Abstract
Objective:
A history of depression has been linked to an increased dementia risk. This risk may be particularly high in recurrent depression due to repeated brain insult. We investigated whether there is a dose-dependent relationship between the number of episodes of elevated depressive symptoms (EDS) and the risk for mild cognitive impairment (MCI) and dementia.
Methods:
A total of 1,239 older adults from the Baltimore Longitudinal Study of Aging were followed for a median of 24.7 years. Diagnoses of MCI and dementia were made based on prospective data. Participants completed the Center for Epidemiologic Studies Depression Scale at 1- to 2-year intervals and were considered to have an EDS if their score was ≥16. Kaplan-Meier survival curves, log-rank test for trend for survivor functions, and Cox proportional hazards models were conducted to examine the risk of MCI and dementia by number of EDS.
Results:
We observed a monotonic increase in risk for all-cause dementia and Alzheimer disease as a function of the number of EDS. Each episode was associated with a 14% increase in risk for all-cause dementia. Having 1 EDS conferred an 87%–92% increase in dementia risk, while having 2 or more episodes nearly doubled the risk. Recurrence of EDS did not increase the risk of incident MCI.
Conclusions:
Our findings support the hypothesis that depression is a risk factor for dementia and suggest that recurrent depression is particularly pernicious. Preventing the recurrence of depression in older adults may prevent or delay the onset of dementia.
GLOSSARY
- AD
= Alzheimer disease;
- BLSA
= Baltimore Longitudinal Study of Aging;
- CDR
= Clinical Dementia Rating;
- CES-D
= Center for Epidemiologic Studies Depression Scale;
- CI
= confidence interval;
- DQ
= Dementia Questionnaire;
- DS
= depressive symptoms;
- DSM
-
- III-R
= Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised;
- EDS
= elevated depressive symptoms;
- HR
= hazard ratio;
- MCI
= mild cognitive impairment.
Late-life depression is associated with cognitive impairment and dementia. Converging evidence suggests that depressive symptoms (DS) and major depression are prevalent in dementia,1 but whether depression is a prodrome of dementia2,3 or a risk factor for dementia4,5 or they simply have similar neuropathologic substrates6 is a matter of dispute. According to a recent meta-analysis,7 the preponderance of evidence supports 3 possible hypotheses to explain the association between depression and dementia: 1) depression is a prodrome of dementia, 2) depression affects the threshold for manifesting dementia, or 3) depression leads to hippocampal damage through a glucocorticoid cascade, thus contributing to the development of dementia.
The latter hypothesis proposes that glucocorticoid hypersecretion observed in some individuals with major depression increases neuronal death in the hippocampus due to overexpression of glucocorticoid receptors in that region.8 Based on this model, recurrent depressive episodes would be expected to result in greater hippocampal damage due to repeated insults to the brain. Given the association between hippocampal volume loss and dementia,9,10 a greater risk of dementia may result from a higher number of previous depressive episodes. Indeed, previous research with psychiatric inpatients has shown that the number of depressive episodes was associated with cognitive impairment and dementia.11,12 However, less is known about the relationship between recurrence of less severe affective episodes in a community sample and dementia risk. The goal of the present study was to examine whether there is a monotonic increase in dementia risk as a function of the number of prior episodes of elevated DS (EDS).
METHODS
Data from the Baltimore Longitudinal Study of Aging (BLSA), an ongoing prospective study of community-dwelling adults, were used.13 Analyses included a sample of 1,239 BLSA participants with available diagnostic information (mean baseline age 55.5 ± 18.8 years). Participants are well-educated (mean years of education 16.6 ± 2.8) and were without history of CNS disease, severe cardiac disease, or metastatic cancer at enrollment.
Standard protocol approvals, registrations, and patient consents.
The National Institute on Aging Intramural Research Program Institutional Review Board approved this study and all subjects gave written informed consent.
Incident dementia and mild cognitive impairment.
All subjects were followed annually to biennially and were reviewed at a consensus conference if their Blessed Information Memory Concentration score14 was ≥3, if their informant or subject Clinical Dementia Rating (CDR)15 score was ≥0.5, or if their Dementia Questionnaire (DQ)16 results were abnormal. All subjects, regardless of screening tests, were evaluated by case conference at the time of death or withdrawal. Dementia diagnosis was determined according to DSM-III-R17 criteria. Diagnoses of dementia type were formulated during multidisciplinary conferences based on prospectively collected evidence using National Institute of Neurological and Communication Disorders–Alzheimer's Disease and Related Disorders Association criteria.18 Cognitive domains were deemed impaired if the participant exhibited progressive decline over time rather than if they scored below a cutoff on neuropsychological tests. Information from medical records, including medical diagnoses, medication use, and neuroimaging data, was considered when making diagnoses. A diagnosis of mild cognitive impairment (MCI) not meeting criteria for dementia was made when participants had either single domain cognitive impairment or cognitive impairment in multiple domains without significant functional loss, following the Petersen algorithm.19 Age at dementia and MCI onset was determined based on consecutive case conference findings. Classification of incident dementia and MCI was based on participant's cognitive status at last visit.
Depressive symptoms.
The Center for Epidemiologic Studies Depression Scale (CES-D)20 provided a measure of DS at each visit. This 20-item inventory assesses the frequency and severity of DS experienced in the past week and has adequate validity in older community-dwelling adults.21 Participants were considered to have elevated DS if their CES-D score was ≥16. This cutoff is a well-accepted standard for identifying clinically significant DS.20 To determine whether EDS are monotonically related to dementia risk, EDS was used as a categorical variable (i.e., participants were classified as having 0, 1, or 2+ EDS) or a continuous variable (range of 0–14 episodes), depending on the statistical analysis.
Statistical analysis.
All analyses were performed using Stata version 10.0.22 Differences in continuous variables across levels of categorical variables were tested using t test and analysis of variance while differences in proportions across levels of categorical variables were assessed using χ2 test. Analyses focused on incident dementia (excluding MCI subjects from the at-risk population) and incident MCI (excluding dementia cases). Separate Kaplan-Meier survival curves and log-rank test for trend for survivor functions23 compared each outcome by time-dependent recurrence of EDS. Cox proportional hazards models examined whether dementia and MCI risks were associated with recurrent EDS (time-dependent) after controlling for sociodemographic and lifestyle factors (baseline age, sex, race/ethnicity, education, and smoking status [never, former, or current smoker]) and medical factors (self-reported history of type 2 diabetes, hypertension, cardiovascular disease [stroke, congestive heart failure, nonfatal myocardial infarction, or atrial fibrillation], or dyslipidemia, and directly measured body mass index [weight in kg over squared height in m2] and systolic blood pressure [in mm Hg]). Alzheimer disease (AD) was also analyzed as an outcome in a sensitivity analysis. The dependent variables were age at onset of dementia or MCI for incident cases, or the last observed (censored) age of noncases. The type I error used for statistical significance was 0.05 for all analyses.
RESULTS
Baseline characteristics of the BLSA study sample.
Of the 1,239 participants, 142 participants developed dementia (67.6% [n = 96] AD) and 88 developed MCI. In analysis 1 with dementia as the outcome (excluding MCI), participants were followed for a median time of 23.6 years (up to 51 years) with an incidence rate of dementia of 957 per 100,000 person-years (95% confidence interval [CI] 812–1,128). For analysis 2 with MCI as the outcome (excluding dementia cases), median follow-up time was 23.0 years (up to 51 years) with an incidence rate of 603.5 per 100,000 person-years (95% CI 488.5–745.5).
Table 1 shows characteristics of study participants by recurrence of EDS and by dementia/MCI status. Experiencing 2 or more depressive episodes during follow-up was associated with a greater proportion of women (59.2% vs 40.1%) and a greater proportion of current smokers (28.1% vs 17.6%) compared to those who did not experience any episodes (p < 0.05).
Table 1 Characteristics of participants included in main analysis according to recurrence of DS and dementia/MCI status
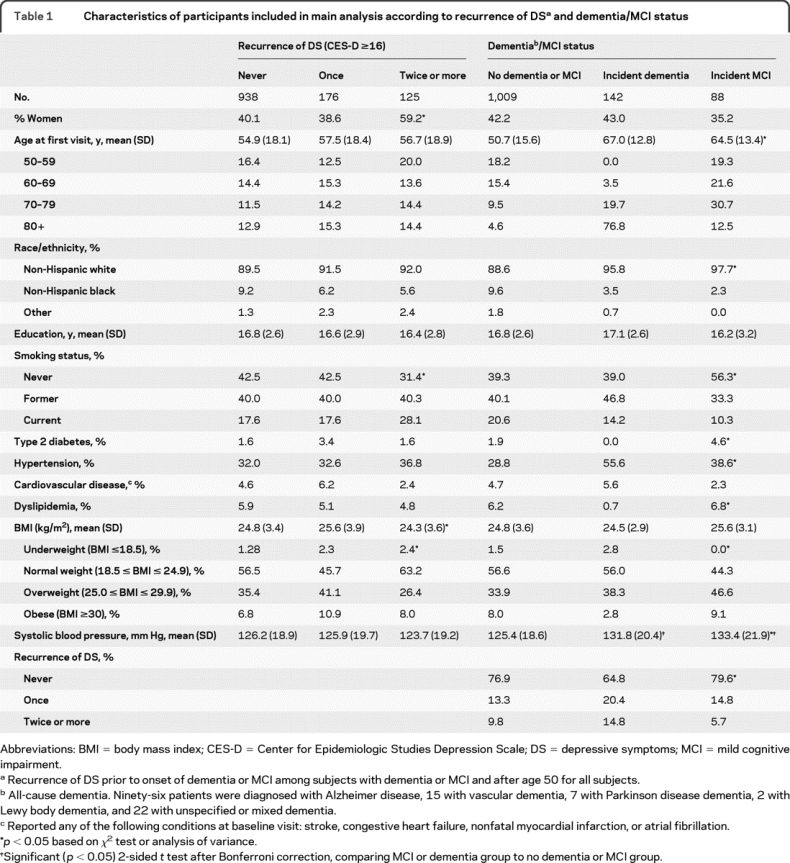
Compared to healthy subjects, patients with MCI and dementia tended to be older and had a higher prevalence of hypertension and a more elevated systolic blood pressure at baseline, although they were less likely to be of minority group and to be current smokers (p < 0.05 with Bonferroni correction). Subjects who developed dementia had a lower prevalence of type 2 diabetes and reported dyslipidemia than healthy subjects.
Recurrent DS, dementia, and MCI: Kaplan-Meier survival curves.
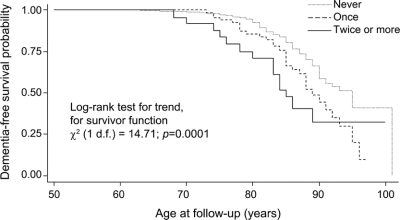
Figures 1 and 2 show Kaplan-Meier survival curves for incident cognitive outcomes comparing 3 levels of recurrent EDS during follow-up, namely 0, 1, or 2+ episodes (time-independent variable). When the cognitive outcome considered was incident all-cause dementia, there was a clear dose-response relationship whereby the more recurrent the DS, the higher the probability of incident dementia at each age (p < 0.001; see figure 1). Analysis of AD cases only (n = 96) and all cognitive impairment cases (dementia plus MCI) revealed a similar pattern (p = 0.0350 for AD, p = 0.0146 for all cognitive impairment; data not shown). In a sensitivity analysis of all-cause dementia stratifying by sex, the log-rank test for trend was significant (p < 0.05) only among women.
Figure 1 Kaplan-Meier survival curve of time to incidence of dementia by recurrence of depressive symptoms (DS)
Results are based on Cox proportional hazards model and log-rank test for trend. Recurrence of DS was based on the number of visits in which the Center for Epidemiologic Studies Depression Scale (CES-D) score was ≥16. The variable was time-dependent so that a person can be without a history of elevated DS in 1 period of time, screening positive once in another, and twice or more in a subsequent period of time, in a cumulative fashion. However, visits with missing CES-D scores were considered as missing for the time-dependent variable. This analysis was based on 142 failures.
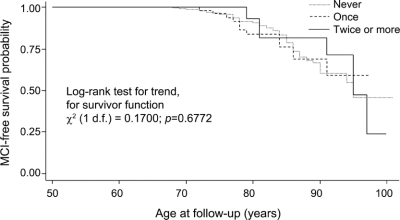
Figure 2 Kaplan-Meier survival curve of time to incidence of mild cognitive impairment (MCI) by recurrence of depressive symptoms (DS)
Results are based on Cox proportional hazards model and log-rank test for trend. Recurrence of DS was based on the number of visits in which the Center for Epidemiologic Studies Depression Scale (CES-D) score was ≥16. The variable was time-dependent so that a person can be without a history of elevated DS in 1 period of time, screening positive once in another, and twice or more in a subsequent period of time, in a cumulative fashion. However, visits with missing CES-D scores were considered as missing for the time-dependent variable. This analysis was based on 86 failures.
When incident MCI was considered as the outcome of interest (figure 2), MCI-free survival probability did not differ between levels of recurrent DS (p = 0.6772).
Recurrent DS, dementia, and MCI: Cox proportional hazards models.
Table 2 presents the findings from a series of Cox proportional hazards models examining the risk of dementia in relation to EDS recurrence as both a continuous (1–14) and a categorical (0, 1, and 2+) variable, controlling for sociodemographic, lifestyle, and health-related factors. In models using EDS as a continuous variable, each occurrence of EDS prior to onset of dementia or by end of follow-up was associated with a 14% increase in risk of all-cause dementia. The incidence of AD and all cognitive impairment (dementia + MCI) was not associated with EDS recurrence over time (AD hazard ratio [HR] 1.06; 95% CI 0.90–1.25; p = 0.455; all cognitive impairment HR 1.07; 95% CI 0.96–1.18; p = 0.204).
Table 2 Risk of dementia by time-dependent recurrent DS (continuous and categorical) among the population at risk, excluding MCI cases: Results from Cox proportional hazards models
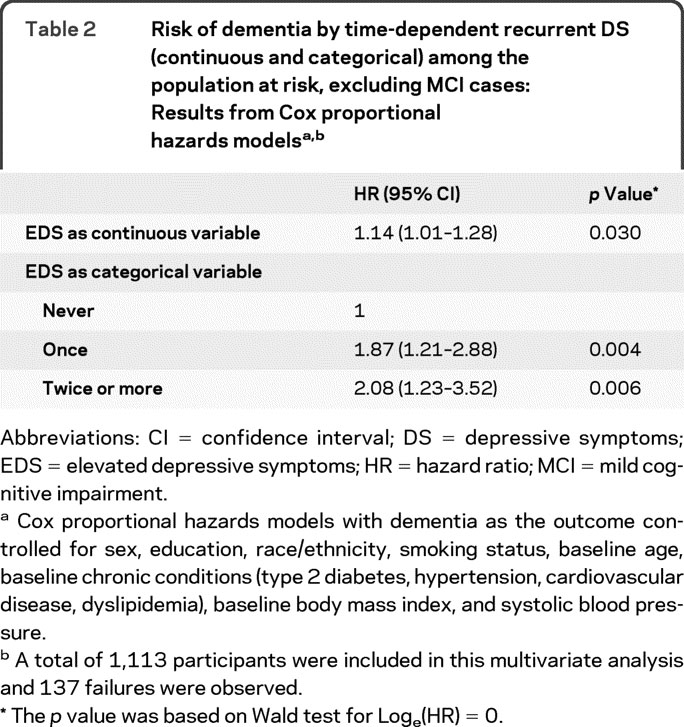
When examining EDS as a categorical variable, having 1 EDS during follow-up was associated with an 87% average increase in risk of dementia (HR 1.87; 95% CI 1.21–2.88), whereas having 2 or more EDS during follow-up almost doubled the risk of dementia compared to having no EDS throughout the study interval (HR 2.08; 95% CI 1.21–2.88; p = 0.006). There was no sex × DS interaction (p > 0.05; Wald test) in a separate model with sex included in the main effects. Having 1 EDS (HR 1.83; 95% CI 1.10–3.02; p = 0.019), but not having 2 or more episodes (HR 1.47; 95% CI 0.73–2.97; p = 0.275), was associated with AD incidence compared to having no history of EDS.
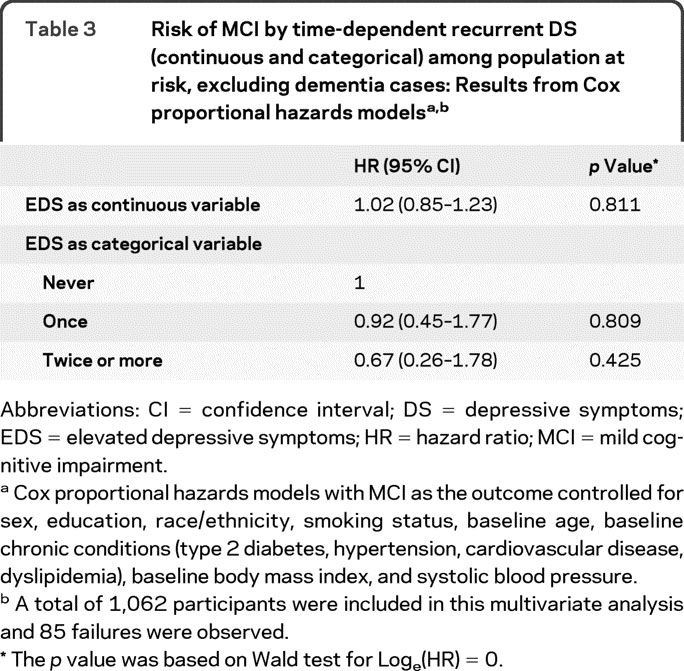
Similar analyses conducted with incident MCI are presented in table 3. HRs in models with continuous and categorical exposures indicate that incidence of MCI was not associated with recurrent DS (p > 0.05).
Table 3 Risk of MCI by time-dependent recurrent DS (continuous and categorical) among population at risk, excluding dementia cases: Results from Cox proportional hazards models
DISCUSSION
In this prospective study of 1,239 community-dwelling older adults at risk for dementia and MCI followed for up to 51 years starting from age 50, we found a monotonic increase in dementia risk as a function of the number of EDS. Participants with 1 EDS had an 87% increased risk of developing dementia, while those with 2 or more EDS were nearly twice as likely to develop dementia. Cox proportional hazards models showed a 14% increase in dementia risk with each occurrence of an EDS. Results remained significant when controlling for a variety of potentially confounding factors. MCI was not related to recurrence of EDS.
These results are consistent with previous studies which have reported a relationship between a history of depression or DS and risk for cognitive impairment and dementia.4,5,7,24,25 Most previous studies have relied on dichotomous depression groups or continuous measures of DS at 1 time point. A dose-dependent relationship between severe depressive episodes and dementia risk was found in a study that reported an average 13% increase in the risk of dementia with every episode leading to hospitalization for depression.11 Our findings add to the existing literature by demonstrating a monotonic increase in dementia risk as a function of EDS in a community sample. In contrast to a previous report of increased dementia risk only in severe depression,26 we observed an increased risk in individuals whose CES-D scores were sufficiently elevated to be considered clinically significant but whose symptoms were not severe enough to warrant hospitalization, and for most participants, did not result in treatment of any kind.
Not all studies have shown an association between depression and dementia risk,27–29 and some found that only first episodes of depression occurring proximal to dementia onset are associated with dementia, suggesting that depression is a prodromal feature of dementia.2,3 Moreover, evidence that individuals with dementia have an increased probability of developing DS following the onset of cognitive impairment27 and that DS accompany the progression of cognitive decline suggests that DS may be a reaction to perceived loss of cognitive ability.30 Our finding of a monotonic increase in dementia risk for each EDS suggests that depression is not merely a prodrome of dementia. Indeed, we would not expect the number of previous EDS to increase dementia risk if only the episode proximal to dementia diagnosis were significant. Moreover, the average 5.92 ± 4.23-year interval between first EDS and dementia diagnosis is not consistent with depression as a prodromal symptom of dementia. Because participants in the BLSA who develop dementia do not return for regular visits, we are unable to examine the course of DS following the development of dementia to determine whether symptoms might be a reaction to cognitive loss. Thus, our findings lend the most support to the hypothesis that DS are a risk factor for the development of dementia or perhaps are related to a common neurophysiologic substrate.
Our findings would be predicted by the glucocorticoid cascade hypothesis8 since repeated EDS would result in repeated insult to the hippocampus based on this model. Research in the traumatic brain injury31 and cerebrovascular32 literature also supports the proposition that recurrent brain injury increases the risk of dementia. Because depressive disorders are a treatable cause of neural insult, understanding the relationship between recurrent depression, hippocampal damage, and dementia risk is important for identifying and treating a group of older adults who are at risk for dementia.
Vascular disease is associated with late-life depression and dementia.7 Although detailed psychiatric information is not available to determine the presence of vascular depression, we were able to distinguish between incident AD and vascular dementia in our sample. The majority of participants were diagnosed with AD, and our results remained significant when we limited the analyses to individuals with AD. Moreover, significant associations between EDS and dementia risk were found when controlling for a variety of vascular conditions. Altogether, this suggests that our findings are not completely explained by the presence of vascular depression or vascular dementia in our sample.
In a previous study of BLSA participants, only men with a history of at least 1 CES-D score ≥16 had an increased risk of dementia.25 Similarly, other studies have found that men appear to be more vulnerable to the adverse impacts of depressive syndromes on cognitive functioning and brain integrity.33,34 We did not find such a sex difference in the present study. This may be due at least in part to statistical power since the number of men in our sample, particularly in the incident dementia analysis, was smaller than the number of women. Previous demonstrations of an increased dementia risk only in men have used dichotomous depression variables or continuous measures of depression severity, rather than numbers of depressive episodes. In contrast, we compared multiple levels of depressive symptom recurrence. This approach, combined with our long follow-up period, may have provided more sensitivity in detecting the relationship between recurrent EDS and dementia risk in both men and women.
Recurrence of EDS was not associated with risk of MCI in our sample, contrary to previous reports of an increased risk of MCI as a function of either a history of depression or depressive episodes at baseline. For example, DS were associated with incident dementia in the Cardiovascular Health Study35 and Mayo Alzheimer's Disease Patient Registry36 cohorts. There are several possible explanations for our discrepant findings. First, our MCI analyses were based on a group that excluded individuals who converted to dementia during follow-up. As a result, the cognitive impairment in this group may be attributable to transient factors (e.g., current stressors) rather than incipient dementia. In that case, DS would not be expected to predict the cognitive impairment observed in those individuals. Previous demonstrations of a relationship between depressive syndromes and MCI risk may have included a mix of individuals with transient cognitive difficulties and those with prodromal dementia. Second, the association between MCI risk and depression may be greater for nonamnestic MCI than amnestic MCI,37 consistent with the well-documented relationships of depressive syndromes with executive functions and frontal lobe abnormalities.38 Consequently, we may have failed to find a relationship between DS and MCI because of the preponderance of amnestic MCI in our sample. Finally, the characteristics of the DS in our sample may differ from previous studies. It has been suggested that the relationship between DS and MCI risk is mediated by confounding factors such as chronic distress39 or antidepressant use.37 Few participants with MCI in our sample have a history of antidepressant use (19.32%), which may contribute to our null findings. Because we do not have data regarding psychological distress for our sample, we cannot rule out the possibility that our sample included fewer individuals with chronic distress.
Our study has several strengths. First, it is based on a large prospective cohort study with long follow-up time and extends previous findings by examining recurrence of DS in relation to dementia and MCI risk in a community sample. The well-characterized nature of the BLSA sample, including extensive information regarding potentially confounding lifestyle and medical variables, allows us to more confidently rule out extraneous variables that could impact our findings. Further, time-dependent exposure variables were studied, avoiding both issues of temporality and reliability due to single measurement. Study limitations include the lack of detailed information regarding psychiatric history, such as age at onset of first DS. Moreover, our measure of EDS was based on participant report of DS experienced in the week preceding testing and did not include episodes of significant DS that participants may have experienced at other times. In addition, the BLSA is a sample of convenience and is limited to primarily white, highly educated individuals. Finally, secular trends in some of the effects of certain variables were possible. However, after controlling for year of birth in our longitudinal analyses, our main findings were not altered.
Our findings contribute to a growing body of literature linking late-life depression and dementia. Because the direction of the relationship between these 2 common conditions has not been completely clarified, more longitudinal work is needed to understand the nature of the association. Our findings provide support for the contention that depression is a risk factor for dementia. Moreover, our finding of a dose-dependent association between EDS and dementia provides indirect support for the hypothesis that depression results in neural insult to the brain and in turn increases the risk for dementia. This line of work has important implications. Depression is a potentially treatable risk factor for dementia. Because the occurrence of 1 depressive episode greatly increases the risk of future episodes,40 our findings suggest that older adults with a history of depression should be closely monitored for both DS and cognitive decline. Early detection and treatment of at-risk older adults may ultimately delay the onset of cognitive impairment and dementia.
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. May A. Beydoun.
Address correspondence and reprint requests to Dr. Vonetta M. Dotson, Department of Clinical and Health Psychology, University of Florida, PO Box 100165, Gainesville, FL 32610-0165 vonetta@phhp.ufl.edu
Editorial, page 12
See also pages 21 and 35
Study funding: Supported by the Intramural Research Program of the NIH/NIA.
Disclosure: The authors report no disclosures.
Received December 4, 2009. Accepted in final form March 24, 2010.
REFERENCES
- 1.Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA 2002;288:1475–1483. [DOI] [PubMed] [Google Scholar]
- 2.Alexopoulos GS, Young RC, Meyers BS. Geriatric depression: age of onset and dementia. Biol Psychiatry 1993;34:141–145. [DOI] [PubMed] [Google Scholar]
- 3.Wetherell JL, Gatz M, Johansson B, Pedersen NL. History of depression and other psychiatric illness as risk factors for Alzheimer disease in a twin sample. Alzheimer Dis Assoc Disord 1999;13:47–52. [DOI] [PubMed] [Google Scholar]
- 4.Devanand DP, Sano M, Tang MX, et al. Depressed mood and the incidence of Alzheimer's disease in the elderly living in the community. Arch Gen Psychiatry 1996;53:175–182. [DOI] [PubMed] [Google Scholar]
- 5.Starkstein SE, Jorge R, Mizrahi R, Robinson RG. The construct of minor and major depression in Alzheimer's disease. Am J Psychiatry 2005;162:2086–2093. [DOI] [PubMed] [Google Scholar]
- 6.Butters MA, Young JB, Lopez O, et al. Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues Clin Neurosci 2008;10:345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jorm AF. History of depression as a risk factor for dementia: an updated review. Aust NZ J Psychiatry 2001;35:776–781. [DOI] [PubMed] [Google Scholar]
- 8.Sapolsky RM. Why stress is bad for your brain. Science 1996;273:749–750. [DOI] [PubMed] [Google Scholar]
- 9.Fan Y, Resnick SM, Wu X, Davatzikos C. Structural and functional biomarkers of prodromal Alzheimer's disease: a high-dimensional pattern classification study. Neuroimage 2008;41:277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jack CR, Jr., Petersen RC, Xu YC, et al. Hippocampal atrophy and apolipoprotein E genotype are independently associated with Alzheimer's disease. Ann Neurol 1998;43:303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessing LV, Andersen PK. Does the risk of developing dementia increase with the number of episodes in patients with depressive disorder and in patients with bipolar disorder?. J Neurol Neurosurg Psychiatry 2004;75:1662–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tham A, Engelbrektson K, Mathe AA, Johnson L, Olsson E, Aberg-Wistedt A. Impaired neuropsychological performance in euthymic patients with recurring mood disorders. J Clin Psychiatry 1997;58:26–29. [DOI] [PubMed] [Google Scholar]
- 13.Shock N, Greulich RC, Andres R, Arenberg D, Costa PT, Lakatta EG, Tobin J. Normal Human Aging: The Baltimore Longitudinal Study of Aging. Washington, DC: US Government Printing Office; 1984. [Google Scholar]
- 14.Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry 1968;114:797–811. [DOI] [PubMed] [Google Scholar]
- 15.Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr 1997;9 suppl 1:173–176; discussion 177–178. [DOI] [PubMed]
- 16.Kawas C, Segal J, Stewart WF, Corrada M, Thal LJ. A validation study of the Dementia Questionnaire. Arch Neurol 1994;51:901–906. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-III-R. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 18.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 1984;34:939–944. [DOI] [PubMed] [Google Scholar]
- 19.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med 2004;256:183–194. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 21.Haringsma R, Engels GI, Beekman AT, Spinhoven P. The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. Int J Geriatr Psychiatry 2004;19:558–563. [DOI] [PubMed] [Google Scholar]
- 22.Statistics/Data Analysis: release 10.0. College Station, TX: Stata Corporation; 2007. [Google Scholar]
- 23.Freedman LS. Tables of the number of patients required in clinical trials using the logrank test. Stat Med 1982;1:121–129. [DOI] [PubMed] [Google Scholar]
- 24.Bassuk SS, Berkman LF, Wypij D. Depressive symptomatology and incident cognitive decline in an elderly community sample. Arch Gen Psychiatry 1998;55:1073–1081. [DOI] [PubMed] [Google Scholar]
- 25.Dal Forno G, Palermo MT, Donohue JE, Karagiozis H, Zonderman AB, Kawas CH. DS, sex, and risk for Alzheimer's disease. Ann Neurol 2005;57:381–387. [DOI] [PubMed] [Google Scholar]
- 26.Chen R, Hu Z, Wei L, Qin X, McCracken C, Copeland JR. Severity of depression and risk for subsequent dementia: cohort studies in China and the UK. Br J Psychiatry 2008;193:373–377. [DOI] [PubMed] [Google Scholar]
- 27.Chen P, Ganguli M, Mulsant BH, DeKosky ST. The temporal relationship between DS and dementia: a community-based prospective study. Arch Gen Psychiatry 1999;56:261–266. [DOI] [PubMed] [Google Scholar]
- 28.Ganguli M, Du Y, Dodge HH, Ratcliff GG, Chang CC. DS and cognitive decline in late life: a prospective epidemiological study. Arch Gen Psychiatry 2006;63:153–160. [DOI] [PubMed] [Google Scholar]
- 29.Li YS, Meyer JS, Thornby J. Longitudinal follow-up of DS among normal versus cognitively impaired elderly. Int J Geriatr Psychiatry 2001;16:718–727. [DOI] [PubMed] [Google Scholar]
- 30.Amieva H, Le Goff M, Millet X, et al. Prodromal Alzheimer's disease: successive emergence of the clinical symptoms. Ann Neurol 2008;64:492–498. [DOI] [PubMed] [Google Scholar]
- 31.Uryu K, Laurer H, McIntosh T, et al. Repetitive mild brain trauma accelerates Abeta deposition, lipid peroxidation, and cognitive impairment in a transgenic mouse model of Alzheimer amyloidosis. J Neurosci 2002;22:446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leys D, Hénon H, Mackowiak-Cordoliani M-A, Pasquier F. Poststroke dementia. Lancet Neurol 2005;4:752–759. [DOI] [PubMed] [Google Scholar]
- 33.Lavretsky H, Kurbanyan K, Ballmaier M, Mintz J, Toga A, Kumar A. Sex differences in brain structure in geriatric depression. Am J Geriatr Psychiatry 2004;12:653–657. [DOI] [PubMed] [Google Scholar]
- 34.Videbech P, Ravnkilde B, Pedersen TH, et al. The Danish PET/depression project: clinical symptoms and cerebral blood flow: a regions-of-interest analysis. Acta Psychiatr Scand 2002;106:35–44. [DOI] [PubMed] [Google Scholar]
- 35.Barnes DE, Alexopoulos GS, Lopez OL, Williamson JD, Yaffe K. DS, vascular disease, and mild cognitive impairment: findings from the Cardiovascular Health Study. Arch Gen Psychiatry 2006;63:273–279. [DOI] [PubMed] [Google Scholar]
- 36.Geda YE, Knopman DS, Mrazek DA, et al. Depression, apolipoprotein E genotype, and the incidence of mild cognitive impairment: a prospective cohort study. Arch Neurol 2006;63:435–440. [DOI] [PubMed] [Google Scholar]
- 37.Ravaglia G, Forti P, Lucicesare A, et al. Prevalent DS as a risk factor for conversion to mild cognitive impairment in an elderly Italian cohort. Am J Geriatr Psychiatry 2008;16:834–843. [DOI] [PubMed] [Google Scholar]
- 38.Rogers MA, Kasai K, Koji M, et al. Executive and prefrontal dysfunction in unipolar depression: a review of neuropsychological and imaging evidence. Neurosci Res 2004;50:1–11. [DOI] [PubMed] [Google Scholar]
- 39.Wilson RS, Schneider JA, Boyle PA, Arnold SE, Tang Y, Bennett DA. Chronic distress and incidence of mild cognitive impairment. Neurology 2007;68:2085–2092. [DOI] [PubMed] [Google Scholar]
- 40.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry 2003;160:1147–1156. [DOI] [PubMed] [Google Scholar]