In 2003, the British Columbia Ministry of Health Services contracted with the Centre for Health Services and Policy Research at the University of British Columbia to conduct three years of work to establish a population-based information system to describe the primary healthcare (PHC) sector from temporal, geographic, population and provider perspectives. In this special issue of Healthcare Policy/Politiques de Santé, we share lessons from that experience for those interested in conducting similar work, and point readers to other reports that have emerged from these undertakings. This information will be of interest to healthcare policy makers and managers, as we describe key challenges and opportunities in developing information systems designed to support performance management and research in this sector. The topic is timely, given the importance that Canadians attribute to PHC and the magnitude of public investments over the past decade to improve PHC performance.
Why Focus on the PHC Sector?
Canadians are increasingly concerned about access to and quality of PHC, and they hold specific expectations about the importance of this sector, the type of renewal they want and the need for public reporting on progress (Watson and Krueger 2005). For instance, when asked in 2002 to deliberate about various options to sustain their healthcare system, Canadians recommended multidisciplinary PHC teams that would be supported by a central information system to provide more coordinated care and relieve family physicians of current workload burdens (Maxwell et al. 2002). In that same year, 80% of Canadians reported that more spending on “new, more efficient methods for providing PHC” should be a top or important priority among the nation's leaders. Canadians also want to learn about progress – in 2000 and 2003, approximately 45% reported that they were somewhat or very dissatisfied with the level of public reporting regarding healthcare system performance (Soroka 2007).
In response, the prime minister and premiers (“First Ministers”) made commitments in 2003 to a Health Accord, and in 2004 to a 10-Year Plan to Strengthen Health Care in Canada in order to renew PHC and enhance accountability and transparency (Government of Canada 2003, 2004). These investments were additional to multi-year investments that commenced in 2000 to catalyze renewal through the Primary Health Care Transition Fund (Government of Canada 2000). All federal, provincial and territorial governments now invest in renewal initiatives designed to improve the organization, funding and delivery of these services. Some jurisdictions report to their citizens on an annual basis, while others do not (Health Council of Canada 2007).
It is possible to use case studies, project evaluations and anecdotal evidence to inform quality improvement of local services. But population-based information systems that generate relevant information are needed to enable the healthcare policy and management communities to monitor the performance of this sector at regional levels, identify areas requiring attention and action, assess the relative impact of different strategies to catalyze system renewal and account to citizens on progress. This type of system stores information about all events experienced by a population, as recorded and measured using administrative data encompassing all encounters (e.g., payments by governments to remunerate doctors) or through deliberate sampling strategies that ensure data are representative of populations (e.g., patient or provider surveys).
Today, few jurisdictions in Canada have developed a population-based PHC information system for routine use. A number of jurisdictions, such as British Columbia, Manitoba and Ontario, have undertaken work to develop and validate information systems, particularly regarding the use of administrative data relevant to payments by governments to remunerate doctors. Other jurisdictions and organizations have conducted population-based surveys of providers, citizens or both. However, these systems aren't routinely used for performance management to improve quality or for accountability via routine and comprehensive public reporting.
Although initiatives are underway across the country to develop electronic information systems to support clinical care (e.g., disease registries, medical records and reminder systems), only 23% of primary care doctors in Canada reported that they had these systems in their office in 2006 (Schoen et al. 2006). Even if these systems were in place, they would be unlikely to offer the array of information required by the healthcare policy and management communities. Other information systems are needed, for example, to understand and better plan for the future supply of health human resources. In fact, even if administrative data on clinical and health human resources were in place, other information systems are needed to understand and better plan to improve patients' experiences with care and providers' experiences at work. While initiatives are underway to survey nurses, for example, the information collected has not been prospectively defined as a priority vis-à-vis the performance of the PHC sector, nor collected to represent providers that deliver this type of care.
What Lessons Does the BC Experience Hold for Others?
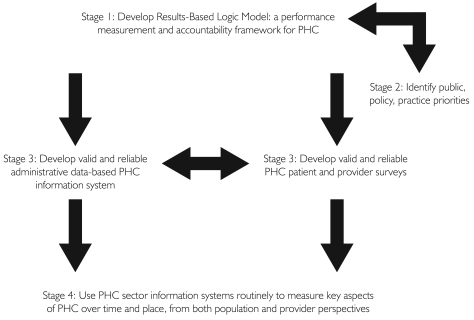
Our vision is to ensure that healthcare policy makers and managers receive relevant, valid and timely information about the PHC sector that is useful to them in assuming their accountability and decision-making responsibilities. The steps that we undertook to design an information system – one that is data-based and can be used to monitor PHC performance at regional levels and across time – identify areas requiring attention and action, assess the relative impact of different strategies to catalyze system renewal and account to citizens on progress, using robust principles for organizing data (summarized in Figure 1). The papers in this special issue document lessons learned at each step. A glossary at the end of this preface defines many of the terms used throughout the special issue to ensure specificity in meaning when communicating complex or nuanced issues. Our website contains information generated using our population-based information system (www.chspr.ubc.ca).
FIGURE 1.
Steps taken to develop a population-based PHC information system in British Columbia to support routine use of information for performance measurement and research
The first paper, “A Results-Based Logic Model for Primary Healthcare: A Conceptual Foundation for Population-Based Information Systems” (Watson, Broemeling et al.) describes work conducted to create a performance measurement and accountability framework for this sector. We used the approach of the Treasury Board of Canada in designing performance measurement and accountability frameworks, beginning with the creation of a results-based logic model. This was done through completion of a policy analysis regarding important objectives, processes and outcomes expected of PHC, a literature review regarding the important dimensions of PHC services and broad consultation regarding presumed linkages between PHC inputs, activities, outputs and outcomes.
The next challenge was to define priorities for information on the PHC sector among healthcare policy, management and practice communities, as well as the public, so that data development and collection strategies aligned with those needs. Thus, this first paper also describes initiatives in British Columbia and elsewhere in Canada using our logic model to identify priorities among the policy and management communities.
Although the creation of information systems to support performance measurement and research was needed to leverage current measurement, monitoring and reporting efforts, also required was new architecture to fill information gaps in priority areas. In order to assist ongoing work in identifying potential indicators that could be measured using existing population data, the authors of the second paper, “Measuring the Performance of Primary Healthcare: Existing Capacity and Potential Information to Support Population-Based Analyses” (Broemeling, Watson et al.) identify an array of existing population-based administrative and survey data sources and highlight gaps in current information. Our logic model was used as the conceptual framework, and clearly highlighted gaps that must be addressed to enable comprehensive performance measurement, research, accountability and public reporting.
In response to growing concerns regarding the completeness and accuracy of fee-for-service (FFS) administrative data in measuring the performance of the PHC sector in terms of physician services, we spent considerable time between 2003 and 2006 further developing the administrative data holdings at the CHSPR at the University of British Columbia.
The jurisdictions most notable for developing and using population-based administrative data relevant to PHC rely principally on FFS and shadow billing payment files. In British Columbia, there has been a decline in the proportion of total payments to physicians via FFS, and no form of shadow billing identifies information on provider–patient encounters. More recently, the validity of analyses based solely on FFS payment files has come into question, in terms of completeness and therefore accuracy, with the growth in alternative funding of physicians. No uniform nationwide standards exist to guide the establishment of databases designed to track those payments and to support pooling of data from FFS and alternative funding sources. As the size of alternative funding for physician services grows in Canada, the usefulness of FFS payment data as a sole source of population-based information describing encounters between patients and physicians will erode. Therefore, a number of papers in this special supplement address the designing of information systems within this evolving environment and highlight the importance of design for future information needs.
In order to support the development and use of administrative data for measuring and tracking supply and use of health services by the public and special populations, valid population-based registries are needed. Challenges exist in the creation of registries when provincial ministries of health, such as the one in British Columbia, charge monthly fees for enrolment in the Medical Services Plan, and when patients receive services from PHC organizations that aren't required to submit patient identifiers to receive remuneration. The calculation of population-based rates should include all users and non-users, irrespective of enrolment status. A further critical challenge is that of maintaining privacy and security of confidential, individual-level information. Thus, Broemeling, Kerluke and colleagues (“Developing and Maintaining a Population Research Registry to Support Primary Healthcare Research”) describe work undertaken to develop and validate a population registry of residents irrespective of their enrolment status with the BC Ministry of Health and identify special populations for cohort analyses.
Because family physicians are increasingly remunerated through alternative funding mechanisms such as capitation or block funding to group practice organizations, it is increasingly necessary to count the size of the clinical workforce and describe their patterns of practice using databases other than FFS payment files. Watson, Peterson and colleagues (“Methods to Develop and Maintain a Valid Physician Registry in Evolving Information Environments”) describe new methods to develop and validate an anonymous registry of the physician workforce (general practitioners, family physicians and specialists) to support analyses in environments where doctors are increasingly funded through diverse arrangements.
One of the key policy objectives of renewal efforts in Canada is the inclusion of nurses in PHC teams. Because PHC is defined by service attributes, the challenge is to identify and track physicians and nurses who deliver these services. In “Supply and Distribution of Primary Healthcare Registered Nurses in British Columbia,” Wong and colleagues describe new methods developed to classify nurses using self-reported data from the College of Registered Nurses of British Columbia. The authors assess geographic patterns of supply of these nurses relative to PHC physicians and to the health of populations. Other reports by our team describe methods to identify and track PHC who are registered as family physicians, general practitioners or specialists (Watson, Black et al. 2006) and to identify and track shifts in single and group practices among this workforce (McKendry, Watson et al. 2006).
Quality improvement and public reporting activities require routine use of PHC information systems to measure key aspects of care over time and place, from both population and provider perspectives. Yet, the degree to which these activities are conducted depends critically on sustained demand for information about healthcare from citizens and a commitment from healthcare policy makers and administrators to deliver it.
Routine public reporting is also critically dependent on sustained fiscal investments as well as the supply of highly trained research, analytical and communications staff. Internationally, Canadian policy makers and researchers have partnered to be leaders in the development and use of administrative data to describe the supply, distribution and use of physicians and their services. But these systems are in their infancy vis-à-vis the PHC sector, and little work has been done to support survey information systems for PHC.
Thus, the concluding paper, “For Discussion: A Roadmap for Population-Based Information Systems to Enhance Primary Healthcare in Canada” (Watson) summarizes lessons learned from the BC experience and offers advice to inform work to expand population-based information systems across Canada intended to support PHC renewal. A roadmap of options for new information systems is sketched and the opportunities and limitations associated with each are described. The intent is to offer an array of alternatives, since jurisdictions vary in their vision and objectives for renewal and priorities for information. The author concludes with general recommendations to improve the situation so that governments and researchers are better able to monitor the PHC sector and report to Canadians about investments designed to enhance patient experiences with PHC and the health outcomes that emerge from these public investments.
References
- Canadian Institute for Health Information (CIHI) The Status of Alternative Payment Programs for Physicians in Canada, 2003-2004 and Preliminary Information for 2004-2005. 2006. Retrieved January 9, 2009. < http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=GR_27_E>.
- Government of Canada. “Communiqué on Health.”. News release, First Ministers' meeting; Ottawa: Canadian Intergovernmental Conference Secretariat; 2000. Sep 11, Ref. no. 800-038-004. Retrieved January 9, 2009. < http://www.scics.gc.ca/cinfo00/800038004_e.html>. [Google Scholar]
- Government of Canada. First Ministers' Accord on Health Care Renewal. Ottawa: Health Canada; 2003. Retrieved January 7, 2009. < http://www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2003accord/index-eng.php>. [Google Scholar]
- Government of Canada. First Ministers' Meeting on the Future of Health Care 2004: A 10-Year Plan to Strengthen Health Care; 2004. May 9, Retrieved January 6, 2009. < http://www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index_e.html>. [Google Scholar]
- Health Council of Canada. Measuring Up? 2006 Annual Report to Canadians. Toronto: Author; 2007. [Google Scholar]
- Maxwell J., Jackson K., Legowski B., Rosell S., Yankelovich D., Forest P.-G., Lozowchuk L. Report on Citizens' Dialogue on the Future of Health Care in Canada. Saskatoon: Commission on the Future of Health Care in Canada; 2002. [Google Scholar]
- McKendry R., Watson D.E., Goertzen D., Mooney D., Peterson S. Single and Group Practices Among Primary Health Care Physicians in British Columbia. Vancouver: Centre for Health Services and Policy Research; 2006. Retrieved March 7, 2009. < http://www.chspr.ubc.ca/research/phc/provider/physician>. [Google Scholar]
- Schoen C., Osborn R., Huynh P.T., Doty M., Peugh J., Zapert K. “On the Front Lines of Care: Primary Care Doctors' Office Systems, Experiences, and Views in Seven Countries.”. Health Affairs W555-71. 2006 Nov 2; doi: 10.1377/hlthaff.25.w555. Retrieved January 8, 2009. < http://content.healthaffairs.org/cgi/content/abstract/hlthaff.25.w555v1>. [DOI] [PubMed] [Google Scholar]
- Soroka S.N. Canadians' Perceptions of the Health Care System: A Report to the Health Council of Canada. Toronto: Health Council of Canada; 2007. [Google Scholar]
- Watson D.E., Krueger H. Primary Health Care Experiences and Preferences: Research Highlights. Vancouver: Centre for Health Services and Policy Research; 2005. Retrieved January 7, 2009. < http://www.chspr.ubc.ca/node/90>. [Google Scholar]
- Watson D.E., Black C., Peterson S., Mooney D., Reid R.J. Who are the Primary Health Care Physicians in British Columbia: 1996/97 – 2005/05. Vancouver: Centre for Health Services and Policy Research; 2006. Retrieved March 7, 2009. < http://www.chspr.ubc.ca/research/phc/provider/physician>. [Google Scholar]