Abstract
BACKGROUND & AIMS
Donor race has been proposed to predict graft failure after liver transplantation. We evaluated the extent to which the center where the transplantation surgery was performed and other potential confounding factors might account for the observed association between donor race and graft failure.
METHODS
We analyzed data from the Organ Procurement and Transplantation Network (January 2003–December 2005) for adult patients undergoing primary liver transplantation in the United States. We examined the association between graft failure and the donor races of African American (AA), Caucasian, Asian/Pacific Islander (API), or those classified as other.
RESULTS
Of 10,874 livers that were donated for transplantation, 7631 came from Caucasians, 1579 from AAs, 243 from APIs, and 1421 from others. After 36 months of follow-up evaluation, 2687 grafts failed. Without any adjustments, AA donors (hazard ratio [HR], 1.11; 95% confidence interval [CI], 1.00–1.24), API donors (HR, 1.41; 95% CI, 1.12–1.77), and other donors (HR, 1.16; 95% CI, 1.04–1.29) were associated with graft failure. After stratification by center and adjustments for age, height, and hepatitis B core antibody status of donors as well as serum creatinine and hepatitis C status of recipients, donor race was no longer statistically significant for AA (HR, 1.06; 95% CI, 0.95–1.20) and API (HR, 1.15; 95% CI, 0.89–1.49) donors. However, livers donated from members of other race still had an increased risk of graft failure (HR, 1.19; 95% CI, 1.05–1.35), although the effect was not uniform across donor–recipient pairs.
CONCLUSIONS
Donor race is not a uniform predictor of graft failure and should not be construed as an indicator of donor quality.
Keywords: African American, Donor Factors, Organ Allocation, Donor Risk Index
Donor race has been proposed as a predictor of graft failure after liver transplantation (LTx).1,2 For example, according to a report from the Scientific Registry of Transplant Recipients based on data from 1998 to 2002, receipt of an African American (AA) donor organ or a non Caucasian non-AA donor organ was associated significantly with a 19% and 13% increase in the risk of graft failure, respectively.1 Based on these data, a scoring system known as the Donor Risk Index (DRI) has been proposed to include donor race as an indicator of the quality of a donor organ. If donor race is truly predictive of graft failure, it may need to be incorporated in organ allocation decisions.3
However, the biological plausibility of donor race uniformly being a contributor to poor outcomes is questionable. Although it is possible that immunologic differences or other genetically determined incompatibility between the donor and the recipient of discordant races may lead to worse survival, evidence is lacking to support such a hypothesis.4,5 Further, it is common for racial disparity in health outcome to turn out to be attributable to other socioeconomic factors for which race is merely a surrogate indicator.6,7 The real danger of misusing race as an indicator of poor donor quality is that minority donors will be thought of automatically as marginal donors and may be directed preferentially to marginal recipients, creating a self-fulfilling prophecy that may be very difficult to disprove with future analyses.
We hypothesized that a large part of the association between donor race and graft failure is explained by differences in transplantation centers and other unadjusted confounders. We also looked for evidence of an interaction between donor and recipient race as an indicator of possible biological mismatch between racially discordant donor and recipient pairs. Our present analysis of the Organ Procurement and Transplantation Network data under the current allocation system based on the Model for End-Stage Liver Disease (MELD) score shows that the association between donor race and graft failure is attenuated substantially by taking into account a small number of previously unadjusted confounders.
Materials and Methods
Database
We used data from the Organ Procurement and Transplantation Network of all adult (age, ≥18 y) LTx recipients from January 1, 2003, to December 31, 2005. In the primary analysis, we excluded status 1 recipients (n = 1143) and recipients diagnosed with hepatocellular carcinoma (n = 1666) to create a uniform cohort of patients undergoing transplantation for chronic liver disease. We then conducted a sensitivity analysis adding status 1 and HCC patients back to address the whole LTx population. The primary variable of interest was physician-reported donor race: Caucasian, AA, Asian Pacific Islander (API), or other.
Covariates
We considered covariates that may confound the association between donor race and graft survival, including the following: (1) donor-related factors: age, sex, height, weight, cause of death (anoxia, cerebrovascular accident, head trauma, or other), graft size mismatch (difference in height between recipient and donor), hepatitis B core antibody status (transplantation into a recipient without hepatitis B virus infection),8 and donation after cardiac death; (2) transplant-related factors: partial/split liver transplantation, cold ischemia time, regional or national share, and ABO incompatibility; and (3) recipient-related factors: age, sex, MELD score and serum creatinine level at transplantation, diagnosis (hepatitis C virus [HCV] infection vs other), and type of health insurance.
Statistical Analysis
We compared baseline donor, transplant, and recipient characteristics by donor race (Caucasian, AA, API, or other). We conducted between-group comparisons using the Kruskal–Wallis test for continuous variables and the chi-square test for categoric data. The primary outcome was graft failure, which was defined as patient death or re-transplantation within 3 years. Patients who were alive with a functioning graft at 3 years after LTx were censored.
First, we used the Kaplan–Meier method to estimate graft survival based on donor race. Second, we examined the association between donor race and graft failure in univariate analysis and then multivariable analyses after adjustment for donor-, recipient-, and transplant-related characteristics as listed earlier using the Cox proportional hazards regression analysis. The primary confounder of interest, namely LTx center, was handled by stratifying the analysis for each center, which enables detection of differences in patient populations and outcomes between transplant centers.9 Stratification allows assignment of a baseline hazard unique to each center and compares the risk of graft failure of one donor race compared with another within a center. Third, we examined the interaction between donor and recipient race. For this analysis, we compared graft survival in separate strata of donor and recipient pairs, using concordant donor and recipient race pairs as reference, while stratifying for center. If a certain donor race truly is associated with graft failure, one would expect a uniform increase in the risk of graft failure regardless of the recipient race. Finally, we examined the impact of donor race in the context of variables included in the DRI. This analysis also was undertaken with stratification by center.1
Results
Donor and Recipient Characteristics at Transplantation
There were 10874 transplants that met the inclusion criteria for the study. Information about donor race was missing in 11 recipients, and these transplants were excluded from the analyses. A majority of the donors were Caucasian (n = 7631; 70.2%), followed by AA (n = 1579; 14.5%), and API (n = 243; 2.2%). The remainder (n = 1421; 13.1%) were categorized as other. Of those classified as other, 92% were indicated to be of Hispanic ethnicity.
Table 1 describes donor, recipient, and transplant characteristics by donor race. The mean (±standard deviation) age of donors was 41.9 ± 17.7 years. API donors were oldest (mean age, 45.2 ± 17.6 y), whereas donors of other race were the youngest (mean age, 37.4 ± 16.9 y). In total, a slight majority of the donors were male (58%). The proportion of female donors was the highest among API donors (49%) and lowest in other donors (33%). Death from cerebrovascular accident was most common among API donors (59%), followed by AA donors (54%). Anti– hepatitis B core (anti-HBc) positivity was by far the most common in API donors (29%). Anti–HBc-positive organs (n = 580) were transplanted primarily into non–hepatitis B recipients (91%). Overall, API donors were shortest in stature. Mismatch in height between recipient and donor was the greatest with API donors (5.7 ± 13.7 cm), followed by other (2.8 ± 13.3 cm).
Table 1.
Baseline Characteristics of LTx From January 1, 2003, to December 31, 2005, by Donor Race
| Donor race |
|||||
|---|---|---|---|---|---|
| Caucasian N = 7631 |
AA N = 1579 |
API N = 243 |
Other N = 1421 |
P | |
| Donor | |||||
| Mean age, y (SD) | 42.9 (17.8) | 40.8 (17.0) | 45.2 (17.6) | 37.4 (16.9) | <.01 |
| Female | 3295 (43.2%) | 659 (41.7%) | 119 (49.0%) | 465 (32.7%) | <.01 |
| Cause of death (reference, head trauma) | |||||
| Anoxia | 984 (12.9%) | 165 (10.5%) | 30 (12.3%) | 151 (10.6%) | .01 |
| Cerebrovascular accident | 3391 (44.4%) | 855 (54.2%) | 144 (59.3%) | 581 (40.9%) | <.01 |
| HBc positive | 246 (3.2%) | 185 (11.8%) | 70 (28.8%) | 79 (5.6%) | <.01 |
| Mean height, cm (SD) | 172.4 (10.6) | 172.1 (11.5) | 164.0 (10.3) | 168.2 (10.4) | <.01 |
| Mean difference in recipient–donor height, cm (SD) | 0.2 (13.2) | 0.4 (13.9) | 5.7 (13.7) | 2.8 (13.3) | <.01 |
| Recipient | |||||
| Mean age, y (SD) | 52.6 (9.5) | 52.4 (9.5) | 53.3 (10.0) | 52.3 (9.8) | .24 |
| Diagnosis | |||||
| Hepatitis C | 3387 (44.4) | 710 (45.0%) | 119 (49.0%) | 674 (47.4%) | .11 |
| Hepatitis B | 239 (3.1%) | 66 (4.2%) | 21 (8.6%) | 53 (3.7%) | <.01 |
| Alcoholic liver disease | 1227 (16.1) | 255 (16.1%) | 32 (13.2%) | 250 (17.6%) | .29 |
| MELD score at transplant (SD) | 20.6 (8.6) | 20.2 (8.5) | 20.3 (9.3) | 22.3 (9.5) | <.01 |
| Public insurance | 1776 (23.3%) | 358 (22.7%) | 55 (22.6%) | 293 (20.6%) | .18 |
| Median creatinine level, mg/dL (IQR) | 1.1 (0.8–1.6) | 1.0 (0.8–1.5) | 1.1 (0.8–1.6) | 1.1 (0.8–1.7) | .02 |
| Transplant | |||||
| Donation after cardiac death | 346 (4.5%) | 34 (2.2%) | 5 (2.1%) | 26 (1.8%) | <.01 |
| Partial/split liver | 123 (1.6%) | 21 (1.3%) | 5 (2.1%) | 40 (2.8%) | <.01 |
| Mean cold ischemia time, h (SD) | 7.8 (3.6) | 7.6 (3.9) | 7.7 (3.5) | 7.5 (3.4) | <.01 |
| Regional share | 1643 (21.5%) | 300 (19.0%) | 46 (18.9%) | 308 (21.7%) | .12 |
| National share | 532 (7.0%) | 140 (8.9%) | 18 (7.4%) | 34 (2.4%) | <.01 |
SD, standard deviation; IQR, interquartile range.
Although statistical significance was achieved because of the large number of recipients, there were few noticeable differences in recipient and transplant characteristics according to the donor race. The mean MELD score of recipients of donors of other race (22.3 ± 9.5) was higher as compared with those of Caucasian (20.6 ± 8.6), AA (20.2 ± 8.5), and API (20.3 ± 9.3) donors. As expected from the frequency of anti-HBc positivity, the proportion of hepatitis B–related liver disease was higher among recipients of Asian donors (8.6%, compared with 3.1%, 4.2%, and 3.7% for Caucasian, AA, and other donors, respectively). Donation after cardiac death was more common among Caucasian donors (4.5%), whereas partial/split transplantation was most common and national share least common among other donors.
Transplant Outcome by Donor Race and Center Effect
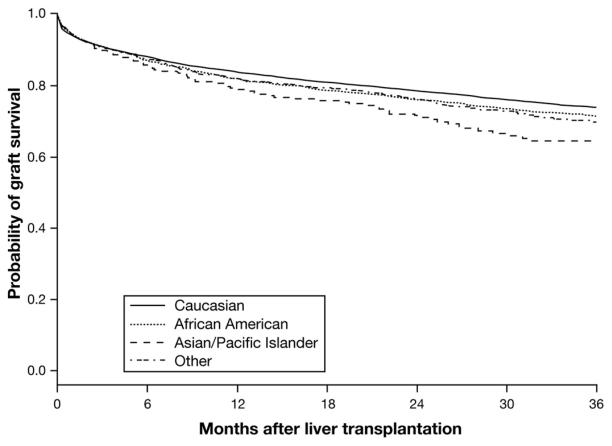
After transplantation, the median follow-up period was 35 months. Figure 1 shows the Kaplan–Meier estimates for graft survival by donor race without any adjustment. There were a total of 2687 graft failures including 2253 patient deaths after 3 years of follow-up evaluation. The 3-year graft survival rate was 74%, 72%, 70%, and 65% for Caucasians, AA, other, and API donors, respectively (P < .01).
Figure 1.
Probability of graft survival by donor race (unadjusted).
Table 2 illustrates the effect of transplant center on graft survival. Without stratification on center, AA donor race was associated with an 11% increased risk (hazard ratio [HR], 1.11; 95% confidence interval [CI], 1.00–1.24) of graft failure. Risk of failure for API and other grafts also was higher than Caucasian counterparts with an HR of 1.41 (95% CI, 1.12–1.77) for API and 1.16 (95% CI, 1.04–1.29) for other. Once the analysis was stratified on center, the HR associated with AA donor decreased to 5% and was no longer significant (HR, 1.05; 95% CI, 0.94–1.17). The effect of API decreased but remained significant with an HR of 1.35 (95% CI, 1.07–1.71), whereas that of other race remained unchanged with an HR of 1.18 (95% CI, 1.05–1.33).
Table 2.
Association of Donor Race and Graft Failure Before and After Stratification by Transplant Center Using Cox Proportional Hazards Regression
| No stratification |
Stratification by transplant center |
|||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Donor race | ||||
| AA | 1.11 | 1.00–1.24 | 1.05 | 0.94–1.17 |
| API | 1.41 | 1.12–1.77 | 1.35 | 1.07–1.71 |
| Other | 1.16 | 1.04–1.29 | 1.18 | 1.05–1.33 |
| Caucasian | 1.0 | Reference | 1.0 | Reference |
Consideration of Other Covariates
Table 3 reports the results of univariate analyses of donor-, recipient-, and transplant-related factors as predictors of graft failure after stratification on center. The analysis presented in Table 4 incorporates potentially important predictors of graft failure observed in the univariate analyses in addition to stratification by center. These covariates include recipient factors (age, serum creatinine level, HCV diagnosis) and donor factors other than race (age, donor height, and transplantation of anti–HBc-positive organs into hepatitis B–negative recipient). After adjusting for these factors, AA donor was associated with a nonsignificant 6% increased risk of graft failure (HR, 1.06; 95% CI, 0.95–1.20). The effect of API donor decreased to a nonsignificant 15% increase of graft failure (HR, 1.15; 95% CI, 0.89–1.49). The effect of other race remained unchanged and significant (HR, 1.19; 95% CI, 1.05–1.35). Addition of donor weight, ABO incompatibility, difference in height between donor and recipient, recipient MELD score at transplantation, recipient race, and type of insurance did not alter the observed associations in multivariable analysis. We also examined graft failure after inclusion of all status 1 recipients and recipients transplanted for hepatocellular carcinoma. After adjusting for the factors mentioned earlier, AA donor was associated with a nonsignificant 5% increased risk of graft failure (HR, 1.05; 95% CI, 0.95–1.17), API donor was associated with a nonsignificant 6% increased risk of graft failure (HR, 1.06; 95% CI, 0.84–1.33), and other race was associated with a significant 17% increased risk of graft failure (HR, 1.17; 95% CI, 1.05–1.31).
Table 3.
Univariate Analyses of Predictors of Graft Survival After Stratification by Center
| HR (95% CI) | P | |
|---|---|---|
| Donor | ||
| Age, decade | 1.13 (1.10–1.15) | <.01 |
| Female | 1.12 (1.04–1.22) | <.01 |
| Height, 10 cm | 0.91 (0.88–0.94) | <.01 |
| Weight, 5 kg | 0.99 (0.98–1.00) | .06 |
| Cause of death (reference, head trauma) | ||
| Anoxia | 1.18 (1.04–1.34) | .01 |
| Cerebrovascular accident | 1.39 (1.28–1.52) | <.01 |
| Other | 1.06 (0.83–1.36) | .64 |
| Height difference (recipient–donor) | 1.05 (1.02–1.08) | <.01 |
| HBcAb (+) donor/HBV (−) recipient | 1.17 (1.00–1.38) | .05 |
| Recipient | ||
| Age, decade | 1.09 (1.05–1.14) | <.01 |
| Female | 1.02 (0.93–1.10) | .70 |
| MELD at transplantation, 5 points | 1.06 (1.03–1.08) | <.01 |
| Indication for transplantation, HCV | 1.26 (1.17–1.36) | <.01 |
| Ln creatinine | 1.25 (1.16–1.34) | <.01 |
| Insurance (reference, private) | ||
| Medicaid | 1.10 (0.98–1.23) | .11 |
| Public | 1.23 (1.12–1.35) | <.01 |
| Other | 0.88 (0.56–1.39) | .59 |
| Transplant | ||
| Donation after cardiac death | 1.51 (1.27–1.80) | <.01 |
| Partial/split liver | 1.06 (0.80–1.42) | .67 |
| Cold ischemia time | 1.01 (1.00–1.02) | .09 |
| Regional share | 1.15 (1.04–1.28) | <.01 |
| National share | 1.11 (0.94–1.31) | .21 |
| ABO incompatibility | 1.44 (0.81–2.56) | .22 |
HBcAb, hepatitis B core antibody positive; HBV, hepatitis B virus; Ln, natural log.
Table 4.
Multivariable Analysis of the Association of Donor Race and Graft Failure After Stratifying on Transplant Center and Adjusting for Donor-, Recipient-, and Transplant-Related Characteristics
| HR (95% CI) | P | |
|---|---|---|
| Donor | ||
| Race (reference, Caucasian) | ||
| AA | 1.06 (0.95–1.20) | .29 |
| API | 1.15 (0.89–1.49) | .30 |
| Other | 1.19 (1.05–1.35) | <.01 |
| Age, decade | 1.12 (1.09–1.15) | <.01 |
| Height, 10 cm | 0.91 (0.88–0.95) | <.01 |
| HBcAb (+) donor/HBV (−) recipient | 1.06 (0.89–1.27) | .51 |
| Recipient | ||
| Age, decade | 1.08 (1.03–1.13) | <.01 |
| Ln creatinine | 1.26 (1.17–1.36) | <.01 |
| Diagnosis, HCV | 1.28 (1.18–1.39) | <.01 |
HBcAb, hepatitis B core antibody positive; HBV, hepatitis B virus; Ln, natural log.
Interaction Between Donor and Recipient Race
Table 5 considers the interaction between donor and recipient race. The first row of Table 5 compares the hazard of graft failure in recipients of AA donors. In comparison with AA donor organs transplanted into AA recipients, there was a significant decrease in the risk of graft failure when an AA donor organ was transplanted to an other race recipient (HR, 0.62; 95% CI, 0.40–0.99), and a nonsignificant decrease when transplanted into a Caucasian recipient (HR, 0.93; 95% CI, 0.69–1.24) or API recipient (HR, 0.85; 95% CI, 0.44–1.66). API organs transplanted to non-API recipients were associated with a large increase in the risk of graft failure, although the effect was statistically significant only for AA recipients. However, only 16 API organs were transplanted into AA recipients. With regard to donors of other race, the increased risk of graft failure in multivariable analysis (Table 4) was not uniform. As shown in Table 5, transplantation of an other donor organ into an AA recipient (HR, 1.42; 95% CI, 0.94–2.14) was associated with an increased risk of graft failure whereas no association was observed when transplanted into an API recipient (HR, 0.94; 95% CI, 0.54–1.65) or Caucasian recipient (HR, 0.92; 95% CI, 0.7–1.22).
Table 5.
The Association Between Donor Race and Graft Failure in Separate Donor–Recipient Pairs After Stratification by Center
| Recipient race |
||||
|---|---|---|---|---|
| AA | API | Other | Caucasian | |
| Donor race | ||||
| AA (N = 1579) | N = 208 (13%) | N = 50 (3%) | N = 187 (12%) | N = 1134 (72%) |
| 1.0 (reference) | 0.85 (0.44–1.66) | 0.62 (0.40–0.99) | 0.93 (0.69–1.24) | |
| API (N = 243) | N = 16 (6%) | N = 36 (15%) | N = 48 (20%) | N = 143 (59%) |
| 5.14 (1.28–20.67) | 1.0 (reference) | 1.95 (0.64–5.98) | 2.41 (0.85–6.79) | |
| Other (N = 1421) | N = 103 (7%) | N = 63 (4%) | N = 300 (21%) | N = 955 (67%) |
| 1.42 (0.94–2.14) | 0.94 (0.54–1.65) | 1.0 (reference) | 0.92 (0.70–1.22) | |
| Caucasian (N = 7631) | N = 543 (7%) | N = 237 (3%) | N = 832 (11%) | N = 6019 (79%) |
| 1.21 (1.02–1.43) | 0.97 (0.73–1.30) | 0.87 (0.73–1.03) | 1.0 (reference) | |
NOTE. Transplantation of an organ between the same donor and recipient race serves as the reference. The HR of graft survival and the associated 95% CI are presented.
Examination of the DRI
A second multivariable analysis was performed to include the variables in the DRI, stratified on center (Table 6). Similar to results of the first multivariable analysis, the effect of AA donor was small and nonsignificant (HR, 1.04; 95% CI, 0.92–1.17). The effect of API was larger, but still not significant (HR, 1.18; 95% CI, 0.90–1.55), whereas that of other race was the largest and remained significant (HR, 1.22; 95% CI, 1.07–1.39; P < .01). The results were unchanged when only 3 race categories (Caucasian, AA, or other) were used. In addition to donor race, other donor factors such as age and height, donation after cardiac death, and cerebrovascular accident as a cause of death were confirmed to be important predictors of graft failure. On the other hand, anoxia or other cause of death and national/regional share had a small and nonsignificant effect. The effect of a partial/split donor was relatively large, yet statistically insignificant. The concordance statistics of the full DRI model (with race included) was 0.588 (95% CI, 0.576–0.600), whereas elimination of race from the model did not change the concordance (0.586; 95% CI, 0.574–0.598).
Table 6.
Association of Donor Race and Graft Failure After Inclusion of DRI Variables and Stratifying on Transplant Center
| HR (95% CI) | P | |
|---|---|---|
| Donor race (reference, Caucasian) | ||
| AA | 1.04 (0.92–1.17) | .53 |
| APIa | 1.18 (0.90–1.55) | .22 |
| Other | 1.22 (1.07–1.39) | <.01 |
| Donor age (reference, age <40 y) | ||
| 40–50 y | 1.17 (1.04–1.33) | .01 |
| 50–60 y | 1.33 (1.17–1.51) | <.01 |
| 60–70 y | 1.58 (1.37–1.83) | <.01 |
| >70 y | 1.82 (1.53–2.17) | <.01 |
| Cause of death (reference, head trauma) | ||
| Anoxia | 1.04 (0.90–1.21) | .57 |
| Cerebrovascular accident | 1.12 (1.00–1.26) | .04 |
| Other | 0.92 (0.70–1.22) | .58 |
| Donor height adjustedb | 1.07 (1.03–1.11) | <.01 |
| Donation after cardiac death | 1.73 (1.42–2.09) | <.01 |
| Partial/split liver | 1.30 (0.94–1.82) | .12 |
| National share | 0.96 (0.80–1.16) | .68 |
| Regional share | 1.03 (0.92–1.16) | .60 |
| Cold ischemia time, h | 1.01 (1.00–1.02) | .09 |
In DRI, other race included API donor.
Adjusted height: (170 – height)/10.
Discussion
Over the past 2 decades, the outcome of LTx has improved steadily. More recently, however, the shortage of available organs has necessitated increasing the use of marginal donors. In that context, identification of donor-related factors that portend a poor outcome after LTx and analyses to guide the use of organs according to donor characteristics has become increasingly important. The race of the donor has been identified as a predictor of graft failure, in other words, an indicator of donor quality. If there is a biological basis to this characterization, it has important consequences in organ allocation policy and patient management.
However, there are several reasons why donor race should not be construed as an indicator of donor quality. First, it is likely that various factors confound the observed association between donor race and graft failure. As discussed later, the results of this analysis suggest that at least part of the association between donor race and graft survival could be explained by considering a few simple covariates. Second, even if there is truly a biological basis, it is unlikely that the risk of graft failure is uniform across all donor–recipient race pairs.10,11 Third, the DRI that proposes an association between non-Caucasian donor race and graft failure has not been validated based on an independent data set. Similarly, the DRI is based on an analysis of data before implementation of the current allocation system based on the MELD score. To the extent that the new allocation system represented a fundamental change in the practice of LTx, the DRI needed to be examined with a modern data set.1
Our analysis clearly showed that stratification by transplant center led to diminution of the association between donor race and graft failure, especially AA donors. Transplantation outcomes have been associated with center volume, provider volume, and “center quality.”12-14 Transplant centers vary in the number of annual number of transplants, surgeon experience, and center performance, all factors associated with graft failure.12-15 Furthermore, high-volume centers (>100 transplantations/y) tend to have shorter waiting times, which allows transplantations for patients with a lower MELD score as compared with medium- or low-volume centers, possibly contributing to differential outcomes.9 Given that there is regional variability in organ procurement for LTx as well as regional variation in population demographics, it is possible that non-Caucasian donors, specifically AA donors, may be overrepresented in centers/regions with poor outcomes, which could lead to an erroneous conclusion that donor race is associated with poor outcomes.16
The risk of graft failure associated with API donors decreased from 41% to 15% after adjusting for center and other confounders including HBc status and donor height. The deleterious effects of donor organs too small for the recipient body size as well as transplantation of HBc–positive organs into hepatitis B–naive recipients are well recognized.8 The fact that these organs were used despite the knowledge of these factors may indicate that the recipients were desperate enough to receive these organs, the details of which may not be captured by the information available in the Organ Procurement and Transplantation Network data. Thus, the residual effect of API organs still may not be attributable to the donor, per se.
The effect of the other donor race was not explained easily. One still could hypothesize a contribution of unmeasured confounders in the recipient. For example, Table 1 shows that recipients of other donor organs were significantly more likely to have a high MELD score and to receive a partial/split organ than other recipients, raising the possibility that there may have been a systematic difference in that recipient group that is not apparent in the variables represented in the database. Further, Table 5 shows that the effect of other race was not uniform and limited to AA recipients, extending the possibility that recipient factors may explain the observation. Another hypothesis may be put forth based on epidemiologic data that individuals of Hispanic ethnicity in the United States have a higher prevalence of obesity and nonalcoholic fatty liver disease. Thus, macrovesicular steatosis in the donor organ, which has been associated with decreased graft survival, may be more common in these donors.17,18 The Organ Procurement and Transplantation Network data are limited in that biopsy information is available in only 30% of all donors and less than half of those records (45.2%) have data on macrovesicular steatosis. In this highly selected group, a larger percentage of other donors had macrovesicular steatosis (8.4% ± 13.5%) vs API (4.1% ± 8.2%), AA (6.5% ± 9.6%), and Caucasian (7.4% ± 10%) donors; however, this result was not statistically significant (P = .65).
Although some of these important questions remain to be answered, our data largely refute suggestions that donor race be considered as an indicator of donor quality. Although we were unable to completely explain the association of donor race with graft failure, substantial parts were attributable to more direct factors. As discussed earlier, some of the residual effects may reflect nonracial donor or recipient characteristics that are not identified in the database. Finally, the concordance statistics of the DRI model with and without donor race leave little justification to keep the variable in the model.
We conclude, based on analyses conducted in a representative data set from a recent era, that donor race (eg, AA and API) largely may be a surrogate of other more direct biological or socioeconomic factors of the donor and recipient that affect the graft outcome. Some of the effects of the donor race/ethnicity (eg, Hispanic ethnicity) could not be explained easily with the current analysis and further focused research is indicated. In our opinion, this analysis provides sufficient grounds to recommend against using donor race in the organ allocation process.
Acknowledgments
Funding
This study was supported by a grant from the National Institutes of Health (R01DK-34238) and a National Institutes of Health digestive diseases training grant (T32 DK07198).
Abbreviations used in this paper
- AA
African American
- API
Asian or Pacific Islander
- CI
confidence interval
- DRI
Donor Risk Index
- HR
hazard ratio
- LTx
liver transplantation
- MELD
Model for End-Stage Liver Disease
Footnotes
Conflicts of interest
The authors disclose no conflicts.
References
- 1.Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783–790. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 2.Ioannou GN. Development and validation of a model predicting graft survival after liver transplantation. Liver Transpl. 2006;12:1594–1606. doi: 10.1002/lt.20764. [DOI] [PubMed] [Google Scholar]
- 3.Schaubel DE, Guidinger MK, Biggins SW, et al. Survival benefit-based deceased-donor liver allocation. Am J Transplant. 2009;9:970–981. doi: 10.1111/j.1600-6143.2009.02571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dawson S, 3rd, Imagawa DK, Johnson C, et al. UCLA liver transplantation: analysis of immunological factors affecting outcome. Artif Organs. 1996;20:1063–1072. doi: 10.1111/j.1525-1594.1996.tb00642.x. [DOI] [PubMed] [Google Scholar]
- 5.Neylan JF. Racial differences in renal transplantation after immunosuppression with tacrolimus versus cyclosporine. FK506 Kidney Transplant Study Group. Transplantation. 1998;65:515–523. doi: 10.1097/00007890-199802270-00011. [DOI] [PubMed] [Google Scholar]
- 6.Volk ML, Choi H, Warren GJ, et al. Geographic variation in organ availability is responsible for disparities in liver transplantation between Hispanics and Caucasians. Am J Transplant. 2009;9:2113–2118. doi: 10.1111/j.1600-6143.2009.02744.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee TH, Shah N, Pedersen RA, et al. Survival after liver transplantation: is racial disparity inevitable? Hepatology. 2007;46:1491–1497. doi: 10.1002/hep.21830. [DOI] [PubMed] [Google Scholar]
- 8.Wachs ME, Amend WJ, Ascher NL, et al. The risk of transmission of hepatitis B from HBsAg(−/−), HBcAb(+), HBIgM(−/−) organ donors. Transplantation. 1995;59:230–234. [PubMed] [Google Scholar]
- 9.Ahmad J, Bryce CL, Cacciarelli T, et al. Differences in access to liver transplantation: disease severity, waiting time, and transplantation center volume. Ann Intern Med. 2007;146:707–713. doi: 10.7326/0003-4819-146-10-200705150-00004. [DOI] [PubMed] [Google Scholar]
- 10.Callender CO, Cherikh WS, Miles PV, et al. Blacks as donors for transplantation: suboptimal outcomes overcome by transplantation into other minorities. Transplant Proc. 2008;40:995–1000. doi: 10.1016/j.transproceed.2008.03.063. [DOI] [PubMed] [Google Scholar]
- 11.Eckhoff DE, McGuire BM, Young CJ, et al. Race: a critical factor in organ donation, patient referral and selection, and orthotopic liver transplantation? Liver Transpl Surg. 1998;4:499–505. doi: 10.1002/lt.500040606. [DOI] [PubMed] [Google Scholar]
- 12.Burroughs AK, Sabin CA, Rolles K, et al. 3-month and 12-month mortality after first liver transplant in adults in Europe: predictive models for outcome. Lancet. 2006;367:225–232. doi: 10.1016/S0140-6736(06)68033-1. [DOI] [PubMed] [Google Scholar]
- 13.Scarborough JE, Pietrobon R, Tuttle-Newhall JE, et al. Relationship between provider volume and outcomes for orthotopic liver transplantation. J Gastrointest Surg. 2008;12:1527–1533. doi: 10.1007/s11605-008-0589-5. [DOI] [PubMed] [Google Scholar]
- 14.Schold JD, Srinivas TR, Howard RJ, et al. The association of candidate mortality rates with kidney transplant outcomes and center performance evaluations. Transplantation. 2008;85:1–6. doi: 10.1097/01.tp.0000297372.51408.c2. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Medicare and Medicaid Services Medicare program; hospital conditions of participation: requirements for approval and re-approval of transplant centers to perform organ transplants. Final rule. Fed Regist. 2007;72:15197–15280. [PubMed] [Google Scholar]
- 16.Kemmer N, Safdar K, Kaiser T, et al. Impact of geographic location on access to liver transplantation among ethnic minorities. Transplantation. 2008;85:166–170. doi: 10.1097/TP.0b013e31816223f8. [DOI] [PubMed] [Google Scholar]
- 17.Marsman H, Matsushita T, Dierkhising R, et al. Assessment of donor liver steatosis: pathologist or automated software? Hum Pathol. 2004;35:430–435. doi: 10.1016/j.humpath.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 18.Weston SR, Leyden W, Murphy R, et al. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology. 2005;41:372–379. doi: 10.1002/hep.20554. [DOI] [PubMed] [Google Scholar]