Abstract
Background
Patients undergoing ERCP receive nontrivial doses of radiation, which may increase their risk of developing cancer, especially young patients. Radiation doses to patients during ERCP correlate closely with fluoroscopy time.
Objective
The aim of this study was to determine whether endoscopist experience is associated with fluoroscopy time.
Design
Retrospective analysis of a prospectively collected database.
Setting
Data from 69 providers from 6 countries.
Patients
9,052 entries of patients undergoing ERCP.
Main Outcome Measurements
Percent difference in fluoroscopy time associated with endoscopist experience and fellow involvement.
Results
For procedure types that require less fluoroscopy time, compared with endoscopists who performed > 200 ERCPs in the preceding year, endoscopists who performed < 100 and 100 to 200 ERCPs had 104% (95% confidence interval [CI], 85%–124%) and 27% (95% CI, 20%–35%) increases in fluoroscopy time, respectively. Every 10 years of experience was associated with a 21% decrease in fluoroscopy time (95% CI, 19%–24%). For fluoroscopy-intense procedures, compared with endoscopists who performed > 200 ERCPs in the preceding year, endoscopists who performed < 100 and 100 to 200 ERCPs had 59% (95% CI, 39%–82%) and 11% (95% CI, 3%–20%) increases in fluoroscopy time, respectively. Every 10 years of experience was associated with a 20% decrease in fluoroscopy time (95% CI, 18%–24%).
Limitations
Database used is a voluntary reporting system, which may not be generalizable. Data is self-reported and was not verified for accuracy.
Conclusions
Fluoroscopy time is shorter when ERCP is performed by endoscopists with more years of performing ERCP and a greater number of ERCPs in the preceding year. These findings may have important ramifications for radiation-induced cancer risk.
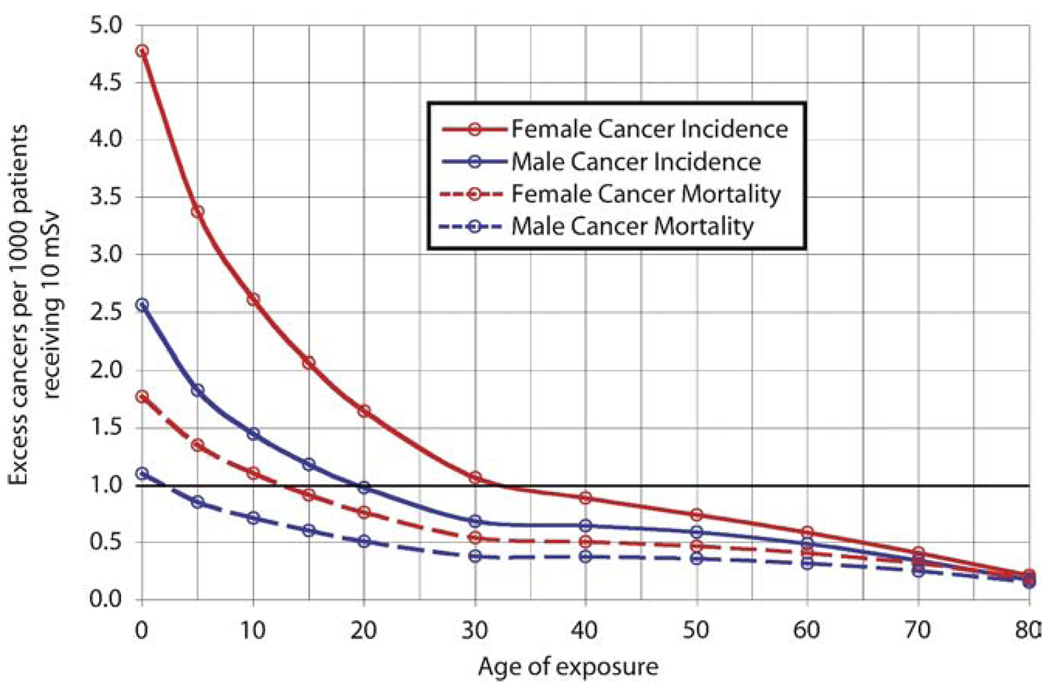
Endoscopic retrograde cholangiopancreatography, as with any radiographic study, should be performed only if the benefits to the patient outweigh the risks of the procedure. Endoscopists frequently counsel patients on the risks of bleeding, infection, perforation, pancreatitis, and cardiopulmonary arrest, but may not routinely advise them on the risks associated with radiation exposure, namely, risk of future carcinoma. Studies of the atomic bomb survivors in Japan indicate that even very low doses of radiation are associated with an increased risk of cancer, especially when exposure occurs at a young age1–4 (Fig. 1).
Figure 1.
Excess cancers per 1000 patients receiving 10 mSv radiation. From: Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, Cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 2009;251:175-84. Reproduced with permission from the Radiological Society of North America and Dr. Sodickson.
Radiation dose to patients during ERCP depends on many factors (Table 1). The endoscopist cannot control some variables, such as patient size or procedure type. Other factors are intrinsic to the equipment. More modern equipment incorporates features such as (1) pulsed fluoroscopy, whereby the x-ray beam is turned on and off at a fixed rate (eg, at 4, 8, or 15 pulses per second), which can significantly reduce exposure compared with having the x-ray beam on continuously, (2) copper x-ray beam filtration, which limits patient dose from low-energy x-rays, (3) fluoroscopic loop review and last image hold options which allow review of images without additional x-ray exposure, and (4) the ability to adjust collimation and patient position graphically from the last image rather than requiring additional radiation to accomplish these tasks. A few factors can be partially controlled by the endoscopist, such as the number of digital spot films taken, fluoroscopy time, the rate on the pulse mode setting, the intensifier magnification mode, the dose mode, and aggressive use of collimation. There is often a tradeoff between image quality and radiation exposure. For example, choosing a low dose may result in a noisy image, especially for an obese patient, so for such patients, the endoscopist will often choose a medium- or high-dose setting. Several studies have demonstrated that most of the radiation exposure during ERCP is due to fluoroscopy as opposed to spot imaging, and the exposure is directly related to fluoroscopy time. For example, up to 92% of the exposure for therapeutic ERCP5–7 is related to fluoroscopy time, with a correlation coefficient of > 0.9.5,6 However, many of the parameters shown in Table 1 can be adjusted to decrease exposure during fluoroscopy time.
TABLE 1.
Contributors of radiation exposure to patients undergoing ERCP
| Parameter | Control of Parameter | How it changes radiation exposure |
|---|---|---|
| Patient size | Not controllable | Thicker patients require up to 10× as much radiation owing to decreased penetration of the x-ray beam |
| Difficulty or type of procedure |
Not controllable | Some procedures inherently require more fluoroscopy time, which increases radiation exposure |
| Copper x-ray beam filtration |
Property of newer equipment | Automatic addition of copper filtration preferentially attenuates low-energy x-rays and reduces exposure |
| Collimation and patient positioning without radiation |
Property of newer equipment | Done graphically from the last image hold, eliminating the need for additional exposure to accomplish these tasks |
| Fluoroscopic loop review | Property of newer equipment | Shows the last 10 or more seconds of fluoroscopy without further exposure |
| Last image hold | Property of newer equipment | Shows just the last image without further exposure |
| Number of digital spot images taken |
Partially controlled by endoscopist |
Fewer digital spot images require less radiation |
| Fluoroscopy time | Partially controlled by endoscopist |
Less fluoroscopy time results in less radiation exposure |
| Pulse mode setting | Partially controlled by endoscopist |
Choosing a lower rate will result in less exposure |
| Image-intensifier magnification mode |
Partially controlled by endoscopist |
Choosing a lower magnification mode results in lower exposure (exposure in normal mode < exposure in Mag1 < exposure in Mag2) |
| Dose mode | Partially controlled by endoscopist |
Choosing a lower dose setting results in less tube current and less radiation exposure |
| Collimation | Partially controlled by endoscopist |
Using the filtration blades to limit the size of the field reduces the area exposed and improves image contrast |
| Imaging geometry | Partially controlled by endoscopist |
Positioning the patient as close to the image intensifier and as far from the x-ray tube as practical reduces radiation exposure |
| X-Ray tube potential (kVp) |
Partially controlled by endoscopist |
Use of an automatic algorithm that uses higher kVp results in more-penetrating x-ray beams and less radiation exposure, although at the expense of less image contrast |
Mag1, magnification mode 1; Mag2, magnification mode 2.
Take-home Message
Patients are being referred for medical imaging testing involving radiation exposure at increasing rates; experts currently believe that up to 2% of all cancers in the United States may be attributable to radiation from CT studies alone. Although radiation exposure during ERCP depends on many factors, most exposure occurs as a result of fluoroscopy time, which is under partial control of the endoscopist. To improve patient safety and outcomes, endoscopists should educate themselves in methods of decreasing radiation exposure to patients during ERCP, with particular attention to minimizing fluoroscopy time when possible.
Several articles have reported mean fluoroscopy times, which range from 2.3 minutes for diagnostic ERCP to 13.7 minutes for therapeutic ERCP.5–11 However, only a few articles have sought to determine what factors influence fluoroscopy time. Uradomo et al9 showed that trainees who had performed < 50 ERCPs had longer fluoroscopy times than those who had done > 50. That study also demonstrated that more complicated cases were associated with longer fluoroscopy times and that time-limited fluoroscopy was associated with shorter fluoroscopy times.10 We aimed to estimate the association between endoscopist experience and fluoroscopy time, adjusting for procedure complexity and trainee involvement in the procedure.
METHODS
The ERCP Quality Network, sponsored by Olympus America, is a voluntary reporting system that prospectively collects data pertaining to endoscopist demographics and experience, as well as procedure indication, type, duration, difficulty, and outcomes, including complications. Endoscopists worldwide have been encouraged to submit their ERCP information to the database for the purpose of developing individual report cards and benchmarking standards. All procedure and provider information is deidentified and accessible upon the request of individual endoscopists in the network.
We analyzed 9052 procedures submitted to the ERCP Quality Network between March 28, 2007, and January 29, 2009, to determine factors associated with fluoroscopy time. Correlations between univariate factors were explored using Pearson correlation. Because we were primarily interested in endoscopist-level factors, we performed multivariate stepwise forward multilevel linear regression, accounting for the clustering of case types within endoscopists. Analyses were performed using SAS 9.1 software (SAS Institute, Cary, NC). Because fluoroscopy time was found to be heavily skewed, we treated the outcome as log-transformed fluoroscopy time in these regression models, resulting in estimates for the percent-age difference in fluoroscopy time associated with each factor. We also performed multivariate multilevel logistic regression to estimate the adjusted odds ratio of fluoroscopy times > 20 minutes. Endoscopist-level factors examined included number of years of ERCP experience, number of ERCPs performed in the preceding year, and total number of lifetime ERCPs. We identified a number of specific procedures associated with increased fluoroscopy time (Table 2). Because each of these procedures was relatively rare, in the multivariate regression models we adjusted for a single dichotomous factor for whether or not one of these procedures had been attempted. We also adjusted for fellow involvement by using percentage of time trainees handled the duodenoscope (0%, 1%–50%, 51%–99%, or 100%). Other factors explored but not used in the final models included American Society of Anesthesiologists grade, ERCP difficulty grade,12 and type of anesthesia used. Informed consent was waived by the University of Michigan Institutional Review Board, because the study used only publicly available deidentified data.
TABLE 2.
Percentage increase in fluoroscopy time for fluoro-intense procedures
| Procedure | n (%) | Increase in fluoroscopy time, %(95% CI) |
|---|---|---|
| Precut sphincterotomy | 418 (4.8%) | +49 (35–64) |
| Pancreatic stone extraction | 197 (2.3%) | +55 (34–79) |
| Biliary brushing | 550 (6.4%) | +70 (56–86) |
| Extraction of biliary stones > 10 mm | 743 (8.6%) | +71 (59–85) |
| Balloon dilation of a stricture | 784 (9.1%) | +96 (95–128) |
| Hilar stent placement | 667 (7.7%) | +110 (95–128) |
CI, Confidence interval.
RESULTS
As of January 29, 2009, the ERCP Quality Network contained 9052 entries from 68 endoscopists practicing at 30 institutions in 6 countries. We excluded 397 entries that did not contain fluoroscopy time, for a total of 8655 entries. Eighty-one percent of providers were from the United States, and 10% were from the United Kingdom. A total of 4030 procedures (47% of all procedures) were completed by 34 academic endoscopists (52% of all endoscopists). The remaining 4625 (53%) procedures were completed by 31 endoscopists practicing in the community (48% of all endoscopists). Median fluoroscopy time was 3.0 minutes, ranging from 0.1 to 60.0 minutes (inter-quartile range [IQR], 1.6–6.0 minutes). A total of 1109 procedures (13%) used ≥ 10 minutes, and 270 (3%) used ≥ 20 minutes of fluoroscopy time.
Procedure difficulty
ERCP difficulty was determined by a published grading system that was developed for the assessment of ERCP outcomes.12 In univariate analysis, fluoroscopy time was not consistently associated with this grading system: Compared with grade 1 (standard procedures), grade 2 (advanced procedures) had 50% longer fluoroscopy time (95% confidence interval [CI], 42%–58%), but grade 3 (tertiary procedures) had 9% shorter fluoroscopy time than grade 1 procedures (95% CI, 5%–14%). Therefore, we analyzed each individual procedure type to determine which were associated with significantly longer fluoroscopy time. Attempt of precut sphincterotomy, pancreatic stone extraction, biliary brushings, extraction of biliary stones > 10 mm, balloon dilation of a stricture and placement of a hilar stent were associated with longer fluoroscopy times (Table 2). Therefore, we defined “fluoroscopy-intense” procedures as the attempt of any of these specific procedures. All other ERCPs were classified as “less-fluoroscopy” procedures. A total of 2740 (32%) of the procedures were fluoroscopy-intense, and 5915 (68%) of the procedures were the type that required less fluoroscopy. The median fluoroscopy time for the fluoroscopy-intense procedures was 4.9 minutes (IQR, 2.9–9.0 minutes), compared with less-fluoroscopy procedures, which had a median fluoroscopy time of 2.5 minutes (IQR, 1.2–4.8 minutes).
Experience
ERCP experience per provider ranged from 1 to 36 years (median, 13 years), 157 to 15,000 lifetime ERCPs performed (median, 1300), and 10 to 940 ERCPs performed in the preceding year (median, 150). Twenty-three providers (34%) performed < 100 ERCPs in the preceding year, 26 providers (38%) performed from 100 to 200 procedures in the preceding year, and 19 providers (28%) performed > 200 procedures in the prior year.
Using univariate multilevel linear regression, we found that fewer ERCPs performed in the preceding year, fewer lifetime ERCPs performed, and fewer years performing ERCP were each associated with a statistically significant increase in fluoroscopy time. Lifetime number of ERCPs was closely associated with the number performed in the preceding year (ρ = 0.74; P < .0001), and less so with years performing ERCP (ρ = 0.36; P = .0029). However, there was no correlation between years of experience and ERCPs performed in the preceding year (ρ = −0.02; P = .88). Therefore, to avoid issues of colinearity, the multivariate models did not examine the effect of lifetime number of ERCPs.
Sixty-four percent of the fluoroscopy-intense procedures were performed by endoscopists who perform > 200 ERCPs annually, 26% were performed by endoscopists who perform 100 to 200 ERCPs annually, and only 9% of the fluoroscopy-intense procedures were performed by endoscopists who perform < 100 ERCPs annually. However, endoscopists from each category had about one-third of their case load consisting of these procedures (Table 3). There was significant interaction between annual volume of ERCPs and fluoroscopy-intense procedures for fluoroscopy time (P < .0001). Therefore, estimates of the effect of provider experience are provided stratified by type of procedure.
TABLE 3.
Demographics by case load of ERCPs in preceding year
| < 100 | 100–200 | > 200 | |
|---|---|---|---|
| No. of providers | 23 (34%) | 26 (38%) | 19 (28%) |
| No. of cases performed (n = 8655) | 782 (9%) | 2291 (26%) | 5582 (64%) |
| No. of fluoroscopy-intense cases performed (n = 2740) |
214 (8%) | 779 (28%) | 1747 (64%) |
| Provider’s case load consisting of fluoroscopy-intense procedures, % |
27% | 34% | 31% |
For less-fluoroscopy procedures, compared with endoscopists who performed > 200 ERCPs in the preceding year, endoscopists who performed < 100 ERCPs were associated with more then a doubling in fluoroscopy time (104% increase; 95% CI, 85%–124%; Table 4). Endoscopists who performed 100 to 200 ERCPs in the preceding year had a 27% increase in fluoroscopy time (95% CI, 20%–35%). Additionally, every 10 years of experience was associated with a 21% decrease in fluoroscopy time (95% CI, 19%–24%).
TABLE 4.
Multilevel adjusted differences in fluoroscopy time by experience
| Factor | Difference in fluoroscopy time, %(95% CI) | |
|---|---|---|
| Less-fluoroscopy procedures | Fluoroscopy-intense procedures | |
| Number of ERCPs in preceding year | ||
| >200 | Reference: 0% | Reference: 0% |
| 100–200 | +27 (20–30) | +11 (3–20) |
| < 100 | +104 (85–124) | +59 (39–82) |
| Years of experience performing ERCP (each incremental 10 years) |
−21 (−19 to −24) | −20 (−18 to −24) |
CI, Confidence interval.
For fluoroscopy-intense procedures, compared with endoscopists who performed > 200 ERCPs in the preceding year, endoscopists who performed < 100 ERCPs had a 59% increase in fluoroscopy time (95% CI, 39%–82%; Table 4). Endoscopists performing 100 to 200 ERCPs in the preceding year was associated with an 11% increase in fluoroscopy time (95% CI, 3%–20%). In addition, every 10 years of experience was associated with a 20% decrease in fluoroscopy time (95% CI, 18%–24%).
We also estimated the odds ratios for using > 20 minutes of fluoroscopy time (Table 5). For less-fluoroscopy procedures, compared with endoscopists who perform > 200 ERCPs, endoscopists who performed < 100 ERCPs were 4.0 times (95% CI, 2.4–6.6) more likely to use ≥ 20 minutes of fluoroscopy time. Endoscopists who performed 100 to 200 ERCPs were 1.7 times (95% CI, 1.1–2.7) more likely to use ≥ 20 minutes of fluoroscopy time. For fluoroscopy-intense procedures, compared with endoscopists who performed > 200 ERCPs in the preceding year, endoscopists who performed < 100 ERCPs were 3.6 times (95% CI, 2.1–5.9) more likely to use ≥ 20 minutes of fluoroscopy time. Endoscopists who performed 100 to 200 ERCPs were 2.0 times (95% CI, 1.3–3.1) more likely to require ≥ 20 minutes of fluoroscopy time. For less-fluoroscopy procedures, every 10 years of experience was associated with an odds ratio of 0.7 (95% CI, 0.6–0.9), and for fluoroscopy-intense procedures, every 10 years of experience was associated with an odds ratio of 0.6 (95% CI, 0.5–0.8).
TABLE 5.
Multilevel adjusted odds ratios for fluoroscopy time ≥ 20 minutes by experience
| Factor | Odds ratio (95% CI) | |
|---|---|---|
| Less-fluoroscopy procedures | Fluoroscopy-intense procedures | |
| No. of ERCPs in preceding year | ||
| > 200 | Reference: 1.0 | Reference: 1.0 |
| 100–200 | 1.7 (1.1–2.7) | 2.0 (1.3–3.1) |
| < 100 | 4.0 (2.4–6.6) | 3.6 (2.1–5.9) |
| Years of experience performing ERCP (each incremental 10 years) |
0.7 (0.6–0.9) | 0.6 (0.5–0.8) |
CI, Confidence interval.
Trainee involvement
Trainees were involved in 39% of the cases. For both less-fluoroscopy and fluoroscopy-intense cases, after adjusting for endoscopist experience, trainee involvement was associated with greater fluoroscopy time (Table 6). However, the increase was most notable for cases where the trainee was involved from 1% to 50% of the time. Compared with procedures without trainee involvement, only procedures with trainee involvement between 1% and 50% of the time were significantly associated with an increased odds ratio of using > 20 minutes of fluoroscopy time (Table 7).
TABLE 6.
Multilevel adjusted difference in fluoroscopy time by trainee involvement
| Factor | Difference in fluoroscopy time %(95% CI) | |
|---|---|---|
| Less-fluoroscopy procedures | Fluoroscopy-intense procedures | |
| Time handling duodenoscope | ||
| 0% | Reference: 100% | Reference: 100% |
| 1%–50% | +112 (98–128) | +82 (68–99) |
| 51%–99% | +60 (48–73) | +41 (28–56) |
| 100% | +14 (4–25) | +9 (−4–22) |
CI, Confidence interval.
TABLE 7.
Multilevel adjusted odds ratios for fluoroscopy time ≥ 20 minutes by trainee involvement
| Factor | Odds ratio (95% CI) | |
|---|---|---|
| Less-fluoroscopy procedures | Fluoroscopy-intense procedures | |
| Time handling duodenoscope | ||
| 0% | Reference 1.0 | Reference 1.0 |
| 1%–50% | 1.5 (1.0–2.4) | 1.9 (1.2–2.9) |
| 51%–99% | 0.7 (0.4–1.3) | 0.9 (0.5–1.7) |
| 100% | 0.2 (0.1–0.7) | 0.0 (0.0–0.0)* |
CI, Confidence interval.
Estimates did not converge, owing to limited size in this stratum.
Specific scenarios
Finally, we determined the median fluoroscopy time for a “best-case” and a “worst-case” case scenario. The best case was defined as ERCPs performed by an endoscopist with ≥ 20 years experience who performs > 200 ERCPs per year and in which the procedure was performed without trainee involvement. The worst case was defined as ERCPs performed by a endoscopist with < 5 years of experience who performs < 100 ERCPs per year and in which the procedure was performed with fellows involved between 1% and 50% of the time. For less-fluoroscopy procedures, the median fluoroscopy time for the best-case scenario (n = 122) was 3.0 minutes (IQR, 1.8–4.8 minutes) compared with 6.0 minutes (IQR, 4.0–10.0 minutes) for the worst-case scenario (n = 79). For fluoroscopy-intense procedures, the median fluoroscopy time for the best-case scenario (n = 31) was 4.9 minutes (IQR, 2.8–8.3 minutes) compared with 10.2 minutes (IQR, 4.9–15.0 minutes) for the worst-case scenario (n = 34).
DISCUSSION
Overall, our analysis showed that certain procedure types, less-experienced endoscopists, and procedures performed by fellows were associated with longer fluoroscopy times.
Both cumulative years of performing ERCP and ERCP volume in the preceding year were independently associated with shorter fluoroscopy exposure. At this time, there are insufficient data to support using fluoroscopy time as a surrogate end point for competency, but it is an easily measureable and comparable variable. The present data support the recent trend in recommending minimal annual requirements to maximize patient safety13 and should encourage more endoscopists to contribute to the ERCP Quality Network so that they can anonymously compare their outcomes.
Cases with trainees had longer fluoroscopy time than cases without trainees. Even after adjusting for the fluoroscopy intensity of the procedure, when a trainee handled the duodenoscope between 1% and 50% of the time, this resulted in the longest fluoroscopy times. Of note, the present observational study can not assign a causal direction to this association, ie, it is not clear whether fellows use more fluoroscopy time or if the fact that the attending endoscopist took over the procedure indicates that there were other unmeasured factors that made that procedure require more fluoroscopy regardless of who was performing the procedure. Both factors were likely at play here, because the association with fluoroscopy time was weaker in cases where the fellow was allowed to complete 51% to 99% of the procedure. If the fellow was allowed to complete the entire procedure alone, fluoroscopy time was minimally increased and the odds ratio for requiring ≥ 20 minutes of fluoroscopy time was 0.2, likely representing either very competent trainees or straightforward cases.
Most of the data we have regarding radiation-induced cancer risk comes from studies of survivors from the atomic bombs in Hiroshima and Nagasaki. Preston et al1–3 reported that there is a linear dose response over the range from 0 to 2 Gy (2 Gy = 2000 mSv). The risk depends on not only the exposure dose, but also the age at exposure and the age attained.4,14,15 One’s lifetime risk of developing cancer at baseline from all causes is 41%,16,17 and one’s lifetime risk of dying from cancer is 21%.16 As a general estimate of risk, for every sievert of exposure, one’s absolute risk of developing cancer increases by 10%,15 although Figure 1 clearly demonstrates the increased risk that occurs with exposure to patients < 30 years old.14
To put things into perspective, effective dose from natural background radiation is about 3 mSv per year. Effective doses from abdominal CT range from 4 to 18 mSv,18–20 and 8 mSv is the generally accepted average effective dose associated with an abdominal CT.21,22 Median effective doses to patients during ERCP range from 1.8 mSv to 12.5 mSv.5–11 The radiation dose from any one ERCP depends on a number of factors, but several studies have demonstrated that most of the exposure comes from fluoroscopy time, up to 92% for therapeutic ERCP.5–7 The correlation coefficient (r) between radiation dose and fluoroscopy time has been reported to be > 0.9.5,6 Therefore, longer fluoroscopy times directly correlate with increased radiation exposure to patients.
Although there is no one conversion factor to relate fluoroscopy time during ERCP to effective dose, using the values previously reported in the literature5,7,8 as benchmarks, 20 minutes of fluoroscopy time roughly correlates to ~30 mSv. Using an average absolute increased risk of developing cancer of 10% per sievert,15 this represents a potential increased absolute risk of developing cancer of 0.3% with 20 minutes of fluoroscopy or 3 additional cancers for every 1000 patients. Fortunately, only 3.1% of the procedures required fluoroscopy time of this magnitude or more. Median fluoroscopy time and the difference between the present best- and worst-case scenarios was about 3 minutes. Three minutes of fluoroscopy time represents an individual absolute increased risk of developing cancer of only about 0.05%. However, even at this dose, exposure risk to a growing population of patients undergoing ERCP, sometimes repeatedly and at young ages, may be quite significant. Furthermore, many of these patients likely have received CT and will receive additional medical radiation in the future. Fazel et al22 recently reviewed the medical records of almost a million patients and demonstrated that 70% of the patients had undergone at least 1 medical imaging procedure over a 3-year period, with about 20% of patients receiving 3 to 20 mSv and 2% receiving >20 mSv radiation exposure. The referral rates for medical imaging tests has increased so much over the last decade that experts are now estimating that up to 2% of all cancers in the United States may be attributable to radiation from CT studies alone.4 It therefore seems prudent to minimize exposure to radiation whenever possible.
Increased awareness of radiation exposure has been shown to result in shorter fluoroscopy times.23 In addition to consciously limiting fluoroscopy time, the endoscopist can also modify several other factors that contribute to radiation exposure during ERCP (Table 1). Some factors that contribute to prolonged fluoroscopy time and therefore increased radiation doses are not modifiable. For example, obese patients may be exposed to 5 to 10 times more radiation than their thin counterparts for a constant fluoroscopy time. However, increased awareness of the contributions of fluoroscopy time and other factors on radiation exposure and future risks of cancer to our patients may help endoscopists minimize these risks as much as possible to improve patient safety and outcomes.
The present study has some limitations that should be mentioned. The ERCP Quality Network is a voluntary reporting system which, although available to any endoscopist wishing to participate, is currently underused and may not be representative of the broader range of endoscopist experience worldwide. Also, all entries are self-reported and have not been verified for accuracy. Nonetheless, we do not expect the reporting to be systematically biased, particularly because the endoscopists were not aware of our hypothesis.
In summary, using a large multinational endoscopy database, we have found that endoscopist experience is inversely associated with fluoroscopy time. Because fluoroscopy time correlates closely with radiation exposure to patients, this may have important clinical relevance regarding carcinogenesis. We hope that awareness of this association might prompt endoscopists with less experience to minimize their fluoroscopy time, and to consider referral of more difficult cases to more experienced endoscopists.
Abbreviations
- CI
confidence interval
- IQR
interquartile range
Footnotes
DISCLOSURE: The following author received research support for this study from the Damon Runyon Cancer Research Foundation (CI-36-07) and the National Institutes of Health (K23 DK079291): J.H. Rubenstein. All other authors disclosed no financial relationships relevant to this publication.
REFERENCES
- 1.Preston DL, Pierce DA, Shimizu Y, et al. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat Res. 2004;162:377–389. doi: 10.1667/rr3232. [DOI] [PubMed] [Google Scholar]
- 2.Preston DL, Shimizu Y, Pierce DA, et al. Studies of mortality of atomic bomb survivors. Report 13: solid cancer and noncancer disease mortality:1950–1997. Radiat Res. 2003;160:381–407. doi: 10.1667/rr3049. [DOI] [PubMed] [Google Scholar]
- 3.Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res. 2007;168:1–64. doi: 10.1667/RR0763.1. [DOI] [PubMed] [Google Scholar]
- 4.Brenner DJ, Hall EJ. Computed tomography-an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 5.Larkin CJ, Workman A, Wright RE, et al. Radiation doses to patients during ERCP. Gastrointest Endosc. 2001;53:161–164. doi: 10.1067/mge.2001.111389. [DOI] [PubMed] [Google Scholar]
- 6.Heyd RL, Kopecky KK, Sherman S, et al. Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287–292. doi: 10.1016/s0016-5107(96)70166-9. [DOI] [PubMed] [Google Scholar]
- 7.Buls N, Pages J, Mana F, et al. Patient and staff exposure during endoscopic retrograde cholangiopancreatography. Br J Radiol. 2002;75:435–443. doi: 10.1259/bjr.75.893.750435. [DOI] [PubMed] [Google Scholar]
- 8.Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, et al. Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosimetry. 2003;106:241–246. doi: 10.1093/oxfordjournals.rpd.a006355. [DOI] [PubMed] [Google Scholar]
- 9.Uradomo LT, Lustberg ME, Darwin PE, et al. Effect of physician training on fluoroscopy time during ERCP. Dig Dis Sci. 2006;51:909–914. doi: 10.1007/s10620-005-9007-y. [DOI] [PubMed] [Google Scholar]
- 10.Uradomo LT, Goldberg EM, Darwin PE. Time-limited fluoroscopy to reduce radiation exposure during ERCP: a prospective randomized trial. Gastrointest Endosc. 2007;66:84–89. doi: 10.1016/j.gie.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 11.Samara ET, Stratakis J, Enele Melono JM, et al. Therapeutic ERCP and pregnancy: is the radiation risk for the conceptus trivial? Gastrointest Endosc. 2009;69:824–831. doi: 10.1016/j.gie.2008.05.068. [DOI] [PubMed] [Google Scholar]
- 12.Johanson JF, Cooper G, Eisen GM, et al. Quality assessment of ERCP. Endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 2002;56:165–169. doi: 10.1016/s0016-5107(02)70172-7. [DOI] [PubMed] [Google Scholar]
- 13.Guda NM, Freeman ML. Are you safe for your patients—how many ERCPs should you be doing? Endoscopy. 2008;40:675–676. doi: 10.1055/s-2008-1077486. [DOI] [PubMed] [Google Scholar]
- 14.Sodickson A, Baeyens P, Andriole K, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;215:175–184. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 15.Pierce DA, Shimizu Y, Preston DL, et al. Studies of the mortality of atomic bomb survivors. Report 12, part I. Cancer 1950–1990. Radiat Res. 1996;146:1–27. [PubMed] [Google Scholar]
- 16.National Institutes of Health. Surveillance epidemiology and end results. [Accessed December 5, 2009]; Available at: http://seer.cancer.gov/statfacts/html/all.html.
- 17.Monson RR, Cleaver JE, Abrams HL, et al. BEIR VII: health risks from exposure to low levels of ionizing radiation, report in brief. Washington, DC: National Academies; 2005. pp. 1–4. [Google Scholar]
- 18.Ware DE, Huda W, Mergo PJ, et al. Radiation effective doses to patients undergoing abdominal CT examinations. Radiology. 1999;210:645–650. doi: 10.1148/radiology.210.3.r99mr05645. [DOI] [PubMed] [Google Scholar]
- 19.Fujii K, Aoyama T, Koyama S, et al. Comparative evaluation of organ and effective doses for pediatric patients with those for adults in chest and abdominal CT examinations. Br J Radiol. 2007;80:657–667. doi: 10.1259/bjr/97260522. [DOI] [PubMed] [Google Scholar]
- 20.Tsapaki V, Aldich JE, Sharma R, et al. Dose reduction in CT while maintaining diagnostic confidence: diagnostic reference levels at routine head, chest, and abdominal CT—IAEA-coordinated research project. Radiology. 2006;240:828–834. doi: 10.1148/radiol.2403050993. [DOI] [PubMed] [Google Scholar]
- 21.Mettler FA, Huda W, Yoshizumi TT, et al. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 22.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Eng J Med. 2009;361:849–857. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vehmas T. Hawthorne effect: shortening of fluoroscopy times during radiation measurement studies. Br J Radiol. 1997;70:1053–1055. doi: 10.1259/bjr.70.838.9404210. [DOI] [PubMed] [Google Scholar]