Abstract
Aim
To determine the feasibility of transporting post cardiac arrest patients to tertiary care facilities, the rate of re-arrest, and the rate of critical events during critical care transport team(CCTT) care.
Methods
Retrospective chart review of cardiac arrest patients transported via CCTT between 1/1/2001 and 5/31/2009. Demographic information, re-arrest, and critical events during transport were abstracted. We defined critical events as hypotension (systolic blood pressure<90mmHg), hypoxia (oxygen saturation<90%), or both hypotension and hypoxia at any time during CCTT care. Comparisons were performed using Chi-squared test and a Cox proportional hazards model was employed to determine predictors of events.
Results
Of the 248 patients studied, the majority was male (61%), presented in ventricular fibrillation or ventricular tachycardia (VF/VT, 50%), and comatose (80%). Re-arrest was uncommon (N=15; 6%). Critical events affected 58 patients (23%) during transport. Median transport time was 63 minutes (IQR 51, 81) in both those who experienced a critical event and those who did not. Vasopressor use was associated with any decompensation during CCTT (Hazard Ratio 1.81; 95% CI 1.29, 2.54). Three patients (20%) suffering re-arrest survived to hospital discharge. Survival (Chi square 11.77; p<0.01) and good neurologic outcome (Chi square 5.93; p=0.01) were higher in patients who did not suffer any event during transport.
Conclusions
Transport of resuscitated cardiac arrest patients to a tertiary care facility via CCTT is feasible, and the duration of transport is not associated with re-arrest during transport. Repeat cardiac arrest occurs infrequently, while critical events are more common. Outcomes are worse in those experiencing an event.
Introduction
Regionalization has led to improvements in the care of patients requiring specialized treatment including trauma [1-3], acute myocardial infarction [4] and stroke [5]. Recent studies have demonstrated that specialized, multidisciplinary care including aggressive cardiac catheterization and hypothermia can improve outcomes among post cardiac arrest patients [6-13]. While evidence suggests that a dedicated care plan improves outcomes [6, 7], the risk of transport to a facility that can provide comprehensive post-cardiac arrest care has not been examined. Highly trained critical care transport teams (CCTT) may mitigate the risk of decompensation during flight and have been successfully employed in our region for post-cardiac arrest, acute myocardial infarction, stroke, and trauma patients.
One necessary parameter is the duration of transport between the referring and referral facility. Davis, et al., suggested that transport times do not adversely affect patient outcomes; however, this preliminary study involved only ground transports from a scene with short transport times. [14] More recent studies have determined that transport times are not associated with survival in large out of hospital cardiac arrest populations [15, 16]. These data are limited, however, as transport times averaged less than seven minutes and survival was the only outcome studied [14-16]. Importantly, none of these studies have examined the effect of transport over long distances or interfacility transport from acute care facilities to tertiary care centers capable of specialized post-arrest care. [17] While the risks of repeat cardiac arrest or clinical deterioration during transport exist, CCTT are trained to address these situations.
The safety and feasibility of long-distance critical care transport of post cardiac arrest patients to tertiary care facilities is unknown. Furthermore, the balance between the benefits of additional services at tertiary facilities versus the risks of repeat cardiac arrest or clinical decompensation during transport remains unknown.
Our goal was to determine the rate of re-arrest and the frequency of critical events during critical care transport of resuscitated cardiac arrest patients. We hypothesize that transport of post cardiac arrest patients by CCTT is feasible and that the duration of transport is not associated with adverse events.
Methods
We conducted a retrospective chart review of cardiac arrest patients transported via CCTT between January 1, 2001, and May 31, 2009, to determine the frequency of repeat cardiac arrest and critical events during transport. This study was approved by the University of Pittsburgh Institutional Review Board.
The study was conducted at a single urban academic medical center that serves as a referral center for over four million people. Patients are transported from a four state region using a CCTT with seventeen aircraft. In 2007, this facility developed a program for specialized post-cardiac arrest comprehensive care including therapeutic hypothermia, aggressive coronary revascularization, rehabilitation, and secondary prevention for all patients admitted after resuscitation from cardiac arrest. [6] We noted that most patients were being referred to our facility for dedicated post-cardiac arrest care and thus included data from both before and after the program.
Two authors (AH, BM) assessed CCTT charts for demographic information, critical events during transport (re-arrest, hypotension, hypoxia), Glasgow Coma Score (GCS), transport time, and a priori defined therapeutic interventions including antiarrhythmic use (generally lidocaine or amiodarone), vasopressor infusion (i.e. dopamine, dobutamine, vasopressin, epinephrine, norepinephrine, or phenylephrine), heparin infusion, nitroglycerin infusion, and intra-aortic balloon pump (IABP) use during CCTT care. Any discrepancies between these two authors were adjudicated by one author (JCR). One author (JCR) analyzed hospital records for coronary angiography, percutaneous coronary intervention (PCI- defined as angioplasty with or without stent of ≥1 vessel), therapeutic hypothermia usage, (defined as temperature manipulation to ≤34°C as part of post-cardiac arrest care plan), IABP usage, automated implantable cardioverterdefibrillator (AICD) placement, hospital length of stay (LOS), and discharge disposition. We defined re-arrest as loss of central pulses requiring cardiopulmonary resuscitation (CPR) and/or defibrillation at any time while the patient was under the flight crew’s care. We defined critical events as hypotension (systolic blood pressure<90mmHg), hypoxia (oxygen saturation<90%), or both hypotension and hypoxia at any time while the patient was under the CCTT’s care. We reported discharge disposition using survival and good neurologic outcome. A good outcome is defined as discharge to home or to acute rehabilitation facility, which has been shown to correlate with a Cerebral Performance Category of 1 or 2. [6]
Data are presented using descriptive statistics. We combined the re-arrest and critical event groups to “any decompensation during transport group” for analysis of survival and good outcome as well as the proportional hazards model. Our primary outcome was the frequency of re-arrest during transport. Secondary outcomes were frequency of critical events during transport, factors associated with re-arrest or critical event during transport, and discharge disposition. Comparisons of outcomes between patients who suffered re-arrest versus those who did not were performed using Chi-squared test. A Cox proportional hazards model was used to determine predictors of “any event” during CCTT care. This model included age, sex, location of arrest, primary rhythm of arrest, IABP use by CCTT, vasopressor use by the CCTT, and antiarrhythmic use by the CCTT. All analyses were performed using STATA statistical software (Version 10, College Station, TX).
Results
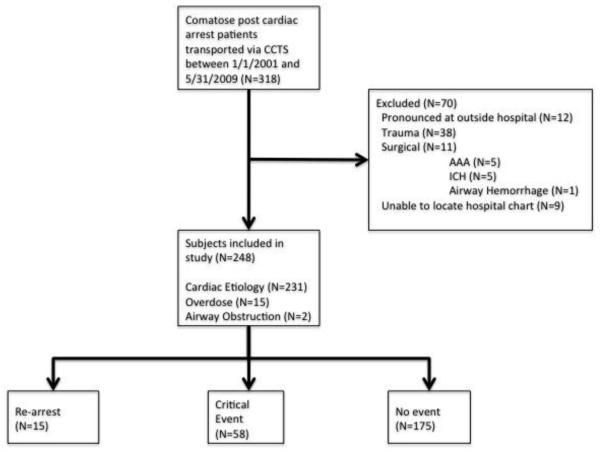
Three hundred eighteen patients with a diagnosis of post cardiac arrest were identified in the CCTT database. We excluded 70 patients who expired prior to transport, suffered traumatic cardiac arrest, arrested secondary to a surgical etiology, or had incomplete in-hospital data. The remaining cohort of 248 patients comprised the population for analysis. These patients were sub-classified by arrest etiology, with 231 from presumed cardiac etiologies, 15 from toxicologic overdoses, and two from primary airway obstruction. (Figure 1)
Figure 1.
Charts reviewed for inclusion in study.
The cohort was comprised of 153 males (61%) and had a mean age of 58 ±17 years. (Table 1) The most common primary rhythm of arrest was ventricular fibrillation/ventricular tachycardia (VF/VT, N=126, 51%). Eighty percent of patients were comatose prior to transport with a median GCS of 3 (IQR 3, 6). Most patients required at least one continuous infusion during transport; these included vasopressors (N=115; 46%), anti-arrhythmic drugs (N=101; 41%), heparin (N=80; 33%), and nitroglycerin (N=25; 11%). Median duration of CCTT patient care was 63 minutes (IQR 51, 81).
Table 1.
Critical care transport team demographic data and interventions by CCTT.
| No critical event (N=175) |
Critical event (N=58) |
No re-arrest (N=233) |
Re-arrest (N=15) | |
|---|---|---|---|---|
| Age (SD) | 57 (18%) | 60 (16%) | 58 (17%) | 59 (17%) |
| Male | 114 (64%) | 40 (56%) | 143 (61%) | 10 (67%) |
| Rhythm of Arrest | ||||
| VF/VT | 101 (57%) | 25 (35%) | 121 (52%) | 5 (33%) |
| PEA | 28 (16%) | 22 (31%) | 43 (18%) | 7 (47%) |
| Asystole | 19 (11%) | 11 (16%) | 27 (12%) | 2 (13%) |
| Unknown | 29 (16%) | 13 (18%) | 41 (18%) | 1 (7%) |
| Out-of-hospital cardiac arrest |
122 (69%) | 38 (53%) | 153 (65%) | 6 (40%) |
| Initial GCS (IQR) | 5.9 (4.3%) | 4.7 (3.5%) | 3 (3, 6) | 3 (3, 6) |
| Coma (GCS<9) | 3 (3, 7) | 3 (3, 6) | 184 (79%) | 14 (93%) |
| IABP | 4 (2%) | 3 (4%) | 7 (3%) | 0 (0%) |
| Anti-arrhythmic Drugs |
81 (46%) | 20 (28%) | 96 (41%) | 5 (33%) |
| Heparin | 64 (36%) | 16 (23%) | 75 (32%) | 5 (33%) |
| Nitroglycerin infusion | 22 (13%) | 3 (4%) | 24 (10%) | 1 (7%) |
| No vasopressors | 115 (65%) | 17 (24%) | 127 (55%) | 5 (33%) |
| 1 vasopressor | 50 (28) | 35 (49) | 80 (34) | 4 (27) |
| 2 vasopressors | 12 (7) | 19 (27) | 25 (11) | 6 (40) |
| Median patient care duration in minutes (IQR) |
63 (50, 82) | 63 (55, 80) | 63 (51, 81) | 70 (56, 97) |
Re-arrest during CCTT care was uncommon (N=15; 6%). (Table 2) Patients on vasopressors were not more likely to re-arrest (Chi square 2.60, p=0.10). Median transport durations were 70 minutes in patients who re-arrested versus 63 minutes in those who did not. Four patients were in arrest upon CCTT arrival, one arrested a second time during flight. Four of the in flight rearrests were VF/VT, cardiac etiology and of short duration (range: 1-5 minutes). Three of the four responded to CPR with rescue shock and were in a sinus mechanism upon hospital arrival. One patient could not be resuscitated. The other eight patients were PEA arrests with more prolonged resuscitative efforts (range: 4-13 minutes). These patients required CPR, epinephrine, and atropine. One patient received vasopressin. Seven remained in PEA on hospital arrival, while one was in a sinus mechanism on hospital arrival. Five of the PEA arrests were cardiac in etiology, one was a respiratory arrest from pneumonia leading to the cardiac arrest, one presumed secondary to septicemia, and one from presumed carbon monoxide intoxication. This patient was a scene run found in PEA arrest, was resuscitated on scene, suffered a repeat PEA arrest during the flight and could not be resuscitated.
Table 2.
Critical events, re-arrests, and outcomes during transport.
| Occurred at referring facility |
Survival | Good outcome | |
|---|---|---|---|
| No event (N=175) | -- | 92 (53%)* | 58 (33%)# |
| Any event (N=73) | 17 (23%) | 21 (29%)* | 13 (18%)# |
| Hypotension (N=50) | 11 (22%) | 16 (32%) | 10 (20%) |
| Hypoxemia (N=7) | 1 (14%) | 2 (29%) | 1 (14%) |
| Both (N=1) | 1 (100%) | 0 (0%) | 0 (0%) |
| Re-arrest (N=15) | 4 (27%) | 3 (20%) | 2 (13%) |
p<0.01 between the no event and any event groups
p<0.01 between the no event and any event groups.
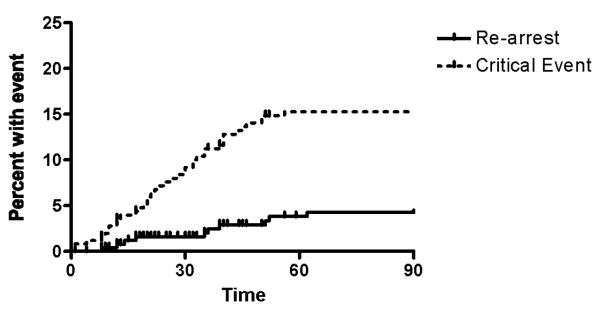
Critical events were common and affected 58 (23%) patients during transport. Patients on vasopressors were more likely to suffer a critical event (Chi square 34.26, p<0.01). Median transport durations were 63 minutes in both those who experienced a critical event and those who did not. Most re-arrests and critical events occurred during the first hour of transport with 27% of critical events occurring at the referring facility prior to departure. (Figure 2, Table 2)Patients on vasopressors were more likely to suffer any decompensation event during transport (Hazard Ratio 1.81; 95%CI 1.29, 2.54).
Figure 2.
Time to re-arrest or critical event.
After hospital arrival, the majority of patients underwent at least one diagnostic study and/or therapeutic intervention. (Table 3) One hundred twenty-six patients (51%) underwent cardiac catheterization, and 77 (31%) received PCI. Therapeutic hypothermia was initiated in 48 (20%) patients. Forty-two (17%) patients received an intra-aortic balloon pump for hemodynamic support. Implantable cardiac defibrillators for secondary prevention were placed in 29 (12%) patients. The median length of stay was 6.0 (IQR 2, 12) days.
Table 3.
Hospital interventions and outcomes.
| Coronary Angiography | 126 (51%) |
| Percutaneous Coronary Intervention |
77 (31%) |
| Therapeutic Hypothermia | 48 (20%) |
| IABP | 42 (17%) |
| AICD | 29 (12) |
| Hospital LOS in days | 6.0 (IQR 2, 12) |
| Survival | 113 (46%) |
| Good Outcome | 71 (29%) |
Overall, 113 (46%) patients survived, and 71 (29%) had a good outcome. Survival (Chi square 11.77; p<0.01) and good neurologic outcome (Chi square 5.93; p=0.01) were higher in patients who did not suffer any event during transport. Three patients (20%) suffering re-arrest during transport survived to hospital discharge, two (13%) with a good neurologic outcome.
Discussion
During the first 60 minutes of interfacility transport, re-arrest of post-cardiac arrest patients occurs in about 6% of cases, and other critical events occur in about 23% of cases. Patients experiencing re-arrest, hypotension, hypoxemia, or both hypotension and hypoxemia are less likely to survive or have a good neurologic outcome. Nevertheless, post cardiac arrest transport by a highly trained CCTT is feasible and can result in good neurologic outcomes. While this study was not designed to demonstrate a survival benefit in those patients transported to a tertiary-care facility, the high proportion of patients on vasopressor medications during transport and cardiac interventions performed at the receiving facility suggest that these patients have significant resource needs that may benefit from tertiary care. Our overall survival of 53% and survival of 29% in patients suffering a critical event are higher than those noted in the previously (19, 20), suggesting that referral of post-cardiac arrest patients to a facility with a comprehensive care plan may improve outcome despite the risk of transport. The presence of a CCTT may mitigate the risk of transport as prior work has demonstrated that patients suffering initial cardiac arrest in the presence of EMS are more likely to survive than those who do not. [18] These data have important ramifications for resource allocation. We have previously noted that development of a post-cardiac arrest service is resource intensive and may not be possible in all facilities. [6, 17] These data suggest that patients referred from outlying facilities derive benefit from transport to a comprehensive post-cardiac arrest center with an acceptable risk of decompensation during transport.
The high acuity and long transport distances in this regional post cardiac arrest cohort should be extrapolated with caution to standard advanced life support teams. Many patients required ongoing stabilization by the CCTT prior to leaving the scene or referring facility. These interventions were directed by online medical consultation with a dedicated physician and included titration of ventilator settings, titration of vasopressor infusions, and/or initiation of therapeutic hypothermia. Outcomes might be worse if transport were attempted with less trained or resource-limited crews. Importantly, the risk of re-arrest or critical event is largely noted during the first hour of transport. We noted that one in four events occurred at the referring facility, suggesting that a significant number of patients are unstable on CCTT arrival.
The median transport time of over one hour is the result of a catchment area that extends approximately 100 miles in all directions. This region is largely rural with all tertiary care assets located in a single city. A large number of patients in this region are transported by rotorcraft, as ground transportation would take three to four times as long. It is important to note that transport time was not associated with the presence of any decompensation during CCTT care.
Limitations
This retrospective observational study represents the experience of one tertiary care hospital and one CCTT and may not be generalizable. The nurse/paramedic flight teams differ from most emergency medical systems (EMS) ground crews in that they are highly trained and have extensive experience with critical care transport including the ability to transport IABP and other assist devices. The dedicated bundle of post cardiac arrest care may not be widely available at other institutions.
Our rate of survival is higher than that previously noted [19, 20]. This likely reflects selection bias of patients who have survived cardiac arrest and are referred to our tertiary care facility for post-cardiac arrest care. This is partially represented in the high rate of VF/VT in this study. Our prior work has demonstrated a higher than average survival and good outcome rate after implementation of a dedicated post-cardiac arrest care plan that may mitigate the risk of transport. [6] However, the possibility of a Hawthorne effect cannot be excluded.
Conclusion
Transport of resuscitated cardiac arrest patients to a tertiary care facility via CCTT is feasible, and the hazard of critical events is relatively constant over the first hour of transport. Repeat cardiac arrest occurs at a rate of 6% during transport. In contrast, critical events occur in an additional 23% of cases and necessitate aggressive critical care during transport of these patients. Patients on vasopressors are more likely to suffer decompensation during CCTT care. Re-arrest, hypotension, hypoxemia, or both hypotension and hypoxemia during transport are associated with lower survival and a worse neurologic outcome.
Acknowledgements
Dr. Rittenberger is supported by Grant Number 1 KL2 RR024154-02 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Dr. Rittenberger is also supported by an unrestricted grant from the National Association of EMS Physicians/Zoll EMS Resuscitation Research Fellowship.
Footnotes
Conflict of Interest Statement The authors have no conflict of interest to report.
Presented at the American Heart Association Resuscitation Science Symposium. November 14, 2009 in Orlando, Florida
Presented at the National Association of EMS Physicians Meeting, January 2010 in Phoenix, AZ.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this earlyversion of the manuscript. The manuscript will undergo copyediting,typesetting,and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content,and all legal disclaimers that apply to the journal pertain.
References
- 1.Celso B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371–8. doi: 10.1097/01.ta.0000197916.99629.eb. discussion 378. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 3.Lurie KG, Idris A, Holcomb JB. Level 1 cardiac arrest centers: learning from the trauma surgeons. Acad Emer Med. 2005;12(1):79–80. doi: 10.1197/j.aem.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Henry TD, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116(7):721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 5.Foley N, Salter K, Teasell R. Specialized stroke services: a meta-analysis comparing three models of care. Cerebrovasc Dis. 2007;23(2-3):194–202. doi: 10.1159/000097641. [DOI] [PubMed] [Google Scholar]
- 6.Rittenberger JC, et al. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79(2):198–204. doi: 10.1016/j.resuscitation.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sunde K, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73(1):29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Spaulding CM, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336(23):1629–33. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 9.Keelan PC, et al. Early direct coronary angioplasty in survivors of out-of-hospital cardiac arrest. Am J Cardiol. 2003;91(12):1461–3. A6. doi: 10.1016/s0002-9149(03)00398-9. [DOI] [PubMed] [Google Scholar]
- 10.Oddo M, et al. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006;34(7):1865–73. doi: 10.1097/01.CCM.0000221922.08878.49. [DOI] [PubMed] [Google Scholar]
- 11.Bernard SA, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 12.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–56. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds JC, et al. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. J Intensive Care Med. 2009;24(3):179–86. doi: 10.1177/0885066609332725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis DP, et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation. 2007;74(1):44–51. doi: 10.1016/j.resuscitation.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Spaite DW, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008;79(1):61–6. doi: 10.1016/j.resuscitation.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Spaite DW, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54(2):248–55. doi: 10.1016/j.annemergmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 17.Rittenberger JC, Callaway CW. Transport of patients after out-of-hospital cardiac arrest: closest facility or most appropriate facility? Ann Emerg Med. 2009;54(2):256–7. doi: 10.1016/j.annemergmed.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Hostler DP, Thomas EG, Emerson SS, Christenson J, Rittenberger JC, Bigham B, Callaway CW, Stiell IG, Vilke GM, Beaudoin T, Cheskes S, Craig A, Gorman KR, Reed A, Idris A, Nichol G. Survival after EMS witnessed cardiac arrest. Observations from the Resuscitation Outcomes Consortium (ROC) Epistry- cardiac arrest. Circulation. 2007;116:II_484. doi: 10.1016/j.resuscitation.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davs D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2009;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sasson C, Hegg AJ, Macy M, Park A, Kellermann A, McNally B. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300(12):1432–8. doi: 10.1001/jama.300.12.1432. [DOI] [PubMed] [Google Scholar]