Abstract
Objective
Adult posttraumatic stress symptoms (PSS) and a biomarker index of current health risk in childhood sexual abuse (CSA) survivors was investigated in relation to CSA severity, disclosure and other peri-and post-trauma factors.
Methods
A community sample of 94 African American and Latina women CSA survivors was assessed.
Results
Severe CSA predicted PSS overall, avoidance/numbing symptoms and greater biomarker risk, and was not mediated by post-trauma variables. Moderate CSA severity was mediated by post-trauma disclosure, predicted re-experiencing symptoms but was unrelated to biomarker risk. No overall ethnic differences were found.
Conclusions
Results suggest targets for interventions to improve the well-being of minority women CSA survivors.
Introduction
Despite extensive documentation of the association between childhood sexual abuse (CSA) and negative psychological and physiological sequelae in adulthood, research on the predictors and mechanisms of that association is limited. First, studies have been conducted primarily with clinical or college samples of European American women (Siegel, Sorenson, Golding et al, 1987), or without reporting the participants’ ethnic background (Mennen, 1995). The absence of studies of community samples of women from diverse ethnic backgrounds limits our understanding of how sociocultural factors may exacerbate or protect CSA victims from negative outcomes.
Second, it is not clear which aspects of CSA are more closely linked to posttraumatic stress disorder (PTSD) symptoms. Most studies to date document only whether or not CSA occurred, or provide limited information on pre-trauma contextual factors (e.g., age, gender, ethnicity and SES of the child), peri-trauma factors (e.g., type or severity of abuse, duration of abuse, relationship to perpetrator, peritraumatic dissociation) and post-trauma factors (e.g., disclosure) (Johnson, Pike & Chard, 2001). Among the latter, disclosure and self-blame have received attention in theoretical models (i.e., Spaccarelli, 1994) and empirical research (Ullman & Fillipas, 2005a: Ullman, 2007), but have not been fully investigated in women of diverse ethnic backgrounds.
Third, psychobiological dysregulation following acute and chronic stress in childhood may have long-lasting effects (Lupien, McEwen, Gunnar & Heim, 2009). For example, adult survivors of CSA have increased health problems and physical pain unaccounted for by psychiatric disorders (Sachs-Ericsson, Cromer, Hernandez & Kendall-Tackett, 2009). Yet, the relative contributions of pre, peri- and post-trauma factors for current health risk in adult CSA survivors is unknown. Health risk, operationally defined by a composite biomarker index (BI) of cumulative psychological stress burden (allostatic load), has been shown to predict mortality and morbidity in population studies (McEwen & Seeman, 1999). Examining CSA factors in relation to a BI may help shape prevention and intervention efforts.
The present study examined the role of pre-, peri- and post-trauma factors in predicting current posttraumatic stress symptoms and BI health risk in a community sample of African American and Latina women.
CSA and PTSD
Lifetime rates of PTSD in nationally representative samples of women are significantly higher for those who have histories of CSA, compared to those who do not, even while controlling for other adverse family conditions (Wyatt, Carmona, Loeb, Ayala & Chin, 2002). Such background factors as early family environment and adverse childhood experiences are important covariates of CSA and mental health outcomes (Loeb, Williams, Carmona et al., 2002; Marx, 2005; Molnar, Buka & Kessler, 2001).
Biological Impact of CSA
Recent findings suggest that sexual abuse before age 18 is associated with increased pituitary reactivity to stress and reduced hippocampal volume, culminating in a biological vulnerability to psychopathology (Heim, Newport, Heit, Graham, et al., 2000; Teicher, Tomoda & Andersen, 2006). Most post-CSA data come from retrospective studies among adult women. These studies demonstrate that sexual abuse is associated with differences in 24-hour urinary cortisol excretion (Lemieux & Coe, 1995), catecholamines (Friedman, Jalowiec, McHugo, et al, 2007), changes in autonomic activity and adrenocorticotropic hormone responses to laboratory stress (Heim, Newport, Bonsall et al., 2001), as well as deficits in size and function of the hippocampus and other neurological areas (Bremner, Vythilingam, Vermetten, et al., 1997).
CSA Characteristics
Despite inconsistencies in definitions, research typically utilizes the presence of penetration either alone or in combination with other CSA characteristics to define the incident as severe, especially compared to those involving only fondling and frottage (Johnson, et al., 2001; Wyatt, et al., 2002). CSA severity may influence risk for adult mental health symptoms, along with the duration of abuse (e.g., repeated vs. isolated incident) and the child’s relationship to the perpetrator (e.g., family member vs. stranger) (Molnar, Buka & Kessler, 2001).
Disclosure of CSA
Nondisclosure has been considered a form of avoidant coping and associated with negative outcomes (Whiffen & Macintosh, 1995) whereas disclosure (if followed by supportive responses), has been described as an active form of coping that buffers against psychological distress and dysfunction. Although disclosure in some instances may help to terminate the abuse, the majority of those who disclose their experience encounter negative reactions (Jonzon & Linblad, 2004), including being blamed or not believed, which further traumatizes the child (Ullman, 2007). Deciding not to disclose an abuse incident may therefore be more protective than disclosing it and receiving a negative response. Research suggests that more severe abuse, including longer duration, more than one perpetrator, violence, and intra-familial abuse, may be associated with negative responses to the disclosure of CSA (Jonzon & Linblad, 2004; Ullman, 2007).
The majority of children who are sexually abused do not disclose the incident (Smith, Letourneau, Saunders et al, 2000), even years later (Goodman-Brown, Edelstein, Goodman et al, 2003). The likelihood of disclosing has been associated with the child’s appraisal of how others may respond to disclosure, as well as their perceptions of responsibility for the abuse (i.e., self-blame) (Goodman-Brown, et. al., 2003). Severity of the abuse has also been investigated in relation to disclosure (Finkelhor, 1994). Given that most CSA incidents are not disclosed, it is important to target both disclosed and non-disclosed incidents in interventions for CSA survivors (Wyatt, Loeb, Solis, et al., 1999).
CSA and Self-Blame
CSA victims that blame themselves for the abuse may be at greater risk for negative mental health outcomes as adults (Spaccareli, 1994; Coffey, Leitenberg, Henning, Turner, & Bennett, 1996), and often take longer to disclose (Goodman-Brown, et al, 2003). Females, especially younger females, are more likely to blame themselves than males (Hunter, Goodwin & Wilson, 1992) and than older females if the abuse is long lasting (Whiffen & MacIntosh, 2005).
Conceptual model and study hypotheses
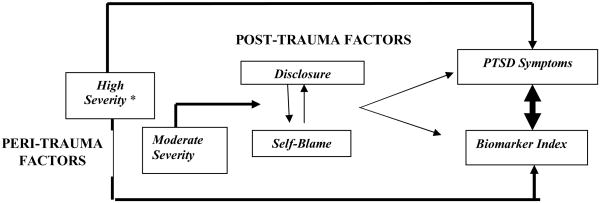
In this study, we examined peri-trauma and post-trauma factors at the first CSA episode as predictors of posttraumatic stress symptoms (PSS) and BI health risk. Recent models of pathways to PSS following physical trauma in childhood (Saxe, Stoddard, Hall, et al, 2005) and CSA (Kaplow, Dodge, Amaya-Jackson & Saxe, 2005) identify distinct predictors for avoidance/numbing symptoms versus hyperarousal symptoms and suggest that these symptom clusters represent different phenotypes of biobehavioral systems relevant for PTSD. Based on these models, we formulated a new conceptual model to guide this study. As shown in Figure 1, we propose that the peri-trauma factor of CSA severity will have a direct pathway to PSS and biomarker risk and that this direct pathway will be associated with the avoidance/numbing symptom cluster (DSM-IVR, American Psychiatric Association, 2000). In contrast, post-trauma factors of disclosure (yes/no), negative responses to disclosure from others, and self-blame for the incident are proposed to indirectly influence outcomes by modifying the effects of peri-trauma CSA severity, and will have greatest effects on the hyperarousal symptom cluster. Potential moderating effects of pre-existing contextual factors (e.g., ethnicity and childhood socio-economic status) will be explored, but are not the primary focus here.
Figure 1.
Conceptual model. Primary pathway (bold lines) indicate that peri-trauma factors predict posttraumatic stress symptoms and biomarker dysregulation. Secondary pathway predict that negative outcomes is mediated by the interaction of post-trauma disclosure and self-blame.
*Severity is defined as severe (e.g. digital penetration, attempted rape, rape, oral copulation, and anal sex) or moderate (fondling and frottage).
Our first path hypothesizes that: a) severe CSA will be directly associated with greater PSS and BI; b) this association will not be mediated by post-trauma factors; and c) this effect will primarily be associated with the avoidance/emotional numbing symptom cluster. The secondary pathway during the post-trauma period is guided by Spaccarelli’s (1994) model, which proposes that the effects of CSA on psychological outcomes are mediated by negative self-attributions (e.g., self-blame) and avoidant coping strategies (e.g. non-disclosure). In this secondary pathway we hypothesize that the impact of less severe CSA will be mediated by self-blame and negative responses to disclosure; women with moderate CSA, high self-blame (with or without disclosure) and negative responses to disclosure will evidence greater PSS than those with low self-blame, non-disclosure or disclosure without a negative response. We further hypothesize that this pathway will primarily influence hyperarousal symptoms. No ethnic differences between African American and Latina women on CSA severity, self-blame or disclosure are expected, but there may be differences in outcome patterns that reflect socio-cultural influences on how psychological and physiological distress are manifested.
Methods
Sample
A convenience sample of 132 Los Angeles County resident African American and Latina women, 18–50 years of age with histories of CSA were recruited through a network of community based organizations, hospitals, and clinics. In this study, CSA is defined as unwanted or coerced sexual body contact before age 18 (Wyatt, 1985). This physical contact may range from fondling and frottage to digital penetration and attempted or completed oral, vaginal, anal sex or rape. Women were prescreened by telephone according to the following criteria: female sex, between the ages of 18–50 years, self-reported ethnic identification as African-American or Latina, speak English, have a history of CSA, and HIV-negative by self-report. CSA history was screened with responses to nine criterion experiences of sexual abuse. Of 187 women prescreened, 132 met all eligibility criteria, and of these, 96 were consented and 94 completed the study. The study was approved by the UCLA Institutional Review Board.
Measures and Procedures
All eligible women were scheduled for an in-person interview. Transportation, childcare and refreshments were provided, and informed consent was obtained. CSA, disclosure and appraisal of CSA questions were completed in private, face-to-face interview due to the sensitivity of the topics. The remaining measures were completed by Audio Computer Assisted Self-Interview (ACASI), which has been shown to significantly decrease social desirability bias compared to face-to-face interviews and self-administered surveys (Metzger, Koblin, Turner et al, 2000). Assessments averaged 2.5 hours. Compensation of $50 and referral information was provided as needed.
Measures
Predictors
Demographic characteristics included: age, race/ethnicity, personal and household income in the past year, education, employment, occupation, household composition, and marital or relationship status.
Child sexual abuse was assessed using 9 items from the revised Wyatt Sexual History Questionnaire (Wyatt, Lawrence, Voudonon et al, 1992). Nine yes/no screening questions were asked about experiences with an adult or someone older than the victim before age 18, including fondling, frottage, attempted intercourse, intercourse, oral copulation, and digital or object penetration. A positive answer to any of these experiences was followed with questions about the age at the time of each experience and the duration. Recall was facilitated by use of bounding and framing techniques, which are designed to assist participants to recall the CSA event in more detail by anchoring the time period with other meaningful experiences.
For purposes of analyses, a dichotomous CSA severity score was calculated, with penetration indicating greater severity than non-penetrative abuse.
CSA attribution was assessed with 4 items from the Coffey et al. (1996) self-blame measure. Items included “How much do/(did) you feel that you were personally to blame for what happened?” and “How much do/(did) you feel to blame for this sexual experience occurring because you acted in a way to allow it to happen?” Responses ranged from (1) not at all to (7) very much so for a maximum total self-blame score of 28 (Cronbach α = 0.76). Due to restriction of range and violations of normality in this sample, the self-blame score was dichotemized into high (4 and above) and low levels (<3).
CSA disclosure was assessed in two stages. First, women were asked whether they ever disclosed the CSA experience, and those who answered “no” were categorized as “Not disclosed” and compared to those who had disclosed. Second, those who disclosed completed the seven-item Non-Supportive Responses to Disclosure scale of the Checklist of Sexual Abuse and Related Stressors (C-SARS; Spaccarelli, 1995). Sample questions included “Some people in your family were angry at you when they found out what happened,” and “When they found out what happened some people in your family blamed it on you.” Scores ranged from 0 (no negative responses) to 7 (maximum negative response) (Cronbach α = .70).
Covariates
Chronic stress
Current life stress was assessed with the Chronic Burden Scale (Gurung, Taylor, Kemeny & Myers, 2004), a 21-item measure of difficulties experienced in the past month from a number of stressors (e.g., economic, employment, crime, legal problems, discrimination, etc.). Responses range from (1) not a problem to (4) a major problem. A reliable sum score was calculated (Cronbach α = 0.85), with a higher score indicating greater stress burden.
Childhood Adversity
The revised 16-item Childhood Adversity measure (Kessler & McGee, 1993) was used to assess non-sexual, adverse early life experiences (e.g. severe parental incarceration, illness, disability, or death, severe poverty), with a higher score indicating greater childhood adversity (Cronbach α = 0.81).
Outcomes
Posttraumatic Stress Symptoms (PSS) was measured with the 17-symptom Posttraumatic Stress Disorder Scale (PDS; Foa, 1997), which yields both a DSM-IV PTSD diagnosis and a measure of symptom severity. Respondents report which of 12 traumatic events (e.g., accident or fire, natural disaster, sexual abuse, life-threatening illness) they have ever experienced or witnessed and identify the most disturbing event. Subsequent symptom questions are responded to in relation to that “worst” event. Symptoms experienced during the past month include clusters of re-experiencing (e.g. intrusive images, nightmares), avoidance/emotional numbing (e.g. not remembering aspects of the trauma, having restricted emotions) and hyperarousal (e.g., overly alert, easily startled) symptoms. Response options range from 0 (not at all or only one time) to 3 (five or more times a week or almost always) (Cronbach α = .90).
Biomarker Index (BI)
Seven biomarkers were used as a composite to assess current health risk: waist-to-hip ratio, resting systolic and diastolic blood pressure, and 12-hour overnight urinary cortisol, norepinephrine, epinephrine and dopamine levels. Urine samples were collected at home in a container with a preservative (0.3 g of sodium metabisulfite) by participants during a 12-hour overnight collection period within 2 days of the interview. Supplies for urine collection (a urine specimen container, toilet “hat” and cooler) were provided. Samples were kept cool in an “igloo” container until transport to the laboratory. After evaluation of total urine volume, aliquots were frozen at −80C until analyzed via EIA and Enzyme Immunoassay for the quantitative determination of endocrine concentration (cortisol and catecholamines). Safeguards for assuring compliance to urine collection procedures include measuring the volume of urine, the amount of creatinine per total volume, and the concentration of each biomarker in total and as a function of the creatinine level. Reference ranges for each of these measurements allow for identification of potentially contaminated samples that should be discarded.
A composite of the sum of risk indicators was calculated as in other studies of allostatic load (McEwen & Seeman, 1999; Glover, Stuber & Poland, 2006); the sum score represents the number of indicators (except cortisol) on which each participant scores in the top quartile of risk for the total sample. Due to replicated findings of low cortisol in PTSD samples (e.g., Glover & Poland, 2002) cortisol is calculated as a risk if the value falls within the highest or lowest 12.5% of the total sample.
Health Behaviors
The Health Behaviors Questionnaire (HBQ; Glover, 2002) was administered to assess activities in the 24 hours prior to biomarker collection that are important in interpreting the biomarker findings. Questions assess the number of caffeine drinks, cigarettes, and alcoholic beverages, the quality and amount of aerobic and anaerobic exercise, sleep, meals, use of prescribed and recreational medication, and illness symptoms. HBQ information was used to exclude urine samples that may be contaminated by known confounders and to identify potential associations with the biomarker index. Participants recorded all activities in the previous 24 hours prior to urine collection.
Statistical Analyses
Data analyses were conducted in several phases. First, frequency distributions were examined for each variable and data were categorized when necessary to achieve a normal distribution and/or to ensure adequate cell sizes for statistical analyses of the primary aims. For example, the first incident of CSA was selected as the focus for primary analyses because too few women had more than one incident to be useful. Normality and homogeneity assumptions were tested using a General Linear Model (GLM). Second, ethnic differences on the primary variables were examined with Chi-Square for categorical variables and Analysis of Variance for continuous variables. Finally, a series of mixed linear regression models were conducted for each outcome (PSS total severity, each symptom cluster, and the BI) on the total sample, with childhood adversity and adult stress burden included as covariates, and CSA severity, disclosure (or self-blame) and the severity X disclosure (or self-blame) entered in invariant order. The recommendations by Kraemer, Kiernan, Essex & Kupfer (2008) outlining the MacArthur approach to evaluating mediators and moderators were followed.
Results
The final study sample consisted of 94 women, including 63 African Americans and 31 Latinas (Table 1). The sample was relatively young (mean age = 35 years), poor (68% report little or no income) and unemployed (60%). Participants reported between 1 to 5 distinct incidents of CSA (M=1.5, SD=0.9). Multiple incidents were separated by months or years and often involved a different perpetrator. To maximize use of the entire sample all tested models focused only on the first incident of CSA. A small percentage (11%) of the sample reported that the first incident lasted less than 1 week, and 33% estimated that it lasted about one week. Of the remaining participants (57%), the range was from 2 weeks to many years (M= 4.2, SD=3.9 years). In most cases, there was one perpetrator, and this person was usually a family member (38%) or someone with whom they were familiar (51%).
Table 1.
Descriptive Characteristics of the Sample
| Total Sample (N=94) | African American (N=63) | Latina (N = 31) | |
|---|---|---|---|
| Demographics | |||
| Age Mean (SD) | 35.1(9.3) | 36.3(9.5) | 32.5(8.5) |
| Monthly Income (n, %) | |||
| None/other | 64(68%) | 44(70%) | 20(65%) |
| < $1043 | 25(27%) | 17(27%) | 8(26 %) |
| > $1043 | 5(5%) | 2(3%) | 3(9%) |
| Employment (n, %) | |||
| Unemployed/unable to work | 56(60%) | 36(57%) | 20(65%) |
| In school/homemaker | 17(18%) | 13(63%) | 4(13%) |
| Work full or part time | 21(22%) | 14(22%) | 7(23%) |
| Relationship statusa (n, %) | |||
| No relationship in 3 months | 22(23%) | 17(27%) | 5(16%) |
| Dating | 52(55%) | 35(56%) | 17(55%) |
| Live with partner | 19(20%) | 10(16%) | 9(29%) |
| First Incident Only | |||
| Severity of CSA – First Incident (n, %) | |||
| Moderate | 43(46%) | 25(40%) | 17(55%) |
| Severe | 50(53%) | 36(57%) | 14(45%) |
| Disclosure b First Incident (n,%) | |||
| No disclosure | 41(44%) | 29(46%) | 12(39%) |
| Disclosed | 44 (52%) | ||
| High negative response | 23(52%) | 15(52%) | 8(53%) |
| Low negative response | 21(48%) | 14(48%) | 7(47%) |
| PTSD Prevalence | |||
| Above symptom cut of 17 (n,%) | |||
| PTSD only | 11 (12%) | 9 (14%) | 2 (7%) |
| PTSD w/depression | 33 (36%) | 24 (38%) | 9 (30%) |
| Any PTSD | 44 (47%) | 33 (52%) | 11 (37%) |
missing data on 1 respondent;
missing disclosure response data on 9 respondents
The mean age at the first incident was 9.58 years (SD=3.93), was more likely to have occurred prior to or during elementary school (57%) than during adolescence (42%). Chi-square analysis for peri-trauma variables related to disclosure revealed that only age at the time was linked to disclosure, with younger victims more likely to non-disclose than those victimized as teens (38% vs. 25%) (X2(2) =12.47, p=.002).
Frequency distributions and violations of normality resulted in the need to categorize the type of first CSA experience as either severe (digital penetration, attempted rape, rape, oral copulation, and anal sex) or moderate (fondling and frottage). As shown in Table 1, 53% of the sample experienced severe first-incident CSA, with more African Americans reporting severe events than Latinas (57% vs. 45%) (X2(1) = 1.59, NS).
Complete BI data were collected for 67 women and 9 of these (13%) cases were discarded due to a) indication of substance use or behaviors detrimental to accurate interpretation of assays reported on the HBQ; or b) values outside normative ranges on urinary volume and creatinine levels.
A series of Chi square and ANOVAs were run comparing the two ethnic groups on all demographic, predictors, and outcome variables, and no significant differences were noted on any variables. Therefore, and because sample size constraints reduced statistical power and limited reliability, ethnic groups were combined in all subsequent PSS regression model analyses. Due to the small sample of Latinas and previous evidence with a similar biomarker index showing greater health risk among African Americans (Geronimus, Hicken, Keen & Bound, 2006), all BI regression models were run only on the African American (AA) women.
CSA Severity
Raw means are shown in Table 2. An ANOVA for group differences in PSS showed that severe CSA was associated with significantly greater PSS overall than moderate CSA [F(1,90)=5.08, p=.03]. ANOVA analyses of each PSS symptom cluster indicated that exposure to severe (vs. moderate) CSA was associated with greater avoidance/numbing [F(1,90)=9.51, p=.003], as well as a trend for re-experiencing, [F(1,90)=3.60 p=.06], but not for hyperarousal symptoms [F(1,90)=<1]. Victim’s age at the first incident, the duration of the episode, and the relationship to the perpetrator did not modify the relationship between CSA severity and PSS (examined via ANCOVA and as potential main effects in ANOVA).
Table 2.
PTSD Symptoms (PSS) as a function of CSA severity, disclosure and response to disclosure of the first abuse incident
| CSA Severity | DISCLOSURE | ||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Mean (SD) | Severe | Moderate | Negative Response-Low (NRL) | Negative Response-High (NRH) | |
| PTSD Total symptoms | 18.68* (12.43) | 13.42 (9.18) | 15.56 (11.31) | 14.17 (10.42) | 21.16* (12.19) |
| PTSD Symptom Clusters | |||||
| Reexperiencing | 4.65# (4.19) | 3.24 (3.14) | 3.50# (3.64) | 4.35 (3.61) | 5.63 (4.32) |
| Avoidance/Numbing | 8.24*** (5.66) | 5.10 (4.12) | 6.91 (5.30 | 6.06 (5.40) | 8.16 (5.42) |
| Hyperarousal | 5.57 (4.3) | 5.07 (3.95) | 5.21 (4.27) | 4.00 (3.18) | 7.37 (4.57) |
p <.09
p <.05
p<.003
Disclosure, Negative Response, and Self-Blame
Slightly less than half of the women (44%) did not disclose the first CSA incident (non-disclosers). Contrary to expectation, disclosure (yes/no) was unrelated to total PSS or to avoidance/numbing or hyperarousal symptoms, but there was a trend for not disclosing to be associated with lower re-experiencing symptoms relative to disclosing [mean = 3.50 vs. 4.99; F(1,88) = 2.99, p = .09]. See Table 2 for descriptives. The effect of disclosure on PSS was not modified by the victim’s age at the first incident, the duration of the episode, or by the relationship to the perpetrator.
For those who disclosed and reported on the responses via the C-SARS, the mean negative response (NR) was 2.98 (SD=2.09). Violations of normality and skewed frequency distributions necessitated categorization of the variable into two groups. About half of the sample (n=19) reported a C-SARS score of 4 or more and were categorized as Negative Response-High (NRH). The other half (n-18) reported a C-SARS of 3 or less and were categorized as Negative Response-Low (NRL). Among those who disclosed, NR had a significant effect on PSS. As shown in Table 2, a NRH was associated with higher PSS compared to NRL and to non-disclosure cases (mean = 21.16 vs. 14.17 and 15.56; F(2,84) = 2.15, reverse Helmert contrast p=.04]. Self-blame at the time of the first CSA incident was not associated with total PSS or to any symptom clusters (data not shown).
Peri- and Post-Trauma Models
A mixed linear regression analysis with chronic stress and childhood adversity treated as covariates and with CSA severity, self-blame at the time of the incident, and negative response to disclosure entered in invariant order were run to predict level of PSS. These analyses were run for non-disclosers first, then repeated for those who disclosed (examining negative response), and finally for the entire sample. Self-blame at the time of the incident was unrelated to PSS in any model, either as a main effect or as a moderator of CSA severity and thus was dropped.
Final models are shown in Table 3. The model for non-disclosers indicated severe CSA was significantly associated with higher PSS [F(1,42)=6.91, p=.01], and neither chronic stress nor childhood adversity were significant predictors, although there was a trend for childhood adversity [F(1,42)=3.02, p=.09].
Table 3.
Regressions for non-disclosers, disclosers and the total sample predicting PSS from CSA severity, disclosure and negative response after controlling for childhood adversity and chronic stress.
| F-values Predictors in Model | Non Disclosed n=41 | Disclosed+ |
Total Sample n=78 |
||||
|---|---|---|---|---|---|---|---|
| Moderate Severity n=18 | High Severity n=19 | Total PSS | Re-Experiencing | Avoid/Numbing | Hyperarousal | ||
| Adult Stress | 2.20 | 8.03** | 2.38 | 9.99** | 10.80*** | 8.82*** | 2.27 |
| Childhood Adversity | 3.02# | <1 | <1 | 3.70# | 2.58 | 4.50* | 1.16 |
| CSA Severity | 6.91** | - | - | <1 | <1 | 2.62 | <1 |
| Negative Response (High/Low) | - | 5.14* | <1 | ||||
| 3-Level Disclosure No, Yes-NRH, Yes-NRL | - | - | - | 1.75 | 3.06* | <1 | 2.46# |
| Severity X Disclosure | - | - | - | 2.99# | 1.92 | 2.50# | 1.78 |
p<.09
p<.05
p<.01
p<.001
Negative Response missing 16 cases.
The model for all disclosers indicated no significant effect of CSA severity, NR, or severity X NR interaction (not shown). However, when separate regressions for moderate versus severe CSA were conducted, results showed that high NR increased PSS among those with moderate CSA [F(1,17)=5.14, p=.05], but had no effect among those with severe CSA.
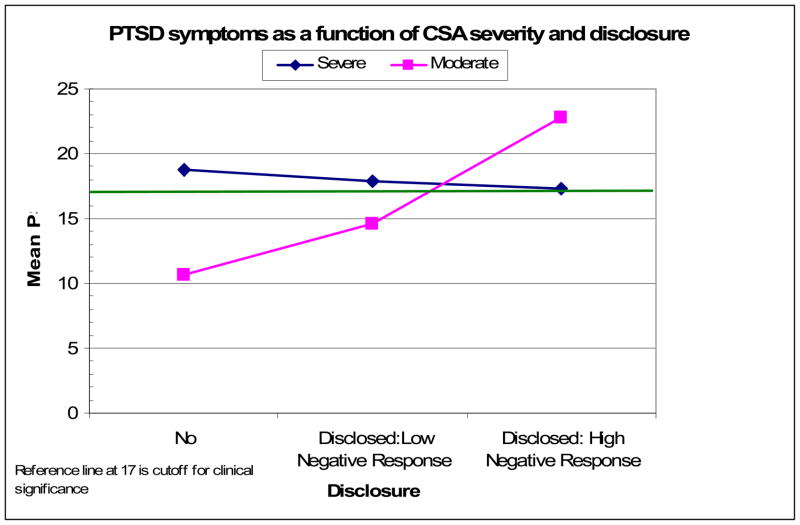
A third model using the entire sample created a new disclosure variable with all 3 groups: Non- Disclosed, Disclosed-NRL, Disclosed-NRH. There was no main effect of severity of CSA or of disclosure on PSS, but a trend for a severity of CSA by disclosure interaction [F(2,75) = 2.99, p=.06]. As illustrated in Figure 2, among non-disclosers, severe CSA was associated with higher PSS than moderate CSA. In contrast, moderate CSA was associated with the highest PSS when a high negative response accompanied disclosure. CSA severity did not significantly impact PSS for those who disclosed and received little or no negative response. This same pattern was evident when this model was repeated to predict avoidance/numbing symptoms. When repeated to predict re-experiencing symptoms, the model showed a main effect of the 3-group disclosure [F(2,74)=3.06, p=.05], as nondisclosers demonstrated lower re-experiencing (M=3.20, SE=.51) than NRL (M=5.06, SE=.87) or NRH (5.19, SE=.80) disclosers. The model predicting hyperarousal symptoms was similar to re-experiencing, (3-group disclosure effect) but showed only a trend (p=.08).
Figure 2.
Posttraumatic stress symptoms as a function of CSA severity, disclosure, and negative response to disclosure after controlling for chronic stress and childhood adversity.
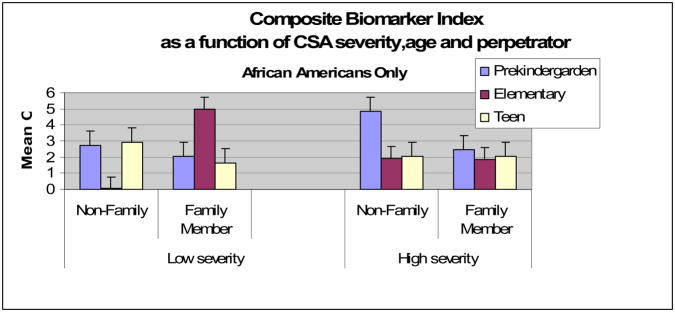
Biomarker Index
Mixed linear regression was used to predict BI health risk among AA women, with chronic burden and childhood adversity as covariates, and CSA severity, age at the first CSA incident, and relationship to the perpetrator (i.e. family member or known non-family member) as predictors.
Results demonstrated no significant main effects, and a significant 2-way age X perpetrator interaction [F(2,21) = 6.91, p=.005] which was superseded by a 3-way CSA severity X age X perpetrator interaction [F(4,21) = 3.44, p = .03]. As shown in Fig. 3, abuse by a family member during elementary school was associated with the highest BI in AA women exposed to low severity CSA. However, high severity CSA was associated with the highest BI among AA women abused by a non-family member during pre-kindergarten years. Notably, these effects were observed even after controlling for current chronic stress burden and early childhood adversity.
Figure 3.
Three-way interaction of age at the first incident X perpetrator and X CSA severity predicting biomarker risk index in African American women.
Post-trauma variables of disclosure (yes/no and negative response) and self-blame, current age, current perceived stress, and childhood adversity were not significantly related to BI. Thus, it appears that the BI is associated with peri-trauma (severity, age at the time and perpetrator), but not with post-trauma variables in this sample.
Discussion
To our knowledge, this is the first study to simultaneously investigate hypothetical mechanisms linking CSA to adult PSS and a BI in a community sample of disadvantaged urban ethnic minority women. We found partial support for our conceptual model of two distinct pathways from CSA to negative outcomes. As shown by the outward arrows in Figure 1, the first pathway from peri-trauma variables to negative outcomes was driven by CSA severity, was not mediated by post-trauma variables, predicted avoidance/numbing symptoms, and was associated with greater biomarker risk. The second pathway involved moderate CSA only, was mediated by post-trauma disclosure experiences, predicted re-experiencing symptoms, and was not associated with BI risk.
Specifically, severe CSA was associated with greater PSS relative to moderate CSA, after controlling for chronic stress and childhood adversity. Importantly, this relationship was not mediated by whether the incident was disclosed, a negative response if disclosed, or self-blame. Examination of separate PSS clusters indicated that the relationship between severe CSA and increased PSS was particularly strong with avoidance/numbing.
Disclosure experiences mediated the relationship of CSA and PSS only in women who experienced moderate severe CSA. Among women with moderate CSA, PSS symptoms were lowest in non-disclosers, higher in disclosers who experienced a low negative response, and highest for disclosers who experienced a highly negative response. Counter-intuitively, a high negative response to disclosure after moderately severe CSA was associated with greater PSS than among women with severe CSA who disclosed and received high negative responses. Other peri-trauma variables (age at the time, duration of the incident and perpetrator) were not directly linked to PSS and were not related to post-trauma disclosure or self-blame.
A greater BI among AA women was predicted by interactions between CSA severity, age at the time, and the perpetrator characteristics. For moderately severe CSA, incidents perpetrated by a family member when the victim was of elementary school age showed nearly double the BI as other low severity categories. For high severity CSA, the BI was nearly doubled for pre-kindergarten survivors victimized by a familiar, but non-family member perpetrator. The significance of a BI score above 4 among these women who average 35 years of age is illustrated by reference to population means on a similar BI obtained via a national survey (Geronimous, Hicken, Keene & Bound, 2006). White and black women aged 35–44 had mean BI’s of 2.36 and 3.00, respectively and rose to mean BI’s of 4.29 and 4.99 at the 55–64 age groups. Thus, some CSA survivors in this sample are showing BI levels similar to women 20 years older.
We replicated previous work and showed that severe CSA was associated with significantly greater PSS overall, after controlling for childhood adverse experiences other than CSA and adult chronic stress. The latter is a strength of our study, contributing to the literature by showing that the effect of CSA severity on PSS was not modified by the victim’s age at the time of the first CSA incident, the duration of the incident, or by the relationship to the perpetrator. This could mean that there is a ceiling effect of penetrative CSA on PSS, and that additional abuse characteristics that predict adult distress (i.e., younger age, longer duration, closeness to the perpetrator) are not associated with more severe symptoms.
We also found that the relationship between CSA severity and adult PSS was mostly accounted for by the effect of CSA severity on the avoidance/numbing symptom cluster. This is consistent with previous findings that a general tendency to avoid or escape from unpleasant internal experiences may be a specific factor that exacerbates psychological distress among women with a history of childhood (Rosenthal, Rassmussen, Palm, et al, 2005) or adolescent sexual victimization (Polusny et al, 2004). In addition, cumulative adverse childhood experiences (including multiple types of abuse) are associated with increased reliance on avoidant coping strategies (Leitenberg, Gibdon & Novy, 2004).
On the other hand, disclosure effects among those who experienced moderate CSA incidents were evident for re-experiencing symptoms and not for avoidance/numbing symptom clusters. In other words, variables that preceded or coincided with the abuse (e.g., penetration) are more likely associated with the PSS cluster of avoidance/numbing, whereas post-trauma variables (e.g., negative reactions to abuse disclosure) are more likely to impact the re-experiencing and possibly the hyperarousal cluster. Since re-experiencing, avoidance and dissociation seem to engage distinct neural circuits (Hopper, Frewen, van der Kolk & Lanius, 2007), we speculate that these circuits are preferentially activated in sequence, some during the abuse and others in its aftermath, to result in the pattern of associations we found.
A large proportion (44%) of the women in our sample did not disclose their first CSA incident, which is consistent with previous studies (Goodman-Brown et al, 2003; Smith et al, 2000; Wyatt et al, 1999). Like others, we also found that the majority of those who disclose their abuse in childhood received negative reactions (Filipas & Ullman, 2001; Jonzon & Linblad, 2004). While some studies found that women who disclosed their abuse reported fewer PTSD symptoms in adulthood (Arata, 1998), others have found that negative reactions to disclosure are associated with greater PTSD symptoms (Ullman, 2007). Our results partially confirmed Ullman’s findings, where more negative reactions to CSA disclosure were associated with increased PSS, but only for women who experienced moderate CSA. For women with severe CSA, negative responses to disclosure had no significant effect on PSS in this sample.
To our knowledge, this is the first use of a BI as an outcome of exposure to CSA among adult minority women. The evidence that peri-trauma factors of age, perpetrator and CSA severity interact to affect biomarker risk with no evidence of an effect of post-trauma factors supports the conceptualization of CSA as a traumatic event with long-lasting biological dysregulation effects into adulthood. The post-trauma of responses to disclosure and self-blame may be more likely to operate on depression and other psychological symptoms which develop over time, but not to PSS in this sample. Our results also support the models of Saxe and Kaplow (Kaplow et al, 2005; Saxe et al, 2005), which suggest different predictors for avoidance/numbing symptoms versus anxiety/hyperarousal symptoms. Future exploration of individual biomarkers in relation to symptom clusters may be helpful in elucidating the biobehavioral mechanisms of hypothesized phenotypes.
Our results support the relevance of further research on the factors that individuals take into account when they are faced with the decision of whether or not to disclose CSA. The finding that not disclosing moderate CSA was associated with the least psychological distress runs somewhat counter to clinical judgments about the value of disclosure. It highlights the need to understand when disclosing may be disadvantageous to the victim. The factors that women (or girls) must weigh when considering whether or not to disclose and their perceptions of the reactions they will receive have not been adequately examined. Likely, the appraisal process involved will be dissimilar for children and adults. Further research is also needed to examine other abuse characteristics (i.e., the relationship of the perpetrator to the victim, the duration of the incident) that may influence the likelihood of a subsequent disclosure.
Even less is known about women whose abuse is disclosed for them; that is, the disclosure is out of their personal control (i.e., it is witnessed or interrupted by someone). Results of this study suggest that important targets for future interventions with CSA survivors may be to teach CSA victims how to disclose appropriately to receive support (Whiffen & Macintosh, 2005). In addition, although no main effects were found for CSA severity or negative response to disclosure, their marginally significant interaction suggests the importance of testing for interactions in future studies.
The results of this study must be interpreted in light of several limitations. First, the small sample size limited power and only allowed us to examine a dichotomous definition of CSA severity and the first incident. This means that we could not examine the effect of increasingly severe CSA, or the cumulative effects of multiple incidents. We were also underpowered to test for differences between the two ethnic groups and we were only able to examine the relationship between CSA and the BI among AA women. Second, because there was no comparison group of women without CSA histories, we cannot distinguish the impact of CSA on later mental health independent of other risk factors (e.g. low SES, exposure to discrimination, other traumas, etc.). Relatedly, most of the sample did not select CSA as their “worst” traumatic experience on the PSS instrument and of the 21.7% who did, some may not have been referring to the first CSA incident, which was the focus of our analyses here. Future studies should compare CSA-specific PSS and PSS related to other traumas to examine the relative contributions of each on PSS in adult CSA survivors. Finally, assessment of self-blame was limited here and could have contributed to the absence of self-blame effects.
Despite these limitations, this is one of the first studies to address these questions in a sample of socio-economically disadvantaged, ethnic minority women. Because sample size constraints limited our ability to test for between group differences, these questions will need to be investigated with larger, more ethnically and socioeconomically diverse samples. It will also be important to recognize the diversity within each of these ethnic groups and to include samples that are large enough to permit within-group analyses as well.
Acknowledgments
This study was supported in part by National Institute of Mental Health grant No. T32 MH17140.
Footnotes
Complete Address of Co-Authors
Jennifer Vargas Carmona, Ph.D., Associate Research Psychologist, Dept of Psychiatry and Biobehavioral Sciences, UCLA Semel Institute, 760 Westwood Plaza C9 432, Los Angeles, CA 90024-1759
Tamra Burns Loeb, Ph.D., Associate Research Psychologist, Dept of Psychiatry and Biobehavioral Sciences, UCLA Semel Institute, 760 Westwood Plaza C9 432, Los Angeles, CA 90024-1759
Andres Sciolla, M.D., Assistant Clinical Professor, Associate Residency Training Director, University of California, San Diego, 9500 Gilman Drive # 9116-A, La Jolla, CA 92093-9116-A
Hector F. Myers, Ph.D., Professor and Director of Clinical Training, Department of Psychology, UCLA, 1285 Franz Hall, Box 91563, Los Angeles, CA 90095-1563, myers@psych.ucla.edu
Gail E. Wyatt, Ph.D., Professor, Dept. of Psychiatry & Biobehavioral Sciences, UCLA Semel Institute for Neuroscience and Human Behavior, 760 Westwood Plaza C9 432, Los Angeles, CA 90024-1759, gwyatt@mednet.ucla.edu
Muyu Zhang, M.S.1, Dept of Psychiatry and Biobehavioral Sciences, UCLA Semel Institute, 760 Westwood Plaza C9 432, Los Angeles, CA 90024-1759
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Arata CM. To tell or not to tell: Current functioning of child sexual abuse survivors who disclosed their victimization. Child Maltreatment. 1998;3(1):63–71. [Google Scholar]
- Bremner JD, Wythilingam M, Vermetten E, Southwick SM, McGlashan T, Nazeer A, Khan S, Vaccarino LV, Soufer R, Garg PK, Ng CK, Staib LH, Duncan JS, Charney DS. MRI and PET study of deficits in hippocampal structure and function in women with childhood sexual abuse and posttraumatic stress disorder. American Journal of Psychiatry. 2003;160(5):924–932. doi: 10.1176/appi.ajp.160.5.924. [DOI] [PubMed] [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. Mediators of the long-term impact of child sexual abuse: Perceived stigma, betrayal, powerlessness, and self-blame. Child Abuse and Neglect. 1996;20(5):447–455. doi: 10.1016/0145-2134(96)00019-1. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. Current information on the scope and nature of child sexual abuse. Future of Children. 1994;4(2):31–53. [PubMed] [Google Scholar]
- Foa EB. Trauma and women: Course, predictors, and treatment. Journal of Clinical Psychiatry. 1997;58(Suppl 9):25–28. [PubMed] [Google Scholar]
- Friedman MJ, Jalowiec J, McHugo G, Wang S, McDonagh A. Adult sexual abuse is associated with elevated neurohormone levels among women with PTSD due to childhood sexual abuse. Journal of Traumatic Stress. 2007;20(4):611–7. doi: 10.1002/jts.20221. [DOI] [PubMed] [Google Scholar]
- Filipas HH, Ullman SE. Social reactions to sexual assault victims from various support sources. Violence and Victims. 2001;16(6):673–92. [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–33. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover DA. The Health Behaviors Questionnaire. Unpublished instrument 2002 [Google Scholar]
- Glover DA, Poland RE. Urinary cortisol and catecholamines in mothers of child cancer survivors with and without PTSD. Psychoneuroendocrinology. 2002;27(7):805–819. doi: 10.1016/s0306-4530(01)00081-6. [DOI] [PubMed] [Google Scholar]
- Glover DA, Stuber M, Poland RE. Allostatic load in PTSD-symptomatic middle-aged mothers of child cancer survivors. Psychiatry: Interpersonal and Biological Processes. 2006;69(3):191–203. doi: 10.1521/psyc.2006.69.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman-Brown TB, Edelstein RS, Goodman GS, Jones DP, Gordon DS. Why children tell: A model of children’s disclosure of sexual abuse. Child Abuse and Neglect. 2003;27(5):525–540. doi: 10.1016/s0145-2134(03)00037-1. [DOI] [PubMed] [Google Scholar]
- Gurung RAR, Taylor SE, Kemeny M, Myers H. “HIV Is Not My Biggest Problem”: The impact of HIV and chronic burden on depression in women at risk for AIDS. Journal of Social & Clinical Psychology. 2004;23(4):490–511. [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. Journal of the American Medical Association. 2000;284(5):592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Bonsall R, Miller AH, Nemeroff CB. Altered pituitary-axis responses to provocative challenge tests in adult survivors of childhood abuse. American Journal of Psychiatry. 2001;158(4):575–581. doi: 10.1176/appi.ajp.158.4.575. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Frewen PA, van der Kolk BA, Lanius RA. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. Journal of Traumatic Stress. 2007;20(5):713–25. doi: 10.1002/jts.20284. [DOI] [PubMed] [Google Scholar]
- Hunter JA, Goodwin DW, Wilson RJ. Attributions of blame in child sexual abuse victims: An analysis of age and gender influences. Journal of Child Sexual Abuse. 1992;1(3):75–89. [Google Scholar]
- Johnson DM, Pike JL, Chard KM. Factors predicting PTSD, depression, and dissociative severity in female treatment-seeking childhood sexual abuse survivors. Child Abuse & Neglect. 2001;25(1):179–198. doi: 10.1016/s0145-2134(00)00225-8. [DOI] [PubMed] [Google Scholar]
- Jonzon E, Linblad F. Disclosure, reactions, and social support: Findings from a sample of adult victims of child sexual abuse. Child Maltreatment. 2004;9(2):190–200. doi: 10.1177/1077559504264263. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Dodge KA, Amaya-Jackson L, Saxe GN. Pathways to PTSD, part II: Sexually abused children. American Journal of Psychiatry. 2005;162(7):1305–10. doi: 10.1176/appi.ajp.162.7.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGee WJ. Childhood adversities and adult depression: Basic patterns of association in a US national survey. Psychological Medicine. 1993;23(3):107–115. doi: 10.1017/s0033291700025460. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2 Suppl):S101–8. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitenberg H, Gibson LE, Novy PL. Individual differences among undergraduate women in methods of coping with stressful events: the impact of cumulative childhood stressors and abuse. Child Abuse & Neglect. 2004;28(2):181–92. doi: 10.1016/j.chiabu.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: Evidence for chronic neuroendocrine activation in women. Psychosomatic Medicine. 1995;57(2):105–115. doi: 10.1097/00006842-199503000-00002. [DOI] [PubMed] [Google Scholar]
- Loeb TB, Williams JK, Carmona JV, Rivkin I, Wyatt GE, Chin D, Asuan-O’Brien A. Child sexual abuse: associations with the sexual functioning of adolescents and adults. Annual Review of Sex Research. 2002;13:307–345. [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews of Neuroscience. 2009;10(6):434–45. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Marx BP. Lessons learned from the last twenty years of sexual violence research. Journal of Interpersonal Violence. 2005;20(2):225–230. doi: 10.1177/0886260504267742. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostatis & allostatic load. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic Status & Health in Industrial Nations: Social, Psychological and Biological Pathways. Annals of New York Academy of Science; 896. New York, New York: 1999. pp. 30–47. [DOI] [PubMed] [Google Scholar]
- Mennen FE. The relationship of race/ethnicity to symptoms in childhood sexual abuse. Child Abuse & Neglect. 1995;19(1):115–124. doi: 10.1016/0145-2134(94)00100-9. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, Gross M, Sheon A, Miller H, Cooley P, Seage GR., III Randomized controlled trial of audio computer-assisted self-interviewing: Utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. American Journal of Epidemiology. 2000;152(2):99–106. doi: 10.1093/aje/152.2.99. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health 2001. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny MA, Rosenthal MZ, Aban I, Follette VM. Experiential avoidance as a mediator of the effects of adolescent sexual victimization on negative adult outcomes. Violence & Victims. 2004;19(1):109–20. doi: 10.1891/vivi.19.1.109.33238. [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Rasmussen-Hall ML, Palm KM, Batten SV, Follette V. Chronic avoidance helps explain the relationship between severity of childhood sexual abuse and psychological distress in adulthood. Journal of Child Sexual Abuse. 2005;14(4):25–41. doi: 10.1300/J070v14n04_02. [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Cromer K, Hernandez A, Kendall-Tackett K. A review of childhood abuse, health, and pain-related problems: The role of psychiatric disorders and current life stress. Journal of Trauma & Dissociation. 2009;10(2):170–88. doi: 10.1080/15299730802624585. [DOI] [PubMed] [Google Scholar]
- Saxe GN, Stoddard F, Hall E, Chawla N, Lopez C, Sheridan R, King D, King L, Yehuda R. Pathways to PTSD, Part I: Children with burns. American Journal of Psychiatry. 2005;162(7):1299–304. doi: 10.1176/appi.ajp.162.7.1299. [DOI] [PubMed] [Google Scholar]
- Siegel JM, Sorenson SB, Golding JM, Burman MA, Stein JA. The prevalence of childhood sexual assault: The Los Angeles Epidemiologic Catchment Area Project. American Journal of Epidemiology. 1987;126(6):1141–1164. doi: 10.1093/oxfordjournals.aje.a114752. [DOI] [PubMed] [Google Scholar]
- Smith DW, Letourneau EJ, Saunders BE, Kilpatrick DG, Resnick HS, Best CL. Delay in disclosure of childhood rape: Results from a national survey. Child Abuse & Neglect. 2000;24(2):273–287. doi: 10.1016/s0145-2134(99)00130-1. [DOI] [PubMed] [Google Scholar]
- Spaccarelli S. Stress, appraisal, and coping in child sexual abuse: A theoretical and empirical review. Psychological Bulletin. 1994;116(2):340–362. doi: 10.1037/0033-2909.116.2.340. [DOI] [PubMed] [Google Scholar]
- Spaccarelli S. Measuring abuse stress and negative cognitive appraisals in child sexual abuse: Validity data on two new scales. Journal of Abnormal Child Psychology. 1995;23(6):703–727. doi: 10.1007/BF01447473. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Tomoda A, Andersen SL. Neurobiological consequences of early stress and childhood maltreatment: Are results from human and animal studies comparable? In: Yehuda R, editor. Psychobiology of Posttraumatic Stress Disorder: A Decade of Progress. Annals of the New York Academy of Sciences; NewYork, NY: 2006. pp. 313–323.pp. 1071 [DOI] [PubMed] [Google Scholar]
- Ullman SE. Relationship to perpetrator, disclosure, social reactions, and PTSD symptoms in child sexual abuse survivors. Journal of Child Sexual Abuse. 2007;16(1):19–36. doi: 10.1300/J070v16n01_02. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH. Ethnicity and child sexual abuse experiences of female college students. Journal of Child Sexual Abuse. 2005;14(3):67–89. doi: 10.1300/J070v14n03_04. [DOI] [PubMed] [Google Scholar]
- Whiffen VE, Macintosh HB. Mediators of the link between childhood sexual abuse and emotional distress: A critical review. Trauma, Violence & Abuse. 2005;6(1):24–39. doi: 10.1177/1524838004272543. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sexual abuse of Afro-American and White-American women in childhood. Child Abuse & Neglect. 1985;9(4):507–519. doi: 10.1016/0145-2134(85)90060-2. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Lawrence J, Vodounon A, Mickey MR. The Wyatt Sex History Questionnaire: A structured interview for female sexual history taking. Journal of Child Sexual Abuse. 1992;1(4):51–68. [Google Scholar]
- Wyatt GE, Loeb TB, Solis B, Carmona JV, Romero G. The prevalence and circumstances of child sexual abuse: Changes across a decade. Child Abuse & Neglect. 1999;23(1):45–60. doi: 10.1016/s0145-2134(98)00110-0. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Carmona JV, Loeb TB, Ayala A, Chin D. Sexual abuse. In: Wingood GM, DiClemente RJ, editors. Handbook of women’s sexual and reproductive health. Issues in women’s health. New York, NY: Kluwer Academic/Plenum Publishers; 2002. pp. 195–216. [Google Scholar]