Abstract
Objective
Diets of lower energy density are associated with higher diet quality, lower body weights, and better health outcomes. This study examined the association between dietary energy density, energy-adjusted diet costs and socioeconomic indicators of study participants.
Design
In this cross-sectional study, energy and nutrient intakes for 164 men and women aged 25–65y were obtained using a food frequency instrument between June 2005 and September 2006. Dietary energy density (kcal/g) was calculated with and without beverages. Energy-adjusted diet costs ($/2,000 kcal) were calculated using food prices in Seattle. Tertile splits of energy density and energy cost were analyzed using tests for linear trend. Linear regression models tested the association between gender, education, income and dietary variables, adjusting for age.
Results
Diets of lower energy density were associated with higher absolute nutrient intakes. Diets of lower energy density were also associated with higher energy-adjusted diet costs. Conversely, highest energy density diets were associated with lower intakes of micronutrients and fiber and lower costs. Education and household income showed a negative association with dietary energy density in regression models. Education and household incomes showed a positive association with the energy-adjusted cost of the diet and education was a stronger predictor of both energy density and energy cost than was household income.
Conclusion
Higher-quality diets were not only more costly per kcal but were also consumed by persons of higher educational level. The impact of diet quality on health, observed in some epidemiologic studies, might be modulated by unobserved indices of socioeconomic status.
Keywords: Dietary energy density, energy intake, food price, diet cost, incomes, education, nutritional epidemiology, Diet quality, dietary guidance, obesity, economics
Introduction
Studies on the social and economic determinants of health have shown that persons and groups of higher socioeconomic status (SES) have lower rates of obesity, type 2 diabetes, and cardiovascular disease (1). The literature suggests that some of the observed disparities in health may be related to disparities in diet quality (2–5). The more affluent are not only healthier and thinner but also consume higher-quality diets (6). It is not clear whether the more favorable health outcomes can be attributed to better diets, higher SES, or some combination of both (7).
The energy density of the diet (i.e. available energy per unit weight) (8) is one indicator of diet quality. Lean meats, fish, low-fat dairy products and fresh vegetables and fruit provide less energy per unit weight than do fast foods, sweets, candy and desserts (9, 10). Whereas energy-dense foods tend to be nutrient-poor, foods of low energy density provide more nutrients relative to calories (11). An inverse relation between energy density and nutrient density has now been demonstrated both for individual foods (11) and for total diets (12).
Diets of low energy density and high nutrient content have been associated with less weight gain (13) and with lower rates of obesity (14–16), type 2 diabetes (17), cardiovascular disease (18–20), and some forms of cancer (21). In contrast, energy-dense diets have been linked to higher obesity rates and higher disease risk (22). Improving diet quality by lowering its energy density is standard advice for weight control (23), cancer prevention (24), and better health (25).
However, higher quality diets of lower-energy-density are likely to cost more (2, 26). Diets composed of whole grains, lean meats and fish, low-fat dairy products, and fresh vegetables and fruit were more costly per kilocalorie than were energy-dense diets, rich in fats and sweets (27–32). In Europe, high nutrient content of the diet was strongly associated with higher diet costs, adjusted for energy (33–35). In the United States (US), the price disparity between foods of low versus high energy density continues to grow: a recent study showed that the lowest energy density foods, mostly fresh vegetables and fruit, increased in price by almost 20% over a 2 year period, whereas energy-dense sugars and fats did not (36, 37).
The important question is whether higher-quality but more costly diets are more likely to be consumed by more affluent persons. A key challenge in nutritional epidemiology is to make sure that persons or groups characterized by a given eating pattern do not differ in some fundamental yet unobserved way from persons with another type of eating pattern. Given that higher SES groups often have both higher quality diets and lower disease risk, epidemiologic studies tend to treat SES as a potential confounder. In order to reveal associations between dietary exposures and chronic disease risk, studies have adjusted for SES (38) whenever such variables were available. The present study had a different purpose, focusing on indicators of SES as exposure variables, and exploring the association between SES measures and dietary energy density and energy-adjusted diet cost.
The hypothesis was that lower-energy-density diets would be associated with higher nutrient intakes – and with higher dietary energy costs. A related hypothesis was that diets with higher energy costs but that were also more nutrient-rich would be associated with higher educational levels and higher incomes. Clarifying the relation between SES variables, diet quality, and diet cost has many implications for studies of diet and disease risk and for the design of dietary strategies for health promotion.
Methods
Participants
The study was based on a stratified sample of faculty and staff of a large public university in the Pacific Northwest. The sampling frame was stratified by ranges of university salaries, obtained from the publicly-available payroll system. There were 20 salary strata, with means ranging from a $1,408 per month to $13,924 per month, with participant recruitment based on random sampling within each strata. While salary data were used for targeting recruitment letters, the key income variable in the final analyses was household income, not individual salaries (see below). Heights and weights for all participants were measured in the laboratory using a physician’s 175 kg scale and stadiometer (Detecto, Webb City, MO). All participants were compensated $100 at the termination of the study. Since a key feature of the study was the estimation of diet costs using supermarket food prices, individuals who consumed away-from-home foods or beverages six times or more during the one-week food record period were excluded. All procedures had been reviewed and approved by the university institutional review board (IRB).
Dietary Intake Assessment
Dietary intakes used in these analyses were obtained using the G-SEL version of the Fred Hutchinson Cancer Research Center (FHCRC) food frequency instrument (FFQ). Participants received a 20 minute training by a registered dietitian on how to complete the FFQ during their first visit to the laboratory. The training involved a serving size photo booklet for reference. Participants completed the FFQ during this visit and project staff were on hand during the administration of the questionnaire to answer questions and assist with serving size or frequency estimations. Participants recorded the frequency of consumption of 152 line-item foods and beverages and indicated portion size. Each questionnaire was reviewed for completion before the participant left the laboratory. Customized nutrient analysis software, developed by the FHCRC, links the FFQ food intake data to the nutrient database at the Nutrition Coordinating Center at the University of Minnesota (39, 40). The Minnesota database is primarily derived from the United States Department of Agriculture’s (USDA) National Nutrient Database for Standard Reference, maintained by the Nutrient Data Laboratory in Beltsville and supplemented with information from food manufacturers. To calculate individual nutrient intakes, the software multiplies frequency of use of each FFQ item by portion size and by the weighted vector of nutrient values for each component food. Each of the 384 component foods in is associated with an array of nutrient values, energy and water per 100g serving.
Dietary energy density and nutrient content
Nutrient composition analyses of dietary intake data yielded dietary energy (kcal), the weight of foods, beverages, and drinking water (g), and the estimated daily intakes of over 45 macro- and micronutrients. Dietary energy density was calculated as available energy divided by the weight of foods and beverages. Calculations of energy density (kcal/g) followed past models (10, 16, 41). Dietary energy density calculations were based on: 1) all foods and all beverages, with the exception of drinking water; and 2) on foods only, excluding all beverages, both caloric and non caloric. In past studies (10, 16), dietary energy density based on foods only was better correlated with indices of diet quality, including micronutrient content (10, 34).
Diet cost assessment
Mean daily diet costs were estimated by attaching a food price vector to the nutrient composition database. The FHCRC FFQ is composed of 152 line item foods and 384 underlying component foods. For example, the nutrient composition of a composite item such as “apples, applesauce and pears” is actually based on a weighted mean of underlying component foods, which include fresh apples, applesauce, fresh pears, and canned pears. The weights used in the construction of the FFQ are derived based on food consumption data (when available) or on expert judgment. The present method to estimated diet costs was based on attaching retail price for each of the 384 component food items in the FFQ nutrient composition database. Price collection methods are provided in detail in a separate study (37). The analyses were based on 2006 prices obtained at 3 different supermarket chains in the Seattle metropolitan region.
The monetary value for each diet was calculated in a manner analogous to that used to obtain nutrient values. Retail prices, expressed per 100g edible portion, were added to the G-SEL nutrient database, to parallel nutrient values, expressed as amounts (g/mg/μg/IU) per 100g edible portion. In this way, each of the 384 foods in the G-SEL database was associated with 45 nutrient vectors and a single cost vector, both expressed per 100g of edible portion. The final monetary variable associated with each individual’s diet was the mean cost per day ($/d). For each diet, this variable was then divided by the individual’s reported mean energy intake- in kcal- and multiplied by 2000 in order to express the cost of the diet per 2000 kcal of dietary energy.
Socioeconomic Measures
For each participant, self-reported education and household incomes were used as indicators of SES. The highest level of formal education was measured in 9 categories ranging from “elementary school” to “doctorate degree (PhD, DPhil)”. Options for reporting household incomes ranged from “less than $15,000 per year” in 10,000 increments to “$115,000 per year and above”. For regression analyses these variables were re-coded. Highest level of education completed was re-coded into 3 categories relative to the attainment of a bachelor’s (4-yr) degree. Household income categories were re-coded into 4 categories (see results below).
Statistical analyses
All analyses were first conducted separately for men and women. Bivariate methods were used to explore the relation between dietary energy density and energy-adjusted diet costs. Participants were stratified by gender-specific tertiles of energy density and energy-adjusted diet costs, same as in past studies (10, 16), and linear trend tests were used to identify significant differences in the mean intakes of macro- and micronutrients among tertiles. Data for men and women were combined to examine the crude relation between income, education and measures of energy-adjusted diet cost and diet quality. Finally, linear regression models tested the association between SES variables and dietary energy density and energy-adjusted diet costs, with age, gender, and household size as covariates. SES variables were coded as dummy variables, with the lowest level used as the reference group. Race and ethnicity were not included as covariates, given that the sample was small and 85% white.
Results
Study Participants
Over 3,000 introductory letters were sent to pre-selected respondents via campus mail. Of these, 350 persons responded by mail or by phone and, depending on work schedules and other commitments, 259 were invited to attend an introductory orientation meeting and provide consent. Persons who never began study protocols; those who dropped out in the course of the 5-week study; those who failed to complete all questionnaires, including food frequency questionnaires and dietary records, or who did not keep food expenditure records for 4 weeks, were excluded from analysis. The final sample of 164 (103 women and 61 men) provided complete food frequency questionnaires and four-day dietary records, and completed all demographic and behavioral questionnaires
Mean age of participants was 40.3 y (range 25–65y). Mean age was 42.2 y for women and 38.0 y for men. Most men (92%) and most women (85%) had completed a bachelor’s degree or higher. A majority of women (60%) and half the men (50%) had annual household incomes of $55,000 and above. Most men (84%) and women (82%) identified themselves as white, with the rest being Asian or Pacific Islander (6.8% of men, 12% of women) and African American (3.4% of men, 4% of women). Demographic and SES data are summarized in Table 1.
Table 1. Demographic and socio-economic characteristics of study sample.
Unless otherwise indicated, values shown are means (SD)
| Men | Women | All | |
|---|---|---|---|
| Sample size | 61 | 103 | 164 |
| Age (years) | 37.7 (9.7) | 42 (10.4) | 40.3 (10.3) |
| Body Weight (kg) | 77.7 (10.8) | 73.9 (18.5) | 75.4 (16.1) |
| Body Mass Index (kg/m2) | 25 (2.8) | 26.6 (6.3) | 26 (5.3) |
| Number of individuals residing in householda | 2.1 (1.1) | 2.4 (1.4) | 2.3 (1.3) |
| % reporting very good or excellent health | 82 | 75.7 | 78 |
| % never smoked | 63.9 | 67 | 65.9 |
| % non-Hispanic white | 84.7 | 82 | 83 |
| % with bachelor’s degree or higher | 91.8 | 85.3 | 89 |
| % with household incomes ≥$55,000/y | 50.8 | 60.2 | 56.7 |
includes adults and children.
Energy and nutrient intakes
Daily energy intakes calculated including all foods and all beverages except drinking water were 2,088 kcal (8.74 MJ) for men and 1,779 kcal (7.44 MJ) for women. Dietary energy density was 0.92 kcal/g (3.85MJ/kg) for men and 0.85 kcal/g (3.56 MJ/kg) for women.
Daily energy intakes calculated for foods only and excluding all beverages were 1,806 kcal for men and 1,543 kcal for women. Dietary energy density was 1.48 kcal/g (6.2 MJ/kg) for men and 1.35 kcal/g (5.6 MJ/kg) for women. These values are entirely consistent with prior research, sometimes based on far larger population samples (10).
Dietary energy density was positively associated with crude macronutrient intakes (in g), also consistent with past studies (10, 41). For both men and women, higher dietary energy density was associated with higher intakes of total fat and saturated fat and with lower intakes of dietary fiber, potassium and vitamins A and C. Table 2 shows mean energy and nutrient intakes by gender-specific energy density tertiles, where energy density was calculated without beverages.
Table 2.
Mean energy & nutrient intake and diet cost by tertile of dietary energy density for women and men. Diets excluding beverages.
| Women | Lowest Tertile (n=34) | Middle Tertile (n=35) | Highest Tertile (n=34) | Trend Test Pa | |||
|---|---|---|---|---|---|---|---|
| Nutrient | Mean | SD | Mean | SD | Mean | SD | |
| Dietary Energy Density (kcal/g) | 1.04 | 0.11 | 1.32 | 0.08 | 1.69 | 0.19 | <0.001 |
| Energy (kcal) | 1484 | 501 | 1538 | 446 | 1609 | 634 | .335 |
| Total Fat (g) | 49.5 | 21.8 | 59.8 | 17.3 | 71.6 | 30.1 | <0.001 |
| Total Saturated Fatty Acids (g) | 15.0 | 6.6 | 18.8 | 6.1 | 22.6 | 10.0 | <0.001 |
| Total Dietary Fiber (g) | 25.9 | 10.1 | 20.8 | 8.0 | 16.8 | 6.4 | <0.001 |
| Added Sugars (g) | 40.4 | 16.0 | 46.8 | 24.9 | 48.4 | 30.9 | .187 |
| Vitamin A (IU) | 22267 | 13291 | 12587 | 7822 | 6706 | 3553 | <0.001 |
| Vitamin C (mg) | 138 | 59 | 95 | 36 | 65 | 32 | <0.001 |
| Calcium (mg) | 750 | 304 | 717 | 301 | 671 | 318 | .292 |
| Iron (mg) | 14 | 7 | 14 | 6 | 13 | 6 | .474 |
| Potassium (mg) | 2790 | 931 | 2332 | 763 | 1899 | 717 | <0.001 |
| Dietary Energy Cost ($/2000kcal) | 9.55 | 1.82 | 8.06 | 1.25 | 6.76 | 0.87 | <0.001 |
| Men | Lowest Tertile (n=20) | Middle Tertile (n=21) | Highest Tertile (n=20) | Trend Test Pa | |||
| Nutrient | Mean | SD | Mean | SD | Mean | SD | |
| Dietary Energy Density (kcal/g) | 1.19 | 0.10 | 1.42 | 0.09 | 1.84 | 0.25 | <0.001 |
| Energy (kcal) | 1760 | 614 | 1758 | 518 | 1902 | 846 | .505 |
| Total Fat (g) | 58.5 | 24.9 | 65.7 | 18.2 | 86.5 | 38.5 | .003 |
| Total Saturated Fatty Acids (g) | 17.3 | 8.5 | 20.7 | 4.9 | 27.0 | 11.5 | .001 |
| Total Dietary Fiber (g) | 28.2 | 11.0 | 23.6 | 10.7 | 19.2 | 9.9 | .008 |
| Added Sugars (g) | 48.7 | 24.7 | 51.5 | 31.4 | 47.9 | 34.8 | .939 |
| Vitamin A (IU) | 16082 | 9901 | 10515 | 6414 | 7927 | 7288 | .002 |
| Vitamin C (mg) | 112 | 51 | 98 | 56 | 64 | 27 | .002 |
| Calcium (mg) | 819 | 343 | 789 | 336 | 770 | 437 | .680 |
| Iron (mg) | 17 | 5 | 17 | 7 | 16 | 8 | .856 |
| Potassium (mg) | 2807 | 1071 | 2465 | 854 | 2098 | 1018 | .026 |
| Dietary Energy Cost ($/2000kcal) | 7.82 | 1.28 | 7.74 | 1.27 | 6.71 | 1.15 | .006 |
Significance based on test of linear change in mean across tertiles of dietary energy density.
Diet quality and diet cost
Daily diet cost ($/day) was slightly higher for men ($6.72/day) than women ($6.21/day), reflecting the fact that men ate more. However, the difference reversed after adjusting for energy. For each 2,000 kcal of dietary energy, men spent $7.43 compared to $8.12 spent by women. The cost of dietary energy was negatively and significantly associated with dietary energy density in the sample of women. Table 2 shows that the mean energy cost ($/2000kcal) of the lowest tertile by energy density group was 41% higher than the energy cost of the highest tertile ($9.55 vs $6.76). Men showed similar, but weaker associations between energy density and energy cost.
Figure 1 shows the inverse relation between dietary energy density and energy-adjusted diet cost (r2=0.37), one that was largely driven by a stronger correlation for women (r2=0.51) but not for men (r2=0.09; ns). Men and women also showed differences in the slope of the relation between dietary energy density and energy cost. Each additional dollar in energy cost for women led to a decrease in energy density of 0.12 kcal/g (0.50 MJ/kg). In contrast, each additional dollar in energy cost for men led to a decrease in energy density of only 0.07 kcal/g (0.29 MJ/kg).
Figure 1.
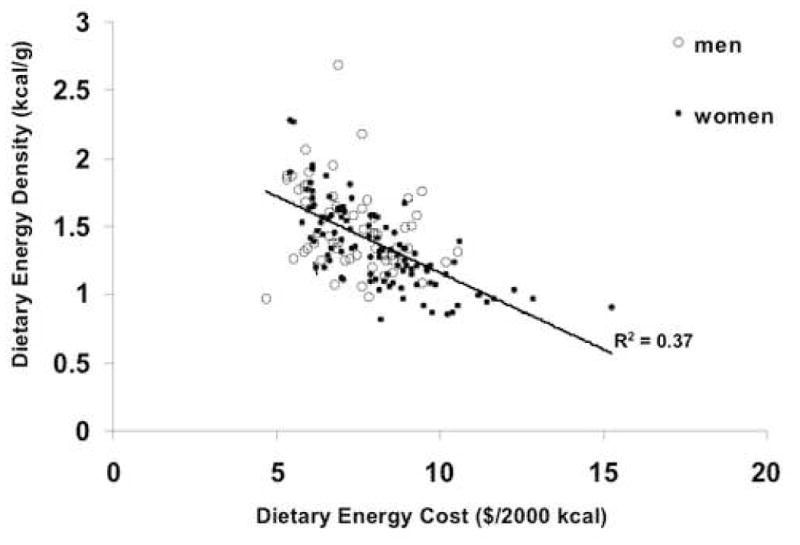
Dietary energy density is inversely correlated with diet cost. A scatterplot showing the relation between energy density (kcal/g) and diet cost adjusted for energy intake ($/2000 kcal) for 164 subjects. Energy density calculated without beverages. Symbols indicate males (n=61) and females (n=103). Least-squares regression line fit to all data points. Correlation coefficient r2= 0.37.
Diets that were more costly in terms of $/2000 kcal were also lower in energy density and contained higher levels of nutrients. Table 3 shows mean energy and nutrient intakes by gender-specific tertiles of dietary energy cost, calculated without beverages. For both women and men, higher energy costs were associated with significantly lower dietary energy density and with significantly higher intakes of vitamin C, potassium and total fiber. Higher energy costs were also associated with significantly higher intakes of vitamin A and saturated fat in women.
Table 3.
Mean energy & nutrient intake and diet cost by tertile of dietary energy cost for women and men. Diets excluding beverages.
| Women | Lowest Tertile (n=34) | Middle Tertile (n=35) | Highest Tertile (n=34) | Trend Test Pa | |||
|---|---|---|---|---|---|---|---|
| Nutrient | Mean | SD | Mean | SD | Mean | SD | |
| Dietary Energy Cost ($/2000kcal) | 6.35 | 0.43 | 7.94 | 0.53 | 10.09 | 6.35 | <0.001 |
| Dietary Energy Density (kcal/g) | 1.60 | 0.27 | 1.33 | 0.22 | 1.12 | 1.60 | <0.001 |
| Energy (kcal) | 1594 | 562 | 1545 | 529 | 1490 | 1594 | 0.423 |
| Total Fat (g) | 65.8 | 26.7 | 60.8 | 24.6 | 54.2 | 65.8 | 0.056 |
| Total Saturated Fatty Acids (g) | 20.7 | 9.0 | 19.2 | 8.3 | 16.4 | 20.7 | 0.034 |
| Total Dietary Fiber (g) | 18.5 | 8.3 | 21.3 | 8.9 | 23.8 | 18.5 | 0.016 |
| Added Sugars (g) | 50.9 | 27.8 | 45.1 | 27.2 | 39.6 | 50.9 | 0.060 |
| Vitamin A (IU) | 7592 | 5578 | 14487 | 10538 | 19426 | 7592 | <0.001 |
| Vitamin C (mg) | 64 | 33 | 102 | 40 | 132 | 64 | <0.001 |
| Calcium (mg) | 661 | 285 | 738 | 316 | 738 | 661 | 0.302 |
| Iron (mg) | 12 | 5 | 14 | 7 | 14 | 12 | 0.219 |
| Potassium (mg) | 1997 | 705 | 2340 | 843 | 2684 | 1997 | 0.001 |
| Men | Lowest Tertile (n=20) | Middle Tertile (n=21) | Highest Tertile (n=20) | Trend Test Pa | |||
| Nutrient | Mean | SD | Mean | SD | Mean | SD | |
| Dietary Energy Cost ($/2000kcal) | 5.96 | 0.53 | 7.42 | 0.45 | 8.90 | 0.67 | <0.001 |
| Dietary Energy Density (kcal/g) | 1.58 | 0.29 | 1.51 | 0.39 | 1.35 | 0.18 | 0.017 |
| Energy (kcal) | 1781 | 717 | 1742 | 610 | 1897 | 686 | 0.588 |
| Total Fat (g) | 73.3 | 38.5 | 65.7 | 28.4 | 71.6 | 23.0 | 0.862 |
| Total Saturated Fatty Acids (g) | 22.7 | 11.7 | 20.9 | 9.6 | 21.5 | 6.8 | 0.698 |
| Total Dietary Fiber (g) | 20.6 | 7.0 | 21.9 | 8.9 | 28.5 | 14.5 | 0.022 |
| Added Sugars (g) | 44.7 | 31.8 | 49.9 | 30.1 | 53.6 | 29.3 | 0.361 |
| Vitamin A (IU) | 9138 | 7259 | 11606 | 9948 | 13726 | 7943 | 0.093 |
| Vitamin C (mg) | 67 | 28 | 79 | 33 | 130 | 60 | <0.001 |
| Calcium (mg) | 805 | 410 | 733 | 308 | 843 | 393 | 0.743 |
| Iron (mg) | 16 | 8 | 16 | 6 | 18 | 8 | 0.358 |
| Potassium (mg) | 2192 | 808 | 2257 | 867 | 2932 | 1189 | 0.019 |
Significance based on test of linear change in mean across tertiles of dietary energy cost.
Socioeconomic Status, Dietary Energy Density and Diet Cost
Higher education and incomes were associated with lower dietary energy density and higher energy costs. Table 4 shows the impact of education and income levels on dietary energy density (kcal/g), mean daily diet cost ($/day), and energy adjusted diet costs ($/2000kcal). In these analyses, dietary energy density and cost were calculated without beverages and including all beverages except drinking water. As expected, the inclusion of beverages increased mean daily diet costs and energy-adjusted diet cost, while energy density was reduced.
Table 4.
Unadjusted mean daily diet cost, dietary energy cost, and energy density by categories of participant’s income and education levels. Energy density (ED) calculated excluding and including beverages.
| Diet excluding all beverages |
Diet including all beverages except drinking water |
|||||
|---|---|---|---|---|---|---|
| Daily diet cost ($/d) | Energy cost ($/2000 kcal) | Dietary ED (kcal/g) | Daily diet cost ($/d) | Energy cost ($/2000 kcal) | Dietary ED (kcal/g) | |
| Income | ||||||
| $15,000 – $44,999 (n=50) | 6.57 ± 2.75 | 7.59 ± 1.54 | 1.42 ± 0.30 | 7.56 ± 2.86 | 7.78 ± 1.47 | 0.94 ± 0.22 |
| $45,000 – $74,999 (n=57) | 6.31 ± 2.28 | 7.71 ± 1.44 | 1.43 ± 0.29 | 7.62 ± 2.64 | 7.99 ± 1.53 | 0.87 ± 0.21 |
| $75,000 – $104,999 (n=27) | 6.16 ± 2.63 | 8.06 ± 2.01 | 1.41 ± 0.37 | 7.79 ± 2.71 | 8.67 ± 1.96 | 0.79 ± 0.20 |
| ≥ $105,000 (n=30) | 6.47 ± 2.34 | 8.45 ± 1.74 | 1.29 ± 0.30 | 7.80 ± 2.74 | 8.83 ± 1.79 | 0.83 ± 0.23 |
| Education | ||||||
| < Bachelor’s Degree (n=18) | 5.63 ± 2.15 | 7.07 ± 1.46 | 1.66 ± 0.42 | 6.86 ± 2.47 | 7.39 ± 1.74 | 1.02 ± 0.23 |
| Bachelor’s Degree (n=68) | 6.50 ± 2.48 | 7.92 ±1.77 | 1.42 ± 0.27 | 7.80 ± 2.71 | 8.17 ±1.68 | 0.87 ± 0.21 |
| Post-graduate Degree (n=77) | 6.51 ± 2.56 | 8.00 ± 1.55 | 1.32 ± 0.28 | 7.77 ± 2.77 | 8.40 ± 1.64 | 0.85 ± 0.22 |
While daily diet cost followed no consistent trend with higher levels of income, energy-adjusted diet cost increased monotonically with income. Similarly, dietary energy density decreased monotonically with progressively higher levels of household income. Educational level showed similar associations with dietary measures. Notably, higher levels of education were associated with a higher cost per kcal and progressively lower dietary energy density.
The associations between SES variables and dietary energy density were examined using regression models to control for covariates, shown in Table 5. Income effects were examined at three higher levels with reference to the lowest-income group. Similarly, education effects were examined at two higher levels with reference to the least-educated group. Again, analyses were conducted for dietary intakes excluding all beverages and including all beverages except water. Both analyses adjusted for age and household size and as covariates of education and household income.
Table 5.
Coefficients for two regression models. Dependent Variable: Dietary Energy Density (ED, kcal/g) calculated without beverages and including all beverages except drinking water. All Subjects (n=164)
| ED of diet excluding all beverages |
ED of diet excluding water only |
|||||||
|---|---|---|---|---|---|---|---|---|
| β | 95 % CI for β | Sig | β | 95 % CI for β | Sig | |||
| lower | upper | lower | upper | |||||
| Gendera | −0.16 | −0.25 | −0.07 | .001 | −0.09 | −0.15 | −0.02 | .008 |
| Household Income (thousands)b: | ||||||||
| $45 -- $74.9 | −0.01 | −0.10 | 0.12 | .844 | −0.05 | −0.13 | 0.03 | .200 |
| $75 -- $104.9 | −0.02 | −0.16 | 0.11 | .761 | −0.14 | −0.24 | −0.04 | .005 |
| $105 and higher | −0.03 | −0.17 | 0.11 | .652 | −0.07 | −0.17 | 0.04 | .195 |
| Highest education c: | ||||||||
| Bachelor’s degree | −0.27 | −0.42 | −0.11 | .001 | −0.14 | −0.26 | −0.03 | .014 |
| Post-graduate degree | −0.34 | −0.49 | −0.19 | <0.001 | −0.16 | −0.27 | −0.05 | .006 |
Reference group for gender was men.
Reference group for household income are households with incomes between $15 and $44.9 thousand.
Reference group for highest education was group attaining any level of education below a bachelor’s (4-yr) degree.
Both models adjusted for total weight of the diet, respondent’s age and household size.
In both analyses, gender was significantly associated with dietary energy density with women consuming lower-energy density diets than men. Both analyses also showed that the lowest-energy density diets were consumed by the most highly-educated respondents, independent of income. The effect of education showed a dose-response pattern with higher levels of education linked to progressively lower dietary energy density.
Regression models then examined the relative impact of education and income on energy costs. As in the analysis of energy density, energy-adjusted diet costs were calculated with and without beverages, shown in Table 6. Both analyses revealed that gender was significantly associated with dietary energy cost, with females spending significantly more per 2000 kcal (8.37 MJ) than men.
Table 6.
Coefficients for two regression models. Dependent Variable: Energy-adjusted diet cost ($/2000 kcal), calculated without beverages and including all beverages except drinking water. All Subjects (n=164).
| Energy-adjusted diet cost excluding all beverages |
Energy-adjusted diet cost excluding water only |
|||||||
|---|---|---|---|---|---|---|---|---|
| β | 95 % CI for β | Sig | β | 95 % CI for β | Sig | |||
| lower | upper | lower | upper | |||||
| Gendera | 0.73 | 0.19 | 1.26 | .009 | 0.624 | 0.08 | 1.17 | .025 |
| Household Income (thousands) b: | ||||||||
| $45 -- $74.9 | 0.12 | −0.52 | 0.76 | .704 | 0.23 | −0.41 | 0.87 | .470 |
| $75 -- $104.9 | 0.439 | −0.37 | 1.25 | .285 | 0.89 | 0.08 | 1.70 | .032 |
| $105 and higher | 0.705 | −0.13 | 1.54 | .098 | 0.91 | 0.07 | 1.75 | .035 |
| Highest education c: | ||||||||
| Bachelor’s degree | 0.99 | 0.07 | 1.90 | .034 | 0.89 | −0.03 | 1.80 | .059 |
| Post-graduate degree | 0.97 | 0.06 | 1.88 | .038 | 0.99 | 0.07 | 1.91 | .034 |
Reference group for gender was men.
Reference group for household income are households with incomes between $15 and $44.9 thousand.
Reference group for highest education was group attaining any level of education below a bachelor’s (4-yr) degree.
Both models adjusted for total dietary energy, respondent’s age and household size.
Both analyses also showed that higher household incomes were associated with progressively higher energy-adjusted diet costs. In the analysis including beverages, the monotonic positive association between income and diet cost was significant for the two highest income groups (P < 0.05), who spent an additional $0.90 per 2000 kcal (8.37 MJ) of dietary energy compared to the reference group.
Both analyses also showed a positive and significant effect of education on energy-adjusted diet cost that was independent of household income. In the analysis excluding beverages, both higher levels of education were associated with significantly higher spending on dietary energy. The two higher education groups spent nearly $1/2000 kcal more than the reference group. The analysis including beverages also revealed higher spending among the more educated groups, with only the most highly-educated group (post-graduate degrees) showing significantly higher energy-adjusted diet cost after adjusting for covariates.
Discussion
Lower-energy-density diets were associated with higher nutrient intakes. In contrast, the more energy-dense diets contained more total fat and saturated fat but were lower in fiber and micronutrients. These present findings that energy density and nutrient density of diets are inversely linked are entirely consistent with past data, based on much larger populations, and representative samples in the United States (10) and in France (34, 35).
The present analyses included an important and sometimes under-appreciated economic variable: food prices and diet costs. Dietary energy was strongly and negatively linked to energy-adjusted diet costs (Table 3). The most energy-dense diets with the lowest fiber and micronutrient content were associated with the lowest energy costs (Table 2). By contrast, higher quality diets were associated with higher energy costs (34, 35). This association between diet quality and energy cost was much stronger for women than for men
Higher quality diets were not only more costly per 2000 kcal but were associated with higher SES of study participants. Education, rather than incomes was the dominant factor. Regression models that adjusted for age and gender revealed that energy cost was positively associated with both education and household incomes but education showed the stronger effect. More highly-educated respondents reported higher quality and therefore more costly diets, independent of household income level. The 2004 Consumer Expenditure Survey (CES) of the Bureau of Labor Statistics reported that total expenditures on food in the US for persons in the highest four income quintiles ranged from $5.04 to $7.70 per person per day. That range of incomes corresponded most closely to those in this study sample (42).
While many prior studies have examined socioeconomic correlates of diet quality (2, 43–45), fewer have included the intermediate variable of diet cost. This was likely due to the lack of appropriate methods for estimating the cost of individual diets. In the US, data on the cost and quality of the diet are collected by different agencies, in different populations, and at different levels of demographic resolution. For example, the CES collects household data on food expenditures for the Consumer Price Index (46) but does not report quantities of foods purchased or collect food consumption data. The USDA’s Continuing Survey of Food Intake of Individuals (CSFII) collected individual-level dietary intake data but had no information on food expenditures. The USDA has been tracking food prices using the AC Nielsen Scantrack program and is in the process of calculating the prices of foods consumed by respondents in the National Health And Nutrition Examination Survey (NHANES), using procedures similar to those outlines in the present study. This new dataset will provide a way to analyze the relation between diet quality and imputed diet cost, following procedures similar to those in the present study.
Published analyses of the relation between diet quality and diet cost, largely based on European populations, also estimated diet costs by merging food record data with national food prices (34, 35). One such study (33) integrated a food price index into an otherwise conventional FFQ to estimate food costs in a population of Spanish adults. In common with Darmon and colleagues (23–32, 34, 35), the methods of Schröder et al (33) relied on national food price data to estimate the food costs of the study population in northeastern Spain.
These observations confirm earlier findings on the positive association between diet quality and energy adjusted diet cost. Higher-cost diets have previously been shown to be lower in energy density (33) and higher in micronutrients and dietary fiber than lower-cost diets (34). Notably, vitamin C intake was strongly and positively associated with energy-adjusted diet cost. Dietary vitamin C is a proxy of fruit and vegetable consumption and an indicator of diet quality (10, 47). Beyond nutrient-by-nutrient indicators of diet quality, studies on a large US food survey database have shown that dietary energy density is inversely associated with other conventional methods of overall diet quality (10).
The present study had some limitations. First, dietary intake and cost estimates were derived from a modified food frequency questionnaire, an instrument that is subject to known biases (48, 49). Second, the present findings were based on a relatively small convenience sample of adults residing in and around Seattle, Washington, US, who do not represent the national population. The present sample was primarily white and highly educated, and while incomes tended to be higher than the national median, they were in line with state and local incomes (50). Third, the ability of this FFQ to accurately estimate costs is limited by the validity of the prices that were used in the database. For each food in the FFQ’s database, $/100g edible portion was computed using local retail prices. The prices selected were always the lowest, non-sale price available for the product from one of 3 largest supermarket chains in the Seattle metropolitan area. Thus, the prices used in estimating diet costs might not adequately reflect the prices paid by individuals. Finally, the present modeling of diet cost was based on the strong assumption that most foods consumed, other than fast foods, were purchased at retail and prepared at home. The validity of the present diet cost estimates for individuals who frequently consumed away-from-home foods and beverages would likely be low. It is worth noting that this limitation is common to epidemiologic studies on dietary exposures, including the Women’s Health Initiative, which excluded women who frequently ate away from home (51).
Despite these limitations, the present estimates of dietary energy density and diet cost were comparable to those obtained from other sources. For example, the present estimates of dietary energy density were 1.48 kcal/g and 1.35 kcal/g for men and women, respectively. Using a similar method, Ledikwe et al. obtained values of 1.91 kcal/g for men and 1.79 kcal/g for women based on the CSFII dataset (41). The discrepancy between the average energy densities reported here and those reported by Ledikwe and colleagues might be due to the differences in socioeconomic characteristics between the present sample and that in the earlier study. Unlike the CSFII, the present sample was composed mainly of white, affluent and highly-educated individuals, who are more likely to consume diets of low energy density (6). More research on larger and more diverse populations will be needed to establish whether the trade-offs between cost and quality of the diet revealed in the present sample also exist in men and in lower-SES groups.
Conclusions
The finding that higher-quality diets were consumed by women of higher SES and more costly per 2000 kcal has implications for epidemiologic studies of diet and chronic disease. Nutritional epidemiology has historically been based on the premise that nutrient exposures are directly linked to health outcomes. However, nutritional status is also intimately linked to SES (52) and the findings reported here raise the possibility that the higher monetary cost of nutritious diets may provide one explanation for these observations. Future studies, based on more representative samples, will be needed to elucidate the connections between diet quality and diet cost across socioeconomic strata. A new and important opportunity for such analyses has been recently made possible with the creation of food prices corresponding to the dietary intake data from NHANES (53).
Acknowledgments
Supported by the National Research Initiative of the USDA Cooperative State Research Education and Extension Service grant 2004-35215-14441 and by a NIDCR fellowship T32 DE07132 to PM
Footnotes
Reprints not available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Marmot M, Wilkinson RG. Social determinants of health. New York, NY: Oxford University Press; 1999. [Google Scholar]
- 2.Boyd-Orr J. Report on a survey of adequacy of diet in relation to income. London, UK: Macmillan and Co; 1937. Food, health and income. [Google Scholar]
- 3.James WP, Nelson M, Ralph A, Leather S. Socioeconomic determinants of health. The contribution of nutrition to inequalities in health. BMJ. 1997;314:1545–9. doi: 10.1136/bmj.314.7093.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leather S, Dowler E. Intake of micronutrients in Britain’s poorest fifth has declined. BMJ. 1997;314:1412. [PMC free article] [PubMed] [Google Scholar]
- 5.Dowler E. Inequalities in diet and physical activity in Europe. Pub Health Nutr. 2001;4:701–9. doi: 10.1079/phn2001160. [DOI] [PubMed] [Google Scholar]
- 6.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–17. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 7.Turrell G, Hewitt B, Patterson C, Oldenburg B. Measuring socio-economic position in dietary research: is choice of socio-economic indicator important? Pub Health Nutr. 2003;6:191–200. doi: 10.1079/PHN2002416. [DOI] [PubMed] [Google Scholar]
- 8.Drewnowski A. The role of energy density. Lipids. 2003;38:109–15. doi: 10.1007/s11745-003-1039-3. [DOI] [PubMed] [Google Scholar]
- 9.Drewnowski A. Energy density, palatability, and satiety: Implications for weight control. Nutr Rev. 1998;56:347–353. doi: 10.1111/j.1753-4887.1998.tb01677.x. [DOI] [PubMed] [Google Scholar]
- 10.Ledikwe JH, Blanck HM, Kettel Khan L, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. Low-energy-density diets are associated with high diet quality in adults in the United States. J Am Diet Assoc. 2006;106:1172–80. doi: 10.1016/j.jada.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Drewnowski A. Concept of a nutritious food: toward a nutrient density score. Am J Clin Nutr. 2006;83:722–3. doi: 10.1093/ajcn/82.4.721. [DOI] [PubMed] [Google Scholar]
- 12.Andrieu E, Darmon N, Drewnowski A. Low-cost diets: more energy, fewer nutrients. Eur J Clin Nutr. 2006;60:434–6. doi: 10.1038/sj.ejcn.1602331. [DOI] [PubMed] [Google Scholar]
- 13.Halkjaer J, Tjonneland A, Thomsen BL, Overvad K, Sorensen TI. Intake of macronutrients as predictors of 5-y changes in waist circumference. Am J Clin Nutr. 2006;84:789–97. doi: 10.1093/ajcn/84.4.789. [DOI] [PubMed] [Google Scholar]
- 14.Guo X, Warden BA, Paeratakul S, Bray GA. Healthy Eating Index and obesity. Eur J Clin Nutr. 2004;58:1580–6. doi: 10.1038/sj.ejcn.1601989. [DOI] [PubMed] [Google Scholar]
- 15.Kant AK, Graubard BI. Energy density of diets reported by American adults: association with food group intake, nutrient intake, and body weight. Int J Obes (Lond) 2005;29:950–6. doi: 10.1038/sj.ijo.0802980. [DOI] [PubMed] [Google Scholar]
- 16.Ledikwe JH, Blanck HM, Kettel Khan L, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. Dietary energy density is associated with energy intake and weight status in US adults. Am J Clin Nutr. 2006;83:1362–8. doi: 10.1093/ajcn/83.6.1362. [DOI] [PubMed] [Google Scholar]
- 17.van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med. 2002;136:201–9. doi: 10.7326/0003-4819-136-3-200202050-00008. [DOI] [PubMed] [Google Scholar]
- 18.Fung TT, Rimm EB, Spiegelman D, Rifai N, Tofler GH, Willett WC, Hu FB. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73:61–7. doi: 10.1093/ajcn/73.1.61. [DOI] [PubMed] [Google Scholar]
- 19.McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, Spiegelman D, Hunter DJ, Colditz GA, Willett WC. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76:1261–71. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 20.Hung HC, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Colditz GA, Rosner B, Spiegelman D, Willett WC. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96:1577–84. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 21.Fung TT, Hu FB, McCullough ML, Newby PK, Willett WC, Holmes MD. Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women. J Nutr. 2006;136:466–72. doi: 10.1093/jn/136.2.466. [DOI] [PubMed] [Google Scholar]
- 22.Mendoza JA, Drewnowski A, Christakis DA. Dietary energy density is associated with obesity and the metabolic syndrome in U.S. adults. Diabetes Care. 2007;30:974–9. doi: 10.2337/dc06-2188. [DOI] [PubMed] [Google Scholar]
- 23.Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc. 2005;105:S98–103. doi: 10.1016/j.jada.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 24.World Cancer Research Fund International. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. [Accessed 2 November 2007];Second Expert Report. Available at: http://www.dietandcancerreport.org/?p=ER.
- 25.World Health Organization. Tech Rep Ser. 916. Geneva: World Health Org; 2003. Diet, Nutrition and the Prevention of Chronic Diseases; pp. i–viii.pp. 1–149. backcover. [PubMed] [Google Scholar]
- 26.Williams F. Mon Labor Rev. Washington, D.C: Apr, 1936. Food consumption at different economic levels. [Google Scholar]
- 27.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82:265S–273S. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- 28.Drewnowski A. Obesity and the food environment: dietary energy density and diet costs. Am J Prev Med. 2004;27:154–62. doi: 10.1016/j.amepre.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 29.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 30.Darmon N, Briend A, Drewnowski A. Energy-dense diets are associated with lower diet costs: a community study of French adults. Pub Health Nutr. 2004;7:21–7. doi: 10.1079/phn2003512. [DOI] [PubMed] [Google Scholar]
- 31.Darmon N, Ferguson E, Briend A. Do economic constraints encourage the selection of energy dense diets? Appetite. 2003;41:315–22. doi: 10.1016/s0195-6663(03)00113-2. [DOI] [PubMed] [Google Scholar]
- 32.Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr. 2002;132:3764–71. doi: 10.1093/jn/132.12.3764. [DOI] [PubMed] [Google Scholar]
- 33.Schröder H, Marrugat J, Covas MI. High monetary costs of dietary patterns associated with lower body mass index: a population-based study. Int J Obes (Lond) 2006;30:1574–79. doi: 10.1038/sj.ijo.0803308. [DOI] [PubMed] [Google Scholar]
- 34.Andrieu E, Darmon N, Drewnowski A. Low-cost diets: more energy, fewer nutrients. Eur J Clin Nutr. 2006;60:434–6. doi: 10.1038/sj.ejcn.1602331. [DOI] [PubMed] [Google Scholar]
- 35.Maillot M, Darmon N, Vieux F, Drewnowski A. Low energy density and high nutritional quality are each associated with higher diet costs in French adults. Am J Clin Nutr. 2007;86:690–6. doi: 10.1093/ajcn/86.3.690. [DOI] [PubMed] [Google Scholar]
- 36.Consumer Price Index. Department of Labor, Bureau of Labor Statistics; Washington, DC: [accessed February, 2007]. Available at: http://data.bls.gov/PDQ/outside.jsp?survey=cu. [Google Scholar]
- 37.Monsivais P, Drewnowski A. The rising cost of low energy-density foods. J Am Diet Assoc. 2007;107:2071–6. doi: 10.1016/j.jada.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–88. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 39.Kristal AR, Feng Z, Coates RJ, Oberman A, George V. Associations of race/ethnicity, education, and dietary intervention with the validity and reliability of a food frequency questionnaire: the Women’s Health Trial Feasibility Study in Minority Populations. Am J Epidemiol. 1997;146:856–69. doi: 10.1093/oxfordjournals.aje.a009203. [DOI] [PubMed] [Google Scholar]
- 40.Neuhouser ML, Kristal AR, McLerran D, Patterson RE, Atkinson J. Validity of short food frequency questionnaires used in cancer chemoprevention trials: results from the Prostate Cancer Prevention Trial. Cancer Epidemiol Biomarkers Prev. 1999;8:721–5. [PubMed] [Google Scholar]
- 41.Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr. 2005;135:273–8. doi: 10.1093/jn/135.2.273. [DOI] [PubMed] [Google Scholar]
- 42.Consumer Expenditures in 2004, Report 992. United States Department of Labor, Bureau of Labor Statistics; Washington, DC: Apr, 2006. [accessed 21 November 2007]. Available at: http://www.bls.gov/cex/csxann04.pdf. [Google Scholar]
- 43.Davis CG. Linkages between socioeconomic characteristics, food expenditure patterns and nutritional status of low income households: A critical review. Am J Agr Econ. 1982;64:1017–25. [Google Scholar]
- 44.Morgan KJ. Socioeconomic factors affecting dietary status: An Appraisal. Am J Agr Econ. 1986;68:1240–6. [Google Scholar]
- 45.McDowell DR, Allen-Smith JE, McLean-Meyinsse PE. Food expenditures and socioeconomic characteristics: Focus on income class. Am J Agr Econ. 1997;79:1444–51. [Google Scholar]
- 46.United States Department of Labor, Bureau of Labor Statistics. [accessed 21 November 2007];Consumer Price Indexes Program. Available at: http://www.bls.gov/cpi/home.htm.
- 47.Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104:615–35. doi: 10.1016/j.jada.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 48.Drewnowski A. Diet image: a new perspective on the food-frequency questionnaire. Nutr Rev. 2001;59:370–2. doi: 10.1111/j.1753-4887.2001.tb06964.x. [DOI] [PubMed] [Google Scholar]
- 49.Kristal AR, Peters U, Potter JD. Is It Time to Abandon the Food Frequency Questionnaire? Cancer Epidemiol Biomarkers Prev. 2005;14:2826–8. doi: 10.1158/1055-9965.EPI-12-ED1. [DOI] [PubMed] [Google Scholar]
- 50.Median Household Income Estimates by County: 1989 to 2007. Office of Financial Management; [Accessed June 10, 2008]. Available at: http://www.ofm.wa.gov/economy/hhinc/default.asp. [Google Scholar]
- 51.Beresford SA, Johnson KC, Ritenbaugh C, et al. Low-fat dietary pattern and risk of colorectal cancer: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:643–54. doi: 10.1001/jama.295.6.643. [DOI] [PubMed] [Google Scholar]
- 52.Lawlor DA, Davey Smith G, Kundu D, Bruckdorfer KR, Ebrahim S. Those confounded vitamins: what can we learn from the differences between observational versus randomised trial evidence? Lancet. 2004;22:1724–7. doi: 10.1016/S0140-6736(04)16260-0. [DOI] [PubMed] [Google Scholar]
- 53.Carlson A, Lino M, Juan WY, et al. Development of the CNPP Prices Database. United States Department of Agriculture; May, 2008. [Accessed June 10, 2008]. Report. Available at: http://www.cnpp.usda.gov/Publications/FoodPlans/MiscPubs/PricesDatabaseReport.pdf. [Google Scholar]


