Abstract
Study Objectives
This study examines nonmedical use of prescription stimulants (NPS) among 1,253 first-year college students. Comparisons are made between non-users, nonmedical users, and medical users of prescription stimulants for ADHD (ADHD+), some of whom overused their medication.
Design
Cross-sectional study.
Setting
Large public university in the mid-Atlantic region.
Subjects
Twelve hundred fifty three college students.
Measurements and Main Results
Of 1,208 students who were not using prescription stimulants medically for ADHD (ADHD-), 18.0% (n = 218) engaged in NPS. Among 45 ADHD+ students, 26.7% (n = 12) overused their ADHD medication at least once in their lifetime, and 15.6% (n = 7) nonmedically used someone else’s prescription stimulants at least once in their lifetime. Among nonmedical users, NPS was infrequent and mainly associated with studying, although 15.6% used prescription stimulants to party or to get high. Lifetime NPS was associated with past-year other drug use. Both NPS and overuse of prescribed stimulants for ADHD were independently associated with past-year use of five drugs, holding constant sociodemographic characteristics. NPS was also associated with alcohol and marijuana dependence.
Conclusions
Physicians should be vigilant for possible overuse and/or diversion of prescription stimulants among ADHD+ patients attending college, as well as the co-occurrence of illicit drug use with NPS. Initiation of comprehensive drug prevention activities that involve parents as well as colleges is encouraged to raise awareness of NPS and its association with illicit drug use.
Keywords: College students, nonmedical use of prescription stimulants, ADHD, polydrug use, drug dependence
Several medications are used in the treatment of attention deficit hyperactivity disorder (ADHD), including different formulations of methylphenidate (e.g., Concerta® (methylphenidate extended release; ALZA Corporation, Mountain View, CA)), Ritalin® (methylphenidate; Novartis Pharmaceuticals Corporation, East Hanover, NJ)) and mixtures of amphetamine salts (e.g., Adderall® (amphetamine-dextroamphetamine; Shire, Wayne, PA)).1 These medications are very effective in reducing symptoms of ADHD.2–8 During the past several years, much attention has focused on the nonmedical use of these medications, as well as other forms of prescription drugs. The general definition of nonmedical use of prescription stimulants (NPS) developed by the Substance Abuse and Mental Health Services Administration (SAMHSA) for national epidemiologic surveys is “use of any form of prescription stimulants that were not prescribed for you or that you took only for the experience or feeling they caused.”9 SAMHSA recognizes that this definition “casts a wide net” and could encompass overusing one’s own prescription.9
Several studies have examined the characteristics of college students who nonmedically use prescription stimulants. Compared to their nonusing counterparts, studies have shown that users are more likely to be male,10, 11 White,10 be a member of a fraternity or sorority,10, 12 have a lower GPA,10 and have multiple sex partners.12 One study observed a link between NPS and a combination of perfectionism and sensation-seeking personality traits.11 Although some previous investigations describing NPS among college students have distinguished between individuals with and without a diagnosis of ADHD,11, 13–15 they have been limited by inconsistencies in how NPS is defined for individuals with ADHD. The question used to assess nonmedical use on Web-based or paper and pencil surveys usually includes a qualification about “using a medication that you took on your own that was not prescribed for you.” However, the possibility still exists that ADHD+ college students could engage in NPS by taking someone else’s medication for recreational purposes in addition to taking their own therapeutic dose as prescribed. The other possibility is that ADHD+ students may overuse their own medication in order to get an increased effect, or crush and snort it to get high, as was observed in some clinically treated samples.16 It is important to determine the extent to which overuse occurs, and the reasons underlying it.
Moreover, it is important to investigate whether different formulations of stimulant medications are associated with differences in abuse liability. Pharmacologically, the reinforcing properties of stimulants are in part determined by the rate at which the drug enters the brain, as well as the rate at which it is cleared.17, 18 Slow-release preparations that are not associated with a fast escalation of dopamine levels and that allow for an extended period of dopamine blockade are thought to have less abuse liability as compared to immediate-release formulations of methylphenidate or amphetamine salt mixtures.19 By consolidating all types of prescription stimulants under one general question on a survey, researchers cannot determine which types of prescription stimulants are being overused or used nonmedically. For instance, it is important to make distinctions between different types of stimulants, such as amphetamine-dextroamphetamine, which is widely prescribed for ADHD.11, 20 Although asking about different types of prescription stimulants adds to the labor-intensiveness of the research and requires large sample sizes, it is necessary to answer critical questions.
The first aim of this study was to define the nature and extent of NPS in a sample of ADHD+ college students, including both overuse of one’s own medication and use of someone else’s medication. This information has important implications for the clinical supervision of these patients, especially when students go to college and less parental supervision is available. The second aim was to replicate and extend previous findings about the characteristics of NPS among college students who were not medically using a prescription stimulant for ADHD (and assumed not to have been diagnosed with ADHD). Third, we aimed to determine whether NPS and overuse of a medically prescribed stimulant for ADHD among college students were independently associated with an increased risk of other illicit drug use and dependence upon alcohol and marijuana.
Methods
Study Design
Sample selection occurred in two stages. First, targeting the entire class of incoming first-year students, ages 17 to 19, at a large, public university in the mid-Atlantic region, we administered a brief screening survey to 3,401 students during new-student orientation in the summer of 2004. The first-stage response rate was 89%, and the sample was similar to the target population with respect to demographics.21 This response rate is consistent with the definition of a minimum response rate as defined by the American Association of Public Opinion Research.22 A stratified random sample of those students was invited to participate in a longitudinal study, beginning with a two-hour interview administered during their first year at college. To select the longitudinal cohort sample, purposive sampling strategies were employed to obtain a disproportionate number of experienced drug users,21 but because the probability of selection was known, prevalence estimates could be obtained by weighting back to the characteristics of the screened population (n = 3,401). The second-stage response rate was 86% and yielded a final longitudinal cohort sample size of 1253 students, ages 17–20 at the time of their interviews.
Participants
The present study is based on analyses of the data gathered on these 1253 students who completed a two-hour personal interview that took place at some point during an eight-month period of time during the students’ first academic year (October 2004 through May 2005). The demographic characteristics of the sample were representative of the general population of first-year students at the university.21 Approximately half were female (51.4%), 72.4% were White, and as a proxy of socioeconomic status, 73.5% indicated their mother had attained a 4-year college degree or more. Respondents received $5 for participating in the screener and $50 for completing the interview. More details on recruitment, weighting procedures and data collection methods can be found elsewhere.21 Informed consent was obtained for participation. A federal Certificate of Confidentiality was also obtained. The study was reviewed and approved by the University Institutional Review Board.
Measures
The field staff team consisted of 18 part-time interviewers, and many interviews were conducted by senior staff including the PI. Interviewers’ education and background varied; most were current students, either undergraduates in their senior year, or graduate students at the master’s level. All interviewers underwent extensive training by the PI and had ongoing supervision. Call-back spot-checks and other quality control measures were performed at regular intervals.
Medical Use of Prescription Stimulants for ADHD and Overuse of Prescription Stimulants
Respondents were questioned about the presence of any current health conditions for which medications had been prescribed for treatment. The following statements were read verbatim: “The next set of questions is about nonmedical use of prescription drugs. Let me begin by telling you that there are two types of nonmedical use that we are interested in. The first is when you are prescribed a drug by a doctor for a specific condition, but then use the drug in a way that is not consistent with the doctor’s orders, like using too much or too frequently. Do you have any current health conditions for which you have been prescribed medications? If so, please specify the type of condition and the name of the medication(s)”. If the respondent did not volunteer, they were asked “What about ADHD?” For individuals who answered affirmatively to the question about medical use of a prescription stimulant for ADHD, they were asked “Did you ever use the medication in a way that was inconsistent with the doctor’s prescription like I described?” Responses were recorded verbatim and later coded for the presence/absence of medical use of a prescription stimulant for ADHD, and also lifetime overuse of the medication. For ease of presentation in this paper, the abbreviation ADHD+ is defined as the medical use of a prescription stimulant for ADHD. The presence of untreated ADHD was not captured; therefore, the abbreviation ADHD- is used to denote students who were not taking any prescription medications for ADHD, and who are assumed not to have been diagnosed with ADHD. Students who indicated they had “self-diagnosed” themselves with ADHD or other attention problems were coded as ADHD-.
Nonmedical Use of Prescription Stimulants (NPS)
Because of the measurement challenges inherent in assessing nonmedical use of prescription drugs, care was taken to train interviewers to understand the nature and complexity of nonmedical use to ensure that respondents had a clear idea of what was being asked. The questioning of the respondent continued with the following statements: “The second type of nonmedical use is when you do not have a prescription, but obtain the drug from someone else. I’m going to ask you now about three types of prescription drugs that you might have used in that way. The first type of prescription drugs is prescription stimulants. For these questions, we are not interested in the use of over-the-counter stimulants (such as Dexatrim® or No-Doz®) that can be bought in drug stores or grocery stores without a doctor’s prescription.” The respondent was then shown a card of photographs of various prescription stimulants. “This card has some examples of the stimulants we are referring to. These pictures show only pills, but we are interested in any form of prescription stimulants that were not prescribed for you or that you took only for the experience or feeling they caused.”
Even students with legitimate prescriptions for various conditions were asked these questions because it was possible that they could obtain other medications illegitimately in addition to having their own. Next, participants were asked about the age at which they were first offered the drug, age at first use, lifetime and past-year frequency of use, and recency of use. The presence of lifetime use was derived from the recency of use variable. Past-year use was derived from the past-year frequency variable. Additional details were captured in qualitative, open-ended questions regarding the formulations, dosage, methods of administration, reasons for use, source, and cost of any prescription stimulants they had used nonmedically in their lifetime. Responses were recorded verbatim and reviewed to develop a coding scheme for the most frequently occurring reasons for use, which are listed in Table 1. Although respondents were asked about the dose they ingested, very few could report the dose with certainty; therefore, these data are not reported.
Table 1.
Characteristics of nonmedical use of prescription stimulants (NPS) among 225 first-year college who ever used prescription stimulants nonmedically, as defined by taking someone else’s prescription at least once in their life. Shown separately in the first two columns are students who also medically used a prescription stimulant for ADHD (ADHD+) and students who had never had never been prescribed a stimulant for ADHD (ADHD−). The third column represents all nonmedical users.
| ADHD+(n = 7) | ADHD− (n = 218) | All Lifetime Nonmedical Prescription Stimulant Users (n = 225) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Lifetime frequency of use | ||||||
| Once or twice | 3 | 42.9% | 96 | 44.0% | 99 | 44.0% |
| 3 to 11 times | 0 | 0.0% | 93 | 42.7% | 93 | 41.3% |
| 12 to 100 times | 4 | 57.1% | 25 | 11.5% | 29 | 12.9% |
| More than 100 times | 0 | 0.0% | 4 | 1.8% | 4 | 1.8% |
| Recency of use | ||||||
| Less than 2 hours ago | 0 | 0.0% | 6 | 2.8% | 6 | 2.7% |
| 1 to 7 days ago | 2 | 28.6% | 25 | 11.5% | 27 | 12.0% |
| 8 to 29 days ago | 2 | 28.6% | 38 | 17.4% | 40 | 17.8% |
| 1 to 6 months ago | 0 | 0.0% | 81 | 37.2% | 81 | 36.0% |
| 7 to 12 months ago | 0 | 0.0% | 23 | 10.6% | 23 | 10.2% |
| More than 1 year ago | 3 | 42.9% | 44 | 20.2% | 47 | 20.9% |
| Formulations used | ||||||
| amphetamine-dextroamphetamine | 7 | 100.0% | 194 | 89.0% | 201 | 89.3% |
| methylphenidate extended release | 4 | 57.1% | 27 | 12.4% | 31 | 13.8% |
| methylphenidate | 3 | 42.9% | 55 | 25.2% | 58 | 25.8% |
| Reasons for use | ||||||
| Study, focus, work | 5 | 71.4% | 160 | 73.4% | 165 | 73.3% |
| Curiosity | 0 | 0.0% | 40 | 18.3% | 40 | 17.8% |
| Get high, feel good | 1 | 14.3% | 14 | 6.4% | 15 | 6.7% |
| Stay awake to party | 1 | 14.3% | 19 | 8.7% | 20 | 8.9% |
| Peer use, peer pressure | 0 | 0.0% | 11 | 5.0% | 11 | 4.9% |
| Other reasons | 1 | 14.3% | 12 | 5.5% | 13 | 5.8% |
| Missing | 0 | 0.0% | 2 | 0.9% | 2 | 0.9% |
| Combination of reasons | ||||||
| Recreation (get high or stay awake) | 2 | 28.8% | 33 | 15.1% | 35 | 15.6% |
| Recreation only | 1 | 14.3% | 12 | 5.5% | 13 | 5.8% |
| Study only | 4 | 57.1% | 127 | 58.3% | 131 | 58.2% |
| Party and study | 1 | 14.3% | 16 | 7.3% | 17 | 7.6% |
| Method of administration | ||||||
| Swallowed pill whole | 4 | 57.1% | 169 | 77.5% | 173 | 76.9% |
| Crushed | 2 | 28.6% | 31 | 14.2% | 33 | 14.7% |
| and inhaled | 2 | 28.6% | 30 | 13.8% | 32 | 14.2% |
| and took with food | 0 | 0.0% | 1 | 0.5% | 1 | 0.4% |
| Missing | 1 | 14.3% | 30 | 13.8% | 31 | 13.8% |
| How stimulants were obtained | ||||||
| Friend with prescription | 7 | 100.0% | 170 | 78.0% | 177 | 78.7% |
| Friend without prescription | 1 | 14.3% | 34 | 15.6% | 35 | 15.6% |
| Friend, unknown prescription status | 0 | 0.0% | 15 | 6.9% | 15 | 6.7% |
| Stranger | 0 | 0.0% | 4 | 1.8% | 4 | 1.8% |
| Family member with prescription | 0 | 0.0% | 7 | 3.2% | 7 | 3.1% |
| Stole from pharmacy | 0 | 0.0% | 1 | 0.5% | 1 | 0.4% |
| Unknown | 0 | 0.0% | 1 | 0.5% | 1 | 0.4% |
| Own prescription | 4 | 57.1% | 0 | 0.0% | 4 | 1.8% |
| Amount paid for one stimulant pill | ||||||
| $0 (free) | 7 | 100.0% | 156 | 71.6% | 163 | 72.4% |
| $1 | 0 | 0.0% | 7 | 3.2% | 7 | 3.1% |
| $2 or $3 | 0 | 0.0% | 28 | 12.8% | 28 | 12.4% |
| $4 or $5 | 0 | 0.0% | 21 | 9.6% | 21 | 9.3% |
| $10 | 0 | 0.0% | 3 | 1.4% | 3 | 1.3% |
For the analyses pertaining to other drug use and dependence upon alcohol and marijuana, lifetime NPS was coded as a binary variable according to the strict definition of using someone else’s prescription stimulants. In addition, a three-level categorical variable was constructed for medical use and overuse of prescription stimulants for ADHD: 1) no ADHD, and therefore medical use and overuse were not possible (ADHD-); 2) medical use, but no overuse reported (ADHD+ Overuse-); 3) overuse of a medically prescribed stimulant for ADHD (ADHD+ Overuse+). This strategy was desirable because it enabled us to simultaneously examine the potentially distinct effects of NPS (using someone else’ prescription), overuse of prescribed ADHD medication, and legitimate medical use of ADHD medication.
Nonmedical Use of Other Prescription Drugs and Illicit Drug Use
Nonmedical use of prescription analgesics and tranquilizers (including benzodiazepines) was captured within a series of questions similar to the questions described above. In addition, participants were assessed for past-year use of seven categories of illicit drugs: marijuana, inhalants, cocaine, hallucinogens, heroin, amphetamines/methamphetamine, and ecstasy. All drug use questions were modeled after the NSDUH.23
Dependence upon Alcohol and Marijuana
Alcohol dependence was assessed using a series of questions from the NSDUH.23 Consistent with the DSM-IV guidelines,24 alcohol dependence cases were defined by the endorsement of three or more of the following seven criteria: acquiring tolerance to alcohol, experiencing withdrawal symptoms, using more alcohol than intended, being unable to cut down on drinking, spending a lot of time obtaining or using alcohol, giving up important activities because of drinking, or continuing to use alcohol despite problems with physical or mental health. A similar series of questions assessed marijuana dependence. To reduce respondent burden, the dependence items were only asked for individuals who used the substance at least five times in the past year. Cases were coded as non-dependent if they met fewer than three criteria for dependence, or if they used the substance less than five times in the past year.
Statistical Analyses
Sampling weights were computed on the basis of gender, race, and history of drug use during high school, using data collected in the screener survey described above. To estimate the prevalence of NPS, unweighted and weighted frequencies were computed separately for all students (n = 1,253) and for the subset (n = 45) who were medically using a prescription stimulant for ADHD. Second, descriptive statistics were used to characterize the sample with respect to their characteristics of NPS defined as using someone else’s prescription, and excluding the eight students who had only overused their own prescriptions.
Finally, to test the hypothesized associations between NPS, medical use (and overuse) of a prescribed stimulant, and other drug use, a series of eight logistic regression analyses were conducted with past-year use of each illicit drug as the dependent variable. Heroin use was not tested in this way due to its extremely low prevalence. Two additional models were also developed with alcohol and marijuana dependence as dependent variables. In all models, both independent variables (lifetime NPS and the three-level overuse variable) were entered as the two main effects. Each model controlled for race, gender, and mother’s education. The model on alcohol dependence was restricted to individuals who had used alcohol at least once during the past year, and controlled for past-year frequency of alcohol use. Similarly, the model on marijuana dependence was restricted to past-year marijuana users and controlled for past-year frequency of marijuana use. For the three-level overuse variable, individual comparisons were evaluated for statistical significance only if the overall χ2 value was significant at p < .05.
Results
Prevalence of Medical Use of a Prescription Stimulant for ADHD
Forty-five of 1,253 students reported medical use of a prescription stimulant for ADHD. The corresponding weighted prevalence for first-year students is 3.0%wt.
Prevalence of NPS
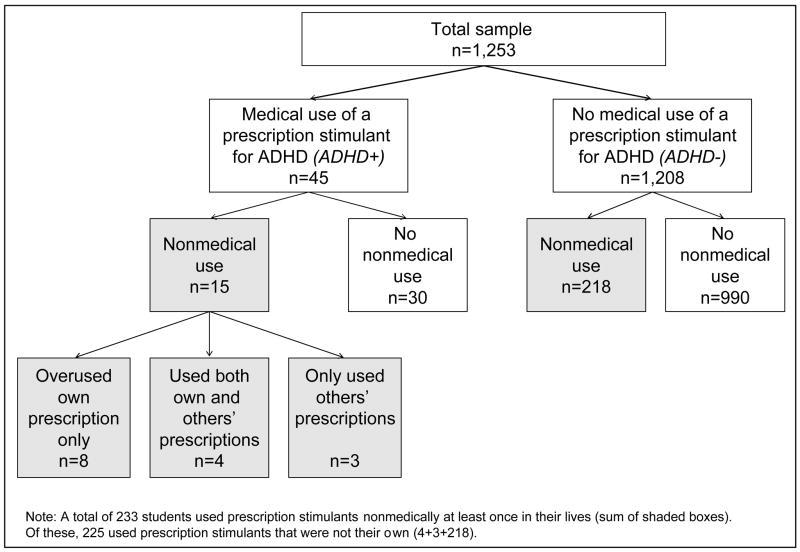
Figure 1 graphically presents the breakdown of all students in the sample (n = 1,253) with respect to NPS. The shaded boxes constitute a total of 233 individuals who used prescription stimulants nonmedically at least once in their lives, representing 13.5%wt of the general population of first-year students at the university. Among the 45 ADHD+ students, 12 (26.7%) had overused their prescribed stimulant medication for ADHD. Interestingly, four of these individuals overused their own medication and also used someone else’s prescription stimulants. Another three individuals did not overuse their own medication, even though they did use someone else’s prescription stimulants. Therefore, 15.6% (7/45) of ADHD+ students qualify for a strict definition of NPS—that is, using someone else’s prescription. The comparable proportion among ADHD- students was quite similar at 18.0% (i.e., 218/1208). However, 33.3% (i.e., 15/45) of ADHD+ students met the broadest definition of NPS (either overusing their own medication and/or using someone else’s).
Figure 1.
Classification of various forms of nonmedical use of prescription stimulants (NPS) observed in a sample of 1,253 college students.
Although an analysis of gender differences is not central to the aims of this paper, exploratory analyses revealed that, using the strict definition described above (i.e., using someone else’s medication), NPS was similarly prevalent among females (16.8%) and males (19.2%) in this sample, regardless of the medical use of a prescription stimulant for ADHD. However, among students who were medically prescribed stimulants for ADHD, overuse was somewhat higher for females (37.5%) than for males (20.7%). These data are not shown in a table as small cell sizes precluded significance testing of gender differences.
Characteristics of NPS
Table 1 presents the results of the descriptive analysis of 225 nonmedical users of prescription stimulants. Frequencies are presented separately for the seven students who were medical users of prescription stimulants who also used someone else’s prescription, because these data may be of interest to clinicians; however, because of the small number of these individuals, significance tests were not conducted. Here, we discuss the overall results (see “All” column). The lifetime frequency of use was relatively low: 44.0% of nonmedical users had used only once or twice in their lives, and the majority had used fewer than 12 times (85.3%). With respect to recency of use, fewer than one-third had used within the past month (32.5%), but the majority of lifetime users were past-year users (78.7%). In summary, the weighted prevalence of NPS for all first-year students was 10.4%wt in the past year and 4.3% wt in the past month.
Students used a variety of different prescription stimulants, with amphetamine-dextroamphetamine (89.3%) being the most commonly reported, followed by methylphenidate (25.8%). Methylphenidate extended release was nonmedically used by 13.8% of users. [Similarly, the most widely prescribed stimulant medication for ADHD was amphetamine-dextroamphetamine (53.3%), followed by methylphenidate extended release (20.0%) and methylphenidate (17.8%); these data are not shown in a table].
The reasons for using prescription stimulants are presented in Table 1. By far, the greatest number of individuals said they used stimulants to help them focus or concentrate so they could study or do schoolwork (73.3%), and over half (58.2%) said that studying was their only reason for using stimulants. Curiosity was the second most prevalent reason for use (17.8%). We constructed a “recreational use” category based on the following verbatim responses from respondents: wanting to get high, feel good or have fun (6.7%); and wanting to enhance wakefulness while partying, drinking, and going out with friends (8.9%). In total, 15.6% of users cited any of these recreational reasons for use, and very few used exclusively for recreational reasons (5.8%). A small proportion of users (4.9%) mentioned using stimulants because of peer pressure or because people around them were using them. Miscellaneous other reasons for using stimulants were reported infrequently and included “weight loss”, “staying awake to drive when they were tired”, “wanting to pass a breathalyzer test”, or “staying awake for no particular reason”.
With respect to route of administration, swallowing pills whole was most common (76.9%), and 14.7% of users crushed the pills prior to inhaling them or ingesting them with food. Of the three most prevalent types of prescription stimulants reported in this sample, inhalation was reported most frequently with methylphenidate (17.3%), somewhat less often with amphetamine-dextroamphetamine (13.1%), and very rarely with methylphenidate extended release (3.8%; data not shown in a table).
Prescription stimulants were obtained from a variety of sources, but the vast majority obtained the medication from friends, primarily from those who had a prescription (78.7%), some from those who did not have a prescription (15.6%), and less from those whose prescription status was unknown (6.7%). Nearly three-quarters obtained their pills for free (72.4%). When students did pay for them, the cost ranged from $1 to $10 per pill. Only one student reported stealing prescription stimulants and no one reported buying prescription stimulants over the Internet. The source of drug was similar regardless of recency of use. However, obtaining pills for free was less common among those who used more recently: 69.9% of past-month users, 67.8% of past-year users, and 95.6% of those whose last use was more than a year ago.
Associations with Illicit Drug Use
Table 2 presents the results of logistic regression analyses examining the association between lifetime NPS and illicit drug use. Lifetime NPS was independently and significantly associated with past-year use of all eight illicit drugs assessed. For example, 88.7% of NPS+ individuals had used marijuana in the past year, compared with 56.2% of NPS- individuals. After controlling for the effects of race, gender, mother’s education, and medical use of a prescription stimulant for ADHD, overuse of a medically prescribed stimulant for ADHD was independently associated with past-year use of hallucinogens, cocaine, ecstasy, and prescription tranquilizers. Nonmedical use of prescription analgesics was also more prevalent among overusers, although the overall χ2 did not achieve statistical significance (χ2 = 5.8, p = .06). Results were extremely similar for models on the association between past-year NPS and other drug use. However, when holding constant past-year NPS, the association between overuse of a prescription stimulant and other drug use became non-significant for all drugs except ecstasy.
Table 2.
Results of multivariate logistic regression models on the association between lifetime nonmedical use of prescription stimulants (NPS) and past-year drug use among 1,253 first-year college students. ADHD+ Overuse+ denotes medical use of a prescription stimulant for ADHD and overuse of that stimulant; ADHD+ Overuse- denotes medical use of a prescription stimulant for ADHD, but no overuse of that stimulant. “No ADHD” denotes no medical use of a prescription stimulant for ADHD and assumes the individual did not have ADHD (see text for further explanation). The effects of race, gender and mother’s education are held constant in each model. Statistically significant differences (p < .05) are bolded.
| Past-Year Drug Use | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Marijuana | Inhalants | Hallucinogens | Cocaine | ||||||||||
| % | AOR(95% CI) | p | % | AOR(95% CI) | p | % | AOR(95% CI) | p | % | AOR(95% CI) | p | ||
| NPS (lifetime) | |||||||||||||
| Yes | 88.7 | 6.9 (4.1–11.6) | <.01 | 12.2 | 3.7 (2.1–6.5) | <.01 | 30.3 | 6.4 (4.0–10.3) | <.01 | 15.4 | 10.2 (5.8–17.9) | <.01 | |
| No | 56.2 | 1.0 | 2.9 | 1.0 | 5.8 | 1.0 | 2.4 | 1.0 | |||||
| Medical use of a prescription stimulant for ADHD | |||||||||||||
| ADHD + Overuse + | 91.7 | 4.5 (.5–38.9) | .17 | 16.7 | 2.5 (0.4–17.1) | .35 | 50.0 | 6.9 (1.5–32.1) | .01 | 25.0 | 10.7 (2.7–41.6) | <.01 | |
| ADHD + Overuse - | 72.7 | 2.1 (.8–5.5) | .14 | 6.1 | 1.8 (.5–7.1) | .39 | 24.2 | 2.4 (.7–7.9) | .15 | 9.1 | .9 (.1–6.5) | .95 | |
| No ADHD | 61.7 | 1.0 | 4.6 | 1.0 | 9.8 | 1.0 | 4.6 | 1.0 | |||||
|
| |||||||||||||
| Past-Year Drug Use | |||||||||||||
| Amphetamines | Ecstasy | Prescription Analgesics | Prescription Tranquilizers | ||||||||||
| % | AOR(95% CI) | p | % | AOR(95% CI) | p | % | AOR(95% CI) | p | % | AOR(95% CI) | p | ||
|
|
|||||||||||||
| NPS (lifetime) | |||||||||||||
| Yes | 5.0 | 44.3 (8.2–240.0) | <.01 | 8.6 | 4.6 (2.1–9.7) | <.01 | 33.9 | 5.6 (3.7–8.5) | <.01 | 14.5 | 4.4 (2.5–7.9) | <.01 | |
| No | 0.2 | 1.7 | 6.9 | 2.9 | |||||||||
| Medical use of a prescription stimulant for ADHD | |||||||||||||
| ADHD + Overuse + | 0.0 | not tested | 16.7 | 7.0 (1.1–45.0) | .04 | 41.7 | 5.2 (1.3–20.7) | .02 | 25.0 | 9.1 (2.1–38.5) | <.01 | ||
| ADHD + Overuse - | 0.0 | 6.1 | 3.6 (.7–18.5) | .12 | 9.1 | .6 (.1–3.0) | .55 | 9.1 | 2.7 (.7–10.0) | .14 | |||
| No ADHD | 1.1 | 2.8 | 1.0 | 11.8 | 1.0 | 4.9 | 1.0 | ||||||
Note: No ADHD+ cases reported past-year use of amphetamines; therefore, the effect of ADHD and Overuse could not be tested. For the three-level overuse variable, individual comparisons were evaluated for statistical significance only if the overall χ2 value was significant at p < .05.
From Table 3, it can be seen that NPS is strongly associated with alcohol and marijuana dependence (AOR = 1.8 and 4.0, respectively), even holding constant demographics and past-year frequency of alcohol and marijuana use, respectively. In addition, overusers of medically prescribed stimulants were significantly more likely to be marijuana dependent than students who were not prescribed a stimulant medication for ADHD (AOR = 5.6, CI = 1.4 to 22.8). The association between overuse and alcohol dependence was similar (AOR = 4.3, CI = 1.1 to 16.0), although the overall χ2 failed to reach statistical significance (χ2 = 4.6, p = .10).
Table 3.
Results of multivariate logistic regression models on the association between lifetime nonmedical use of prescription stimulants (NPS), medical use of a prescription stimulant for ADHD (including overuse of that stimulant), and past-year dependence on alcohol and marijuana among 1,253 first-year college students. ADHD+ Overuse+ denotes medical use of a prescription stimulant for ADHD and overuse of that stimulant; ADHD+ Overuse- denotes medical use of a prescription stimulant for ADHD, but no overuse of that stimulant. “No ADHD” denotes no medical use of a prescription stimulant for ADHD and assumes the individual did not have ADHD (see text for further explanation). The effects of race, gender and mother’s education are held constant in each model. For the model with alcohol dependence as the dependent variable, the sample was restricted to 1141 individuals who used alcohol at least once during the past year, and controlled for past-year frequency of alcohol use. For the model with marijuana dependence as the dependent variable, the sample was restricted to 753 individuals who used marijuana at least once during the past year, and controlled for past-year frequency of marijuana use. Statistically significant differences (p < .05) are bolded.
| Alcohol Dependence | Marijuana Dependence | |||||
|---|---|---|---|---|---|---|
| % | AOR(95% CI) | p | % | AOR(95% CI) | p | |
| NPS (lifetime) | ||||||
| Yes | 28.8 | 1.8 (1.2–2.8) | <.01 | 23.8 | 4.0 (2.3–7.0) | <.01 |
| No | 12.8 | 5.3 | ||||
| Medical Use of a Prescription Stimulant for ADHD | ||||||
| ADHD + Overuse + | 41.7 | 4.3 (1.1–16.0) | .03 | 36.4 | 5.6 (1.4–22.8) | .02 |
| ADHD + Overuse − | 16.1 | 1.1 (0.4–3.3) | .86 | 4.6 | not tested | |
| No ADHD | 15.6 | 1.0 | 9.7 | 1.0 | ||
Note: In the ADHD+ Overuse− group, only one case was marijuana dependent; therefore, the effect of ADHD+ Overuse− could not be tested. For the three-level overuse variable, individual comparisons were evaluated for statistical significance only if the overall χ2 value was significant at p < .05.
Discussion
This study describes the prevalence of various forms of nonmedical use of prescription stimulants. In our sample of college students, 18.0% of ADHD- students used prescription stimulants nonmedically at least once in their lives, meaning they had used someone else’s medications. The comparable proportion among students who were medically using prescription stimulants for ADHD (ADHD+) was about the same: 15.6% (7/45). However, when overuse of one’s own ADHD medications is included in the definition, 33.3% of ADHD+ students could be defined as nonmedical users. Thus, even small changes in the definition of nonmedical use can greatly affect the estimated prevalence.
Earlier studies of clinical samples did not reveal major problems of abuse or diversion of prescription stimulants,25–27 while more recent studies have highlighted the possibility of overuse among children treated for ADHD. Wilens et al.28 reported that of 98 patients with ADHD, 11% diverted their medication, 22% overused it, and 10% used their medication to “get high.” Interestingly, in that study, 83% of the “misusers” in that study had a diagnosis of either a conduct disorder, substance use disorder, or both. In a separate study, Williams et al.29 reviewed the medical charts of 450 adolescents and found that 44% of ADHD patients used their own medications nonmedically.
For the purposes of comparison with prior literature, we prefer to report prevalence estimates based on nonmedical use of someone else’s prescription stimulants: 13.0% wt for lifetime and 10.4%wt for past year. These results are somewhat higher than the corresponding estimates (8.3% and 5.9%) reported in one large college student study which, like the present study, included many types of prescription stimulants.20 Moreover, by capturing multiple forms of prescription stimulants, we obtained prevalence estimates that are higher than the 2005 NSDUH, which reported that 5.8% of 18 to 25 year olds used methylphenidate at least once in their lifetime.30 Other cross-sectional studies of college students reveal a wide range of prevalence estimates for lifetime NPS, from 6.9% to 35.5%.10, 11, 14, 31, 32 The studies vary with respect to age range of the samples, response rates, and the types of stimulants assessed; however, several interesting and consistent findings have emerged and have been replicated in the present study. Consistent with earlier studies,13, 32 we found that NPS appears to be generally infrequent and sporadic, with the majority of NPS+ individuals using them less than 12 times in their lives (85.3%). We also found that most students nonmedically use stimulants “purposefully” as an academic aid, that is, to help them study or cram for exams and write papers.11, 31 We also found that the overwhelming majority of college students obtain prescription stimulants from friends, who either have or do not have a legitimate prescription.13, 33 Lastly, consistent with McCabe et al.,32 we find it noteworthy that the students taking prescribed ADHD medication were outnumbered by lifetime nonmedical users of prescription stimulants, at a ratio of nearly five to one (45 vs. 218).
In this study, the proportion of lifetime nonmedical users who cited recreational reasons for use (i.e., getting high or staying awake to party) was somewhat lower than in previous reports, which yielded estimates ranging from 19.3% to 70%.11, 13, 20, 33 Similarly, inhalation of stimulants (14.2% of lifetime nonmedical users) was also less prevalent in this study than elsewhere. Although these differences may be partially attributable to methodological differences in the wording of questions, mode of administration, or geographic differences; it seems noteworthy that the college student samples in these prior studies have all been considerably older, whereas the present sample was restricted to first-year students aged 17 to 20. Future studies with this cohort will determine the extent to which recreational NPS and inhalation might become more prevalent later in college.
In our study, multivariate analyses revealed that both overuse of medically prescribed stimulants for ADHD and NPS (using the strict definition of using someone else’s medication) were independent risk factors for past-year use of other illicit drugs, even controlling for demographics. These findings confirm those from other studies that reported a strong association between NPS and polydrug use.10, 33, 34 A meta-analysis by Wilens et al.35 concluded that the balance of evidence from six outcome studies supported the notion that individuals who were treated for ADHD were at a lower risk for developing a subsequent substance abuse disorder than children with untreated ADHD. While our study cannot speak to the association between untreated or undiagnosed ADHD and risk of illicit drug use, our finding that overuse of prescription stimulant medication was independently associated with past-year illicit drug use warrants further study. One clear implication is that college students being treated for ADHD might need more careful monitoring for the persistence of ADHD symptoms, inconsistent compliance with treatment (e.g., overuse), and possible illicit drug use. Further studies with this cohort are underway to uncover their diagnostic and treatment history with respect to ADHD, including the age at which they were first diagnosed with ADHD and whether they followed their treatment regimen consistently; the possibility of conducting clinical assessments of ADHD in the sample is also under consideration.
Limitations
The findings of this study must be tempered by the following limitations. First, while the sample was ascertained using stratified random sampling methods and not simply a volunteer or convenience sample, students were sampled from a single university, and thus, the results might not be generalizable to smaller private colleges or universities in other regions of the U.S., or to populations other than college students. Second, we defined our ADHD+ sample as the individuals who were medically using a prescription stimulant for ADHD; therefore, there is a possibility that some students in our ADHD- group would have been diagnosed with ADHD if they had received a clinical assessment. Also, although interviewers were trained to convey a non-judgmental attitude and repeatedly reassure participants about confidentiality throughout the interview, we cannot rule out the possibility that some participants underreported their drug use behaviors due to social desirability effects. Lastly, the analyses performed are cross-sectional and do not shed light on the longitudinal patterns of overuse or NPS. For example, we cannot ascertain from our statistical models whether the associated illicit drug use occurred before, after, or during the same time period as the NPS. As part of the longitudinal design of the study, the initial interview focused on lifetime drug use, whereas subsequent assessments capture more recent intervals of use; therefore, data presented here are limited with respect to details of recent drug use. Moreover, interviews were conducted throughout an eight-month period spanning the academic year, and therefore we cannot determine how many students may have initiated NPS and/or treatment for ADHD at some later point during their freshman year. Kaloyanides et al.36 showed that students who began medical use of prescription stimulants in college, in contrast to initiating medical use earlier in childhood, were more likely to have drug problems than individuals who had not used prescription stimulants medically.
Implications for Clinicians
These findings, together with the growing body of literature on the subject of NPS among college students, suggest a need for additional clinical guidelines for physicians who prescribe stimulant medications to older adolescents who are college-bound. The American Academy of Pediatrics published clinical practice guidelines for the assessment and treatment of ADHD in school-aged children in 2000.1 While extensive information was provided with regard to involvement of parents in the process of assessment and treatment, no mention was made of the risks associated with NPS.
We found that 26.7% of students who medically used a prescription stimulant for ADHD overused their medication, and that three-quarters of NPS+ individuals had obtained prescription stimulants from a friend who had a prescription. These findings suggest that, for ADHD patients in high school and college, physicians should be aware of the possibility of overuse and/or diversion of stimulant medications. Guidelines for clinical practice should include recommendations for age-appropriate educational messages tailored to these older adolescents. For example, patients should be cautioned against diverting their stimulant medications or using their friends’ medications. Although this study did not measure co-ingestion of prescription stimulants with alcohol and other drugs, we found that nonmedical use occurred in the context of “partying” for a number of students, consistent with prior studies documenting significant co-ingestion.11, 33 Physicians should therefore caution patients about the health risks associated with co-ingestion, especially considering recent evidence of the potential for serious adverse effects resulting from interactions of stimulant medications with alcohol and other drugs.33, 37 If, as suggested by the current study, the college environment poses especially high risks for ADHD patients with respect to nonmedical prescription drug use and other drug involvement, then the transition to college is an especially important time for physicians to emphasize these messages. Accordingly, physicians should monitor their ADHD patients for overuse of their medications and other forms of illicit drug use via both drug testing and self-report assessment tools.
Implications for Parent Education
If the findings of the study are replicated and confirmed, this line of inquiry has potentially important implications for prevention of NPS. First, prevention activities can be targeted toward parents. Parents of students with ADHD should be given general information about the possibility of overuse and misuse, especially if their child is in college and having to face the challenges inherent to college life, such as a heavy class schedule and multiple assignments due at similar times. Moreover, we believe that the absence of parental supervision and increased independence associated with being in a college environment may also create more risk for NPS among students with ADHD as compared to being in secondary school, where parents may be able to more closely supervise therapeutic dosing for their adolescent.
Parents of students without ADHD can also be targets for prevention messages aimed at helping them learn to recognize when their college-age child is using someone else’s prescription stimulants, and to respond proactively. Comments provided by a few respondents in our study have highlighted the possibility that in at least some cases, parents are not concerned about this behavior and sometimes even encourage it if it will lead to better grades. For example, one respondent explained that parents “understand because it relieves the pressure.” Teter et al.12 reported that nonmedical users of prescription stimulants actually have lower grades than students who do not take prescription stimulants nonmedically. Similarly, in our own sample, NPS was linked to lower grades by the end of the freshman year of college, and this association was mediated by the effect of skipping class more frequently.38
Given this information, parents should not encourage or simply turn a blind eye to this behavior; rather, they should strongly question the argument that their child’s NPS helps them meet the challenging demands of a college workload. Parents should caution against this practice because of legal risks and unknown health risks associated with taking another person’s prescription stimulants. Moreover, nonmedical use of any prescription drug should serve as a “red flag” to parents since we and others39 have consistently demonstrated the link between nonmedical use and illicit drug use and heavy drinking. Moreover, in this study we report a significant association between NPS and dependence upon alcohol and marijuana. It is possible that students who are drug dependent are more likely than non-dependent students to turn to NPS as a way of compensating for decreases in academic performance. We plan to test this hypothesis prospectively in our longitudinal study by examining incident NPS among dependent and non-dependent marijuana users.
Policy Implications
The findings of this study have implications for college administrators and campus health professionals. The effectiveness of prevention programs that specify both legal and health risks of nonmedical use of prescription drugs needs to be evaluated and could be integrated into efforts to curb tobacco and alcohol use. Placing NPS in the same context as illicit drug use—which is valid given the strong association between the two behaviors—may serve as a way to discourage students who are “on the edge,” that is, those who have had the opportunity but have not yet used the drug. The fact that less than 20% of students are using prescription stimulants nonmedically in their first year of college may be useful in crafting social marketing strategies aimed at increasing students’ awareness that this behavior is not normative.
Research Implications
From a methodological standpoint, researchers should arrive at a consensus regarding terminology, rather than continuing to use a variety of terms, such as “misuse,”13, 33 “abuse,”40 “illicit use,”12, 31 and “unsanctioned use.”41 In our estimation, NPS is a difficult behavior to assess due to the high variability in how participants subjectively interpret the wording of questionnaire items, and these difficulties are compounded with populations being treated for ADHD. Although interview methods may be subject to other limitations, such as underreporting of socially undesirable behaviors, we believe they have distinct advantages over self-administered formats for investigating a behavior as complex as NPS. Moreover, we find no evidence of underreporting based on comparisons of our prevalence estimates with prior studies, especially considering that our sample of college freshman was younger than students in most prior studies. In this study, we attempted to distinguish overuse of one’s own prescription stimulants from use of medications that were not legitimately obtained, yet we observed little substantive differences between these behaviors. We therefore recommend that researchers use a broad definition of nonmedical use with sufficient follow-up questions to clarify the context in which the drugs were obtained and used.
Another promising area of research pertains to understanding the impact of abuse-resistant formulations of prescription stimulants, and the use of non-stimulant alternatives such as atomoxetine on NPS. In this study, the most common nonmedically used prescription stimulant was amphetamine-dextroamphetamine (89.3%), followed by methylphenidate (25.8%) and lastly, methylphenidate extended release (13.8%). This finding is somewhat expected because methylphenidate extended release is formulated to be abuse resistant.18 Our finding that amphetamine-dextroamphetamine is nonmedically used more widely than other stimulant medications is consistent with prior research.20 Other studies are needed to confirm that the immediate-release form of amphetamine-dextroamphetamine is nonmedically used more frequently than the extended-release forms. Prescribing abuse-resistant formulations might be a prudent strategy for physicians to limit nonmedical use, while still gaining therapeutic benefit for ADHD patients.19
Our sample will be followed longitudinally to better understand the development of possible consequences of NPS. In another study of this cohort, we documented that between the freshman and sophomore years of college, 11.7% of NPS-naïve students became new nonmedical users of prescription stimulants, and 60.7% of prior nonmedical users continued to use from one year to the next.21 Further study is warranted to examine whether overusers of prescription stimulants for ADHD have similar or different incidence rates or rates of continuation. Future work with this cohort will examine NPS-related risk of other illicit drug problems, including health problems in the transition to adulthood, and will aim to understand whether or not students who use prescription stimulants nonmedically for academic performance purposes subsequently continue using stimulants in order to improve occupational performance. This line of research will clarify the extent of harm to public health that is associated with nonmedical use of prescription stimulants.
Acknowledgments
This study was funded by the National Institute on Drug Abuse (R01DA14845-03, Dr. Arria, PI). Special thanks are extended to our lead interviewer Erin Johnson, our Graduate Assistant Laura Garnier, the interviewing team, and the participants.
Supported by the National Institute on Drug Abuse, National Institutes of Health (Grant No. R01-DA14845).
Footnotes
Poster presented at the College on Problems of Drug Dependence, Scottsdale, AZ, June 17-22, 2006
References
- 1.American Academy of Pediatrics. Clinical practice guidelines: Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105:1158–70. doi: 10.1542/peds.105.5.1158. [DOI] [PubMed] [Google Scholar]
- 2.The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention deficit hyperactivity disorder. Arch Gen Psychiatry. 1999;56:1073–86. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 3.Greenhill LL, Halperin JM, Abicoff H. Stimulant medications. J Am Acad Child Adolesc Psychiatry. 1999;38(5):503. doi: 10.1097/00004583-199905000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Greenhill LL, Ford RE. Childhood attention-deficit hyperactivity disorder: Pharmacological treatments. In: Nathan PE, Gorman JM, editors. A guide to treatments that work. 2. New York: Oxford University Press; 2002. pp. 25–55. [Google Scholar]
- 5.Wilens TE, Spencer TJ. The stimulants revisited. Child Adolesc Psychiatr Clin N Am. 2000;9(3):573. [PubMed] [Google Scholar]
- 6.Ottenbacher KJ, Cooper HM. Drug treatment of hyperactivity in children. Dev Med Child Neurol. 1983;25:358–66. doi: 10.1111/j.1469-8749.1983.tb13772.x. [DOI] [PubMed] [Google Scholar]
- 7.Thurber S, Walker CE. Medication and hyperactivity: A meta-analysis. J Gen Psychol. 1983;108:79–86. doi: 10.1080/00221309.1983.9711481. [DOI] [PubMed] [Google Scholar]
- 8.Swanson JM, McBurnett K, Wigal T, et al. Effect of stimulant medication on children with attention-deficit disorder: A review of reviews. Except Child. 1993;60:154–62. [Google Scholar]
- 9.Colliver JD, Kroutil LA, Dai L, Gfroerer JC. Misuse of prescription drugs: Data from the 2002, 2003, and 2004 National Surveys on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. [Google Scholar]
- 10.McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: Prevalence and correlates from a national survey. Addiction. 2005;100(1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- 11.Low KG, Gendaszek AE. Illicit use of psychostimulants among college students: A preliminary study. Psychology, Health and Medicine. 2002;7(3):283–7. [Google Scholar]
- 12.Teter CJ, McCabe SE, Boyd CJ, Guthrie SK. Illicit methylphenidate use in an undergraduate student sample: Prevalence and risk factors. Pharmacotherapy. 2003;23(5):609. doi: 10.1592/phco.23.5.609.34187. [DOI] [PubMed] [Google Scholar]
- 13.Prudhomme-White B, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate student sample. J Am Coll Health. 2006;54(5):261–8. doi: 10.3200/JACH.54.5.261-268. [DOI] [PubMed] [Google Scholar]
- 14.Carroll BC, McLaughlin TJ, Blake DR. Patterns and knowledge of nonmedical use of stimulants among college students. Archives of Pediatrics and Adolescent Medicine. 2006;160(5):481–5. doi: 10.1001/archpedi.160.5.481. [DOI] [PubMed] [Google Scholar]
- 15.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. J Am Coll Health. 2006;54(5):269–78. doi: 10.3200/JACH.54.5.269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilens TE. Attention deficit hyperactivity disorder and substance use disorders. Am J Psychiatry. 2006;163(12):2059–63. doi: 10.1176/ajp.2006.163.12.2059. [DOI] [PubMed] [Google Scholar]
- 17.Spencer TJ, Biederman J, Ciccone PE, et al. PET study examining pharmacokinetics, detection and likeability, and dopamine transporter receptor occupancy of short- and long-acting oral methylphenidate. Am J Psychiatry. 2006;163:387–95. doi: 10.1176/appi.ajp.163.3.387. [DOI] [PubMed] [Google Scholar]
- 18.Doskoch P. Why isn’t methylphenidate more addictive? NeuroPsychiatry Rev. 2002;3(1) [Google Scholar]
- 19.Volkow ND. Stimulant medications: How to minimize their reinforcing effects? Am J Psychiatry. 2006;163(3):359–61. doi: 10.1176/appi.ajp.163.3.359. [DOI] [PubMed] [Google Scholar]
- 20.Teter CJ, McCabe SE, Lagrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–10. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arria AM, Caldeira KM, O’Grady KE, et al. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Subst Abus. 29(2) doi: 10.1080/08897070802418451. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The American Association for Public Opinion Research. Standard Definitions: Final dispositions of case codes and outcome rates for surveys. 4. Lenexa, KS: AAPOR; 2006. [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration. 2002 National Survey on Drug Use and Health Questionnaire. Rockville, MD: 2003. [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 25.Goldman LS, Genel M, Bezman RJ, Slanetz PJ. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. J Am Med Assoc. 1998;279(14):1100. doi: 10.1001/jama.279.14.1100. [DOI] [PubMed] [Google Scholar]
- 26.Werry JS, Aman M. Practitioners guide to psychoactive drugs for children and adolescents. 2. New York: Plenum; 1999. [Google Scholar]
- 27.Klein RG, Wender P. The role of methylphenidate in psychiatry. Arch Gen Psychiatry. 1995;52(6):429–33. [PubMed] [Google Scholar]
- 28.Wilens TE, Gignac M, Swezey A, Monutaux MC, Biederman J. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408–14. doi: 10.1097/01.chi.0000199027.68828.b3. [DOI] [PubMed] [Google Scholar]
- 29.Williams RJ, Goodale LA, Shay-Fiddler MA, Gloster SP, Chang SY. Methylphenidate and dextroamphetamine abuse in substance-abusing adolescents. Am J Addict. 2004;13(4):381–9. doi: 10.1080/10550490490483053. [DOI] [PubMed] [Google Scholar]
- 30.Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National findings (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06–4194) Rockville, MD: 2006. [Google Scholar]
- 31.Hall KM, Irwin MM, Bowman KA, Frankenberger W, Jewett DC. Illicit use of prescribed stimulant medication among college students. J Am Coll Health. 2005;53(4):167–74. doi: 10.3200/JACH.53.4.167-174. [DOI] [PubMed] [Google Scholar]
- 32.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett SP, Darredeau C, Bordy LE, Pihl RO. Characteristics of methylphenidate misuse in a university student sample. Can J Psychiatry. 2005;50(8):457–61. doi: 10.1177/070674370505000805. [DOI] [PubMed] [Google Scholar]
- 34.Barrett SP, Darredeau C, Pihl RO. Patterns of simultaneous polysubstance use in drug using university students. Hum Psychopharmacol: Clin & Exp. 2006;21(4):255–63. doi: 10.1002/hup.766. [DOI] [PubMed] [Google Scholar]
- 35.Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179. doi: 10.1542/peds.111.1.179. [DOI] [PubMed] [Google Scholar]
- 36.Kaloyanides KB, McCabe SE, Cranford JA, Teter CJ. Prevalence of illicit use and abuse of prescription stimulants, alcohol, and other drugs among college students: Relationship with age at initiation of prescription stimulants. Pharmacotherapy. 2007;27(5):666–74. doi: 10.1592/phco.27.5.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Markowitz JS, DeVane CL, Boulton DW, et al. Ethylphenidate formation in human subjects after the administration of a single dose of methylphenidate and ethanol. Drug Metab Dispos. 2000;28:620–4. [PubMed] [Google Scholar]
- 38.Arria A, O’Grady K, Caldeira K, Vincent K, Wish E. Nonmedical use of prescription stimulants and analgesics: Associations with social and academic behaviors among college students. J Drug Issues. doi: 10.1177/002204260803800406. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCabe SE, Boyd CJ, Young A. Medical and nonmedical use of prescription drugs among secondary school students. J Adolesc Health. 2007;40:76–83. doi: 10.1016/j.jadohealth.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Babcock Q, Byrne T. Student perceptions of methylphenidate abuse at a public liberal arts college. J Am Coll Health. 2000;49(3):143. doi: 10.1080/07448480009596296. [DOI] [PubMed] [Google Scholar]
- 41.Poulin C. Medical and nonmedical stimulant use among adolescents: From sanctioned to unsanctioned use. Can Med Assoc J. 2001;165(8):1039. [PMC free article] [PubMed] [Google Scholar]