Abstract
In the Fall 2009, the University of Pittsburgh Models of Infectious Disease Agent Study (MIDAS) team employed an agent-based computer simulation model (ABM) of the greater Washington, DC, metropolitan region to assist the Office of the Assistant Secretary of Public Preparedness and Response, Department of Health and Human Services, to address several key questions regarding vaccine allocation during the 2009 H1N1 influenza pandemic, including comparing a vaccinating children (i.e., highest transmitters)-first policy versus the Advisory Committee on Immunization Practices (ACIP)-recommended vaccinating at-risk individuals-first policy. Our study supported adherence to the ACIP (instead of a children-first policy) prioritization recommendations for the H1N1 influenza vaccine when vaccine is in limited supply and that within the ACIP groups, children should receive highest priority.
Keywords: Influenza, Pandemic, Vaccines
INTRODUCTION
Vaccine availability and allocation have been important issues during the 2009 H1N1 influenza pandemic. The unexpected pandemic left little time for vaccine production and resulted in limited vaccine availability and vaccine prioritized distribution rationing during the early fall of 2009. On July 29, 2009, the Advisory Committee on Immunization Practices (ACIP) recommended that the following groups should have higher priority to receive the H1N1 influenza vaccine based primarily on their increased risk of experiencing more severe influenza-related disease complications due contracting and transmitting influenza, particularly to the following occupational risk vulnerable populations[1]: (1) pregnant women, (2) household contacts and caregivers for children younger than 6 months of age, (3) healthcare and emergency medical services personnel, (4) all people from 6 months through 24 years of age, (5) persons aged 25 through 64 years who have health conditions associated with higher risk of medical complications from influenza.
As a result, policy makers have faced several key questions, the answers to which could have important current and future implications for pandemic preparedness: (1) how strictly should ACIP recommendations be adhered to when prioritizing who should receive the limited supplies of H1N1 vaccine? (2) how aggressively should ACIP priority groups be vaccinated? (3) within the ACIP recommended groups, which sub-group should receive greatest priority?
In the fall of 2009, the National Institutes of Health (NIH) Models of Infectious Disease Agent Study (MIDAS) network’s University of Pittsburgh modeling team assisted the Office of the Assistant Secretary of Public Preparedness and Response, Department of Health and Human Services, with these questions. Our team employed an agent-based computer simulation model (ABM) of the greater Washington, DC, metropolitan region to determine the potential effects of various vaccination scenarios, including comparing a vaccinating children-first policy based on transmissibility, advocated by Medlock and Galvani,[2] versus the ACIP-recommended vaccinating at-risk individuals-first policy.
MATERIALS AND METHODS
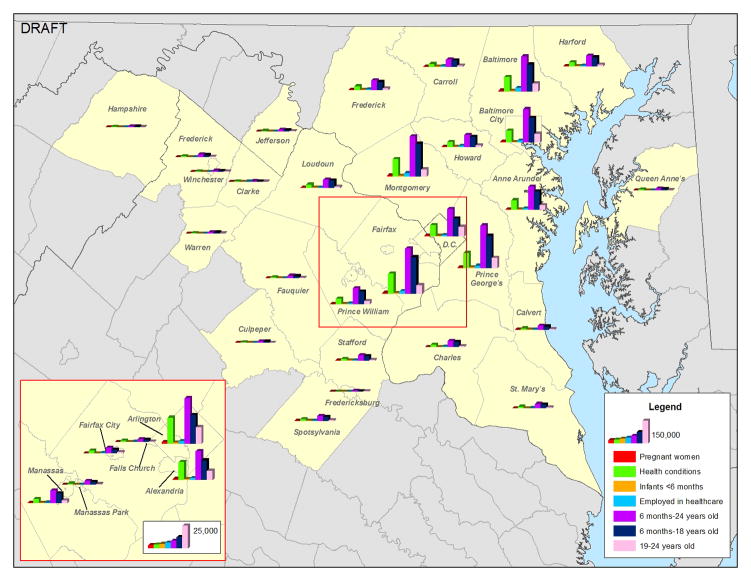
Model Structure and Synthetic Census-Based Population
Our model incorporated many methods from other previously published MIDAS simulation models.[3–5] Figure 1 illustrates the simulated Washington, DC, metropolitan region, which included five census metropolitan statistical areas (Baltimore-Towson, Washington-Arlington-Alexandria, DC-VA-MD-VA, Winchester, VA-WV, Lexington Park, MD, and Culpeper, VA), a total of 7,414,562 virtual people (i.e., computer “agents”), and virtual households, workplaces, healthcare facilities, and general community locations. A method modified from that developed by Beckman, et al. helped extract the agent population from US Census Bureau’s Public Use Microdata files (PUMs) and Census aggregated data.[6, 7] Like a virtual person, each computer agent had a set of socio-demographic characteristics (e.g., age, gender, occupation, workplace, and household location). Each simulation weekday, the agents like virtual people, moved among their respective households, their assigned workplaces (or schools depending on their age), and various locations in the community, where they interacted with other agents who were family members, household members, classmates, and office mates.[7] On weekends, schools and many workplaces closed, prompting agents to increase their community interactions by 50%. A minority (20%) of employees continued to work on weekends. Table 1 lists some key characteristics of the virtual population.
FIGURE 1.
Distribution of ACIP H1N1 Vaccine Priority Groups in Washington DC Metropolitan Region
Table 1.
Key Model Inputs
| Parameter | Age Group | Sources | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to 5 Months | 6 to 23 Months | 2 to 4.9 Years | 5 to 18 Years | 19 to 24 Years | 25 to 49 Years | 50 to 64 Years | 65 Years + | ||
| United States Population (millions) | 2.10 | 6.30 | 12.60 | 53.02 | 29.66 | 106.31 | 55.18 | 38.87 | [29] |
| DC Metropolitan Region Population | 0.052 | 0.16 | 0.32 | 1,52 | 0.48 | 3.00 | 1.16 | 0.73 | [29] |
| H1N1 Hospitalization Ratio per 100 Cases | 0.70 | 0.70 | 0.70 | 0.27 | 0.27 | 0.56 | 1.06 | 1.55 | [30] |
| H1N1 Case Fatality Ratio per 100 Cases | 0.022 | 0.022 | 0.022 | 0.009 | 0.136 | 0.136 | 0.136 | 0.028 | [30] |
| Residual Remote H1N1 Immunity (%) | 0.0% | 0.0% | 0.0% | 2.0% | 2.0% | 6.0% | 9.0% | 34.0% | [23] |
| Percent At-Risk (Immunocompromised) | 0.01% | 0.02% | 0.03% | 0.24% | 0.68% | 1.31% | 3.27% | 6.14% | [31, 32] |
| Percent At-Risk (> 1 chronic condition) | 1.5% | 4.2% | 8.83% | 11.68% | 12.35% | 15.70% | 30.56% | 47.01% | [32] |
| Live Attenuated Virus Vaccine Efficacy | N/A | N/A | 0.25 (1-dose) 0.7 (2-doses) | 0.83 | 0.83 | 0.83 | N/A | N/A | 33, 34] |
| Inactivated Virus Vaccine Efficacy (Novartis) | N/A | N/A | N/A | 0.78 | 0.78 | 0.78 | 0.73 | 0.5 | [33, 34] |
| Inactivated Virus Vaccine Efficacy (GSK) | N/A | N/A | N/A | N/A | 0.78 | 0.78 | 0.73 | 0.5 | [33, 34] |
| Inactivated Virus Vaccine Efficacy (CSL) | N/A | N/A | N/A | N/A | 0.78 | 0.78 | 0.73 | 0.5 | [33, 34] |
| Inactivated Virus Vaccine Efficacy (Sanofi) | N/A | 0.15(1-dose) 0.5(2-doses) | 0.25(1-dose) 0.7(2-doses) | 0.78 | 0.78 | 0.78 | 0.73 | 0.5 | [33, 34] |
Disease Parameters and Model Calibration
Disease parameters and assumptions came from previous MIDAS models.[3, 4, 8–20] Table 2 delineates contact rates and transmission probabilities. Exposed and then infected individuals progressed through Susceptible-Exposed-Infectious-Recovered states. At the start of each simulation (on Simulation Day 1), 100 agents were randomly chosen for initial infection. Unexposed and unvaccinated individuals began the simulation susceptible (S) to influenza. Every susceptible individual who contacted an infectious individual had a probability of contracting influenza, derived from prior studies of the 1957–8 Asian influenza pandemic.[3, 13, 21] Each newly infected person then moved to the exposed (E) state for the duration of the disease’s incubation period, then to the infectious state (I) where the person could infect others for the duration of the disease’s infectious period, and then finally to the recovered state (R), in which he or she was immune to subsequent infections. Vaccination (one dose for those 10 years or older and two doses for those younger than 10 years) had a probability (i.e., vaccine efficacy) of moving a susceptible (S) individual into the recovered (R) state by providing the individual immunity. Initial model calibration utilized the Ferguson et al. approach with data from historical (1957–58, 1968–69) influenza pandemics and targeted an epidemic with a 33.5% attack rate (AR) seen in the 1957–58 pandemic.[3] The Office of the ASPR provided vaccine production and availability schedules as of October 2009.
TABLE 2.
Model Transmission and Person-to-Person Contact Parameter Values
| Transmission Probabilities (Given Contact between Individuals) | |||
|---|---|---|---|
| Location | Infected Individual | Susceptible Individual | Transmission Probability* |
| Household | Adult | Adult | 0.4 |
| Household | Child | Adult | 0.3 |
| Household | Adult | Child | 0.3 |
| Household | Child | Child | 0.6 |
| Workplace | Adult | Adult | 0.0575 |
| Elementary School | Student | Student | 0.0435 |
| Middle School | Student | Student | 0.0375 |
| High School | Student | Student | 0.0315 |
| Community | All | Child | 0.0048 |
| Community | All | Adult | 0.0048 |
| Hospital | HCW | HCW | 0.0575 |
| Hospital | HCW | Patient | 0.01 |
| Hospital | Patient | HCW | 0.01 |
| Contact Parameters | |||
| Location | Individual | Mean Contacts Per Day | |
| Household | Household Member | Everyone in Household | |
| Classroom | Teacher | 15 | |
| Classroom | Student | 15 | |
| School outside of classrooms | Student | 13.5 | |
| School Outside of school | Student | 16.2 | |
| Community | Student (weekends) | 24.1 | |
| Community | All (including students) | 32.4 | |
| Workplace (office) | Worker | 8 | |
| Workplace (outside office) | Worker | 2 | |
| Health care Facility | Health care worker that sees patients | 30 | |
Our simulation runs employed the latest estimates of the current H1N1 pandemic, including a basic reproductive rate (R0) of 1.3, which is the expected number of secondary cases that a typical infected individual will produce in completely susceptible population. Estimates of prior immunity among specific age groups were also included. Case fatality rates were estimates of the H1N1 pandemic as of September 2009[1, 22–24]. Our model assumed that 20% of patients hospitalized with influenza would end up in the intensive care unit[25, 26], 7.5% would require mechanical ventilation.[26] and 52% of ventilated patients would not survive[23]. Antiviral medications (i.e., neuraminidase inhibitors) were utilized only for treating seriously ill patients and were 70% efficacious in decreasing transmission and 70–80% efficacious in decreasing mortality.[21, 27, 28]
Computational Specifics
The ABM was programmed in C++. Simulations were performed at the Pittsburgh Supercomputing Center on Axon, an Intel Xeon based Infiniband cluster. Each simulation is run using parallel computing over 20 computer nodes, taking an average of 10 minutes on each node (200 hours of total computer time).
RESULTS
Each presented result is the average of 20 simulation runs. Table 2 displays the output of the following vaccination scenarios: (1) vaccinating ACIP priority groups first without allowing any non-ACIP individuals to receive vaccine until 40% coverage of ACIP priority groups is achieved, vaccinating ACIP priority groups first but allowing increasing proportions (25%, 50%, 75%) of non-ACIP priority individuals to enter the priority vaccination queue, (2) including versus not including 18 to 24 year old individuals in the ACIP-priority groups, (3) prioritizing within the ACIP priority groups (e.g., children versus high-risk), (4) varying the coverage of the ACIP priority group.
As can be seen, allowing more non-ACIP priority group individuals into the initial vaccination queue increased the number of infected people, hospitalizations, and costs. Lowering the younger age threshold from 24 years old to 18 years old, thereby excluding most college-age individuals, did not have a significant effect. Prioritizing children rather than the entire ACIP priority group generated a slightly lower overall serologic attack (infection) rate. However, simply favoring children over high-risk individuals led to more hospitalizations and ultimately higher cost, since high-risk individuals, although are not necessarily high mixers and transmitters, but are at greater jeopardy for influenza-related complications.
DISCUSSION
When influenza pandemics arrive unexpectedly, limited vaccine availability can be expected, leading to challenging vaccine allocation decisions. The decision to deny some individuals access to the H1N1 vaccine in favor of other higher priority (e.g. risk) individuals is a difficult decision that should be grounded in as much available evidence as possible. Local decision makers may also experience delicate decisions on stringency of adhering to recommendations versus maximizing use of available vaccine to achieve a beneficial end result. Computer simulations can be useful adjuncts to decision making, especially since large- scale clinical trials and epidemiological studies may be difficult to perform.
Prioritizing ACIP-defined at-risk populations, rather than just the high transmitters (i.e., children), may result in slightly more influenza cases but less overall morbidity and mortality, which corresponds to lower overall costs. In contrast to our study, the Medlock and Galvani study focused on overall attack rate rather than morbidity, mortality, and resulting economic impact.[2] However, school-aged children tend not too have more severe influenza outcomes (e.g., hospitalization or death). Our results emphasize the importance of accounting for both high transmitters and individuals more likely to have poor outcomes when determining vaccination prioritization.
Limitations
All computer models are simplifications of reality and can never account for every possible factor or interaction. Rather than make decisions, computer models provide information to decision makers about possible scenarios and relationships. Data collection for the H1N1 influenza pandemic is ongoing and inputs and assumptions may change as the pandemic evolves.
Conclusions
Our study supports adherence to the ACIP prioritization recommendations for the H1N1 influenza vaccine during the 2009 pandemic when vaccine is in limited supply, with children receiving priority over high-risk patients with the ACIP groups. While prioritizing children rather than using the ACIP recommendations may reduce the overall attack rate, it also will result in more hospitalizations and cost to third party payers and society.
Table 3.
Effects of Different Vaccination Scenarios (R0 = 1.3)
| DC Metro Area |
United States |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Serologic Attack Rate |
Hospitalizations |
Costs ($US Billion) |
Hospitalizations |
Costs ($US Billion) |
||||||||
| Scenario | Total | At Risk | Total | At Risk | Third Party Payer | Productivity | Societal | Total | At Risk | Third Party Payer | Productivity | Societal |
| No Mitigation | 30.1% | 25.1% | 6,518 | 1,330 | 0.06 | 1.52 | 1.58 | 267,312 | 54,541 | 2.45 | 62.39 | 64.84 |
| Vaccinating ACIP Priority | 22.5% | 17.9% | 4,187 | 3,002 | 0.04 | 1.14 | 1.18 | 171,686 | 123,126 | 1.73 | 46.72 | 48.46 |
| Allowing Varying Percentages of non-ACIP Priority into Queue | ||||||||||||
| 25% non-ACIP Priority | 22.9% | 18.6% | 4,299 | 3,076 | 0.04 | 1.16 | 1.20 | 176,295 | 126,144 | 1.77 | 47.63 | 49.40 |
| 50% non-ACIP Priority | 23.3% | 19.1% | 4,414 | 3,183 | 0.04 | 1.18 | 1.22 | 181,026 | 130,520 | 1.81 | 48.33 | 50.14 |
| 75% non-ACIP Priority | 23.6% | 19.5% | 4,483 | 3,237 | 0.04 | 1.20 | 1.24 | 183,827 | 132,759 | 1.83 | 49.09 | 50.93 |
| 100% non-ACIP Priority | 24.1% | 20.0% | 4,642 | 3,380 | 0.05 | 1.22 | 1.27 | 190,357 | 138,611 | 1.88 | 50.04 | 51.92 |
| ACIP Priority with 18 year old cut-off instead of 24 year old | ||||||||||||
| 18 year old cut-off | 22.7% | 17.9% | 4,167 | 2,981 | 0.04 | 1.22 | 1.26 | 170,880 | 122,242 | 1.57 | 50.00 | 51.57 |
| Prioritizing Different Age Groups over ACIP Priority Groups | ||||||||||||
| 0 to 24 year olds | 21.5% | 18.3% | 4,223 | 3,105 | 0.04 | 1.19 | 1.23 | 173,181 | 127,323 | 1.52 | 49.00 | 50.52 |
| 5 to 11 year olds | 21.3% | 18.0% | 4,095 | 2,979 | 0.04 | 1.19 | 1.22 | 167,915 | 122,154 | 1.50 | 48.68 | 50.18 |
| 25 to 49 year olds | 22.7% | 18.8% | 4,308 | 3,120 | 0.04 | 1.26 | 1.31 | 176,677 | 127,946 | 1.77 | 51.80 | 53.57 |
| 50 Years and above | 24.5% | 19.7% | 4,538 | 3,260 | 0.05 | 1.36 | 1.41 | 186,092 | 133,673 | 2.02 | 55.97 | 57.99 |
| Vaccinating ACIP Priority with Varying Coverage | ||||||||||||
| 20% Vaccine Coverage | 21.7% | 17.5% | 4,076 | 2,923 | 0.04 | 1.10 | 1.14 | 167,155 | 119,849 | 1.68 | 45.09 | 46.77 |
| 40% Vaccine Coverage | 30.1% | 25.1% | 6,518 | 1,330 | 0.06 | 1.52 | 1.58 | 267,312 | 54,541 | 2.45 | 62.39 | 64.84 |
| 60% Vaccine Coverage | 23.3% | 17.7% | 4,155 | 2,971 | 0.04 | 1.18 | 1.22 | 170,388 | 121,834 | 1.77 | 48.41 | 50.18 |
| 80% Vaccine Coverage | 23.9% | 19.1% | 4,427 | 3,152 | 0.04 | 1.21 | 1.26 | 181,538 | 129,259 | 1.84 | 49.64 | 51.48 |
| Prioritizing Within ACIP Priority | ||||||||||||
| At-Risk Patients First | 23.2% | 17.1% | 4,050 | 2,799 | 0.04 | 1.17 | 1.22 | 166,074 | 114,799 | 1.75 | 48.18 | 49.93 |
| Age Groups First | 21.3% | 18.0% | 4,180 | 3,056 | 0.04 | 1.08 | 1.12 | 171,419 | 125,330 | 1.67 | 44.24 | 45.92 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schultz ED, Tanaka DT, Goldberg RN, Benjamin DK, Smith PB. Effect of Methicillin-Resistant Staphylococcus aureus Colonization in the Neonatal Intensive Care Unit on Total Hospital Cost. Infect Control Hosp Epidemiol. 2009 Feb 17; doi: 10.1086/596610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medlock J, Galvani AP. Optimizing influenza vaccine distribution. Science. 2009 Sep 25;325(5948):1705–8. doi: 10.1126/science.1175570. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006 Jul 27;442(7101):448–52. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halloran ME, Ferguson NM, Eubank S, Longini IM, Jr, Cummings DA, Lewis B, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci U S A. 2008 Mar 25;105(12):4639–44. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee BY, Brown ST, Cooley PC, Zimmerman RK, Wheaton WD, Zimmer SM, et al. A computer simulation of employee vaccination to mitigate an influenza epidemic. Am J Prev Med. Mar;38(3):247–57. doi: 10.1016/j.amepre.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wheaton W, Cajka J, Chasteen B, Wagener D, Cooley P, Ganapathi L, et al. In: A US geospatial database for agent-based models. Park RT, editor. NC: RTI International: RTI Press; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheaton W, Cajka J, Chsteen B, Wagener D, Cooley P, Ganapathi L, et al. Synthesized population databases: A US geospatial database for agent-based models. Jan, 2009. Submitted to RTI Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eubank S, Guclu H, Anil Kumar V, et al. Modeling disease outbreaks in realistic urban social networks. Nature. 2004;429:180–4. doi: 10.1038/nature02541. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson N, Cummings D, Cauchemez S, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 08 September. 2005;437:209–14. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson N, Cummings D, Fraser C, Cajka J, Cooley P, Burke D. Strategies for mitigating an influenza pandemic. Nature. 2006 July 27;442:448–52. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Germann T, Kadau K, Longini IJ, Macken C. Mitigation strategies for pandemic influenza in the United States. PNAS. 2006 April 11; doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halloran E, Ferguson N, Eubank S, Longini IJ, Cummings D, Lewis B, et al. Modeling targeted layered containment of an influenza pandemic in the United States. PNAS. 2008 March;25;105(12):4639–44. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Longini I, Halloran E, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159:623–33. doi: 10.1093/aje/kwh092. [DOI] [PubMed] [Google Scholar]
- 14.Longini IJ, Nizam A, Xu S, et al. Containing pandemic influenza at the source. Science. 2005 August 12;309:1083–7. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 15.Beigi RH, Wiringa AE, Bailey RR, Assi TM, Lee BY. Economic value of seasonal and pandemic influenza vaccination during pregnancy. Clin Infect Dis. 2009 Dec 15;49(12):1784–92. doi: 10.1086/649013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BY, Ercius AK, Smith KJ. A predictive model of the economic effects of an influenza vaccine adjuvant for the older adult (age 65 and over) population. Vaccine. 2009 Apr 6;27(16):2251–7. doi: 10.1016/j.vaccine.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee BY, Mehrotra A, Burns RM, Harris KM. Alternative vaccination locations: who uses them and can they increase flu vaccination rates? Vaccine. 2009 Jul 9;27(32):4252–6. doi: 10.1016/j.vaccine.2009.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee BY, Tai JH, Bailey RR, Smith KJ. The timing of influenza vaccination for older adults (65 years and older) Vaccine. 2009 Nov 23;27(50):7110–5. doi: 10.1016/j.vaccine.2009.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee BY, Tai JH, Bailey RR, Smith KJ, Nowalk AJ. Economics of influenza vaccine administration timing for children. Am J Manag Care. 16(3):e75–85. [PMC free article] [PubMed] [Google Scholar]
- 20.Lee BY, Brown ST, Cooley P, Potter MA, Wheaton WD, Voorhees RE, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. May-Jun;16(3):252–61. doi: 10.1097/PHH.0b013e3181ce594e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Longini I, Nizam A, Xu S, Undchusak K, Hanshaoworakul W, Cummings D, et al. Containing pandemic influenza at the source. Science. 2005;309:1083–9. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 22.Weycker D, Edelsberg J, Halloran M, Longini I, Ciuryla V, Oster G. Population-wide benefits of routine vaccination of children against influenza. Vaccine. 2005;23(10):1284–93. doi: 10.1016/j.vaccine.2004.08.044. [DOI] [PubMed] [Google Scholar]
- 23.Li G, Yilmaz M, Kojicic M, Fernandez-Perez E, Wahab R, Huskins W, et al. Outcome of critically ill patients with influenza virus infection. Journal of Clinical Virology. 2009 doi: 10.1016/j.jcv.2009.07.015. Article in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, et al. Pandemic potential of a strain of influenza A (H1N1): early findings. Science. 2009 Jun 19;324(5934):1557–61. doi: 10.1126/science.1176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Red Book 2009. Montvale, NJ: Thompson Healthcare Inc; 2009. [Google Scholar]
- 26.Zhang X, Meltzer M, Wortley P. FluSurge - A tool to estimate demand for hospital services during the next pandemic influenza. Medical Decision Making. 2006;26:617–23. doi: 10.1177/0272989X06295359. [DOI] [PubMed] [Google Scholar]
- 27.Merler S, Ajelli M, Rizzo C. Age-prioritized use of antivirals during an influenza pandemic. BMC Infectious Diseases. 2009;9(117):1–13. doi: 10.1186/1471-2334-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matheson N, Harnden A, Perera R, Sheikh A, Symmonds-Abrahams M. Neuraminidase inhibitors for preventing and treating influenza in children (Review) The Cochrane Collaboration. 2007;(1):1–53. doi: 10.1002/14651858.CD002744.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Age Groups and Sex: 2000. US Census Bureau: American FactFinder 2000. [cited 2009 19 October]; Available from: http://factfinder.census.gov/servlet/QTTable?_bm=y&qr_name=DEC_2000_SF1_U_QTP1&-geo_id=01000US&-ds_name=DEC_2000_SF1_U&-_lang=en&-format=&-currentselections=DEC_2000_SF1_U_QTP1&-CONTEXT=qt.
- 30.Presanis A, lIPSitch M, Angelis DD. The severity of pandemic H1N1 influenza in the United States, April - July 2009. PLoS Currents Influenza. 2009 Sep 25; doi: 10.1371/currents.RRN1042. [revised 2009 Oct 2]:RRN1042 2009;Version 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cases of HIV infection and AIDS in the United States and dependent areas, 2007. HIV/AIDS Surveillance Report. 2007:19. [Google Scholar]
- 32.Summary Health Statistics for the US Population: National Health Interview Survey, 2006. Washington DC: 2006. [Google Scholar]
- 33.Basta N, Halloran M, Matrajt L, Longini I. Estimating influenza vaccine efficacy from challenge and community-based study data. American Journal of Epidemiology. 2008;168(12):1343–52. doi: 10.1093/aje/kwn259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greensburg M, Lai M, Hartel G, Wichems C, Gittleson C, Bennet J, et al. Response after one dose of a monovalent influenza A(H1N1) 2009 vaccine - Preliminary report. New England Journal of Medicine. 2009:361. doi: 10.1056/NEJMoa0907413. [DOI] [PubMed] [Google Scholar]