been observed after a TRH challenge, and epileptic seizures can occur in children with epilepsy or a low seizure threshold. Pituitary apoplexy after TRH administration has been reported in a few cases of patients with pituitary macroadenoma (e6); thus, the TRH test should not be performed in patients with large pituitary tumors.
Table. Overview of some commonly performed tests of pituitary function and remarks on practical aspects, the hormones to be measured, and the timing of blood drawing.
| Test | Method of performance | Remarks | Hormones to be measured | Blood drawing |
| TRH test | 1 amp (200 µg) TRH Duration of injection: >60 sec | Note: apoplexy occurs very rarely with large macroadenomas | TSH | 0 min before |
| injection | ||||
| then 30 min | ||||
| GnRH test | 1 amp (100 µg) LHRH Duration of injection: <30 sec | Note: apoplexy occurs very rarely with large macroadenomas | LH, FSH | 0 min before |
| injection, | ||||
| then 30 min | ||||
| IHT | 0.15 IU/kg BW regular insulin IV (in renal failure 0.1 IU/kg BW, for patients with abnormal glucose tolerance or acromegaly 0.2 IU/kg BW) | Patient fasting CI: epilepsy, CHD Secure venous access with an indwelling catheter A predrawn syringe with 20% glucose should be readily accessible in case of need Trained personnel should be near the patient at all times | GH, cortisol (- ACTH) | 0 min before |
| injection, then | ||||
| 15 min, 30 min, | ||||
| 45 min, 60 min, | ||||
| 90 min, 120 min | ||||
| CRH test | CRH 1 µg/kg BW IV, to be given immediately after dissolution. Duration of injection: <30 sec | Cortisol (- ACTH) | 0 min before | |
| injection, then | ||||
| 15 min, 30 min, | ||||
| 45 min, 60 min | ||||
| ACTH test | 1 amp (250 µg) ACTH 1–24 solution for injection IV (must be shielded from light in refrigerator and in package). Shake before injection. Duration of injection: <30 sec | Cortisol | 0 min before | |
| injection, | ||||
| then 30 min, | ||||
| 60 min | ||||
| GHRH/arginine test | GHRH 1µg/kg BW IV (can be stored at room temperature), use immediately after dissolution Duration of injection: <30 sec. then, infusion of 30 g arginine in 21.07% solution (7 amp = 30 g) over 30 min, diluted in normal saline. note: lower the arginine dose if bw <60 kg: give half the bw in grams, e.g., 50 kg → 25 g | Patient fasting | GH | 0 min before |
| injection, | ||||
| then 30 min, | ||||
| 45 min, 60 min, | ||||
| 90 min |
There are many variations of the techniques above, particularly relating to the timing of blood draws. TRH, thyrotropin-releasing hormone; GnRH, gonadotropin-releasing hormone; IHT, insulin-hypoglycemia test; CRH, corticotropin-releasing hormone; ACTH, adrenocorticotropic hormone; GHRH, growth-hormone-releasing hormone; GH, growth hormone; CI, contraindications, CHD, coronary heart disease
Testing of the gonadotropic axis
The main symptoms of hypogonadism in men are loss of libido and infertility. When hypogonadism arises suddenly, hot flashes can occur in men as they do in women. Loss of muscle mass, lack of energy, and osteoporosis develop only later on in the course of illness. Clinical signs such as involution of the testes, loss of secondary hair, or gynecomastia can arise, but are not consistent or reliable indicators of the condition.
Serum testosterone levels vary in a circadian rhythm and are highest in the early morning hours. Free, physiologically active testosterone accounts for only about 1% to 2% of the total testosterone level, as most of the total testosterone is bound to albumin and to sex-hormone binding globulin (SHBG) (e7). Formulae for calculating the free testosterone level are currently the most precise means of estimating it, while the usefulness of measuring free testosterone with an analog assay is questionable. The formula of Vermeulen et al. (7), for example, can be used to calculate the free testosterone level from the total testosterone level and the levels of albumin and SHBG (for an online calculator, see www.issam.ch). Male hypogonadism is diagnosed by the repeated measurement of low morning testosterone levels, i.e., total testosterone levels below 10.4 nmol/L (300 ng/dL) and free testosterone levels below 0.255 nmol/L (7 ng/dL) (e8). When the total testosterone level is in borderline range (10–12 nmol/L), the presence or absence of typical clinical manifestations plays an accessory role in diagnosis. The threshold values to be used in individual cases differ depending on the particular assay used, as well as on the patient’s age and body-mass index.
Secondary hypogonadism is diagnosed on the basis of the patient’s history, the physical findings, and the measurement of inappropriately low levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), with a simultaneously low testosterone level (e9). If secondary hypogonadism is found, hyperprolactinemia must be ruled out as a possible cause. In adult patients with classic secondary hypogonadism, dynamic function tests can often be dispensed with. Thus, testing the gamut of all pituitary axes with a combined pituitary test is obsolete for the type of patients under discussion in this article. A GnRH (gonadotropin-releasing hormone) test (table) can be performed to help make the difficult distinction between constitutional delay of puberty and secondary hypogonadism, under consideration of the normal values for the patient’s age and pubertal stage (8– 10). It can also aid in the differential diagnosis of partial androgen deficiency in an aging man (late-onset hypogonadism, LOH) from secondary hypogonadism: pituitary hypogonadism—caused, for example, by a macroadenoma—is definitively ruled out only if the LH level rises above 15 mU/L (11).
In a premenopausal woman, a normal ovulatory cycle proves the patient is not suffering from hypogonadism. Women taking oral contraceptives (OC) are an exception to this rule; thus, OC should be discontinued for at least two months before a diagnostic assessment is performed. Inappropriately low gonadotropin levels in the face of low estradiol levels indicate secondary hypogonadism. In postmenopausal women, the gonadotropin levels are physiologically elevated, and thus levels in the “normal” range also indicate secondary hypogonadism.
Testing of the corticotropic axis
If the cortisol level fails to rise adequately in response to stress, the clinical syndrome of acute adrenal failure can arise, with life-threatening shock. In most cases, however, hypocortisolism develops gradually and manifests itself with nonspecific symptoms and signs such as nausea, vomiting, abdominal pain, loss of energy, fatigue, fever, and impaired alertness, as well as hypoglycemia after prolonged fasting.
An 8 a.m. serum cortisol level may suffice for diagnostic purposes. Because of the circadian rhythmicity of cortisol secretion, standardized blood drawing at one particular time of day with well-defined normal values is of particular importance. If levels at 8 a.m. are repeatedly low, i.e., below 80 to 110 nmol/L, then adrenal insufficiency is highly likely (12) (e10– e12) and supplementation can be recommended right away. On the other hand, values above 470 to 500 nmol/L rule out adrenal insufficiency (e10, e12). If the measured values lie between these upper and lower thresholds, then further study with provocative testing is needed, yet about one-quarter of all such patients can be spared such testing (e13).
The insulin-hypoglycemia test (IHT) (table) is still recommended as the gold standard for functional testing of the entire hypothalamic-pituitary-adrenocortical (HPA) axis in a physiologically relevant stressful situation. It should not be performed in the face of contraindications such as cerebrovascular and cardiovascular disease or epilepsy. As the induced hypoglycemia may have critical effects, a physician should be present during the entire test. Insulin is given intravenously in a dose of 0.15 IU/kg body weight (BW) (0.1 IU/kg BW if there is a high suspicion of adrenal insufficiency, or 0.2 IU/kg BW in patients with diabetes mellitus or acromegaly), and the serum cortisol level is measured 0, 15, 30, 45, 60, 90, and 120 minutes after the injection. For reliable evaluation, published studies have required blood sugar values below 36 to 40 mg/dL combined with clinical signs of hypoglycemia, although a systematic study has shown that the adrenocorticotropic hormone (ACTH) level is certain to rise only if the glucose level drops below 29 mg/dL (13). If an adequate effect has not been obtained by 30 minutes after insulin administration, a second dose of insulin should be given that is 1.5 times larger than the first. The absolute cortisol peak is the important value for diagnosis; the percentage rise cannot be used for reliable evaluation (e10).
The threshold value for a physiological reaction is derived from a comparison with the maximal cortisol concentrations reached during surgery, myocardial infarction, or sepsis. Most publications take a peak cortisol level of 500 nmol/L as the threshold value, but there have been no randomized studies on the long-term course of illness as a function of the cortisol response (e14). The reproducibility of the IHT was studied in three trials on normal subjects and was described as good, with variation coefficients ranging from 7% to 12% (13, e15, e16). One of these studies also included patients with pituitary insufficiency and found the IHT to be much less reproducible in these patients, with a variation coefficient of 41.6% (e15). In this study, the patients—unlike the normal subjects—were given intra- and interindividually variable doses of glucose after hypoglycemia was reached. In a prospective comparison of two groups of 50 children with growth retardation, glucose administration of this type was found to lead to significantly lower cortisol levels (14). On the other hand, a study in healthy adults revealed no significant difference in IHT results when the test was performed with or without additionally administered glucose (e17), although there were large intraindividual variations of the cortisol peak. In accordance with these findings, the extent and duration of hypoglycemia seem to be correlated with the height of the cortisol peak (13). In the absence of data from further studies, it follows that additional glucose should not be given during the test unless clinically necessary.
The metyrapone test is also used to study the integrity of the entire HPA axis. The patient is given 2.5 to 3 grams of metyrapone by mouth at midnight and blood is drawn in the morning for measurement of 11-deoxycortisol. As the enzyme blockade on which this test relies can provoke acute adrenal insufficiency, it is usually performed on an inpatient basis, and only in a few institutions (15). In the corticotropin-releasing hormone (CRH) test (table), exogenously administered human CRH stimulates pituitary secretion of ACTH (16). Typically, CRH is given intravenously in a dose of 1 µg/kg BW and the cortisol level is measured every fifteen minutes for one hour. The important value for diagnosis is the absolute cortisol peak; the interpretation of the percentage rise has not been found to be reliable, at least in the diagnosis of possible adrenal insufficiency of organic origin (12). Peak values above 514–615 nmol/L rule out adrenal insufficiency with near certainty, while values below 349–420 nmol/L make it highly likely (12, 17). CRH testing has a lower diagnostic yield than IHT, providing a diagnosis in only 18% of patients whose problem could not be diagnosed by basal cortisol measurement alone.
In the ACTH test (table), 250 micrograms of ACTH 1–24 are given intravenously, and the serum cortisol level is measured 30 to 60 minutes later (e18). In secondary adrenal insufficiency, the Synacthen-induced rise in cortisol should be lower because of partial atrophy of the zona fasciculata of the adrenal gland, providing indirect evidence of an intact HPA axis. The reported sensitivity of the ACTH test for adrenal insufficiency, with threshold values for the cortisol peak lying between 500 and 600 nmol/L, varies greatly from study to study, ranging from less than 50% to almost 100% (e19, e20). A meta-analysis came to the conclusion that, in view of the limited sensitivity of the ACTH test, other tests involving stimulation of higher centers should be used when secondary adrenal insufficiency is suspected (18). On the other hand, long-term follow-up studies have shown that the ACTH test has a high predictive accuracy for the exclusion of clinically relevant secondary adrenocortical insufficiency (e21). The test should be performed at least three months after the suspected causative event (e.g., surgery), so that adrenocortical atrophy can take place in the meantime (e22, e23). A variant form of the test in which only 1 µg of ACTH is given, the so-called low-dose ACTH test, is said by some authors to be more sensitive than the conventional ACTH test for the diagnosis of partial secondary adrenocortical insufficiency (e19), although others have found no difference (19, e24). An important argument in favor of the conventional ACTH test is that ACTH 1–24 only comes in 250 µg ampoules. Dilution may lead to testing errors because of adsorption of the peptide drug to container surfaces, among other reasons.
Testing of the somatotropic axis
Lack of secretion of growth hormone (GH) causes no immediately apparent symptoms in adults. Thus, suspected GH deficiency can be confirmed only by measurement of hormone levels. Single GH values are inadequate for this purpose, because GH is secreted in pulsatile fashion, and its concentration between pulses normally lies below the detection threshold of very sensitive assays. Likewise, a single measurement of the insulin-like growth factor 1 (IGF-1) concentration usually does not suffice to demonstrate GH deficiency, as the level may be normal even if GH deficiency is severe (20, e25). Very low IGF-1 values (e.g., below 77.2 µg/L [21]) do, however, indicate GH deficiency with a high degree of certainty. The IGF-1 concentration is also low in malnutrition, poorly controlled diabetes mellitus, liver disease, and hypothyroidism.
Stimulation tests are indispensable for the reliable functional assessment of the somatotropic hormonal axis. A basic requirement is that the diagnosis of growth hormone deficiency in an adult patient should be supported by at least two tests. An exception to this rule can be made if more than one other pituitary axis has also been found to be deficient. The tests must be performed with the patient in the fasting state, because glucose suppresses growth hormone. The threshold values given here (and elsewhere) are subject to variability based on the particular assay used, because assays differ markedly from one another in the determination of absolute concentrations, particularly in the low-concentration range.
IHT is considered the gold standard for adults. A GH peak lower than 3 µg/L is very strong evidence for GH deficiency, while a value above 5 µg/L essentially rules it out (22). The reproducibility of the IHT is reportedly poor (e15, e16, e26). The GHRH (growth-hormone-releasing hormone)-arginine test (table) combines somatostatin suppression by arginine (23) with direct pituitary GH stimulation by GHRH and therefore produces a large rise in GH in healthy individuals (24, e27). The stimulating effect of arginine, when given alone, is small (e28). GHRH directly stimulates pituitary GH secretion and thus cannot be used as the sole testing substance when a disturbance above the level of the pituitary is suspected, e.g., in head trauma (e27, e29). No threshold values have yet been established for testing with GHRH alone to diagnose GH deficiency in adults. The maximal GH concentration achieved in the GHRH-arginine test is far above that achieved in the IHT; therefore, the diagnostic value of the GHRH-arginine test for GH deficiency in adults is currently a matter of debate (e30). The proposed threshold values in this test for the diagnosis of GH deficiency depend on the patient’s body-mass index (BMI): 11.5 µg/L for patients whose BMI is under 25 kg/m2, 8.0 µg/L for overweight patients (BMI between 25 and 30 kg/m2), and 4.2 µg/L for obese patients (BMI above 30 kg/m2) (25). The GHRH-arginine test is considered to be more reproducible than the IHT (22) and is probably the best alternative to the IHT if the latter is contraindicated or has yielded inconclusive results. The GHRH-arginine test may cause nausea and a fall in blood pressure. It has no medical contraindications.
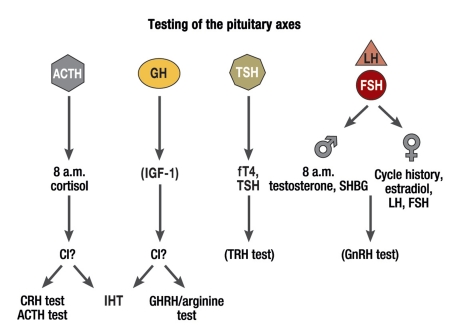
Figure 2.
Structured assessment of basal pituitary hormones followed by evaluation with dynamic testing methods
The relevant anterior pituitary axes are shown in the upper portion of the diagram as in Figure 1, while the steps to be followed in endocrinological assessment are shown in the lower portion.
CI, contraindications;
IGF-1, insulin-like growth factor 1;
fT4, free thyroxine;
TSH, thyroid-stimulating hormone;
LH, luteinizing hormone;
FSH, follicle-stimulating hormone;
CRH, corticotropin-releasing hormone;
ACTH, adrenocorticotropic hormone;
IHT, insulin hypoglycemia test;
GHRH, growth-hormone-releasing hormone;
TRH, thyrotropin-releasing hormone;
GnRH, gonadotropin-releasing hormone;
SHBG, sex-hormone binding globulin
Key Messages. Practical pituitary function testing.
Testing of the pituitary axes makes sense only for patients who are considered likely to have a pathological alteration of the pituitary gland, such as a pituitary tumor or changes resulting from surgery or radiation of the sellar region or from head trauma. There is no rational way to interpret pituitary function tests that have been ordered without an adequate indication.
Because of the many potential sources of error, the basal hormone levels should be interpreted by an endocrinologist, and stimulation tests should likewise be carried out and evaluated by an endocrinologist.
A stepwise algorithm is recommended, beginning with assessment of basal pituitary hormone levels and proceeding to specifically targeted pituitary stimulation tests (figure 2).
For the group of patients to which this article is relevant (those who are likely to have abnormal function of the hypothalamus and/or pituitary gland), the performance of combined pituitary tests with simultaneous testing of all axes has become practically obsolete.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Prof. v. Werder has received honoraria for lectures given in continuing medical education courses that were sponsored by the Novartis company.
The remaining authors state that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Daly AF, Burlacu MC, Livadariu E, Beckers A. The epidemiology and management of pituitary incidentalomas. Horm Res. 2007;68(Suppl 5):195–198. doi: 10.1159/000110624. [DOI] [PubMed] [Google Scholar]
- 2.Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007;369:1461–1470. doi: 10.1016/S0140-6736(07)60673-4. [DOI] [PubMed] [Google Scholar]
- 3.Persani L, Ferretti E, Borgato S, Faglia G, Beck-Peccoz P. Circulating thyrotropin bioactivity in sporadic central hypothyroidism. J Clin Endocrinol Metab. 2000;85:3631–3635. doi: 10.1210/jcem.85.10.6895. [DOI] [PubMed] [Google Scholar]
- 4.Andersen S, Bruun NH, Pedersen KM, Laurberg P. Biologic variation is important for interpretation of thyroid function tests. Thyroid. 2003;13:1069–1078. doi: 10.1089/105072503770867237. [DOI] [PubMed] [Google Scholar]
- 5.Atmaca H, Tanriverdi F, Gokce C, Unluhizarci K, Kelestimur F. Do we still need the TRH stimulation test? Thyroid. 2007;17:529–533. doi: 10.1089/thy.2006.0311. [DOI] [PubMed] [Google Scholar]
- 6.Monig H, Stracke L, Arendt T, Kloehn S. Blunted nocturnal TSH surge does not indicate central hypothyroidism in patients after pituitary surgery. Exp Clin Endocrinol Diabetes. 1999;107:89–92. doi: 10.1055/s-0029-1212080. [DOI] [PubMed] [Google Scholar]
- 7.Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–3672. doi: 10.1210/jcem.84.10.6079. [DOI] [PubMed] [Google Scholar]
- 8.Ghai K, Cara JF, Rosenfield RL. Gonadotropin releasing hormone agonist (nafarelin) test to differentiate gonadotropin deficiency from constitutionally delayed puberty in teen-age boys-a clinical research center study. J Clin Endocrinol Metab. 1995;80:2980–2986. doi: 10.1210/jcem.80.10.7559884. [DOI] [PubMed] [Google Scholar]
- 9.Partsch CJ, Hermanussen M, Sippell WG. Differentiation of male hypogonadotropic hypogonadism and constitutional delay of -puberty by pulsatile administration of gonadotropin-releasing hormone. J Clin Endocrinol Metab. 1985;60:1196–1203. doi: 10.1210/jcem-60-6-1196. [DOI] [PubMed] [Google Scholar]
- 10.Smals AG, Hermus AR, Boers GH, et al. Predictive value of -luteinizing hormone releasing hormone (LHRH) bolus testing -before and after 36-hour pulsatile LHRH administration in the differential diagnosis of constitutional delay of puberty and male hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 1994;78:602–608. doi: 10.1210/jcem.78.3.8126131. [DOI] [PubMed] [Google Scholar]
- 11.Christ-Crain M, Meier C, Huber PR, Zimmerli L, Mueller B. Value of gonadotropin-releasing hormone testing in the differential diagnosis of androgen deficiency in elderly men. J Clin Endocrinol Metab. 2005;90:1280–1286. doi: 10.1210/jc.2004-0850. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt IL, Lahner H, Mann K, Petersenn S. Diagnosis of adrenal insufficiency: evaluation of the corticotropin-releasing hormone test and basal serum cortisol in comparison to the insulin tolerance test in patients with hypothalamic-pituitary-adrenal disease. J Clin Endocrinol Metab. 2003;88:4193–4198. doi: 10.1210/jc.2002-021897. [DOI] [PubMed] [Google Scholar]
- 13.Nye EJ, Grice JE, Hockings GI, et al. The insulin hypoglycemia test: hypoglycemic criteria and reproducibility. J Neuroendocrinol. 2001;13:524–530. doi: 10.1046/j.1365-2826.2001.00664.x. [DOI] [PubMed] [Google Scholar]
- 14.Yeste D, Tomasini R, Dodino G, et al. Hypoglycaemia-insulin test: discordant growth hormone and cortisol response in paediatric patients regarding recovery from hypoglycaemia with or without oral glucose solution. Horm Res. 2007;67:42–45. doi: 10.1159/000096055. [DOI] [PubMed] [Google Scholar]
- 15.Courtney CH, McAllister AS, McCance DR, et al. The insulin hypoglycaemia and overnight metyrapone tests in the assessment of the hypothalamic-pituitary-adrenal axis following pituitary surgery. Clin Endocrinol (Oxf) 2000;53:309–312. doi: 10.1046/j.1365-2265.2000.01093.x. [DOI] [PubMed] [Google Scholar]
- 16.Muller OA, Dorr HG, Hagen B, Stalla GK, von Werder K. Corticotropin releasing factor (CRF)-stimulation test in normal controls and patients with disturbances of the hypothalamo-pituitary-adrenal axis. Klin Wochenschr. 1982;60:1485–1491. doi: 10.1007/BF01716099. [DOI] [PubMed] [Google Scholar]
- 17.Dullaart RP, Pasterkamp SH, Beentjes JA, Sluiter WJ. Evaluation of adrenal function in patients with hypothalamic and pituitary disorders: comparison of serum cortisol, urinary free cortisol and the human-corticotrophin releasing hormone test with the insulin tolerance test. Clin Endocrinol (Oxf) 1999;50:465–471. doi: 10.1046/j.1365-2265.1999.00679.x. [DOI] [PubMed] [Google Scholar]
- 18.Dorin RI, Qualls CR, Crapo LM. Diagnosis of adrenal insufficiency. Ann Intern Med. 2003;139:194–204. doi: 10.7326/0003-4819-139-3-200308050-00009. [DOI] [PubMed] [Google Scholar]
- 19.Oelkers W. The role of high- and low-dose corticotropin tests in the diagnosis of secondary adrenal insufficiency. Eur J -Endocrinol. 1998;139:567–570. doi: 10.1530/eje.0.1390567. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell H, Dattani MT, Nanduri V, et al. Failure of IGF-I and IGFBP-3 to diagnose growth hormone insufficiency. Arch Dis Child. 1999;80:443–447. doi: 10.1136/adc.80.5.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biller BM, Samuels MH, Zagar A, et al. Sensitivity and specificity of six tests for the diagnosis of adult GH deficiency. J Clin -Endocrinol Metab. 2002;87:2067–2079. doi: 10.1210/jcem.87.5.8509. [DOI] [PubMed] [Google Scholar]
- 22.Ghigo E, Aimaretti G, Corneli G. Diagnosis of adult GH defi-ciency. Growth Horm IGF Res. 2008;18:1–16. doi: 10.1016/j.ghir.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Alba-Roth J, Muller OA, Schopohl J, von Werder K. Arginine stimulates growth hormone secretion by suppressing endogenous somatostatin secretion. J Clin Endocrinol Metab. 1988;67:1186–1189. doi: 10.1210/jcem-67-6-1186. [DOI] [PubMed] [Google Scholar]
- 24.Valetto MR, Bellone J, Baffoni C, et al. Reproducibility of the growth hormone response to stimulation with growth hormone-releasing hormone plus arginine during lifespan. Eur J -Endocrinol. 1996;135:568–572. doi: 10.1530/eje.0.1350568. [DOI] [PubMed] [Google Scholar]
- 25.Corneli G, Di Somma C, Baldelli R, et al. The cut-off limits of the GH response to GH-releasing hormone-arginine test related to body mass index. Eur J Endocrinol. 2005;153:257–264. doi: 10.1530/eje.1.01967. [DOI] [PubMed] [Google Scholar]
- e1.Giustina A, Barkan A, Chanson P, et al. Guidelines for the treatment of growth hormone excess and growth hormone deficiency in adults. J Endocrinol Invest. 2008;31:820–838. doi: 10.1007/BF03349263. [DOI] [PubMed] [Google Scholar]
- e2.Molitch ME, Clemmons DR, Malozowski S, et al. Evaluation and treatment of adult growth hormone deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2006;91:1621–1634. doi: 10.1210/jc.2005-2227. [DOI] [PubMed] [Google Scholar]
- e3.Mehta A, Hindmarsh PC, Stanhope RG, et al. Is the thyrotropin–releasing hormone test necessary in the diagnosis of central hypothyroidism in children. J Clin Endocrinol Metab. 2003;88:5696–5703. doi: 10.1210/jc.2003-030943. [DOI] [PubMed] [Google Scholar]
- e4.Spencer CA, Schwarzbein D, Guttler RB, LoPresti JS, Nicoloff JT. Thyrotropin (TSH)-releasing hormone stimulation test responses employing third and fourth generation TSH assays. J Clin Endocrinol Metab. 1993;76:494–498. doi: 10.1210/jcem.76.2.8432796. [DOI] [PubMed] [Google Scholar]
- e5.Hartoft-Nielsen ML, Lange M, Rasmussen AK, et al. Thyrotropin–releasing hormone stimulation test in patients with pituitary pathology. Horm Res. 2004;61:53–57. doi: 10.1159/000075239. [DOI] [PubMed] [Google Scholar]
- e6.Szabolcs I, Kesmarki N, Bor K, et al. Apoplexy of a pituitary macroadenoma as a severe complication of preoperative thyrotropin–releasing hormone (TRH) testing. Exp Clin Endocrinol Diabetes. 1997;105:234–236. doi: 10.1055/s-0029-1211758. [DOI] [PubMed] [Google Scholar]
- e7.Vermeulen A. Reflections concerning biochemical parameters of -androgenicity. Aging Male. 2004;7:280–289. doi: 10.1080/13685530400016615. [DOI] [PubMed] [Google Scholar]
- e8.Nieschlag E, Behre HM, Bouchard P, et al. Testosterone replacement therapy: current trends and future directions. Hum Reprod Update. 2004;10:409–419. doi: 10.1093/humupd/dmh035. [DOI] [PubMed] [Google Scholar]
- e9.Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine -society clinical practice guideline. J Clin Endocrinol Metab. 2006;91:1995–2010. doi: 10.1210/jc.2005-2847. [DOI] [PubMed] [Google Scholar]
- e10.Erturk E, Jaffe CA, Barkan AL. Evaluation of the integrity of the -hypothalamic-pituitary-adrenal axis by insulin hypoglycemia test. J Clin Endocrinol Metab. 1998;83:2350–2354. doi: 10.1210/jcem.83.7.4980. [DOI] [PubMed] [Google Scholar]
- e11.Hagg E, Asplund K, Lithner F. Value of basal plasma cortisol assays in the assessment of pituitary-adrenal insufficiency. Clin Endocrinol (Oxf) 1987;26:221–226. doi: 10.1111/j.1365-2265.1987.tb00780.x. [DOI] [PubMed] [Google Scholar]
- e12.Jones SL, Trainer PJ, Perry L, et al. An audit of the insulin tolerance test in adult subjects in an acute investigation unit over one year. Clin Endocrinol (Oxf) 1994;41:123–128. doi: 10.1111/j.1365-2265.1994.tb03793.x. [DOI] [PubMed] [Google Scholar]
- e13.Deutschbein T, Unger N, Mann K, Petersenn S. Diagnosis of secondary adrenal insufficiency: unstimulated early morning cortisol in saliva and serum in comparison with the insulin tolerance test. Horm Metab Res. 2009;41:834–839. doi: 10.1055/s-0029-1225630. [DOI] [PubMed] [Google Scholar]
- e14.Lindholm J. The insulin hypoglycaemia test for the assessment of the hypothalamic-pituitary-adrenal function. Clin Endocrinol (Oxf) 2001;54:283–286. doi: 10.1046/j.1365-2265.2001.01163.x. [DOI] [PubMed] [Google Scholar]
- e15.Pfeifer M, Kanc K, Verhovec R, Kocijancic A. Reproducibility of the insulin tolerance test (ITT) for assessment of growth hormone and cortisol secretion in normal and hypopituitary adult men. Clin Endocrinol (Oxf) 2001;54:17–22. doi: 10.1046/j.1365-2265.2001.01179.x. [DOI] [PubMed] [Google Scholar]
- e16.Vestergaard P, Hoeck HC, Jakobsen PE, Laurberg P. Reproducibility of growth hormone and cortisol responses to the insulin tolerance test and the short ACTH test in normal adults. Horm Metab Res. 1997;29:106–110. doi: 10.1055/s-2007-979000. [DOI] [PubMed] [Google Scholar]
- e17.Borm K, Slawik M, Beuschlein F, et al. Low-dose glucose infusion after achieving critical hypoglycemia during insulin tolerance -testing: effects on time of hypoglycemia, neuroendocrine stress -response and patient’s discomfort in a pilot study. Eur J Endocrinol. 2005;153:521–526. doi: 10.1530/eje.1.01992. [DOI] [PubMed] [Google Scholar]
- e18.Maghnie M, Uga E, Temporini F, et al. Evaluation of adrenal function in patients with growth hormone deficiency and hypothalamic–pituitary disorders: comparison between insulin-induced hypoglycemia, low-dose ACTH, standard ACTH and CRH stimulation tests. Eur J Endocrinol. 2005;152:735–741. doi: 10.1530/eje.1.01911. [DOI] [PubMed] [Google Scholar]
- e19.Abdu TA, Elhadd TA, Neary R, Clayton RN. Comparison of the low dose short synacthen test (1 microg), the conventional dose short synacthen test (250 microg), and the insulin tolerance test for -assessment of the hypothalamo-pituitary-adrenal axis in patients with pituitary disease. J Clin Endocrinol Metab. 1999;84:838–843. doi: 10.1210/jcem.84.3.5535. [DOI] [PubMed] [Google Scholar]
- e20.Nye EJ, Grice JE, Hockings GI, et al. Adrenocorticotropin stimulation tests in patients with hypothalamic-pituitary disease: low dose, standard high dose and 8-h infusion tests. Clin Endocrinol (Oxf) 2001;55:625–633. doi: 10.1046/j.1365-2265.2001.01389.x. [DOI] [PubMed] [Google Scholar]
- e21.Agha A, Tomlinson JW, Clark PM, Holder G, Stewart PM. The long-term predictive accuracy of the short synacthen (corticotropin) stimulation test for assessment of the hypothalamic-pituitary–adrenal axis. J Clin Endocrinol Metab. 2006;91:43–47. doi: 10.1210/jc.2005-1131. [DOI] [PubMed] [Google Scholar]
- e22.Deutschbein T, Unger N, Mann K, Petersenn S. Diagnosis of -secondary adrenal insufficiency in patients with hypothalamic–pituitary disease: comparison between serum and salivary cortisol during the high-dose short synacthen test. Eur J Endocrinol. 2009;160:9–16. doi: 10.1530/EJE-08-0600. [DOI] [PubMed] [Google Scholar]
- e23.Klose M, Lange M, Kosteljanetz M, Poulsgaard L, Feldt-Rasmussen U. Adrenocortical insufficiency after pituitary surgery: an audit of the reliability of the conventional short synacthen test. Clin Endocrinol (Oxf) 2005;63:499–505. doi: 10.1111/j.1365-2265.2005.02368.x. [DOI] [PubMed] [Google Scholar]
- e24.Streeten DH. Shortcomings in the low-dose (1 microg) ACTH test for the diagnosis of ACTH deficiency states. J Clin Endocrinol Metab. 1999;84:835–837. doi: 10.1210/jcem.84.3.5581. [DOI] [PubMed] [Google Scholar]
- e25.Hilding A, Hall K, Wivall-Helleryd IL, et al. Serum levels of insulin-like growth factor I in 152 patients with growth hormone deficiency, aged 19-82 years, in relation to those in healthy subjects. J Clin Endocrinol Metab. 1999;84:2013–2019. doi: 10.1210/jcem.84.6.5793. [DOI] [PubMed] [Google Scholar]
- e26.Ghigo E, Bellone J, Aimaretti G, et al. Reliability of provocative tests to assess growth hormone secretory status. Study in 472 normally growing children. J Clin Endocrinol Metab. 1996;81:3323–3327. doi: 10.1210/jcem.81.9.8784091. [DOI] [PubMed] [Google Scholar]
- e27.Sato T, Igarashi N, Miyagawa K, et al. Mutual priming effects of GHRH and arginine on GH secretion: informative procedure for evaluating GH secretory dynamics. Endocrinol Jpn. 1990;37:501–509. doi: 10.1507/endocrj1954.37.501. [DOI] [PubMed] [Google Scholar]
- e28.Ghigo E, Aimaretti G, Arvat E, Camanni F. Growth hormone–releasing hormone combined with arginine or growth hormone -secretagogues for the diagnosis of growth hormone deficiency in adults. Endocrine. 2001;15:29–38. doi: 10.1385/ENDO:15:1:029. [DOI] [PubMed] [Google Scholar]
- e29.Crosnier H, Brauner R, Rappaport R. Growth hormone response to growth hormone-releasing hormone (hp GHRH1-44) as an index of growth hormone secretory dysfunction after prophylactic cranial irradiation for acute lymphoblastic leukemia (24 grays) Acta Paediatr Scand. 1988;77:681–687. doi: 10.1111/j.1651-2227.1988.tb10730.x. [DOI] [PubMed] [Google Scholar]
- e30.Darzy KH, Aimaretti G, Wieringa G, et al. The usefulness of the combined growth hormone (GH)-releasing hormone and arginine stimulation test in the diagnosis of radiation-induced GH deficiency is -dependent on the post-irradiation time interval. J Clin Endocrinol Metab. 2003;88:95–102. doi: 10.1210/jc.2002-021094. [DOI] [PubMed] [Google Scholar]