Abstract
Purpose
We evaluated the feasibility of a laparoendoscopic single-site (LESS) nephroureterectomy for an upper urinary tract tumor.
Materials and Methods
Between March 2009 and September 2009, 4 patients with upper urinary tract tumors underwent LESS nephroureterectomy. The mean age of the 2 female and 2 male patients was 69 years old, and their mean body mass index was 23.0. We used a homemade single-port device made with a surgical glove and a wound retractor, which were put into a 4 cm periumbilical incision. Operations with articulating and rigid laparoscopic instruments were performed transperitoneally. An open technique with a 4 cm additional midline incision and laparoscopic technique with an endoscopic stapler were used for the treatment of the distal ureter and bladder cuff.
Results
All cases were completed successfully, without conversion to conventional laparoscopy or open surgery. The mean operative time was 169.5 minutes. The mean estimated blood loss was 361.4 ml. One patient had transfusion and wound infection. The mean hospital stay was 7.8 days. The mean specimen weight and tumor size were 271.8 g and 2.9 cm. Pathologic results of all cases showed urothelial carcinoma with a negative surgical margin. Three patients were in stage T3N0M0 and 1 was in stage T2N0M0.
Conclusions
Our initial experience shows that LESS nephroureterectomy with a homemade single-port device is technically feasible. However, long term follow-up for the effect on cancer control and technical development for comfortable surgery are needed.
Keywords: Kidney neoplasms, Laparoscopy, Nephrectomy, Ureteral neoplasms
INTRODUCTION
Since Clayman et al performed the first nephrectomy by laparoscopy, laparoscopic nephroureterectomy for urothelial tumors of the upper urinary tract has been performed as a less invasive operation [1-4]. Oncologic results of laparoscopic nephroureterectomy are comparable to open nephroureterectomy, and technical modifications include retroperitoneal, transperitoneal, and hand-assisted approaches [5-7].
Laparoendoscopic single-site (LESS) surgery in urology produces a smaller incision, which improves postoperative recovery and cosmesis [8,9]. We tested the feasibility of LESS nephroureterectomy with a homemade port device for urothelial tumors of the upper urinary tract. The operative results were compared to those of conventional laparoscopic nephroureterectomy.
MATERIALS AND METHODS
Between March, 2009, and April, 2010, 45 patients underwent LESS renal surgery. Among of them, 4 patients underwent nephroureterectomy for urothelial tumors of the upper urinary tract. The mean age of the 2 female and 2 male patients was 69 years (range, 64-73 years) old, and their mean body mass index was 23.0 (range, 16.5-26.7). Two patients had renal pelvic tumors, and 2 patients had ureteral tumors. The diagnosis of ureter tumors was confirmed by ureteroscopic biopsy.
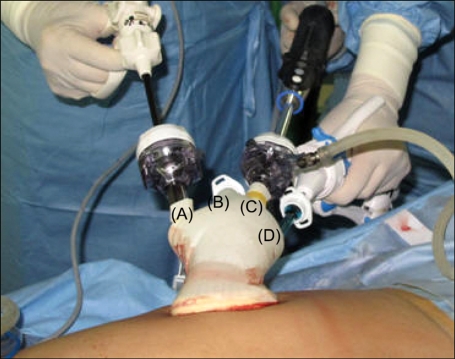
The operation was performed transperitoneally. The patient was positioned in a 70-degree lateral position. A 4 cm periumbilical incision was made, and a small sized Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) was inserted into the peritoneal cavity. A homemade single-port device was made with a size 6 surgical glove, which was attached to the outer ring of the wound retractor. Four trocars were inserted into the glove and fixed by rubber bands. After carbon dioxide insufflation to maintain an intraperitoneal pressure of 15 mmHg, a 30-degree, 10 mm laparoscope (EndoEye; Olympus Optical, Tokyo, Japan) was inserted into the peritoneal cavity. The operation was performed with standard 5 mm laparoscopic instruments, ultrasonic scissors (SonoSurg; Olympus Optical, Tokyo, Japan), and 5 mm articulating instruments (Cambridge Endo, Framingham, MA, USA) (Fig. 1).
FIG. 1.
Homemade single-port device for right nephroureterectomy. (A) A 12 mm trocar for the right hand of the operator is used for scissors, ultrasonic scissors, or endo GIA staplers. (B) A 5 mm trocar for the assistant, used as a sucker and irrigator, or retractor. (C) A 10 mm trocar for the camera holder, used for a 30 degree laparoscope (EndoEye). (D) A 5 mm trocar for the left hand of the operator, used for articulating instruments.
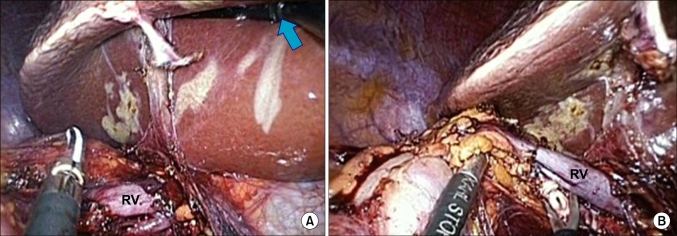
Nephrectomy was performed in a standard manner. The upper ureter was identified in the retroperitoneal fat medial to the psoas muscle. The ureter was dissected proximally and clamped with Hem-o-lok clips (Teleflex Medical, Research Triangle Park, NC, USA) to prevent tumor spread. The gonadal vein was treated in the same manner as the ureter. During the cephalad dissection, lymphadenectomy including the para-aortic and pelvic lymph nodes was performed. For the right nephrectomy, an articulating forceps could be used for liver retraction during the hilar dissection. The renal artery was dissected circumferentially using the ultrasonic scissors and secured with Hemo-lok clips (Fig. 2). The renal vein was treated with a 35 mm vascular endoscopic GIA stapler (Ethicon EndoSurgery, Cincinnati, OH, USA). To dissect the superior margin, the dissected kidney was retracted downward using the grasping forceps. Dissection between the inferior border of the spleen or liver and the kidney was completed. After completion of the nephrectomy, the distal ureter was dissected toward the bladder.
FIG. 2.
Operative findings. (A) An articulating forceps (arrow) is used for liver retraction during the hilar dissection. (B) The renal artery is cut with standard laparoscopic scissors. RV: renal vein.
For treatment of the distal ureter and bladder cuff in the ureteral tumor, a 4 cm lower abdominal midline incision was added to the periumbilical incision. The distal ureter and bladder cuff were transected with an open technique including incision and suture. An open wound retractor and bladder filling assisted the operative procedure. For the renal pelvic tumor, the distal ureter was dissected to the bladder without an additional incision. The detrusor muscle was incised along the distal ureter after dissection of perivesical tissue. An articulating endoscopic GIA stapler was used to transect the bladder cuff while retracting the ureter proximally. A Jackson-Pratt drain was left in the working space and fixed through the periumbilical incision.
RESULTS
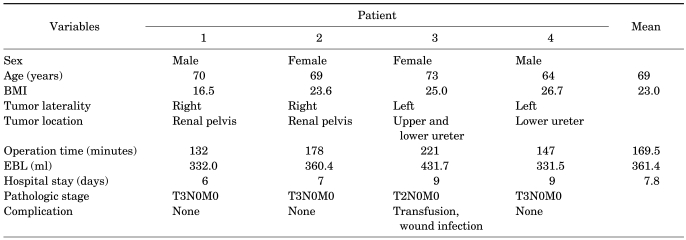
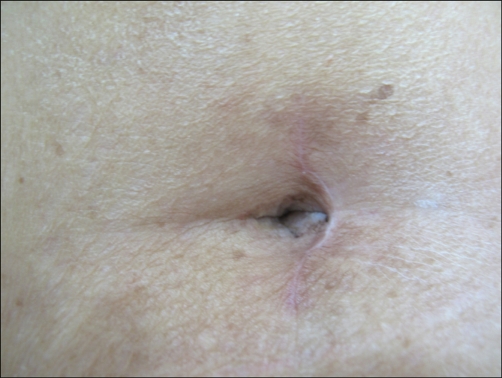
All operations were completed successfully without conversion to standard laparoscopy or open surgery. The mean operative time was 169.5 minutes (range, 132-221 minutes). The mean estimated blood loss was 361.4 ml (range, 322.0-431.7 ml). Postoperative pain control was done by a patient control analgesia (PCA) with 40 mg morphine and 150 mg ketorolac for 2 days. A diclofenac injection was added for two patients. The mean postoperative time to initiate ambulation and diet were 1.25 days (range, 1-2 days) and 1.5 days (range, 1-3 days), respectively. The mean hospital stay was 7.8 days (range, 6-9 days). One patient had complications of transfusion and wound infection (Table 1). She previously had a lower midline operative scar due to lower anterior resection of rectal cancer. The LESS incision overlapped the previous scar and resulted in a wound infection. The other 3 patients were satisfied with their small wound (Fig. 3).
TABLE 1.
Patient characteristics and operative results
BMI: body mass index (kg/m2), EBL: estimated blood loss
FIG. 3.
Operative scar 3 months after a laparoendoscopic single-site (LESS) nephroureterectomy. The distal ureter and bladder cuff were treated with an endoscopic stapler without an additional lower midline incision.
The mean specimen weight and tumor size were 271.8 g (range, 120.0-453.5 g) and 2.9 cm (range, 1.2-5.0 cm), respectively.
Pathologic results of all cases showed urothelial carcinoma with a negative surgical margin. Pathologic stages in the 2 cases of renal pelvic tumor were at stage T3N0M0 with high-grade urothelial carcinoma. The 2 cases of ureteral tumor were at stage T3N0M0 with high-grade urothelial carcinoma and T2N0M0 with low-grade urothelial carcinoma. The 3 patients in stage T3N0M0 were treated with adjuvant cisplatin-based chemotherapy.
DISCUSSION
Surgery has moved toward a minimally invasive approach, such as laparoscopic surgery. Single-incision laparoscopic surgery has superior cosmetic results and faster recovery than standard laparoscopic surgery [10]. Single-incision laparoscopic surgery is named LESS after consensus in Cleveland [11]. Since Raman et al reported the first LESS nephrectomy, successful cases of LESS radical nephrectomy, partial nephrectomy, and donor nephrectomy have been reported [12-15]. However, LESS nephroureterectomy for upper urinary tract tumors has rarely been reported.
We have performed LESS renal surgery. Our initial experience with LESS nephroureterectomy has distinguishing features. An important issue related to nephroureterectomy is the excision of the distal ureter and bladder cuff [6,16,17]. We chose an open excision through an additional lower midline incision for the ureteral tumor, and a laparoscopic treatment with an endoscopic stapler for the renal pelvic tumor. These methods could reduce operative time and improve cosmesis and oncological outcomes. However the lower abdominal midline incision was not acceptable for women. We have recently tried a transverse lower abdominal incision just on the symphysis pubis. This may have greater cosmetic advantage, but it requires another incision. The laparoscopic treatment with an endoscopic stapler may have argument of complete removal including the ureteral orifice. However, it can be confirmed with flexible cystoscopy [6].
Although LESS is a minimally invasive surgery, it requires the development of instruments and operative techniques. Various forms of single-site devices have been used for LESS. We used a homemade, single-site device because a commercial single-port was not available in Korea at the time of the operation [18,19]. Although it took time to make and insert the device into the peritoneal cavity, it is a low-cost device. We used a 10 mm laparoscope, EndoEye, with an integrated coaxial camera head and light cable to provide high-definition images without changing illumination in the bleeding field, which had a 5 mm laparoscope. For liver retraction during right nephrectomy, an articulating instrument is useful. While lifting the liver with the curved portion of the instrument, the tip portion is able to pick or dissect the tissue.
Although we present limited, retrospective data with a small number of cases, the operative data are comparable to those of conventional laparoscopy in our study. This method may provide an alternative operation to standard laparoscopic nephroureterectomy for upper urinary tract tumors. However, it will be based on developing instruments and operative techniques.
CONCLUSIONS
Our initial experience shows that LESS nephroureterectomy for upper urinary tract tumors is technically feasible. However, it demands a great deal of experience and follow-up results to be an alternative operation and to obtain oncological effectiveness. Development of instruments and operative techniques are also needed.
Footnotes
The authors have nothing to disclose.
References
- 1.Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg. 1991;1:343–349. doi: 10.1089/lps.1991.1.343. [DOI] [PubMed] [Google Scholar]
- 2.McDougall EM, Clayman RV, Elashry O. Laparoscopic nephroureterectomy for upper tract transitional cell cancer: the Washington University experience. J Urol. 1995;154:975–979. doi: 10.1016/s0022-5347(01)66949-0. [DOI] [PubMed] [Google Scholar]
- 3.Janetschek G, Reissigl A, Peschel R, Bartsch G. Laparoscopic nephroureterectomy. Br J Urol. 1993;72:987–988. doi: 10.1111/j.1464-410x.1993.tb16326.x. [DOI] [PubMed] [Google Scholar]
- 4.Seo IY, Yu DW, Oh GJ, Rim JS. Early experience of retroperitoneoscopic nephroureterectomy for transitional cell carcinoma of renal pelvis and ureter. Korean J Urol. 2006;47:1263–1268. [Google Scholar]
- 5.Rassweiler JJ, Schulze M, Marrero R, Frede T, Palou Redorta J, Bassi P. Laparoscopic nephroureterectomy for upper urinary tract transitional cell carcinoma: is it better than open surgery? Eur Urol. 2004;46:690–697. doi: 10.1016/j.eururo.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Hattori R, Yoshino Y, Gotoh M, Katoh M, Kamihira O, Ono Y. Laparoscopic nephroureterectomy for transitional cell carcinoma of renal pelvis and ureter: Nagoya experience. Urology. 2006;67:701–705. doi: 10.1016/j.urology.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Bariol SV, Stewart GD, McNeill SA, Tolley DA. Oncological control following laparoscopic nephroureterectomy: 7-year outcome. J Urol. 2004;172:1805–1808. doi: 10.1097/01.ju.0000140995.44338.58. [DOI] [PubMed] [Google Scholar]
- 8.Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008;180:637–641. doi: 10.1016/j.juro.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 9.Steinway ML, Lengu IJ, Cherullo EE, Ponsky LE. Laparoendoscopic single-site (LESS) nephrectomy through a Pfannenstiel incision: porcine model. J Endourol. 2009;23:1293–1296. doi: 10.1089/end.2009.0091. [DOI] [PubMed] [Google Scholar]
- 10.Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol. 2008;5:561–568. doi: 10.1038/ncpuro1215. [DOI] [PubMed] [Google Scholar]
- 11.Gettman MT, Box G, Averch T, Cadeddu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: heralding a new era in urology? Eur Urol. 2008;53:1117–1120. doi: 10.1016/j.eururo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Raman JD, Bensalah K, Bagrodia A, Stern JM, Cadeddu JA. Laboratory and clinical development of single keyhole umbilical nephrectomy. Urology. 2007;70:1039–1042. doi: 10.1016/j.urology.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Raybourn JH, 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010;75:100–103. doi: 10.1016/j.urology.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 15.Aron M, Canes D, Desai MM, Haber GP, Kaouk JH, Gill IS. Transumbilical single-port laparoscopic partial nephrectomy. BJU Int. 2009;103:516–521. doi: 10.1111/j.1464-410X.2008.08007.x. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal DK, Khaira HS, Clarke D, Tong R. Modified transurethral technique for the management of distal ureter during laparoscopic assisted nephroureterectomy. Urology. 2008;71:740–743. doi: 10.1016/j.urology.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 17.Srirangam SJ, van Cleynenbreugel B, van Poppel H. Laparoscopic nephroureterectomy: the distal ureteral dilemma. Adv Urol. 2009:316807. doi: 10.1155/2009/316807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park YH, Kang MY, Jeong MS, Choi H, Kim HH. Laparoendoscopic single-site nephrectomy using a homemade single-port device for single-system ectopic ureter in a child: initial case report. J Endourol. 2009;23:833–835. doi: 10.1089/end.2009.0025. [DOI] [PubMed] [Google Scholar]
- 19.Jeong W, Jeon HG, Yu HS, Kim KH, Yang SC, Rha KH, et al. Embryonic-natural orifice transluminal endoscopic surgery nephrectomy. Korean J Urol. 2009;50:609–612. [Google Scholar]