Abstract
Age-related postural hyperkyphosis is an exaggerated anterior curvature of the thoracic spine, sometimes referred to as Dowager’s hump or gibbous deformity. This condition impairs mobility,2,31 and increases the risk of falls33 and fractures.26 The natural history of hyperkyphosis is not firmly established. Hyperkyphosis may develop from either muscle weakness and degenerative disc disease, leading to vertebral fractures and worsening hyperkyphosis, or from initial vertebral fractures that precipitate its development.
Keywords: aging/geriatrics, kyphosis, osteoporosis, postural relationships, thoracic spine
It is also possible that different individuals may develop the same magnitude of hyperkyphosis from different processes, some from vertebral fractures and others from muscle weakness, degenerative disc disease, or other genetically determined processes. Regardless, there are significant negative consequences of hyperkyphosis, and early intervention and treatment of hyperkyphosis could have important clinical and public health benefits.
Our objectives are to review the prevalence and natural history of hyperkyphosis, along with associated health implications if left untreated. We will discuss evidence-based treatment options and potential contraindications, and observations about the direction for future study of hyperkyphosis.
DEFINITION AND PREVALENCE
While a small amount of anterior curvature of the thoracic spine is normal and present due to the shape of the vertebral bodies and intervertebral discs, a kyphosis angle greater than 40°, which is the 95th percentile of normal for young adults, is defined as hyperkyphosis.15,62 In childhood and through the third decade of life the angle of kyphosis averages from 20° to 29°.15 After 40 years of age, kyphosis angle begins to increase—more rapidly in women than men15—from a mean of 43° in women aged 55 to 60 years to a mean of 52° in women 76 to 80 years of age.12 Reports of prevalence and incidence of hyperkyphosis in older adults vary from approximately 20% to 40% among both men and women.32,60 As kyphosis angle increases, physical performance and quality of life often declines, making early intervention for hyperkyphosis a priority.
MEASUREMENT
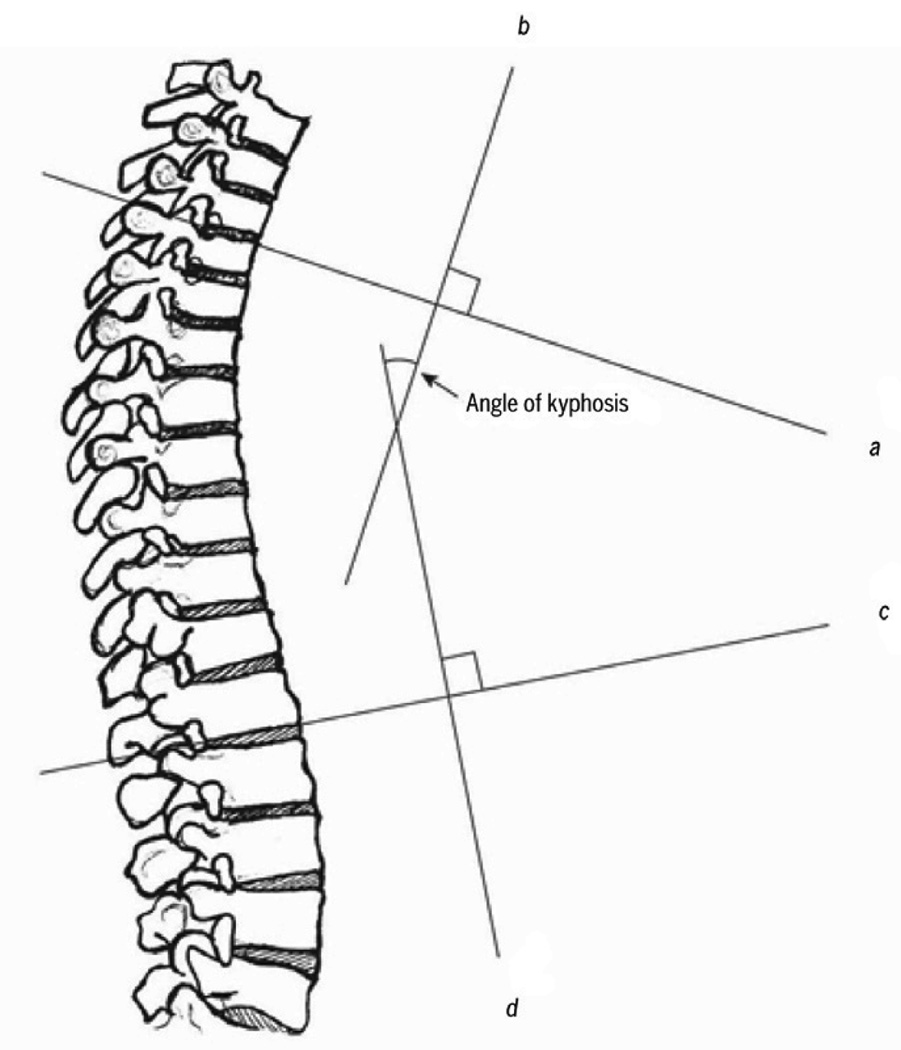
The gold-standard orthopaedic technique for assessment of thoracic kyphosis is standing lateral spine radiographs. In elderly persons, spinal radiographs may be taken in the supine position for comfort. The Cobb’s angle of kyphosis is calculated from perpendicular lines drawn on a standard thoracic spine radiograph: a line extends through the superior endplate of the vertebral body, marking the beginning of the thoracic curve (usually at T4), and the inferior endplate of the vertebral body, marking the end of the thoracic curve (usually at T12) (FIGURE 1).29 While this method is the gold-standard, it is limited by the need for radiography.
FIGURE 1.
Cobb’s angle of kyphosis, calculated from a lateral radiograph. (A) Draw the first line (line a) through the superior end plate of T3, and a second line (line b) that is perpendicular to line a. (B) Draw a third line (line c) through the inferior endplate of T12, and a fourth line (line d) that is perpendicular to line c. Cobb’s angle of kyphosis is the measured angle at the intersection of lines b and d. Diagram from Kado DM, Prenovost K, Crandall C. Narrative Review: Hyperkyphosis in Older Persons. Ann Int Med. 2007;147:330–338, with permissions from Ann Int Med.33
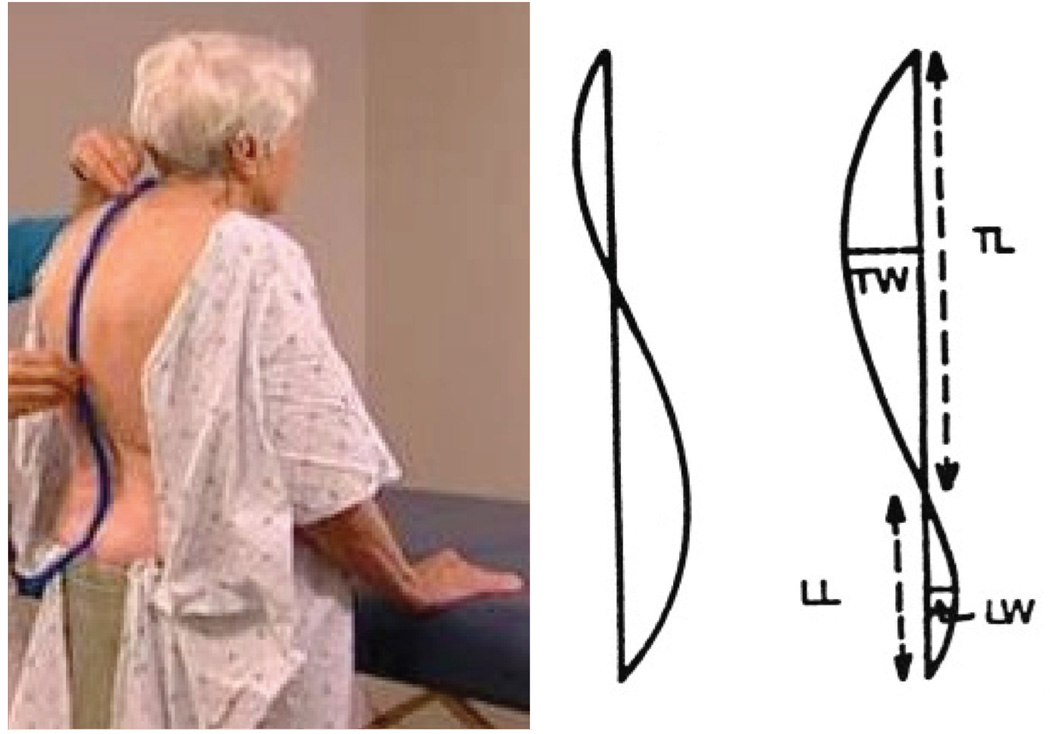
Acceptable alternatives are the Debrunner kyphometer and the flexicurve ruler.41 Both methods are performed standing. The kyphometer measures the angle of kyphosis, the arms of the protractor-like device are placed at the top and bottom of the thoracic curve, usually over the spinous processes of T2 and T3 superiorly, and T11 and T12 inferiorly (FIGURE 2).41 The flexicurve ruler is a plastic, moldable device that is aligned over the C7 spinous process to the L5–S1 interspace; the ruler is molded to the curvature of the spine and the thoracic and lumbar curves are traced (FIGURE 3). The kyphosis index is calculated as the width divided by the length of the thoracic curve, multiplied by 100 (FIGURE 3).47 A kyphosis index value greater than 13 is defined as hyperkyphotic.40
FIGURE 2.
Debrunner kyphometer measurement of kyphosis. (A) Place the upper foot of the kyphometer over the interspace of T2 and T3 spinous processes, and the lower foot of the kyphometer over the interspace of T11 and T12 spinous processes. (B) Ask the patient to exhale and measure the usual kyphosis, and then “stand as straight and tall as you can” to measure the best kyphosis. (C) Read the Cobb’s angle measurement of kyphosis from the device.
FIGURE 3.
Flexicurve ruler measurement of kyphosis. (A) Mark the C7 spinous process and the L5–S1 interspace on the patient’s skin with a grease pencil. (B) Place the superior end of the ruler at C7 and the inferior end over the lumbar spine, molding the ruler to the curves of the thoracic and lumbar spine. (C) Mark the level of the C7 spinous process and the L5–S1 interspace on the ruler. (D) Carefully transfer the molded ruler to tracing paper, with the C7 spinous process and the L5-S1 interspace marks aligned along a vertical line. (E) Trace the thoracic and lumbar curvatures from the ruler onto the paper, drawing a horizontal line from the vertical line to the apex of the thoracic curve. (F) Measure thoracic width (TW) and thoracic length (TL); calculate kyphosis index (KI): (TW/TL) × 100. (G) Lumbar width (LW) and lumbar length (LL) can also be measured. Photograph and diagram used with permission from Carleen Lindsey, PT, MSc, GCS, and the Section on Geriatrics, APTA.38
Lundon et al41 compared the reliability of standing radiographic, kyphometer, and flexicurve methods of measuring kyphosis in a group of 24 postmenopausal women with osteoporosis. There was excellent intrarater and interrater reliability (intraclass correlation coefficients [ICCs] = 0.87–0.92) for each method, indicating the strength of each instrument for measuring kyphosis.41 Kado et al29 compared the agreement between standing kyphometer and supine radiologic measure of Cobb’s angle of kyphosis in older women. While the overall agreement was acceptable (ICC = 0.68), the agreement between the kyphosis measurements greater or equal to 50° was poor (ICC = 0.44). Thus, while all measures can be used to reliably quantify kyphosis, the standing kyphometer method for measuring a kyphotic spine may overestimate the degree of kyphosis compared with supine radiographs. However, the external methods do not involve radiographic exposure and are inexpensive and easy to use in the clinical setting.
Other clinical measures are sometimes used to quantify hyperkyphotic posture. Standing measurements of tragus to the wall or occiput to the wall, and supine measurement of the number of 1.5-cm blocks needed to support the head have been described2,33; however, reliability of these methods has not been investigated and there are no studies comparing these measures to the gold-standard radiograph.
CLINICAL CONSEQUENCES OF HYPERKYPHOSIS
Functional Limitations
Excessive kyphosis has detrimental effects on physical performance, the ability to perform activities of daily living, and overall quality of life.2,52,60 Women with hyperkyphotic posture demonstrate difficulty rising from a chair repeatedly without using their arms,2,31 significantly poorer balance and slower gait velocity, wider base of support with stance and gait, and decreased stair-climbing speed2—impairments that have been associated with increased risk for falls. In addition, osteoporotic women with hyperkyphosis have increased postural sway compared to those with normal posture.42
Hyperkyphosis is also associated with self-reported decline in physical functioning. Women with hyperkyphosis report greater difficulty reaching and performing heavy housework and score lower on the basic activities of daily living scale compared with their peers.2,10,52,60
Musculoskeletal Alterations
As kyphosis increases, there are concomitant alterations in the normal sagittal plane alignment that may cause pain and risk of dysfunction in the shoulder and pelvic girdle, and cervical, thoracic, and lumbar spine. Forward head posture, scapula protraction, reduced lumbar lordosis, and decreased standing height are often associated with hyperkyphosis. 2 These postural changes increase the flexion bias around the hip and shoulder joints that can interfere with normal joint mechanics and movement patterns.
Hyperkyphosis is a significant risk factor for future vertebral and extremity fractures.12,13,26 Older women with hyperkyphosis have a 70% increased risk of future fracture, independent of age or prior fracture, and the risk for fracture increases as hyperkyphosis progresses.26
Quality of Life
Women with hyperkyphosis report more physical difficulty, more adaptations to their lives, and greater generalized fears than women without hyperkyphosis.44 Additionally, community-dwelling men and women aged 65 years and older with hyperkyphosis report poorer satisfaction with subjective health, family relationships, economic conditions, and their lives in general.60
Mortality
Hyperkyphotic posture has been associated with increased mortality, with higher mortality rates associated with the severity of kyphosis.32 Reduced vital capacity is associated with hyperkyphosis, and severe hyperkyphosis is predictive of pulmonary death among community-dwelling women.28,38 Women in the highest quartile of kyphosis were more likely to die of pulmonary death compared with those in the lower quartiles of kyphosis.28 Two recent cohort studies confirm these adverse health effects of hyperkyphosis even after adjusting for vertebral fractures and bone mineral density.30,32
RISK FACTORS
The causes of hyperkyphosis have yet to be fully elucidated. However, multiple musculoskeletal, neuromuscular, and sensory impairments are significant predictors of age-related hyperkyphosis.
Vertebral Fractures
Kyphosis increases with the number of vertebral fractures and is more strongly related to thoracic fractures than lumbar fractures.12 Hyperkyphosis is most prominent in women with multiple thoracic anterior wedge fractures.12 Women without vertebral fractures, who have greater degrees of kyphosis, are more likely to experience a subsequent vertebral fracture. 26 Biomechanical models of stress loading on the spine suggest that forces applied to the osteoporotic spine during daily living can cause vertebral wedging and compression fractures.5,37 The severity of wedging increases as bone mineral density decreases, resulting in greater numbers of vertebral compression fractures and a further cascade of increasing hyperkyphosis.16,21,46
Degenerative Disc Disease
Many people consider vertebral fractures to be the underlying cause of age-related hyperkyphosis, although studies of older adults report only approximately 40% of men and women with the most severe hyperkyphosis have vertebral compression or wedge fractures.53 A common radiographic finding associated with hyperkyphosis among older adults is degenerative disc disease.16,43,53 In a study of healthy women aged 39 to 91 years, there was a significant correlation between anterior disc height and kyphosis angle (r = −0.34, P<.001)43; as the anterior disc height decreased, the angle of kyphosis increased. Others have reported that the majority of older adults 50 to 96 years of age with hyperkyphosis had degenerative disc disease and no evidence of vertebral fractures or osteoporosis,53 suggesting that hyperkyphosis doesn’t predict fractures or osteoporosis. However, a strong association between vertebral body anterior- to-posterior height ratio and kyphosis angle suggests that it is the combined influence of both degenerative disc disease and anterior vertebral deformities that accounts for significant variation in kyphosis.16,53
Muscle Weakness
Several studies confirm that hyperkyphosis is associated with spinal extensor muscle weakness.27,56,57 In healthy postmenopausal women, strength of the spinal extensor muscles is inversely associated with kyphosis (r = −0.30, P = .019).27,56 There is also an inverse relationship between grip and ankle strength and kyphosis,2 suggesting that age-related hyperkyphosis may be part of a larger geriatric syndrome associated with adverse health outcomes that negatively impact physical function.6,9
Decreased Mobility
Decreased spinal extension mobility occurs with aging, interfering with the ability to stand erect and maintain normal postural alignment.22 Cadaver studies suggest that calcification and ossification of the anterior longitudinal ligament in the thoracic region might contribute to increased Cobb’s angle of kyphosis.4 Furthermore, shorter pectoral and hip flexor muscles are linked to severe hyperkyphosis, although it is not known whether the short muscles pull the shoulders and hips anteriorly, or whether the kyphotic posture results in shorter anterior musculature. 2 There are likely other contributing muscular, ligamentous, connective tissue, and joint impairments that have not been identified.
Sensory Deficits
Age-related deficits in the somatosensory, visual, and vestibular systems likely contribute to the loss of upright postural control. With a loss of proprioceptive and vibratory input from the joints in the lower extremities in elderly adults compared with young adults,14 the perception of erect vertical alignment becomes impaired. 14,25 Similar declines occur in the visual system with aging,54 and primary age-related diseases in the eyes, including cataracts and macular degeneration, exacerbate decline in visual acuity. Head pitch position was found to be greater during locomotion for normal elderly compared to young adults,23 and increased even further among older adults wearing bifocals during stair descent.20 Additionally, age-related sensory loss in the vestibular system24 increases the reliance on already declining visual and somatosensory cues, and can further impact upright postural alignment.
TREATMENT OF HYPERKYPHOSIS
There is a lack of efficacious medical interventions for hyperkyphosis. Physical therapy should be a first-line approach, particularly because many of the causes of hyperkyphosis are of musculoskeletal origin. Recognition and treatment of hyperkyphosis could contribute to reduced risk of falls, fractures, and functional limitations. Several physical therapy interventions aimed at reducing hyperkyphosis are currently available (TABLE 1).
TABLE 1.
Evidence-based treatment interventions
| Procedure | Dosage | Goal |
|---|---|---|
| Strengthening | ||
| Prone trunk lift to neutral | 3 sets of 8 repetitions (0-to 2.3-kg dumbbells or wrist cuff weights); progress from arms by side, to arms in “W” position, to fists by ears |
Strengthen spinal extensors,27 strengthen middle and lower trapezius36 |
| Prone trunk lift to neutral with weighted backpack (FIGURE 4) |
1 set of 10 repetitions; 5 times per wk; 30% of 1-repetition maximum weight in backpack |
Strengthen spinal extensors27,50 |
| Quadruped alternate arm/leg lift | 3 sets of 8 repetitions (0- to 2.3-kg wrist and thigh cuff weights) |
Strengthen spinal extensors, scapula and trunk stabilization, reduce anterior tightness18,36 |
| Ankle plantar flexion with resistance bands | 3 sets of 8 repetitions | Increase ankle strength2 |
| Stretching/mobility | ||
| Chest stretching and diaphragmatic breathing on foam roller |
60 s | Lengthen pectoralis muscles, expand ribcage2,38 |
| Prone hip extension/knee flexion | Passive 30 | Lengthen iliopsoas and rectus femoris2 |
| Supine knee extension with hip at 90° flexion | Passive 30 | Lengthen hamstrings2 |
| Sidelying thoracic rotation | 3 sets of 8 repetitions, progress to resistance bands to combine mobility and strength |
Thoracic extension range of motion, strengthen spinal extensors and rotators22 |
| Alternating shoulder flexion with diaphragmatic breathing on foam roller |
Repeat 10–30 times | Mobilize thoracic spine22 |
| Postural alignment | ||
| Postural correction | Performed throughout the day sitting or standing; arms by side or hands behind head and retract scapula; practice standing alignment visualizing lengthening through the crown of the head with sternum lifted |
Improve spinal proprioception3,36,48,55 and postural alignment |
| Neutral spine sit to stand | Performed throughout the day | Integrate neutral spine alignment into activities |
| Bracing | ||
| Spinomed | Wear 2 h/d | Provides proprioceptive input to facilitate upright postural alignment and facilitates spinal extensor muscle activity49 |
| Weighted spinal kyphosis orthosis (FIGURE 5) | Wear when ambulating | Provides proprioceptive input to facilitate upright postural alignment55,58 |
| Taping | ||
| Apply therapeutic tape from the acromioclavicular joint diagonally across trapezius to T6 bilaterally (FIGURE 6) |
Tape can be applied for wear during exercise (skin prep necessary) |
Passive support from the tape19 |
Medicines and Surgery
Many men and women with prevalent hyperkyphosis are treated with osteoporosis antiresorptive or bone-building medications because they have low bone density or spine fractures. While osteoporosis treatment helps to prevent incident spine fractures, no medications have been shown to improve hyperkyphosis. Vertebroplasty and kyphoplasty are surgical procedures primarily used to treat refractory pain following vertebral fracture, and they have been shown to reduce kyphosis angle in select patient populations only.8,61 However, evidence suggests that physical disability and pain relief may be improved after vertebroplasty and kyphoplasty compared to medical management but only within the first 3 months after intervention.45 Furthermore, recent evidence from 2 randomized controlled trials suggests that clinical improvement in physical disability and pain is similar among patients undergoing vertebroplasty, compared to sham procedure for painful vertebral fractures, at 1-month and 6-month follow- up.7,35 High-quality randomized trials with long-term follow-up are needed to investigate benefits of these procedures on subsequent vertebral fractures. No studies have investigated the effects on kyphosis of combined treatment with medications, surgical interventions, and physical therapy interventions.
Exercise: Indications and Contraindications
Seminal research by Sinaki et al59 suggests that the forces applied to the spine during exercise can alter the occurrence of subsequent vertebral compression fractures in women with prior fracture. In this study, 68% of the women who performed flexion exercises developed a subsequent fracture within the following 6 months, compared with only 16% of those who performed extension exercises, suggesting that flexion exercises increase fracture risk.59 In addition, the conceptual models of spinal loading suggest that flexion stress on the spine increases the risk for fractures when the underlying bone strength is impaired5 and may partially explain why older women with hyperkyphosis have an increased risk of future fracture independent of age or prior fracture.26 Hence, it is important to train individuals with age-related hyperkyphosis to avoid flexion stresses on the spine during exercise and activities of daily living (TABLE 2), regardless of whether they have had a prior fracture. Furthermore, training using trunk stabilization should avoid curl-up exercises to reduce flexion bias on the spine.
TABLE 2.
Postural alignment during exercise and activities of daily living
| Dos | Don’ts |
|---|---|
| Maintain good postural alignment during exercise | Avoid seated rowing machines or upper body ergometers |
| Strengthen core stabilizer muscles, such as transversus abdominus, obliques, and multifidus |
Avoid crunches, curl-ups, or flexed position (traditional sit-ups) |
| When bending or lifting objects, keep the spine in neutral, and bend at the hips and knees (hip hinge); keep objects close to the body |
Don’t twist or bend your spine when lifting objects |
| When getting out of bed, roll onto the side before sitting up (log roll) |
Don’t sit straight up from a horizontal position |
| When coughing or sneezing, stabilize trunk in neutral by hugging a pillow, or placing hands on knees while hip hinging, or place hand in small of back to help keep back in neutral |
Avoid forceful trunk flexion while coughing or sneezing |
| Maintain the natural curves in your neck and back while sitting and standing. Imagine that you are lengthening through the crown of your head |
Avoid leaning over towards your work, or standing in a pelvic tilt |
| Adjust height of the walker and walk within the frame when ambulating |
Don’t bend to reach, or push walker |
In a randomized trial of prone trunk extension exercises in 60 healthy postmenopausal women, the angle of kyphosis and back extension strength improved among women with the most severe kyphosis and significant weakness of the spinal extensor muscles at baseline, suggesting that hyperkyphosis may be modified by spinal extensor muscle strengthening exercises.27 Subjects in the intervention group performed 10 repetitions of prone trunk extension exercises 5 times a week for a year while wearing a weighted backpack (FIGURE 4).27 At the 10-year follow-up, the number of vertebral compression fractures was significantly lower in the intervention group compared to controls, regardless of kyphosis or strength, even though the intervention was not continued in the intervening time.57
FIGURE 4.
Prone trunk lift with weighted backpack. (A) Patient lies prone over a pillow, wearing a backpack secured to the upper back. (B) Squeeze shoulder blades together, tighten gluteal muscles and lift chest off the mat, keeping cervical and lumbar spine in neutral. (C) Begin with 1 set of 10 repetitions and progress with weights in backpack, up to a maximum weight of 30% of 1-repetition maximum.27 In lieu of a weighted backpack, patients can use handheld dumbbells and perform the exercise with their elbows bent and their hands by their ears. Progress the dumbbells to 2.27 kg in each hand, and perform 3 sets of 8 repetitions.36
In a randomized controlled trial among 118 men and women 60 years and older with kyphosis greater or equal to 40°, participation in modified classical yoga 3 days a week for 24 weeks resulted in a 5% improvement in kyphosis index (P = .004), and 4.4% improvement in kyphosis angle measured from the flexicurve (P = .006).17 The intervention did not result in statistically significant improvement in kyphometer angle, measured physical performance, or self-assessed health-related quality of life (each P>.1).17 The yoga intervention was limited to poses that included stretching into shoulder flexion, quadruped alternate arm/leg lift, prone trunk extension, and standing lunges with shoulder flexion.17
In an uncontrolled trial of a multidimensional exercise intervention among 21 older women with kyphosis greater or equal to 50°, kyphosis improved 11% after 3 months of exercise.36 The exercise intervention was designed to target multiple strength, range-of-motion, and sensory impairments associated with kyphosis, and included prone and quadruped spinal extension strengthening with weights, lower trapezius and transversus abdominus strengthening, spine mobility, shoulder and hip stretching, and postural alignment training twice a week for 12 weeks in a group setting.36 Participants maintained gains in spinal extension strength and physical performance, and demonstrated additional improvements in measured kyphosis 1 year after completing the 12-week exercise program with no further intervention in the interim. These results present evidence that targeted exercises that reduce hyperkyphosis provide long-term benefits.48
In an investigation among 81 women, aged 50 to 59 years, participants were instructed to perform spinal extension strengthening exercises 3 times per week for 1 year.1 Only 15 of these women complied with the exercises 3 times a week and 20 did not do any of the exercises. The group of 15 women who were compliant were compared to the group of 20 who were not compliant.1 Kyphosis and forward head posture were significantly reduced among the compliant exercise group compared with the noncompliant group.1
Renno et al50 employed respiratory muscle exercises combined with back extensor muscle strengthening and aerobic exercises in a study of 14 women with osteoporosis. They found that respiratory pressures improved 12% to 23%, exercise tolerance increased 13%, and thoracic curvature was reduced 5%.50 While it is not clear whether reducing hyperkyphosis, respiratory muscle exercises, or aerobic exercise training explains the improved respiratory pressures and exercise tolerance, this study suggests the importance of addressing lung capacity and breathing exercises in this population.
Manual Therapy/Mobilization
Three case reports suggest that myofascial, spinal, and scapular mobilization techniques improve postural alignment in patients with hyperkyphosis.11,39,51 Physical therapists reported reduced kyphosis after soft tissue myofascial,11 neurodevelopmental, spinal, and scapular mobilization, 51 and active therapeutic movement techniques.39 These techniques have not been subjected to rigorous evaluation in clinical trials.
Therapeutic exercise, such as self-mobilization lying supine on a foam roller, has been used successfully in a multidimensional exercise program that reduced kyphosis among hyperkyphotic women.36 This type of self-mobilization technique may be appropriately applied in this population.
Bracing
In a randomized controlled trial with 62 community-dwelling older women with osteoporosis and kyphosis greater or equal to 60°, wearing a Spinomed (Medi, Whitsett, NC) spinal orthosis 2 hours a day for 6 months resulted in an 11% decrease in kyphosis angle, improved standing height, increased spinal extensor strength, and decreased postural sway.49 Although the orthosis appeared to be beneficial, passive bracing does not provide the beneficial effects of exercise on bone.63 While not yet studied, bracing used in combination with therapeutic exercises may provide additional beneficial effect.
The spinal weighted kyphosis orthosis is another bracing alternative for hyperkyphosis (FIGURE 5).55 This lightweight vest device reportedly improves balance and reduces pain among osteoporotic hyperkyphotic women.55
FIGURE 5.
Weighted spinal kyphosis orthosis.55 (A) Place the weighted kyphosis orthosis over the thoracic spine and adjust the straps such that the bottom of the pouch is located at the waistline. (B) Begin with a 115-g weight in the orthosis, and progress to a 225-g weight to provide sensory feedback to improve postural alignment. (C) Instruct the patient to wear the device when ambulating.
Taping
Therapeutic taping may also reduce kyphosis angle according to preliminary research in 15 women with osteoporotic vertebral fractures; those with the greatest initial kyphosis had the greatest reduction in kyphosis with taping (FIGURE 6).19 Taping during 3 individual 40-second static standing tasks reduced kyphosis angle immediately after the tasks, compared with sham taping or no taping.19
FIGURE 6.
Thoracic taping for hyperkyphosis. (A) Instruct the patient to stand and elongate the crown of the head towards the ceiling. (B) Apply cover roll as needed to protect the skin. (C) Apply therapeutic tape from the anterior aspect of acromioclavicular joint, over the muscle bulk of the upper trapezius, and diagonally over the spinous process of T6. (D) Apply tape in this method bilaterally, intersecting the strips of tape at T6.
FUTURE RESEARCH
Existing evidence supports the use of exercise, bracing, and taping interventions to reduce hyperkyphosis, improve quality of life, and reduce risk for future fractures for men and women. Additional research, especially large, well-controlled randomized clinical trials are required to confirm the optimal type, duration, and long-term effects of interventions. The effects of combined treatments of bracing or taping with exercise, or medications, surgical interventions, and exercise, warrant further study. Further work is needed to determine whether reducing hyperkyphosis is associated with improved physical performance. Research is also needed to determine the threshold of hyperkyphosis associated with functional impairments. This information could be used to develop screening guidelines that would assist clinicians to time interventions. Prevention strategies for hyperkyphosis require testing to determine whether appropriately timed interventions might prevent age-related hyperkyphosis and reduce the associated cascade of fractures and functional impairments. While at this time evidence is lacking to support manual therapy techniques to reduce hyperkyphosis, case reports suggest that appropriately applied manual treatments may have a place in a comprehensive treatment approach.
CONCLUSION
Kyphosis is common in older individuals, increases risk for fracture and mortality, and is associated with impaired physical performance, health, and quality of life. Screening for hyperkyphosis could be easily implemented in the clinical setting and the evidence to date suggests that relatively simple, available, and inexpensive conservative interventions may have a beneficial effect. Further research and, particularly, large, well-controlled randomized clinical trials are needed to develop optimal strategies to treat hyperkyphosis and prevent its serious associated complications.
ACKNOWLEDGEMENTS
The authors would like to thank Alyssa Herrera-Set, Christine Jacobsen, Tanya Leibovici, and Laura Miller for their assistance with research, editing and photography, and Amy Markowitz for manuscript editing.
The authors would like to acknowledge the UCSF-Kaiser Building Interdisciplinary Research Careers in Women’s Health Program, NICHD/ORWH support, NICHD grant number 5K12 HD052163.
REFERENCES
- 1.Ball JM, Cagle P, Johnson BE, Lucasey C, Lukert BP. Spinal extension exercises prevent natural progression of kyphosis. Osteoporos Int. 2009;20:481–489. doi: 10.1007/s00198-008-0690-3. http://dx.doi.org/10.1007/s00198-008-0690-3. [DOI] [PubMed] [Google Scholar]
- 2.Balzini L, Vannucchi L, Benvenuti F, et al. Clinical characteristics of flexed posture in elderly women. J Am Geriatr Soc. 2003;51:1419–1426. doi: 10.1046/j.1532-5415.2003.51460.x. [DOI] [PubMed] [Google Scholar]
- 3.Benedetti MG, Berti L, Presti C, Frizziero A, Giannini S. Effects of an adapted physical activity program in a group of elderly subjects with flexed posture: clinical and instrumental assessment. J Neuroeng Rehabil. 2008;5:32. doi: 10.1186/1743-0003-5-32. http://dx.doi.org/10.1186/1743-0003-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birnbaum K, Siebert CH, Hinkelmann J, Prescher A, Niethard FU. Correction of kyphotic deformity before and after transection of the anterior longitudinal ligament--a cadaver study. Arch Orthop Trauma Surg. 2001;121:142–147. doi: 10.1007/s004020000193. [DOI] [PubMed] [Google Scholar]
- 5.Bouxsein ML, Melton LJ, Riggs BL, et al. Age- and sex-specific differences in the factor of risk for vertebral fracture: a population-based study using QCT. J Bone Miner Res. 2006;21:1475–1482. doi: 10.1359/jbmr.060606. [DOI] [PubMed] [Google Scholar]
- 6.Brocklehurst JC, Robertson D, James-Groom P. Skeletal deformities in the elderly and their effect on postural sway. J Am Geriatr Soc. 1982;30:534–538. doi: 10.1111/j.1532-5415.1982.tb01693.x. [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–568. doi: 10.1056/NEJMoa0900429. http://dx.doi.org/10.1056/NEJMoa0900429. [DOI] [PubMed] [Google Scholar]
- 8.Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003;53:1354–1360. doi: 10.1227/01.neu.0000093200.74828.2f. discussion 1360-1351. [DOI] [PubMed] [Google Scholar]
- 9.Chow RK, Harrison JE. Relationship of kyphosis to physical fitness and bone mass on post-menopausal women. Am J Phys Med. 1987;66:219–227. [PubMed] [Google Scholar]
- 10.Cortet B, Houvenagel E, Puisieux F, Roches E, Garnier P, Delcambre B. Spinal curvatures and quality of life in women with vertebral fractures secondary to osteoporosis. Spine (Phila Pa 1976) 1999;24:1921–1925. doi: 10.1097/00007632-199909150-00010. [DOI] [PubMed] [Google Scholar]
- 11.Davis CM. Myofascial release as complementary in physical therapy for two elderly patients with osteoporosis and kyphoscoliosis-two case studies. J Geriatr Phys Ther. 2002;25:33. [Google Scholar]
- 12.Ensrud KE, Black DM, Harris F, Ettinger B, Cummings SR. Correlates of kyphosis in older women. The Fracture Intervention Trial Research Group. J Am Geriatr Soc. 1997;45:682–687. doi: 10.1111/j.1532-5415.1997.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 13.Ettinger B, Black DM, Palermo L, Nevitt MC, Melnikoff S, Cummings SR. Kyphosis in older women and its relation to back pain, disability and osteopenia: the study of osteoporotic fractures. Osteoporos Int. 1994;4:55–60. doi: 10.1007/BF02352262. [DOI] [PubMed] [Google Scholar]
- 14.Ferrucci L, Bandinelli S, Cavazzini C, et al. Neurological examination findings to predict limitations in mobility and falls in older persons without a history of neurological disease. Am J Med. 2004;116:807–815. doi: 10.1016/j.amjmed.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Fon GT, Pitt MJ, Thies AC., Jr Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol. 1980;134:979–983. doi: 10.2214/ajr.134.5.979. [DOI] [PubMed] [Google Scholar]
- 16.Goh S, Price RI, Leedman PJ, Singer KP. The relative influence of vertebral body and intervertebral disc shape on thoracic kyphosis. Clin Biomech (Bristol, Avon) 1999;14:439–448. doi: 10.1016/s0268-0033(98)00105-3. [DOI] [PubMed] [Google Scholar]
- 17.Greendale GA, Huang MH, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:1569–1579. doi: 10.1111/j.1532-5415.2009.02391.x. http://dx.doi.org/10.1111/j.1532-5415.2009.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greendale GA, McDivit A, Carpenter A, Seeger L, Huang MH. Yoga for women with hyperkyphosis: results of a pilot study. Am J Public Health. 2002;92:1611–1614. doi: 10.2105/ajph.92.10.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greig AM, Bennell KL, Briggs AM, Hodges PW. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008;13:249–257. doi: 10.1016/j.math.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Hamel K. Head and trunk kinematics during stair descent. International Society of Biomechanics, XVIIIth Congress; Switzerland; Zurich. 2001. [Google Scholar]
- 21.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Reliability of centroid, Cobb, and Harrison posterior tangent methods: which to choose for analysis of thoracic kyphosis. Spine (Phila Pa 1976) 2001;26:E227–E234. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 22.Hinman MR. Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J. 2004;4:413–417. doi: 10.1016/j.spinee.2004.01.002. http://dx.doi.org/10.1016/j.spinee.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 23.Hirasaki E, Kubo T, Nozawa S, Matano S, Matsunaga T. Analysis of head and body movements of elderly people during locomotion. Acta Otolaryngol Suppl. 1993;501:25–30. doi: 10.3109/00016489309126208. [DOI] [PubMed] [Google Scholar]
- 24.Horak FB, Diener HC, Nashner LM. Influence of central set on human postural responses. J Neurophysiol. 1989;62:841–853. doi: 10.1152/jn.1989.62.4.841. [DOI] [PubMed] [Google Scholar]
- 25.Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–738. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 26.Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006;21:419–423. doi: 10.1359/JBMR.051201. http://dx.doi.org/10.1359/JBMR.051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69:1054–1059. doi: 10.1016/s0025-6196(12)61372-x. [DOI] [PubMed] [Google Scholar]
- 28.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 29.Kado DM, Christianson L, Palermo L, Smith-Bindman R, Cummings SR, Greendale GA. Comparing a supine radiologic versus standing clinical measurement of kyphosis in older women: the Fracture Intervention Trial. Spine (Phila Pa 1976) 2006;31:463–467. doi: 10.1097/01.brs.0000200131.01313.a9. http://dx.doi.org/10.1097/01.brs.0000200131.01313.a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14:589–594. doi: 10.1007/s00198-003-1412-5. http://dx.doi.org/10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 31.Kado DM, Huang MH, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: the Rancho Bernardo study. J Gerontol A Biol Sci Med Sci. 2005;60:633–637. doi: 10.1093/gerona/60.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52:1662–1667. doi: 10.1111/j.1532-5415.2004.52458.x. http://dx.doi.org/10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 33.Kado DM, Huang MH, Nguyen CB, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007;62:652–657. doi: 10.1093/gerona/62.6.652. [DOI] [PubMed] [Google Scholar]
- 34.Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007;147:330–338. doi: 10.7326/0003-4819-147-5-200709040-00008. [DOI] [PubMed] [Google Scholar]
- 35.Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–579. doi: 10.1056/NEJMoa0900563. http://dx.doi.org/10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katzman WB, Sellmeyer DE, Stewart AL, Wanek L, Hamel KA. Changes in flexed posture, musculoskeletal impairments, and physical performance after group exercise in communitydwelling older women. Arch Phys Med Rehabil. 2007;88:192–199. doi: 10.1016/j.apmr.2006.10.033. http://dx.doi.org/10.1016/j.apmr.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 37.Keller TS, Harrison DE, Colloca CJ, Harrison DD, Janik TJ. Prediction of osteoporotic spinal deformity. Spine (Phila Pa 1976) 2003;28:455–462. doi: 10.1097/01.BRS.0000048651.92777.30. http://dx.doi.org/10.1097/01.BRS.0000048651.92777.30. [DOI] [PubMed] [Google Scholar]
- 38.Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141:68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 39.Lewis C, Erhard R, Drysdale G. Kyphoscoliosis improvement while treating a patient for adhesive capsulitis using the active therapeutic movement version 2. J Manipulative Physiol Ther. 2008;31:715–722. doi: 10.1016/j.jmpt.2008.10.003. http://dx.doi.org/10.1016/j.jmpt.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 40.Lindsey C, Bookstein NA. Instructional Video: Kypholordosis Measurement Using the Flexible Curve. APTA Section on Geriatrics; 2007. [Google Scholar]
- 41.Lundon KM, Li AM, Bibershtein S. Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine (Phila Pa 1976) 1998;23:1978–1985. doi: 10.1097/00007632-199809150-00013. [DOI] [PubMed] [Google Scholar]
- 42.Lynn SG, Sinaki M, Westerlind KC. Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil. 1997;78:273–277. doi: 10.1016/s0003-9993(97)90033-2. [DOI] [PubMed] [Google Scholar]
- 43.Manns RA, Haddaway MJ, McCall IW, Cassar Pullicino V, Davie MW. The relative contribution of disc and vertebral morphometry to the angle of kyphosis in asymptomatic subjects. Clin Radiol. 1996;51:258–262. doi: 10.1016/s0009-9260(96)80342-4. [DOI] [PubMed] [Google Scholar]
- 44.Martin AR, Sornay-Rendu E, Chandler JM, Duboeuf F, Girman CJ, Delmas PD. The impact of osteoporosis on quality-of-life: the OFELY cohort. Bone. 2002;31:32–36. doi: 10.1016/s8756-3282(02)00787-1. [DOI] [PubMed] [Google Scholar]
- 45.McGirt MJ, Parker SL, Wolinsky JP, Witham TF, Bydon A, Gokaslan ZL. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J. 2009;9:501–508. doi: 10.1016/j.spinee.2009.01.003. http://dx.doi.org/10.1016/j.spinee.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Milne JS, Lauder IJ. The relationship of kyphosis to the shape of vertebral bodies. Ann Hum Biol. 1976;3:173–179. doi: 10.1080/03014467600001281. [DOI] [PubMed] [Google Scholar]
- 47.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12:225–233. doi: 10.1093/ageing/12.3.225. [DOI] [PubMed] [Google Scholar]
- 48.Pawlowsky SB, Hamel KA, Katzman WB. Stability of kyphosis, strength, and physical performance gains 1 year after a group exercise program in community-dwelling hyperkyphotic older women. Arch Phys Med Rehabil. 2009;90:358–361. doi: 10.1016/j.apmr.2008.07.016. http://dx.doi.org/10.1016/j.apmr.2008.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83:177–186. doi: 10.1097/01.phm.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 50.Renno A, Granito RN, Driusso P, Costa D, Oishi J. Effects of an exercise program on respiratory function, posture, and on quality of life in osteoporotic women: a pilot study. Physiotherapy. 2005;91:113–118. [Google Scholar]
- 51.Roehrig SM. Use of neurodevelopmental treatment techniques in a client with kyphosis: a case report. Physiother Theory Pract. 2006;22:337–343. doi: 10.1080/09593980601023713. http://dx.doi.org/10.1080/09593980601023713. [DOI] [PubMed] [Google Scholar]
- 52.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–1486. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 53.Schneider DL, von Muhlen D, Barrett-Connor E, Sartoris DJ. Kyphosis does not equal vertebral fractures: the Rancho Bernardo study. J Rheumatol. 2004;31:747–752. [PubMed] [Google Scholar]
- 54.Shumway-Cook A, Woollacott MH. Motor Control: Theory and Practical Applications. Baltimore, MD: Lippincott Williams and Wilkins; 1995. [Google Scholar]
- 55.Sinaki M, Brey RH, Hughes CA, Larson DR, Kaufman KR. Significant reduction in risk of falls and back pain in osteoporotic-kyphotic women through a Spinal Proprioceptive Extension Exercise Dynamic (SPEED) program. Mayo Clin Proc. 2005;80:849–855. doi: 10.4065/80.7.849. [DOI] [PubMed] [Google Scholar]
- 56.Sinaki M, Itoi E, Rogers JW, Bergstralh EJ, Wahner HW. Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. Am J Phys Med Rehabil. 1996;75:370–374. doi: 10.1097/00002060-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 57.Sinaki M, Itoi E, Wahner HW, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10-year follow-up of postmenopausal women. Bone. 2002;30:836–841. doi: 10.1016/s8756-3282(02)00739-1. [DOI] [PubMed] [Google Scholar]
- 58.Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study. Am J Phys Med Rehabil. 2002;81:241–246. doi: 10.1097/00002060-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984;65:593–596. [PubMed] [Google Scholar]
- 60.Takahashi T, Ishida K, Hirose D, et al. Trunk deformity is associated with a reduction in outdoor activities of daily living and life satisfaction in community-dwelling older people. Osteoporos Int. 2005;16:273–279. doi: 10.1007/s00198-004-1669-3. [DOI] [PubMed] [Google Scholar]
- 61.Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2003;24:1893–1900. [PMC free article] [PubMed] [Google Scholar]
- 62.Voutsinas SA, MacEwen GD. Sagittal profiles of the spine. Clin Orthop Relat Res. 1986:235–242. [PubMed] [Google Scholar]
- 63.Wolff I, van Croonenborg JJ, Kemper HC, Kostense PJ, Twisk JW. The effect of exercise training programs on bone mass: a metaanalysis of published controlled trials in preand postmenopausal women. Osteoporos Int. 1999;9:1–12. doi: 10.1007/s001980050109. [DOI] [PubMed] [Google Scholar]