Abstract
Purpose
Prostate biopsy for diagnosing cancer can be painful. The efficacy and safety of combination perianal-intrarectal lidocaine-prilocaine (PILP) cream and periprostatic nerve block were compared with nerve block alone during transrectal ultrasound guided prostate biopsy (TRUS-Bx).
Materials and Methods
From October 2007 to August 2009, 74 men undergoing a transrectal prostate biopsy were randomized into two groups. In group 1, 36 patients received a combination of PILP cream and a periprostatic nerve block; and in group 2, 38 patients received lubricant jelly and a periprostatic nerve block. Thirty minutes later, the TRUS-Bx was performed. Pain was evaluated by a 10-point visual analogue scale (VAS) after the biopsy.
Results
Patients in group 1 showed a significantly lower VAS score than patients in group 2 (mean score 2.22±0.89 vs. 3.02±1.15, p<0.001). In addition, there was a difference in the number of patients that had a pain score of three or more, 44% in group 1, and 65% in group 2. The overall complication rate was similar in both groups (p=0.45).
Conclusions
A combination of PILP cream and periprostatic nerve block reduced pain compared to the periprostatic nerve block alone. This safe, simple technique can be considered prior to TRUS-Bx to reduce patient discomfort.
Keywords: Analgesia, Biopsy, Pain, Prostate
INTRODUCTION
Transrectal ultrasound guided prostate biopsy (TRUS-Bx) is a standard procedure used for prostate cancer detection. However, it has recently been reported that most of the patients that undergo TRUS-Bx tolerated the associated discomfort, and 20% of these patients experienced severe pain [1-3].
Therefore, researchers have tried to reduce the pain associated with the TRUS-Bx. If the procedure-associated pain could be reduced, this may improve patient compliance. The two main causes of the pain during the biopsy are the transducer inserted into the rectum, and the biopsy needle that advances through the prostate capsule. To decrease the associated pain, several anesthetic methods including analgesics, topical applications, and nerve blocks have been used. Among these methods, the peri-prostatic nerve block (PPNB) provides very effective pain control [4,5].
However, this does not control the pain associated with the transducer being inserted into the anus. Therefore, in an effort to decrease the pain from the insertion, several studies have shown the efficacy of applying lidocaine-prilocaine cream or lidocaine jelly along with PPNB. However, no prior study on the application of lidocaine-prilocaine cream with PPNB has been carried out in Korea. Therefore, the effects on pain control of perianal-intrarectal lidocaine-prilocaine (PILP) cream applied to the anus and rectum in addition to PPNB were evaluated in this study.
MATERIALS AND METHODS
From October 2007 to August 2009, a prospective, randomized, placebo-controlled study was performed. Patients that satisfied the inclusion criteria were enrolled including patients with any of the following: 1) increased prostate-specific antigen (PSA) with or without an abnormal digital rectal examination (DRE); 2) lesions suspicious for a malignancy on the TRUS with or without an abnormal DRE; or 3) an abnormal DRE finding.
Patients were excluded if they had a history of a previous prostate biopsy, had chronic prostatalgia, anal diseases such as an anal fissure, hemorrhoids, anal surgery, chronic prostatitis/pelvic pain syndrome, concomitant analgesic medication, any other medical condition that could potentially interfere with pain assessment, a history of warfarin treatment or a bleeding tendency, or impaired intellectual ability.
A total of 74 men who met the criteria and agreed to participate in the study were enrolled after providing written consent. They were then randomized by a coin toss to undergo TRUS-Bx with combined anesthesia (PILP cream and PPNB) (group 1), or PPNB only (lubricant jelly and PPNB) (group 2). A urologist administered the PILP cream (5 ml, 5 g) or inert lubricant gel intrarectally with a syringe and massaged it into the anterior rectal wall anal canal and perianal skin. Patients were informed that they had received a dose of a topical substance but they were blinded to the randomization results. Thirty minutes after the application the prostate TRUS-Bx was performed.
For the nerve block technique, the patients received 10 cc of 1% lidocaine local injections into both sides of the prostate's lateral posterior area guided by a transrectal ultrasound. A Philips IU-22 transducer (Philips, Bothell, WA, USA) with a 9.5 MHz rectal probe was used for images in the transaxial and sagittal planes. In most patients, 12 core prostate biopsies were performed, including six parasagittal and six laterally targeted biopsies covering the base, mid zones, and apexes, using a spring-loaded biopsy gun and an 18 gauge AceCut biopsy needle (TSK Laboratory, Tochigi, Japan).
Three hours after the biopsy, another urologist who had no information about the two groups asked the patients about the pain during the TRUS-Bx. The scale was a linear, 10-point visual analog scale of 0 to 10 cm with pain/discomfort, scored as 0: no pain, 1 to 3: mild, 4 to 6: moderate, 7 to 9: severe and 10: unbearable pain.
All patients were discharged the next day after observation for complications such as gross hematuria, rectal bleeding, voiding difficulty, or fever. A week after discharge, the patients were assessed for the results of the biopsy and other possible side effects.
Differences in the age, PSA levels, volume of the prostate, VAS scores, and complications were compared between the two treatment and control groups. The difference in pain between the two groups and other variables were analyzed by the Student's t-test. In addition, Pearson's chi-square test was used to compare frequency and complications. The p-value was accepted as significant when it was less than 0.05. All analysis was performed using SPSS® ver. 16.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Among the 74 patients, 36 in group 1 and 38 in group 2, 12 core prostate biopsies were obtained, and they were enrolled in the study for data analysis. The mean patient age, serum PSA, and total prostate volume were similar in the two groups (Table 1). Twenty six patients (35%) were diagnosed with prostate cancer; 13 patients were assigned to group 1 (36%), and 13 to group 2 (34%). There was no significant difference in cancer prevalence between the two groups.
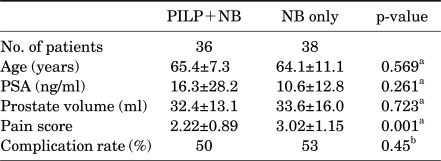
TABLE 1.
Characteristics and VAS results of patients who underwent prostate biopsy
PSA: prostate-specific antigen, VAS: visual analogue scale, PILP: perianal-intrarectal lidocaine-prilocaine, NB: nerve block, a: comparison between PILP+NB and NB only groups using the Student's t-test, b: comparison between PILP+NB and NB only groups using the Pearson chi-square test
Table 1 and Fig. 1 show the VAS scores obtained in the two groups. The mean VAS score in patients with PILP cream application prior to the PPNB was lower than that of the patients that did not receive the cream application prior to the PPNB (2.2 vs. 3.0, p=0.001).
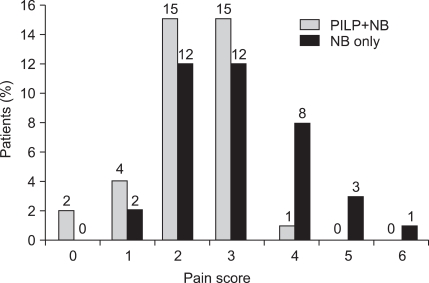
FIG. 1.
Individual pain assessment, gray (PILP+NB), black (NB only). Data are shown as the percent or number of patients with each pain score according to visual analogue scale. PILP: perianal-intrarectal lidocaine-prilocaine, NB: nerve block.
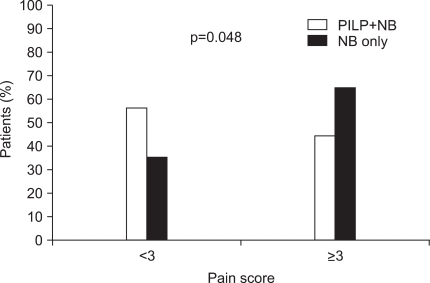
In addition, there was a difference in the number of patients that had a pain score of three or more: 44% in group 1 and 65% in group 2 (Fig. 1, 2).
FIG. 2.
Comparison in the percent of patients with pain score of ≥3 or <3 between PILP+NB and NB only groups. Data are shown as the percent of patients and the comparison between the two is performed using the Pearson chi-square test. PILP: perianal-intrarectal lidocaine-prilocaine, NB: nerve block.
No general or local adverse effects were associated with the anesthetic. There were only minor complications, such as mild hematuria, mild hematochezia and hemospermia. Thirty-three patients had gross hematuria, three patients had hematochezia, and one patient had acute urinary retention. All patients recovered with conservative management; no patient required hospitalization due to complications including sepsis. There were no differences in the complication rates between the two groups.
DISCUSSION
Although the TRUS-Bx is a standard procedure for prostate cancer detection, TURS-Bx related pain or discomfort has been reported during the procedure associated with the anorectal probe and puncture of the prostate capsule. Zisman et al. evaluated the impact of a prostate biopsy on 211 men and reported that immediate pain or discomfort was reported in 96% and 89% of their patients, respectively [6].
Pain during the TRUS-Bx can be attributed to two main factors: anal discomfort due to the ultrasound probe passed into the rectum and the insertion of needles through the prostate gland. Mostly, the prostate biopsy-related pain is caused by the needle penetrating the prostate capsule. This penetration results in periprostatic nerve stimulation of sensory receptors located in the capsule. PPNB is, therefore, a good choice to control this pain. This method has been clinically applied since 1996 when it was first reported by Nash et al, who suggested that bilateral injections at the junction of the base of the prostate and seminal vesicles provided good pain control [7]. Their positive findings were subsequently confirmed by Pareek et al and Leibovici et al [4,8]. Now, periprostatic nerve block with 1% lidocaine is considered the gold standard for analgesic anesthesia before performing an office-based prostate biopsy.
However, control of anal discomfort has not been adequate. The rectum is innervated below the dentate line by the inferior rectal branches of the pudendal nerve. Therefore, another method of pain control is needed for the anal pain.
There are many studies on the efficacy of local anesthetic agents such as lidocaine cream or jelly application. Kandirali et al reported that only perianal anesthesia with lidocaine-prilocaine cream was sufficient to decrease the pain during a TRUS-Bx [9]. Stirling et al reported that the postprocedural pain scores were significantly lower in the group that received 10 ml of 2% lidocaine gel intrarectally compared to the group that received no anesthetic; in addition, the postprocedural scores for probe insertion were significantly lower in the topical group than in the control group [10].
However, other studies did not confirm the efficacy of intrarectal lidocaine, and in some studies inferior results were obtained compared to the PPNB [11-16].
Now lidocaine gel or cream is used in combination with PPNB rather than either method alone. Giannarini et al reported that the combination of PILP cream and periprostatic nerve block provides better pain control than the cream or the PPNB alone [17].
In Korea, one study has investigated the efficacy of a combination of intrarectal lidocaine gel with PPNB [18]. This study showed that the combination of intrarectal lidocaine gel and periprostatic nerve block was effective in reducing pain during repeat prostate biopsies and the pain felt during transrectal probe insertion.
These findings are consistent with the findings of this study. A combination of PILP cream and periprostatic nerve block showed less pain than the periprostatic nerve block alone (2.22±0.89 vs. 3.02±1.15). Pain was assessed in a prospective fashion. The pain score was recorded three hours after the TRUS-Bx. Thus, recall bias was not an issue. The results of this study suggest that the combination of PILP cream and periprostatic nerve block was an effective and useful technique and well tolerated by patients.
PILP cream was chosen as the topical anesthesia because, in addition to its established efficacy and rapid absorption, it has been shown to have no side effects in prior studies [19,20]. In this study, there were no side effects associated with the PILP cream and patient compliance was good. No significant morbidity was noted in either study group. Rectal bleeding, hematuria, and hemospermia were self-limited and did not result in hospitalization or the need for additional treatment.
Lidocaine-prilocaine cream is available at most TRUS-Bx centers, and its use for prostate biopsy procedures is safe and easy. Except for the rare patient with allergies to local anesthesia, PILP cream prior to PPNB should be considered in all men undergoing TRUS-Bx.
The limitations of this study include the following. The study had a small number of patients and there was little difference among the pain scores. After the findings showed less pain in the combination group, PILP cream was applied in all patients undergoing TRUS-Bx. Thus, we could no longer recruit patients.
However, to our knowledge, this is the first domestic report on the combined effect of lidocaine-prilocaine cream with PPNB on pain control during TRUS-Bx. The numerical difference in the pain score was small but statistically meaningful. Prior studies have shown similar pain scores and differences between anesthetic methods [17,18]. Moreover, a difference was also found in the number of patients with three or more on the pain score, 44% in group 1, and 65% in group 2. The frequency of moderate to severe pain was significantly lower in the combination group.
CONCLUSIONS
A combination of lidocaine-prilocaine cream and a periprostatic nerve block was safe and effective for pain control in patients undergoing TURS-Bx. A periprostatic nerve block plus lidocaine-prilocaine cream can be considered for patients undergoing TURS-Bx.
Footnotes
The authors have nothing to disclose.
References
- 1.Collins GN, Lloyd SN, Hehir M, McKelvie GB. Multiple transrectal ultrasound-guided prostatic biopsies--true morbidity and patient acceptance. Br J Urol. 1993;71:460–463. doi: 10.1111/j.1464-410x.1993.tb15993.x. [DOI] [PubMed] [Google Scholar]
- 2.Clements R, Aideyan OU, Griffiths GJ, Peeling WB. Side effects and patient acceptability of transrectal biopsy of the prostate. Clin Radiol. 1993;47:125–126. doi: 10.1016/s0009-9260(05)81188-2. [DOI] [PubMed] [Google Scholar]
- 3.Jones JS, Ulchaker JC, Nelson D, Kursh ED, Kitay R, Angie S, et al. Periprostatic local anesthesia eliminates pain of office-based transrectal prostate biopsy. Prostate Cancer Prostatic Dis. 2003;6:53–55. doi: 10.1038/sj.pcan.4500630. [DOI] [PubMed] [Google Scholar]
- 4.Pareek G, Armenakas NA, Fracchia JA. Periprostatic nerve blockade for transrectal ultrasound guided biopsy of the prostate: a randomized, double-blind, placebo controlled study. J Urol. 2001;166:894–897. [PubMed] [Google Scholar]
- 5.Kaver I, Mabjeesh NJ, Matzkin H. Randomized prospective study of periprostatic local anesthesia during transrectal ultrasound-guided prostate biopsy. Urology. 2002;59:405–408. doi: 10.1016/s0090-4295(01)01538-2. [DOI] [PubMed] [Google Scholar]
- 6.Zisman A, Leibovici D, Kleinmann J, Siegel YI, Lindner A. The impact of prostate biopsy on patient well-being: a prospective study of pain, anxiety and erectile dysfunction. J Urol. 2001;165:445–454. doi: 10.1097/00005392-200102000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Nash PA, Bruce JE, Indudhara R, Shinohara K. Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J Urol. 1996;155:607–609. [PubMed] [Google Scholar]
- 8.Leibovici D, Zisman A, Siegel YI, Sella A, Kleinmann J, Lindner A. Local anesthesia for prostate biopsy by periprostatic lidocaine injection: a double-blind placebo controlled study. J Urol. 2002;167:563–565. doi: 10.1016/S0022-5347(01)69086-4. [DOI] [PubMed] [Google Scholar]
- 9.Kandirali E, Ulukaradag E, Uysal B, Serin E, Semercioz A, Metin A. Is only perianal anesthesia with lidocaine-prilocaine cream sufficient to decrease the pain during transrectal ultrasound-guided prostate biopsy? A prospective randomized study. Urol Int. 2009;82:262–265. doi: 10.1159/000209354. [DOI] [PubMed] [Google Scholar]
- 10.Stirling BN, Shockley KF, Carothers GG, Maatman TJ. Comparison of local anesthesia techniques during transrectal ultrasound-guided biopsies. Urology. 2002;60:89–92. doi: 10.1016/s0090-4295(02)01671-0. [DOI] [PubMed] [Google Scholar]
- 11.Arguelles Salido E, Congregado Ruiz CB, Conde Sanchez JM, Ruiz Zafra V, Medina Lopez RA, Campoy Martinez P. Ultrasound guided transrectal prostatic biopsy and pain. Prospective randomized study comparing lubricant gel, lidocaine gel, and anesthetic blockage of the neurovascular bundles with 1% lidocaine. Arch Esp Urol. 2008;61:579–590. doi: 10.4321/s0004-06142008000500003. [DOI] [PubMed] [Google Scholar]
- 12.Diaz Perez GA, Meza Montoya L, Morante Deza C, Pow-Sang Godoy M, Destefano Urrutia V. Pain during transrectal ultrasound guided needle biopsy of the prostate: comparison of the use or not of lidocaine gel. Actas Urol Esp. 2009;33:134–137. doi: 10.1016/s0210-4806(09)74112-9. [DOI] [PubMed] [Google Scholar]
- 13.Chang SS, Alberts G, Wells N, Smith JA, Jr, Cookson MS. Intrarectal lidocaine during transrectal prostate biopsy: results of a prospective double-blind randomized trial. J Urol. 2001;166:2178–2180. doi: 10.1016/s0022-5347(05)65529-2. [DOI] [PubMed] [Google Scholar]
- 14.Song SH, Ji YH, Lee SB, You DS, Kim JK, Park JY, et al. A prospective randomized study comparing effectiveness of local anesthesia techniques in patients undergoing transrectal ultrasound-guided prostate biopsy. Korean J Urol. 2004;45:236–239. [Google Scholar]
- 15.Lee YI, Seo IY, Jeong HJ, Rim JS. Comparison of two local anesthestic methods for transrectal ultrasound guided prostate biopsy: periprostatic injection of lidocaine and rectal instillation of lidocaine gel. Korean J Urol. 2004;45:423–427. [Google Scholar]
- 16.Matlaga BR, Lovato JF, Hall MC. Randomized prospective trial of a novel local anesthetic technique for extensive prostate biopsy. Urology. 2003;61:972–976. doi: 10.1016/s0090-4295(03)00003-7. [DOI] [PubMed] [Google Scholar]
- 17.Giannarini G, Autorino R, Valent F, Mogorovich A, Manassero F, De Maria M, et al. Combination of perianal-intrarectal lidocaine-prilocaine cream and periprostatic nerve block for pain control during transrectal ultrasound guided prostate biopsy: a randomized, controlled trial. J Urol. 2009;181:585–591. doi: 10.1016/j.juro.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Park SM, Hong SJ, Roh SH. The effects of combination of intrarectal lidocaine-gel with periprostatic lidocaine injection on the pain relief in repeated transrectal prostate biopsy. Korean J Urol. 2005;46:1051–1056. [Google Scholar]
- 19.Raber M, Scattoni V, Roscigno M, Rigatti P, Montorsi F. Perianal and intrarectal anaesthesia for transrectal biopsy of the prostate: a prospective randomized study comparing lidocaine-prilocaine cream and placebo. BJU Int. 2005;96:1264–1267. doi: 10.1111/j.1464-410X.2005.05830.x. [DOI] [PubMed] [Google Scholar]
- 20.De Maria M, Mogorovich A, Giannarini G, Manassero F, Selli C. Lidocaine-prilocaine administration during transrectal ultrasound-guided prostatic biopsy: a randomized, single-blind, placebo-controlled trial. J Endourol. 2006;20:525–529. doi: 10.1089/end.2006.20.525. [DOI] [PubMed] [Google Scholar]