Abstract
OBJECTIVES
To examine whether control-oriented strategies buffer effects of functional difficulties on depressive symptoms over time in older African-American and white adults with disability.
DESIGN
Community-based, prospective study.
SETTING
Baseline and 12-month data from a randomized trial.
PARTICIPANTS
One hundred twenty-nine African-American and 151 white older adults with 12-month data from 319 participants in the trial.
MEASUREMENTS
Data were obtained for functional difficulties, the extent that respondents reported using control (cognitive and behavioral) strategies to enhance and maintain independence, and baseline and 12-month depressive symptoms (Center for Epidemiologic Studies Depression Scale; CES-D).
RESULTS
African Americans reported greater baseline functional difficulty (P = .009), fewer depressive symptoms (P = .002) and higher control strategy use (P = .001) than whites. Functional difficulty was associated with depressive symptoms for both groups at baseline and 12 months. Living alone for whites and low spirituality for African Americans predicted higher 12-month depressive symptom scores. African Americans with baseline functional difficulty and high strategy use had lower 12-month depression than those with similar difficulty levels but low strategy use (P = .04 for interaction), representing a 28.5-point CES-D score differential. Control strategies did not buffer the function–depression relationship over time for whites.
CONCLUSION
Control-oriented strategies moderated the experience of depressive symptomatology over time for African Americans with disability but not for whites. This may explain the paradox of greater functional disparities but less reported emotional distress in African Americans than whites. Results suggest that the use and benefits of adaptive resources to attain functional goals and determinants of depression differ by race. Depression prevention programs should be modified to be suitable for different cultural groups
Keywords: disability, aging in place, late-life mental disorder
Depressive symptomatology is a common mental health problem in old age that is strongly associated with difficulty performing fundamental life tasks. The association between depressive symptoms and functional difficulties is well documented and may be reciprocal, such that each may be a risk factor for the other,1–4 although it is unclear whether the functional disability–depression association differs for African Americans and whites and whether there are race-specific mechanisms that protect against depression for functionally compromised older adults.5,6 Identifying adaptive strategies that moderate the effect of functional limitations on depressed mood for different groups is important to inform clinical guidelines and the development and testing of effective interventions to address both.7,8
Understanding the function–depression relationship is also important in view of existing health disparities.9 Research shows that older African Americans have poorer physical function and more disabling health conditions than whites, which places them at greater risk for minor and major depression.10 However, findings from studies on racial differences in mental health outcomes are inconsistent.11 Some studies report higher depressive symptoms in African Americans than whites, whereas other studies report similar or lower rates of distress even when African Americans with higher levels of physical impairment are compared with whites.12,13 Thus, it remains unclear whether there are racial disparities in depressive symptoms for functionally vulnerable older people; nor is it clear as to the mechanisms that may explain why some functionally impaired African Americans report less distress than whites with similar levels of disability.
The purpose of this study was twofold: to assess differences in depressive symptoms and functional disability levels between community-dwelling, inner-city African-American and white older adults and to examine whether adaptive resources such as the use of control-oriented strategies protect against deleterious effects of functional disability on depressed mood over time for each group. The study draws upon the Life Span Theory of Control, which suggests that threats to or actual losses in the ability to control important outcomes such as performing self-care may activate individuals to use strategies to buffer threats and losses.14,15 To the extent that control-oriented behavioral and cognitive strategies are used that are directed toward attaining functional goals, threats to or actual losses of control may be minimized and positive affect enhanced. There is some evidence to support the psychological advantage afforded by control-oriented strategies to manage threats imposed by acute health problems,16 although their protective effect against threats imposed by functional decline in African Americans and whites has not been examined. In this study, it was hypothesized that the amount of engagement in control-oriented strategies to attain functional goals would moderate depressive affective responses to functional loss over time. It was reasoned that efforts to maintain functionality and engagement in meaningful life activities is a highly desired goal that physical decline brought on by chronic health conditions threatens, although there was no specific hypothesis as to whether there would be differential use and benefit of strategies for each racial group. Participants for this study were enrolled in a randomized trial of a home-based occupational and physical therapy intervention that resulted in reduced functional difficulties and fear of falling at 6 months and risk of mortality at 12 months.17,18 The authors’ interest in the present study was about the specific role of control-oriented strategies as a moderator of functional disability and depressive symptoms using descriptive longitudinal analyses and after controlling for group assignment.
METHODS
Sample and Recruitment Procedures
To participate in the randomized trial, individuals had to be ambulatory, community-dwelling, aged 70 and older, English speaking, cognitively intact (Mini-Mental State Examination (MMSE) score >24;19 and experiencing functional difficulties.20 As described elsewhere,17 recruitment occurred between 2000 and 2003 from social service agencies and media announcements. Individuals determined eligible according to a telephone screen were interviewed at home after signing a consent form approved by the Thomas Jefferson University institutional review board. All participants were randomized to experimental or control groups and reassessed at 6 and 12 months. For this study, baseline and 12-month data on African-American and white participants who were available for the 12-month follow-up were used. Of 319 who were initially enrolled, 145 were African American and 168 were white. At 12 months, 285 were available for follow-up: 129 African Americans and 151 whites.
Measures
Background characteristics included age, sex, education (< high school, high school, >high school), living arrangement (alone, with others), and financial difficulty (0–4, with higher scores representing greater difficulty). Number of common health conditions, depression medication use, and three factors associated with depressive symptoms in previous research (social support, spirituality, and personal agency) were also considered.
For social support, an 8-item measure of network and satisfaction with received support was used.21 Scores represented summed responses, with higher scores indicating greater social support received.
Measures for spirituality and personal agency represented two distinct dimensions of the Valuation of Life scale that were factor-analytically derived.22,23 The Spirituality subscale consisted of eight items (e.g., “My life is guided by strong religious or ethical beliefs”), and the Personal Agency subscale consisted of five items (e.g., “I feel able to accomplish my life goals”). For each item, participants rated agreement along a 5-point scale (1 = disagree strongly to 5 = agree very strongly), with higher scores indicating greater spirituality and goal achievement.
Functional difficulty (disability) was measured using 22 activities; six activities of daily living (ADLs; dressing above and below the waist, grooming, bathing or showering, toileting, and feeding), six instrumental activities of daily living (IADLs; light housework, errands and shopping, preparing meals, managing money, telephone use, taking medications), six mobility tasks (getting in/out of bed, walking indoors, walking one block, climbing one flight of stairs, getting in and out of chair, getting in and out of bed), and four basic activities (raising arm above head, gripping with hands, bending and stooping, opening containers).24 For each task, participants rated difficulty in the previous month along a 5-point scale (1 = no difficulty to 5 = unable to do because of health problems). An overall functional difficulty index score was derived by computing average difficulty level across items, with higher scores indicating greater difficulty.
Control-oriented strategy use was measured using an investigator-developed 8-item Likert-type measure (Table 1) modeled after a health engagement scale developed previously.16 The control-oriented strategy use measure assesses the extent to which respondents endorsed cognitive and behavioral strategies designed to enhance and maintain functional independence. Participants rated the extent to which each statement was true along a 4-point scale (1 = not at all true to 4 = very much true). An index was derived by averaging responses across the eight items, with higher mean scores indicating greater strategy use (Cronbach alpha = 0.69).
Table 1.
Control Strategy Use According to Race (N = 280)
| Control Strategy | African Americans (n = 129) | Whites (n = 151) | Z | P-Value |
|---|---|---|---|---|
| Mean ± SD) | ||||
| I try to learn as much as possible about ways of handling my physical health problems | 3.7 ± 0.6 | 3.4 ± 0.8 | −3.0 | .003 |
| I try to make changes to my home to help me stay independent | 3.0 ± 1.1 | 2.7 ± 1.2* | −2.3 | .02 |
| I try to do things to make myself feel safe in my daily activities at home | 3.4 ± 0.9 | 3.1 ± 1.0* | −2.6 | .009 |
| I pace myself so I do not get too tired | 3.3 ± 1.0 | 2.9 ± 1.1 | −3.0 | .003 |
| I am willing to use special equipment such as grab bars or utility aids to help me stay independent | 3.7 ± 0.6 | 3.5 ± 0.8* | −2.4 | .02 |
| I am willing to ask others for help if I need it | 3.2 ± 1.0 | 3.0 ± 1.0 | −1.4 | .17 |
| When I decide to do something about a health or physical problem, I’m confident I’ll succeed | 3.2 ± 0.9 | 3.0 ± 1.0† | −2.2 | .03 |
| I think about how important it is to stay healthy | 3.8 ± 0.5 | 3.7 ± 0.7 | −1.1 | .27 |
n = 150.
n = 149.
To measure depressive symptoms, the 20-item Center for Epidemiologic Studies Depression Scale (CES-D), which provides a cutoff score (≥16) to identify individuals at risk for clinical depression, was used.25 Participants rated how often they experienced symptoms during the previous week (0 = < 1 day to 3 = 5–7 days). Scores represent summed responses across 20 items, with higher scores indicating greater depressive symptomatology.
Data Analysis
To compare sociodemographics, covariates, functional difficulty, control strategy use, and depressive symptom differences between African Americans and whites at baseline, Wilcoxon rank sum tests were used for continuous variables and chi-square tests for categorical variables. The distribution of predictor and outcome measures and non-parametric (Spearman correlation coefficient; rs) intercorrelations of functional difficulty, control strategies, and depressive symptom scores were examined. Next, a stepwise (step down) regression was conducted to identify potential demographic factors or factor interactions that covary with depressive affect. Using this procedure, age, sex, living arrangement, and education were selected. Other covariates were included based on previous research showing a strong association with depressive symptoms (financial difficulty, spirituality, social support, personal agency).
The relationship between functional difficulty and CES-D was examined at baseline and 12 months using nonparametric correlations in African-American and white samples separately. These relationships were then examined in a cross-sectional multivariate model to determine whether baseline functional difficulty was associated with baseline depressive symptomatology after controlling for sociodemographics and other factors using a four-block hierarchical regression. The dependent variable was baseline CES-D score, the first block included baseline sociodemographics (age, sex, living arrangement, education, financial difficulty, and antidepressant medications); the second block included baseline functional difficulty; the third block included baseline control strategy use, social support, spirituality, and personal agency; and the fourth block included the interaction term functional difficulty by control strategy use.
Next, the primary hypothesis that baseline control-oriented strategy use moderated the relationship between baseline functional disability and depressive symptomatology over time was tested using separate hierarchical multiple regression analyses for each racial group.26,27 For each regression, five blocks were used in which the dependent variable was 12-month CES-D score. The first block included treatment assignment (experimental vs control group) and sociodemographics (age, sex, living arrangement, education, financial difficulty, and antidepressant medications); the second block included baseline CES-D score to operationalize change in depressive symptomatology over time; the third block included baseline functional difficulty; and baseline control strategy use, social support, spirituality and personal agency were entered in the fourth block. The final block included the interaction term baseline functional difficulty by baseline control strategy use. All analyses were conducted using SPSS version 14.0 with level of significance set at .05 (SPSS Inc., Chicago, IL).
RESULTS
In this sample, there was a higher proportion of African-American women, and African Americans were younger and less educated and had greater financial difficulty, better social support, and stronger spirituality and personal agency than whites. There was a higher prevalence of diabetes mellitus, heart disease, and stroke in African Americans and a higher prevalence of cancer in whites. Also, 7.8% of African Americans reported taking antidepressant medication, compared with 19.9% of whites (Table 2).
Table 2.
Characteristics, Baseline Predictors, and Baseline and 12-Month Depressive Symptomatology According to Race (N = 280)
| Characteristics, Baseline Predictors, and Baseline and 12-Month Depressive Symptomatology | African American (n = 129) | White (n = 151) | Chi-Square | Z | P-Value |
|---|---|---|---|---|---|
| Characteristic | |||||
| Age, mean ± SD | 77.4 ± 4.8 | 80.2 ± 6.4 | −3.6 | .001 | |
| Sex, % | 5.1 | .02 | |||
| Male | 11.6 | 21.9 | |||
| Female | 88.4 | 78.1 | |||
| Married, % | 11.6 | 23.8 | 6.7 | .008 | |
| Living alone, % | 61.2 | 67.5 | 1.2 | .27 | |
| Education, % | 10.6 | .005 | |||
| <HS | 40.3 | 22.5 | |||
| HS | 29.5 | 35.1 | |||
| >HS | 30.2 | 42.4 | |||
| Financial difficulty, mean ± SD | 2.7 ± 1.0 | 2.3 ± 1.1 | −3.5 | .001 | |
| Health conditions | |||||
| Number, mean ± SD | 7.1 ± 2.7 | 7.1 ± 2.8 | −0.1 | .89 | |
| Diabetes mellitus, % | 31.3 | 15.2 | 10.2 | .001 | |
| Heart disease, % | 44.2 | 35.3 | 2.3 | .13 | |
| Stroke, % | 12.5 | 8.7 | 1.1 | .30 | |
| Cancer, % | 3.1 | 13.9 | 9.9 | .002 | |
| Baseline predictor | |||||
| Antidepressant medications, % | 7.8 | 19.9 | 8.3 | .004 | |
| Functional difficulty, mean ± SD | 2.3 ± 0.6 | 2.1 ± 0.5 | −2.3 | .02 | |
| Social support, mean ± SD | 22.0 ± 4.7 | 19.1 ± 6.1 | −4.0 | .001 | |
| Spirituality, mean ± SD | 4.3 ± 0.5 | 3.8 ± 0.7 | −6.4 | .001 | |
| Personal agency, mean ± SD | 19.4 ± 3.3 | 17.6 ± 3.5 | −4.2 | .001 | |
| Control strategy use, mean ± SD | 3.4 ± 0.4 | 3.2 ± 0.5 | −3.9 | .001 | |
| Center for Epidemiologic Studies | |||||
| Depression Scale score | |||||
| Baseline | |||||
| Mean ± SD | 12.2 ± 9.9 | 16.6 ± 11.3 | −3.4 | .001 | |
| ≥16, % | 31.8 | 49.0 | |||
| 12-month | |||||
| Mean ± SD | 11.4 ± 9.4 | 15.8 ± 11.2 | −3.5 | .001 | |
| ≥16, % | 27.1 | 44.3 | |||
SD = standard deviation; HS = high school.
Baseline and 12-Month Functional Difficulty Levels
At baseline, African Americans had slightly greater functional difficulty than whites (Table 2). At 12 months, the unadjusted mean values for functional difficulties were slightly lower than at baseline for both groups, but the between-group difference at 12 months was not statistically significant. Nevertheless, for African Americans, decline in difficulty level from baseline to 12 months was statistically significant (z = −5.42, P < .001), suggesting slightly less disability over time, whereas this was not true for whites (z = −1.75, P = .08). Previous work had revealed no differential treatment effects by race, thus suggesting that the intervention does not account for this slight decline in African Americans.28
Baseline and 12-Month Depressive Symptom Scores
At baseline, African Americans reported statistically significantly fewer depressive symptoms than whites, although a substantial proportion of individuals in each group had CES-D scores of 16 or higher, with 31.8% of African Americans and 49.0% whites scoring in the depressed range. At 12 months, mean depressive scores for both groups declined slightly from baseline (but not significantly), although African Americans continued to report statistically significantly fewer symptoms than whites at 12 months (Table 2).
African Americans used each control strategy slightly more than whites, with six of eight items reaching statistical significance (Table 1).
Functional Difficulty and Depressive Symptoms: Cross-Sectional Results
For African Americans, positive correlations were found between functional difficulty and depressive symptoms at baseline (rs = 0.43, P = .001) and 12 months (rs = 0.44, P = .001) such that greater difficulty at each time point was associated with higher depressive symptoms at baseline and 12 months. In multivariate analysis, after controlling for sociodemographics and other covariates, baseline functional difficulty remained significantly associated with baseline CES-D. Also, low spirituality at baseline was a statistically significant correlate of higher depressive scores for African Americans. The interaction between baseline difficulty and control strategy use was not significant (Table 3).
Table 3.
Cross-Sectional Regression Analyses Predicting Depressive Symptomatology at Baseline According to Sociodemographic Characteristics, Spirituality, Personal Agency, and Functional Difficulty (N = 280)
| Baseline Predictors | Baseline Center for Epidemiological Studies Depression Scale Score | |||||
|---|---|---|---|---|---|---|
| African Americans (n = 129) | Whites (n = 151) | |||||
| B (Standard Error) 95% Confidence Interval | ||||||
| Age | 0.2 | (0.2) | −0.08–0.54 | −0.2 | (0.1) | −0.38–0.07 |
| Sex | 3.3 | (2.4) | −1.50–8.02 | −0.4 | (1.8) | −4.00–3.11 |
| Living arrangement | −0.1 | (1.6) | −3.24–3.03 | −4.6** | (1.7) | − 7.83 to −1.43 |
| Education | −1.1 | (0.9) | −2.91–0.78 | −0.8 | (0.9) | −2.57–0.96 |
| Financial difficulty | 0.8 | (0.8) | −0.79–2.27 | 1.6* | (0.7) | 0.17–2.93 |
| Antidepressants | 1.3 | (3.0) | −4.61–7.15 | 3.3 | (1.8) | 0.33–6.84 |
| Functional difficulty | 5.3*** | (1.4) | 2.43–8.11 | 3.7* | (1.5) | 0.77–6.62 |
| Social support | 0.07 | (0.2) | −0.24–0.37 | −0.2 | (0.1) | −0.47–0.01 |
| Control strategy use | −1.1 | (1.8) | −4.68–2.39 | −0.5 | (1.4) | −3.24–2.16 |
| Spirituality | −5.0** | (1.7) | −8.33 to −1.56 | −5.6*** | (1.4) | − 8.33 to −2.90 |
| Personal agency | −.3 | (0.3) | −0.82–0.25 | −0.5 | (0.3) | −1.01–0.01 |
| Functional difficulty by control strategy use | −3.2† | (3.2) | −9.63–3.19 | −3.0‡ | (2.3) | −7.62–1.62 |
Note: Unstandardized coefficients are shown for all variables for block 3 before entering the interaction of functional difficulty by control strategy use into the model.
P<* .05, ** .01, *** .001.
A similar pattern was found for whites. Positive correlations were found between functional difficulty at each time point and depressive symptoms at baseline (rs = 0.36, P = .001) and 12 months (rs = 0.46, P = .001), with greater difficulty associated with higher symptomatology at both time points. In multivariate cross-sectional analysis, after controlling for sociodemographics and other covariates, baseline functional difficulty remained predictive of baseline CES-D. Other statistically significant correlates for whites included living alone and financial difficulty. As with African Americans, low spirituality was associated with higher depression scores at baseline; the interaction between functional difficulty and strategy use was not significant at baseline (Table 3).
Functional Difficulty and Depressive Symptoms: Longitudinal Results
Next, the primary study aim was examined: whether control-oriented strategies moderated the relationship between baseline functional disability and change in depressive symptomatology for African Americans and whites after controlling for baseline covariates and treatment assignment.
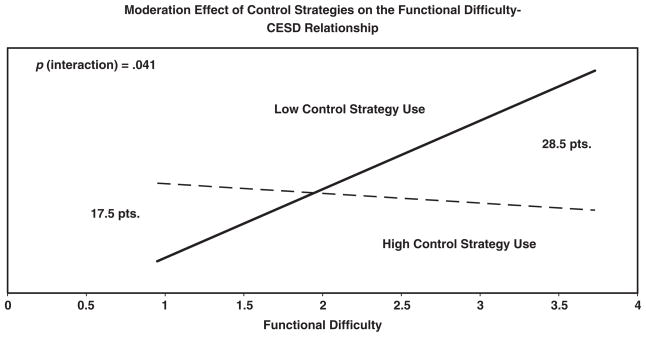
For African Americans, higher baseline CES-D scores and low spirituality were significant predictors of 12-month depression scores (Table 4). A significant interaction effect was found (baseline functional difficulty by baseline control strategy use) for African Americans (P = .04). Higher amounts of baseline control strategy use predicted lower levels of depressive symptoms over time for those with greater baseline functional difficulty levels. Figure 1 shows the interaction. In Figure 1, the solid line, “Low Strategy Use,” shows the estimated relationship between CES-D score and functional difficulty for African Americans with the lowest value of strategy use. The dotted line, “High Strategy Use,” shows the same relationship but for the highest value of strategy use. For individuals with intermediate values of strategy use, the line would be intermediate between the two shown. The horizontal location for each line is the range of functional difficulty. The vertical location for each pair of lines (but not their relationship) varies with covariate values, and so no vertical scale for CES-D score is shown. This is because the actual vertical location of the lines on the CES-D scale is dependent on the values of the other covariates in the analysis. The value of the vertical axis is set arbitrarily for the combination of low control-strategy use and low difficulty (1.0). Thus, the graph correctly represents the differences in CES-D scores between high and low strategy users along functional difficulty levels but not the actual CES-D score.
Table 4.
Moderation Effect of Control-Oriented Strategy Use According to Race at 12 Months (N = 280)
| Baseline Predictor | African Americans (n = 129) | Whites (n = 151) | ||||
|---|---|---|---|---|---|---|
| B (Standard Error) 95% Confidence Interval | ||||||
| Treatment condition | −0.2 | (1.4) | −3.00–2.65 | −0.3 | (1.3) | −2.87–2.36 |
| Age | 0.1 | (0.2) | −0.16–0.43 | −0.1 | (0.1) | −0.29–0.15 |
| Sex | 1.6 | (2.3) | −2.99–6.19 | 0.8 | (1.7) | −2.54–4.14 |
| Living arrangement | 0.9 | (1.5) | −2.12–3.86 | −4.5** | (1.6) | −7.61 to −1.36 |
| Education | −0.4 | (0.9) | −2.19–1.36 | −1.4 | (0.8) | −3.11–0.22 |
| Financial difficulty | 1.1 | (0.7) | −0.32–2.61 | 0.5 | (0.7) | −0.80–1.84 |
| Antidepressants | −1.6 | (2.9) | −7.34–4.07 | −1.1 | (1.7) | −4.50–2.28 |
| CES-D | 0.4*** | (0.1) | 0.23–0.59 | 0.6*** | (0.1) | 0.47–0.79 |
| Functional difficulty | 1.6 | (1.5) | −1.33–4.45 | −0.2 | (1.4) | −3.01–2.69 |
| Social support | 0.1 | (0.2) | −0.23–0.37 | −0.2 | (0.1) | −0.47–0.02 |
| Control strategy use | −1.6 | (1.7) | −5.02–1.79 | 0.4 | (1.3) | −2.17–3.00 |
| Spirituality | −4.6** | (1.7) | −7.93 to −1.22 | −0.6 | (1.4) | −3.30–2.08 |
| Personal agency | 0.4 | (0.3) | −0.10–0.93 | 0.2 | (0.3) | −0.30–0.68 |
| Functional difficulty by control strategy use | −6.4*† | (3.1) | −12.50 to −0.27 | 2.6‡ | (2.4) | −2.08–7.28 |
Note: Dependent variable was the CES-D (Center for Epidemiological Studies Depression Scale) score at 12 months. Unstandardized coefficients are shown for all variables for block 4 before entering the interaction of functional difficulty by control strategy use into the model.
Coefficient of determination (final block) = †0.40, ‡0.58.
P<*.05, **.01, ***.001.
Figure 1.
Moderation effect of control strategies for African-American participants. For the combination of low control strategy use and low difficulty (1.0), the value of the vertical axis is set arbitrarily. This is due to the actual vertical location of scores on the Center for Epidemiologic Studies Depression Scale (CES-D) being dependent on the values of the other covariates (treatment assignment, sociodemographics, baseline CES-D score, functional difficulty, social support, control strategy use, spirituality, and personal agency) in the analysis. The graph correctly represents differences in CES-D scores between high and low strategy users but not an actual CES-D value.
For persons with no functional difficulty (score = 1.0), there was a 17.5-point difference on 12-month CES-D scores between high and low strategy users. However, the differential in 12-month CES-D scores between high and low strategy users increased by 11 points, to 28.5 points, for those with high difficulty scores (≥3.5). That is, high strategy users with greater functional difficulties at baseline experienced fewer depressive symptoms over time. On the CES-D, a score of 16 or greater is considered indicative of depressive symptoms. Thus, the differential in 12-month CES-D scores between high and low strategy users for individuals experiencing greater functional difficulty suggests an important clinical difference.
For whites, living alone and higher baseline CES-D scores predicted 12-month depressive symptoms, although control strategy use at baseline did not significantly moderate the relationship between baseline functional difficulties and change in depressive symptoms at 12 months (P = .27).
DISCUSSION
This study compares the prevalence of functional difficulty and depressive symptoms in African-American and white community-dwelling, inner-city older adults with disability and whether control-oriented strategy use buffered depressive symptoms over time for each group. In keeping with the Life Span Theory of Control, it was reasoned that declines in the ability to engage in meaningful daily activities might activate older adults to engage in strategies that reduce the threat to or loss of control. Use of strategies such as seeking information, modifying the home, or cognitive reframing may contribute to emotional well-being by enabling individuals to compensate for limitations in such a way as to continue participation in valued self-care activities and, hence, the attainment of functional goals.
It was found that this group of older African-American adults had slightly higher functional difficulty and poorer health than whites but lower depressive symptoms at baseline. Over time, African Americans reported a slight decline in functional disability and continued to report fewer depressive symptoms than whites. Consistent with previous research, it was also found that the African-American group reported greater social support, spirituality, personal agency, and use of control-oriented strategies than whites at baseline. For both groups, cross-sectional multivariate models revealed that functional difficulty was associated with depressive symptoms. That is, functional difficulties had a similar deleterious effect on the mental health of both groups.
The findings from this study support the main hypothesis that engagement in control-oriented strategies designed to address functional limitations reduces the negative effect of functional difficulty on affective responses in later life, but this was found to be the case only for the African-American sample. The data suggest that African Americans used strategies representing active attempts to maintain functional capacity slightly more frequently than whites and that, over time, these strategies protected against psychiatric morbidity associated with difficulty performing fundamental life activities. Although the difference between African Americans and whites was not large, it was consistent across all items, with African Americans using control strategies slightly more than whites. Also, the rate of functional decline in African Americans was slightly slower over time than for whites. Although improvement from baseline to 12 months for African Americans was small, it was statistically significant and may be clinically important in view of research showing that even small functional gains result in life quality improvements.29,30 It is unclear why African Americans show functional improvement. It may be due to their use of control strategies, which may minimize functional decline. It is also important to note that, for African Americans, there was a 17.5-point differential in CES-D scores between high and low strategy users for those with no functional decline.
Why do older African Americans with functional limitations use control-oriented strategies more than whites, and why does use afford greater psychological benefit for this group? Qualitative research suggests that older African Americans place a high value on independent functioning, being in control, and overcoming distress by employing strategies that demonstrate resilience to hardships rather than complaining or withdrawal.31 Also, African Americans had higher levels of disability and probably for longer duration and thus may have had more experience managing functional challenges. Thus, one explanation may be that control strategies reflect a form of resilience in the face of adversity and resonate with coping approaches that are consistent with the cultural expressions and life experiences of this group. In focus groups with 60 older African-American men and women, a range of strategies used to confront adversity was found, including keeping busy, remaining engaged in activities, pushing oneself to do things, and staying connected to family and friends, all reflecting attempts to control behavior-event contingencies. In contrast, older whites may not have the same level of cultural exposure to or experience with using behavioral and cognitive control mechanisms in the face of adversity and may therefore require skilled intervention for their successful adoption. The findings from the current study may help explain the paradox found in this and other studies regarding the presence of functional disparities between African Americans and whites but less reported emotional distress by African Americans. These findings add incrementally to research that deconstructs race differences by identifying the underlying causal factors rooted in sociohistorical, cultural, and economic contextual differences between groups.32,33
Several clinical implications can be derived. Although African Americans reported fewer depressive symptoms than whites, scores for both groups were high, with close to one-third of African Americans and almost half of whites scoring 16 or greater on the CES-D, the clinical cutoff for evidence of depressive symptoms. Thus, a substantial number of community-dwelling older adults with functional difficulties were untreated for their emotional distress. The rate of depressive symptoms was much higher for this study group than has previously been reported.34,35
Of most importance is that control strategy use by older African Americans with disability resulted in a 28.5-point score differential on the CES-D over time between those with low and high strategy use, a clinically meaningful difference. This suggests that teaching older adults to use control strategies may represent an important preventive mental health measure that should occur at onset of even the slightest functional change. Previous research shows that older people can learn to use control strategies through a skilled intervention.17 A related point is the need to develop and test approaches to treat the dual burden of functional decline and depression simultaneously.3 Combining treatments such as pharmacological, psychosocial, and training in control strategy use might be effective.
Finally, the findings also show that determinants of depressive symptoms over time differ according to race. Although living alone predicted decline in depressive symptoms over time for whites, only low spirituality did so for African Americans after controlling for baseline CES-D scores and other covariates. Consequently, depression prevention programs may need to be modified to be suitable for different cultural groups to address the unique contributors to depressive symptoms and differential coping preferences.
One limitation of this study is that the control-oriented strategy use scale is investigator developed and has not been evaluated fully for its psychometric properties. Although it had adequate internal consistency, future research needs to assure its construct validity.
CONCLUSION
In summation, consistent with previous research, the current study shows that disability is associated with important psychological processes for older African Americans and whites. Older African Americans with functional disability used control-oriented strategies with greater frequency than whites and appeared to manage the associated negative consequences of physical decline such that, over time, there was less functional disability and lower depressive symptoms. The greater the use of control-oriented strategies by African Americans, the more likely that successful coping and positive mental health will occur for this group. Future research needs to explore why whites do not derive similar benefits, what factors temper their depressive response to functional limitations, and why some whites and African Americans are more successful than others at adapting control-oriented strategies to maintain functional competence.
Acknowledgments
The authors wish to acknowledge the project coordination efforts of Sandy Schinfeld, MPH, and Laraine Winter, PhD. We thank the interviewing staff for their efforts and the study participants for their involvement.
Financial Disclosure: Research reported in this paper was supported in part by National Institute on Aging Grant R01 AG13687 and National Institute of Mental Health Grant R24 MH074779.
Sponsor’s Role: None.
Footnotes
Author Contributions: L. Gitlin: principal investigator, developed study concept and design, and oversaw scientific integrity and interpretation of data; primary responsibility for preparation of manuscript. W. Hauck: statistician, oversaw statistical analyses and integrity of data interpretation. M. Dennis: conducted data analysis and constructed manuscript tables. R. Schulz: served as theoretical consultant on Life Span Theory of Control and helped with analyses and interpretation.
References
- 1.Lenze EJ, Schulz R, Matire LM, et al. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the Cardiovascular Health Study. J Am Geriatr Soc. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- 2.Lenze EJ, Rogers JC, Martire L, et al. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- 3.Callahan CM, Kroenke K, Counsell SR, et al. Treatment of depression improves physical functioning in older adults. Am J Geriatr Psychiatry. 2005;53:367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 4.Lin EHB, Katon W, Von Korff M, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: A randomized controlled trial. JAMA. 2003;12:428–434. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 5.Mills TL, Alea NL, Cheong JA. Differences in the indicators of depressive symptoms among a community sample of African-American and Caucasian older adults. Community Ment Health J. 2004;40:309–330. doi: 10.1023/b:comh.0000035227.57576.46. [DOI] [PubMed] [Google Scholar]
- 6.Cummings SM, Neff JA, Husaini BA. Functional impairment as a predictor of depressive symptomatology: The role of race, religiosity, and social support. Health Soc Work. 2003;28:23–32. doi: 10.1093/hsw/28.1.23. [DOI] [PubMed] [Google Scholar]
- 7.Bruce ML. Depression and disability in late life: Directions for future research. Am J Geriatr Psychiatry. 2001;9:102–112. [PubMed] [Google Scholar]
- 8.Lang FR, Rieckmann N, Baltes MM. Adapting to aging losses: Do resources facilitate strategies of selection, compensation, and optimization in everyday functioning? J Gerontol B Psychol Sci Soc Sci. 2002;57B:501–509. doi: 10.1093/geronb/57.6.p501. [DOI] [PubMed] [Google Scholar]
- 9.Williams DR. The health of U.S. racial and ethnic populations. J Gerontol B Psychol Sci Soc Sci. 2005;60B:53–62. doi: 10.1093/geronb/60.special_issue_2.s53. [DOI] [PubMed] [Google Scholar]
- 10.Kelley-Moore JA, Ferraro KM. The Black/white disability gap: Persistent inequality in later life? J Gerontol B Psychol Sci Soc Sci. 2004;59B:S34–S43. doi: 10.1093/geronb/59.1.s34. [DOI] [PubMed] [Google Scholar]
- 11.George LK, Lynch SM. Race differences in depressive symptoms: A dynamic perspective on stress exposure and vulnerability. J Health Soc Behav. 2003;44:353–369. [PubMed] [Google Scholar]
- 12.Gallo JJ, Cooper-Patrick L, Lesikar S. Depressive symptoms of whites and African Americans aged 60 years and older. J Gerontol B Psychol Sci Soc Sci. 1998;53B:277–286. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- 13.Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60B:136–142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 14.Schulz R, Heckhausen J. A life span model of successful aging. Am Psychol. 1996;51:702–714. doi: 10.1037//0003-066x.51.7.702. [DOI] [PubMed] [Google Scholar]
- 15.Schulz R, Heckhausen J, O’Brien AT. Control and the disablement process in the elderly. Soc Behav Pers. 1994;9:139–152. [Google Scholar]
- 16.Wrosch C, Schulz R, Heckhausen J. Health stresses and depressive symptomatology in the elderly: The importance of health engagement control strategies. Health Psychol. 2002;21:340–348. doi: 10.1037//0278-6133.21.4.340. [DOI] [PubMed] [Google Scholar]
- 17.Gitlin LN, Winter L, Dennis M, et al. A randomized trial of a multi-component home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 18.Gitlin LN, Hauck WW, Winter L, et al. Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable elders: Preliminary findings. J Am Geriatr Soc. 2006;54:950–955. doi: 10.1111/j.1532-5415.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state:’ A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Morris J, Sherwood S, Mor V. An assessment tool for use in identifying functionally vulnerable persons in the community. Gerontologist. 1984;24:373–379. doi: 10.1093/geront/24.4.373. [DOI] [PubMed] [Google Scholar]
- 21.Krause N, Markides K. Measuring social support among older adults. Int J Aging Human Dev. 1990;30:37–53. doi: 10.2190/CY26-XCKW-WY1V-VGK3. [DOI] [PubMed] [Google Scholar]
- 22.Lawton MP, Moss M, Hoffman C, et al. Valuation of life: A concept and a scale. J Aging Health. 2001;13:3–31. doi: 10.1177/089826430101300101. [DOI] [PubMed] [Google Scholar]
- 23.Dennis MP, Winter L, Black HK, et al. What is valuation of life for frail community-dwelling older adults: Factor structure and criterion validity of the VOL. Presented at: Gerontological Society of American Annual Meeting; Orlando, FL. 2005. [Google Scholar]
- 24.Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: The fitness arthritis and seniors trial (FAST) JAMA. 1997;277:25–31. [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychologi Meas. 1977;1:385–401. [Google Scholar]
- 26.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 27.Kraemer HC, Wilson T, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 28.Gitlin LN, Winter L, Dennis MP, et al. Who benefits more from a home intervention to reduce functional difficulties?. Moderator effects by gender, race, age, and education; Presented at the Gerontological Society of American Annual Meeting; Orlando, FL. 2005. [Google Scholar]
- 29.Hortobagyi T, Mizelle C, Beam S, et al. Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci. 2003;58A:M453–M460. doi: 10.1093/gerona/58.5.m453. [DOI] [PubMed] [Google Scholar]
- 30.Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community-living older persons. J Gerontol A Biol Sci Med Sci. 2003;58A:M70–M75. doi: 10.1093/gerona/58.1.m70. [DOI] [PubMed] [Google Scholar]
- 31.McMullen CK, Luborsky MR. Self-rated health appraisal as cultural and identity process: African American elders’ health and evaluative rationales. Gerontologist. 2006;45:431–438. doi: 10.1093/geront/46.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dilworth-Anderson P, Brummett BH, Goodwin P, et al. Effect of race on cultural justifications for caregiving. J Gerontol B Psychol Sci Soc Sci. 2005;60B:S257–S262. doi: 10.1093/geronb/60.5.s257. [DOI] [PubMed] [Google Scholar]
- 33.Manly JJ. Deconstructing race and ethnicity: Implications for measurement of health outcomes. Med Care. 2006;44:S10–S16. doi: 10.1097/01.mlr.0000245427.22788.be. [DOI] [PubMed] [Google Scholar]
- 34.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 35.Miller DK, Malmstrom TK, Joshi S, et al. Clinically relevant levels of depressive symptoms in community-dwelling middle aged African Americans. J Am Geriatr Soc. 2004;52:741–748. doi: 10.1111/j.1532-5415.2004.52211.x. [DOI] [PubMed] [Google Scholar]