Abstract
We found recently that endogenous (free fatty acids) and pharmacological (thiazolidinediones) agonists of nuclear receptor Peroxisome Proliferator-Activated Receptor-γ (PPARγ) stimulate renin transcription. In addition, the renin gene was identified as a direct target of PPARγ. The mouse renin gene is regulated by PPARγ through a distal enhancer direct repeat closely related to consensus PPAR response element (PPRE). In vitro studies demonstrated that PPARγ knockdown stimulated PPRE-driven transcription. These data predicted that deficiency of PPARγ would up-regulate mouse renin expression. Consistent with these observations knockdown of PPARγ increased the transcription of a reporter gene driven by the mouse renin PPRE-like motif in vitro. To study the impact of PPARγ on renin production in vivo we used a cre/lox system to generate double-transgenic mice with disrupted PPARγ locus in renin-producing juxtaglomerular (JG) cells of the kidney (RC-PPARγfl/fl mice). We provide evidence that PPARγ expression was effectively reduced in JG cells of RC-PPARγfl/fl mice. Fluorescent immunohistochemistry showed stronger renin signal in RC-PPARγfl/fl than in littermate control RC-PPARγwt/wt mice. Renin mRNA levels and plasma renin concentration in RC-PPARγfl/fl mice were almost two fold higher than in littermate controls. Arterial blood pressure and pressure control of renal vascular resistance, which play decisive roles in the regulation of renin production were indistinguishable between RC-PPARγwt/wt and RC-PPARγfl/fl mice. These data demonstrate that the JG-specific PPARγ deficiency results in increased mouse renin expression in vivo thus corroborating earlier in vitro results. PPARγ appears to be a relevant transcription factor for the control of renin gene in JG cells.
Keywords: Basic science, Gene expression/regulation, Hypertension (Kidney), Renin, Cell signaling
INTRODUCTION
The nuclear receptor Peroxisome Proliferator-Activated Receptor-γ PPARγ) is the molecular master switch of adipocyte growth and differentiation,1 but an important role of PPARγ in the cardiovascular system is gaining recognition.2,3 A series of compelling studies has demonstrated that PPARγ is involved in the regulation of vascular tone and in the pathogenesis of vascular diseases such as arterial hypertension or atherosclerosis.2–6 Thiazolidinediones (TZDs), which are pharmacological PPARγ agonists, have various and to some extent opposing effects on blood pressure, vascular permeability and cardiac function.2,3,6–10
Renin is a key factor in the regulation of blood pressure and fluid/electrolyte homeostasis.11 Renin is produced mainly in the kidney cortex by a small population of epithelial-like cells called “juxtaglomerular” (JG) located in the glomerular end of the afferent arteriole. The transcription of the renin gene is one of the regulated check-points in the overall renin synthesis.12 We recently identified PPARγ as a transcription factor which controls renin expression in renin-producing cells.13,14 We hypothesize that the effect of PPARγ on renin gene transcription is an additional molecular mechanism whereby PPARγ influences the function of the cardiovascular system.
PPARγ targets two functionally different cis-acting elements in the 5′-flanking region of the renin promoter. First, a direct repeat motif highly similar to canonical PPAR response element (PPRE) is located in a distal regulatory region known as the renal renin enhancer.13,15 We identified a second, atypical PPARγ-binding site termed Pal3 in the proximal renin promoter.13 Thus, the renin gene contains two diverse and widely-separated PPARγ-binding sequences. The renin Pal3 and PPRE motifs have different protein-binding and functional properties.14 The proximal promoter Pal3 site is decisive for the regulation of human renin transcription. On the contrary, the mouse renin gene was targeted by PPARγ through the enhancer PPRE-like sequence since the mouse Pal3 element was transcriptionally silent in response to PPARγ activation. PPARγ knockdown decreased Pal3-driven transcription, but unexpectedly increased PPRE-driven transcription in renin-producing cells.14 The increase of PPRE-driven transcription upon PPARγ deficiency correlated with increased protein binding to PPRE (presumably of other nuclear receptors) which phenomenon was not observed with Pal3.14
Altogether our findings suggested that PPARγ influences renin transcription in a species-dependent manner.14 Because the information regarding PPARγ was obtained using in vitro systems, it is necessary to determine whether PPARγ regulates renin expression in vivo. To study the in vivo relevance of PPARγ in the cellular control of renin gene expression we used a conditional deletion. This approach provides an opportunityto discriminate the role of PPARγ in the cellular control of renin transcription from PPARγ-dependent influence on systemic signals known to regulate renin production. We generated double-transgenic mice with a selective PPARγ knockout in the renin-producing cells.
METHODS
Cell culture
Human renin-producing Calu-6 cells (ATCC-HTB-56) were cultured in Eagle’s minimal essential medium supplemented with 10% fetal bovine serum, sodium pyruvate, 100 U/ml penicillin, 100 μg/ml streptomycin, and 1% nonessential amino acids at 37° C in a humidified atmosphere containing 5% CO2.
Plasmid
The construct mPPREmPal3 represents a firefly luciferase reporter gene driven by a 46 bp long mouse renin enhancer fragment containing a cAMP response element and the PPRE-like element (originally described as Ec/Eb and also termed hormone response element- HRE)13,14 cloned into the 5′-end of the minimal human renin promoter hRenMin in which Pal3 is replaced by mouse Pal3.
Animals
The mice expressing cre recombinase under the control of endogenous renin promoter (Ren-cre) or PPARγ-floxed allele (obtained through The Jackson Laboratory) were described previously.16,17 All animal experiments were performed according to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health and were approved by the local ethics committee. Two to four months old F3 to F7 male mice were used for the experiments.
Blood pressure measurements
Systolic blood pressure was measured by the tail-cuff method. Mice were put in a steel cover on a 30°C pre-warmed platform and trained for 7 days between 9 and 12 AM before the measurement. Data from five to eight measurements per animal were averaged for a single value.
Statistics
All data are presented as mean±SEM. Differences were analyzedby ANOVA and the Student’s unpaired t test. P <0.05 was considered significant.
RESULTS
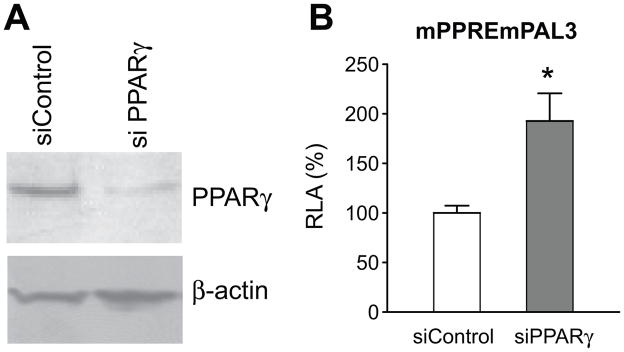
Knockdown of PPARγ up-regulates the basal activity of a reporter gene driven by the mouse renin PPRE-like sequence in vitro
We found previously that PPARγ deficiency increases PPRE-driven transcription and that mouse renin gene is targeted by PPARγ at the enhancer PPRE-like sequence.13,14 To provide further evidence that the mouse renin gene is up-regulated by PPARγ deficiency in renin-producing cells, we used a reporter driven by a human renin promoter construct containing the mouse renin enhancer PPRE-like site (mPPREmPal3). Knockdown of PPARγ by sequence-specific siRNA in the renin-producing Calu-6 cells lead to an almost two fold increase in the transcription of mPPREmPal3 construct (Figure 1A,B). These data demonstrated that the transcription of mouse renin PPRE-like-driven reporter is up-regulated by PPARγ deficiency in vitro.
Figure 1.
Effect of PPARγ knockdown on mouse renin PPRE-like driven transcription. Calu-6 cells were transfected with nontargeting siRNA as control (siControl) or with PPARγ sequence-specific siRNA (siPPARγ) and with the mPPREmPal3 construct. A. Efficacy of the PPARγ knockdown. Representative Western blots of protein extracts probed with anti-PPARγ or antiβ-actin (used for loading control) antibodies; B. Effect of PPARγ knockdown on mPPREmPal3 activity. RLA- relative luciferase activity, n=8 from two separate experiments. *P< 0.05.
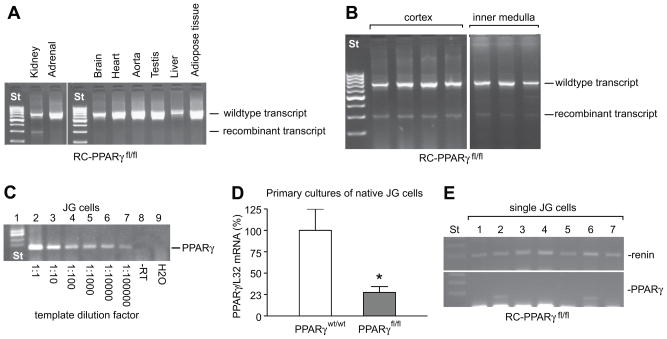
Generation of JG-specific PPARγ knockout mice
To study the role of PPARγ deficiency in the cell-specific control of the renin gene in vivo we used the cre/lox recombination system to generate mice with deletion of PPARγ in JG cells. Mice expressing cre recombinase under the control of the renin locus were crossed to a second transgenic strain in which PPARγ exons 1 and 2 were flanked by loxP sites.16,17 The floxed PPARγ allele is deleted upon expression of cre recombinase. It has been previously shown that expression of cre recombinase from the endogenous renin locus targets recombination to the renin-producing cells.17 Nine genotypes were obtained from crossing of double-heterozygous mice (please see http://hyper.ahajournals.org, Figure S1A). Since we needed endogenous renin as a readout, animals with only two of the nine possible genotypes in the offspring were used: as littermate control - mice with heterozygous renin/cre alleles and wildtype homozygous PPARγ alleles (RC-PPARγwt/wt), and as JG-specific PPARγ knockout - mice with heterozygous renin/cre alleles and floxed homozygous PPARγ alleles (RC-PPARγfl/fl). Cre-positive mice were used in all of the studies to ensure that the littermate control and the PPARγ-deficient mice contained one allele of Ren1 and one allele of Ren2 (please see http://hyper.ahajournals.org, Figure S1A). As expected, recombined PPARγ transcript was reproducibly detected only in kidneys of RC-PPARγfl/fl mice by qualitative RT-PCR (Figure 2A, please see http://hyper.ahajournals.org, Figure S1B). Besides cortex, recombination in the kidneys of RC-PPARγfl/fl mice was also detected in inner medulla where renin is known to be weakly expressed in collecting ducts (Figure 2B).17 These data demonstrated that recombination in kidney is not necessarily restricted to the JG cells, but may be present in other cell types where the renin/cre allele is also active during development (e.g. in larger arteries) or in adults.17,18 Renin-expressing cells represent a very small fraction of total cells in the adult kidney. Consistent with this, PPARγ mRNA level decreased only slightly in total kidney, cortex or medulla of adult RC-PPARγfl/fl mice (please see http://hyper.ahajournals.org, Figure S1C,D). This suggested that cre-mediated recombination in cell types other than JG would be minimal. We used single-cell RT-PCR to determine if PPARγ is expressed by JG cells. By this method we detected PPARγ mRNA in single JG cells of wildtype mice, while no signal was detected in the negative control samples thus demonstrating the specificity of the signal (Figure 2C). We also tested five different anti-PPARγ antibodies on histological kidney sections, but could not reproducibly detect any specific signal (data not shown). We next examined PPARγ expression in primary cultures of native JG cells. In these JG-cell-enriched preparations, PPARγ mRNA from RC-PPARγfl/fl was about 30 % of the level in RC-PPARγwt/wt mice (Figure 2D). These results were confirmed by single-cell RT-PCR. In this study only 30% of the JG cells (two of seven tested) isolated from RC-PPARγfl/fl animals expressed PPARγ Figure 2E), whereas all JG cells isolated from the RC-PPARγwt/wt mice were PPARγ positive (four of four tested, please see http://hyper.ahajournals.org, Figure S1E). The partial retention of PPARγ expression in JG cells of RC-PPARγfl/fl mice may be due to single-allele excision which however could not be discerned by the qualitative single cell RT-PCR. Based on these assays we concluded that PPARγ expression is efficiently knocked-out in the renin-producing JG cells of RC-PPARγfl/fl mice.
Figure 2. Recombination of PPARγ allele and PPARγ expression in RC-PPARγwt/wt and RC-PPARγfl/fl mice.
A. Qualitative PCR-based screening for PPARγ-recombined transcript in different organs of RC-PPARγfl/fl mice; B. PPARγ recombination in renal cortex and inner medulla total RNA samples isolated from RC-PPARγfl/fl mice; C. PPARγ mRNA is expressed in native JG cells of wildtype mice. Lane 1, molecular weight marker; lanes 2 to 7, RT-PCR of serial dilutions of RNA isolated from single JG cells with PPARγ-specific primers; lane 8, “minus” RT, the sample was “reverse-transcribed” in the absence of transcriptase before amplification (negative control); lane 9, water was reverse-transcribed and amplified (negative control); D. PPARγ mRNA levels in primary cultures of native JG cells isolated from RC-PPARγwt/wt (n=4) or RC-PPARγfl/fl (n=4) mice. PPARγ and ribosomal L32 (internal control) mRNA levels were quantified by real-time RT-PCR. *P < 0.05; E. Single-cell RT-PCR with renin (upper panel) or PPARγ (lower panel) specific primers of total RNA extracted from seven different JG cells of RC-PPARγfl/fl mice. The bands at the bottom of the panels represent primer dimers. St- length standard.
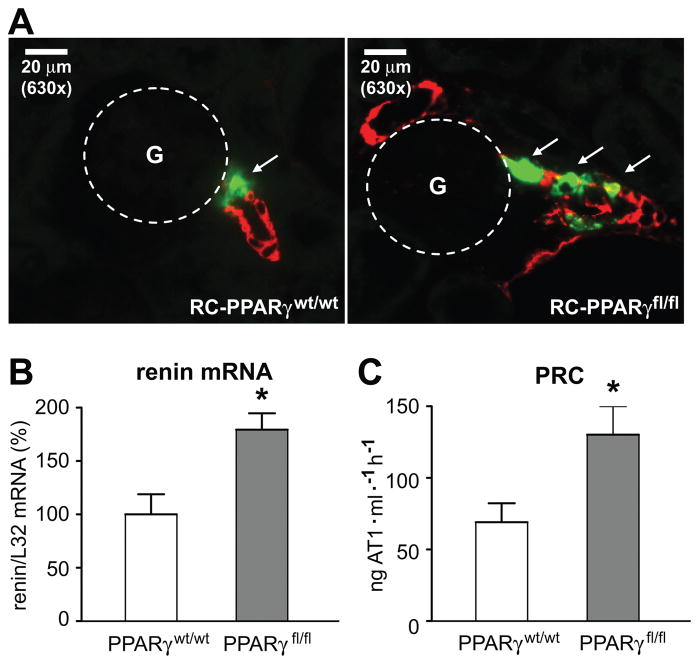
Increased renin production in RC-PPARγfl/fl mice
After confirming the correct targeting of the PPARγ knockout to the JG cells, we studied the renin production in RC-PPARγwt/wt and RC-PPARγfl/fl mice. Immunohistochemical staining of whole kidney slices revealed increased number of renin-positive glomeruli in RC-PPARγfl/fl mice compared with RC-PPARγwt/wt mice (please see http://hyper.ahajournals.org, Figure S2A,B). A few glomeruli (about 3–4, or 1–5 % of total number per slice) in RC-PPARγfl/fl mice contained renin-producing cells located not only in juxtaglomerular position, but also upstream in the afferent arteriolar wall (Figure 3A). This arrangement of the renin-producing cells, known as recruitment, is typically seen at chronic stimulation of renin expression in vivo. To confirm these semiquantitative findings we measured renal renin mRNA levels and plasma renin concentration (PRC) (Figures 3B and 3C, respectively). Both methods demonstrated unequivocally that there is a significant increase of renin in RC-PPARγfl/fl compared to RC-PPARγwt/wt mice. Allele specific TaqMan assays revealed an equivalent up-regulation of Ren1 and Ren2, and confirmed an increase in total renin mRNA (please see http://hyper.ahajournals.org, Figure S3).
Figure 3.
Renin expression in RC-PPARγwt/wt and RC-PPARγfl/fl mice. A. Co-staining for renin (green) and vascular smooth muscle α-actin (red). Dashed circles show the position of glomeruli (G), arrows indicate renin immunoreactivity; B. Renal renin mRNA levels in RC-PPARγwt/wt (n=6) and RC-PPARγfl/fl (n=8) mice. Renin and ribosomal L32 (internal control) mRNA levels were quantified by real-time RT-PCR. *P < 0.05; C. Plasma renin concentration (PRC) in RC-PPARγwt/wt (n=8) and RC-PPARγfl/fl (n=8) mice. *P < 0.05.
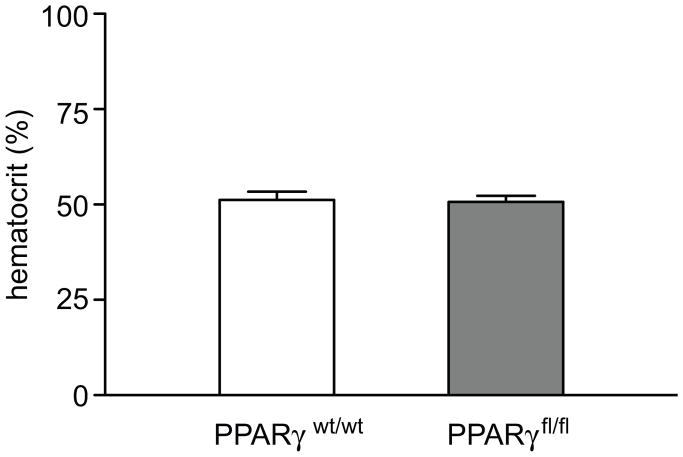
Hematocrit is not different between RC-PPARγwt/wt and RC-PPARγfl/fl mice
Recombined PPARγ transcript was detected in the inner medulla of the kidney (Figure 2B) and could be explained by the transcriptional activity of the renin gene observed in medullary structures such as collecting ducts. Notably, PPARγ is also expressed in collecting duct principal cells.19,20 PPARγ has been reported to induce the expression of γENaC-subunit and presumably the salt-water reabsorption in the terminal portion of the nephron.19,20 However, there was no difference in the hematocrits in RC-PPARγwt/wt and RC-PPARγfl/fl mice thus excluding the possibility that the recombination of PPARγ in the medulla has resulted in significant water deficit (Figure 4).
Figure 4.
Hematocrits in RC-PPARγwt/wt and RC-PPARγfl/fl mice. Blood samples were obtained through mandibular bleeding. The data are means±SD, n=8 in each group.
Arterial blood pressure and pressure-dependent control of renal blood flow are not different between RC-PPARγwt/wt and RC-PPARγfl/fl mice
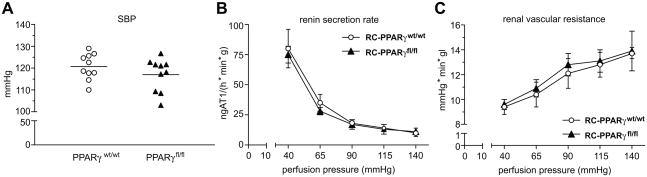
Although the finding that PPARγ deletion in JG cells results in increased renin expression in vivo is compatible with cell culture data, it is still possible that systemic or local factors are affected by the genetic manipulation and thus are responsible for the altered renin production in RC-PPARγfl/fl mice. Arterial blood pressure plays a central role in the control of renin synthesis and secretion.11 Interference with PPARγ function in the vasculature is accompanied by changes in blood pressure.4–6,21 Therefore we measured the blood pressure in conscious mice. The average systolic blood pressure (mean±SD) was not significantly different between RC-PPARγwt/wt and RC-PPARγfl/fl animals (120.7±6 versus 117±7.6 mmHg, p=0.24, Figure 5A). These data are representative for several measurements with a total of almost twenty animals per group performed either early in the morning or in the afternoon (data not shown). Therefore it is unlikely that a minor decrease in blood pressure could have stimulated renin production in RC-PPARγfl/fl mice. In addition, in the isolated perfused kidney we did not find any significant discrepancy in the pressure-dependent control of either renin release or renal vascular resistance between RC-PPARγwt/wt and RC-PPARγfl/fl mice (Figures 5B and 5C, respectively). Altogether these results suggest that baroreceptor mechanisms are not responsible for the increased renin observed in RC-PPARγfl/fl mice.
Figure 5. Arterial blood pressure and renal perfusion parameters of RC-PPARγwt/wt and RC-PPARγfl/fl mice.
A. Systolic blood pressure (SBP) measured by tail-cuff method. Each mark represents the value (average of 5 to 8 measurements) for a single animal (n=10 for each genotype); B, C. Pressure-dependent regulation of renin secretion rate (B.) and renal vascular resistance (C.) in isolated perfused kidneys of RC-PPARγwt/wt and RC-PPARγfl/fl mice, n= 3 and 4, respectively.
DISCUSSION
We have showed here that PPARγ knockdown up-regulates the transcription of a luciferase reporter driven by the mouse renin PPRE-like sequence. We found previously that RNA interference-mediated knockdown of PPARγ in the renin-producing cell line Calu-6 up-regulated the transcription of a reporter gene driven by consensus PPRE.14 Thus, similarly to PPARγ agonists,13,14 the PPARγ deficiency up-regulates the mouse renin PPRE-driven transcription. While these findings appear to be counterintuitive at first sight, they are in fact congruent to earlier data. Results from our group demonstrated that the protein binding to PPRE increases in response to PPARγ deficiency.14 Since PPRE is generally targeted by many nuclear receptors we suggested that the latter bind with higher affinity to PPRE at low cellular level of PPARγ thus resulting in stronger trans-activation. In agreement with this model knockdown of the PPARγ interaction partner retinoid X receptor-alpha (RXRα) also increased the binding to PPRE and up-regulated the PPRE-driven transcription.14 One more possible explanation provide studies on dominant-negative PPARγ mutants.22,23 In the absence of ligand, PPARγ is bound to PPRE complexed to co-repressors such as nuclear co-repressor (NCoR) and silencing mediator of retinoid and thyroid receptors (SMRT). These co-repressors are replaced by transcriptional co-activators (cAMP-response element-binding protein-binding protein, CBP and steroid receptor co-activator-1, SRC-1) upon binding of agonists to PPARγ. Dominant-negative PPARγ mutants have stronger affinity for co-repressors which interfere with the recruitment of co-activators in the presence of ligand.22,23 It is therefore possible that the knockdown of PPARγ diminishes the amount of transcriptional co-repressors bound to PPRE and thus results in trans-activation. The potential relevance of this mechanism however remains to be elucidated.
Based on these in vitro data and on our earlier findings showing that PPARγ targeted mouse renin promoter at a PPRE-like motif in the distal enhancer,13 we predicted that PPARγ deficiency should increase the expression of the mouse renin gene in vivo. To test this hypothesis we crossed two transgenic strains to obtain mice (RC-PPARγfl/fl) with a specific inactivation of PPARγ in the renin-producing JG cells by employing the cre/lox recombination system. As expected, PPARγ mRNA was significantly diminished in primary cultures of native JG cells isolated from JG-specific PPARγ knockout mice and the majority of the JG cells in these animals did not express PPARγ. This finding evidenced for the correct targeting of recombination. As predicted by the cell culture data, renin expression in kidneys of RC-PPARγfl/fl mice was increased compared to their littermate controls. Consistently, PRC in RC-PPARγfl/fl animals was also elevated. On the basis of the cell-specific gene silencing observed, the increased renin production in RC-PPARγfl/fl mice could be primarily attributed to the deficiency of PPARγ in their JG cells.
The recombination of the PPARγ allele in medullary structures such as the collecting duct, could possibly be responsible for the increased renin production in RC-PPARγfl/fl mice. Several lines of evidence suggest, however, that this scenario is quite unlikely. First, hematocrits were not different between RC-PPARγwt/wt and RC-PPARγfl/fl mice thus arguing against possible water deficit in the knockout animals. Second, the baseline plasma and urine parameters of collecting duct-specific PPARγ-deficient mice were indistinguishable from those of their inbred wildtype controls.20 Third, mice with collecting duct-selective deletion of αENaC-isoform, which is critical for the membrane translocation of the ENaC channel, neither have impaired Na+, K+ or water balance, nor were protected against TZD-induced water retention.24 We could not formally rule out that impaired tubular control of renin production through the tubular macula densa (MD) mechanism is causative for the increased renin in RC-PPARγfl/fl mice. However, MD seems to be critical for the short-term, rather than for the chronic regulation of renin synthesis.25
Recombination of PPARγ allele was observed in aortas and adrenals of RC-PPARγfl/fl animals (please see http://hyper.ahajournals.org, Figure S1B). This is in agreement with earlier data indicating that the renin promoter is active in these organs.17,26 Since recombinant transcript was detected in some, but not all, RC-PPARγfl/fl mice we suggested that this is most likely due to a “dilution” of cre/renin-expressing cells in adulthood. The same may be the case with other organs where the renin gene is expressed, such as brain or testis, but where no PPARγ recombination was found.17 Consistent with this suggestion, the robust expression of renin in the adrenal cortex during fetal life occurs mostly in the large fetal zone which regresses after birth and is replaced by other cells presumably originating from the outer cortex.27,28 In adult life, cells that expressed renin (and therefore cre recombinase) persist in some stripes along the adrenal cortex with numerous adrenal cells in between that never expressed renin and/or cre (spared zones).17
We could not exclude that PPARγ locus remained completely intact in the media cells of the afferent arteriole wall upstream of the JG cells, since renin is produced in larger arteries of the kidney during embryonic development and early postnatal life.17,18 Moreover, PPARγ is known to be expressed, albeit weakly, in the vascular media layer and the specific inactivation of PPARγ in smooth muscle cells has been reported to result in impaired vascular reactivity.5,6,21 Changes in blood pressure induce reciprocal responses in renin production in a way that increased blood pressure inhibits, while lowered blood pressure stimulates renin expression and release.11 Since renin, the limiting factor of renin-angiotensin-system (RAS), is causally involved in the regulation of blood pressure through the vasoconstrictor angiotensin II, the blood pressure-dependent control of the renin gene represents a feedback mechanism, which is decisive for the overall cardiovascular homeostasis. We provided three lines of evidence that, if present, the partial inactivation of PPARγ gene in renal and extrarenal vessels does not have impact on the pressure control of renin in RC-PPARγfl/fl mice. First, the systemic blood pressure was not significantly different between RC-PPARγwt/wt and RC-PPARγfl/fl animals. Second, the pressure-dependent control of renal blood flow and consecutively renal vascular resistance were similar in the two genotypes. Third, the pressure regulated renin release was also undistinguishable between RC-PPARγwt/wt and RC-PPARγfl/fl mice suggesting that there is no shift in the pressure/flow rate sensitivity of the PPARγ-deficient afferent arterioles. In addition, the last two findings provided indirect evidence against possible dysregulation of local vasoactive mediator systems known to control renin production such as NO, prostanoids, adenosine or endothelins in RC-PPARγfl/fl mice (please see also http://hyper.ahajournals.org, Figure S4).
One could have expected that the hyperreninemia should have increased the blood pressure in the JG-specific PPARγ knockout mice. However, transgenic mouse models demonstrated that primary changes in renin/RAS activity do not obligatory lead to blood pressure dysregulation, basically because plasma RAS is only one of the players in the complex regulation of circulation.29–31
Thus, the most plausible explanation for the increased renin expression in RC-PPARγfl/fl mice which we report here is the deficiency of PPARγ in the renin-producing cells. On the basis of the compatible in vitro and in vivo data we conclude that the deficiency of PPARγ in renin-producing cells increases the expression of the mouse renin gene.
PERSPECTIVES
The results presented here provide evidence that PPARγ is relevant for the regulation of renin transcription in JG cells in vivo. Our data demonstrated that RC-PPARγfl/fl mice could be used as a model for studying the PPARγ in the regulation of renin production in vivo and validated previous cell culture findings.13,14 The in vitro results predicted also discrepant mode of action of PPARγ on mouse and human genes.14 Therefore we are currently working on a transgenic model which should reveal whether PPARγ regulates the expression of the renin gene in a species-specific manner.
Supplementary Material
Acknowledgments
The expert technical assistance of Anna M’Bangui, Anelia Todorova, Katharina Ehm, Marlies Hamann, Sandra Mayer and Sabine Harlander is gratefully acknowledged.
Source of Funding: Deutsche Forschungsgemeinschaft, Sonderforschungsbereich 699, Project B1.
Footnotes
Conflict of Interest/Disclosures: NONE
References
- 1.Rosen ED, Walkey CJ, Puigserver P, Spiegelman BM. Transcriptional regulation of adipogenesis. Genes Dev. 2000;14:1293–1307. [PubMed] [Google Scholar]
- 2.Duan SZ, Usher MG, Mortensen RM. Peroxisome proliferator-activated receptor-gamma-mediated effects in the vasculature. Circ Res. 2008;102:283–294. doi: 10.1161/CIRCRESAHA.107.164384. [DOI] [PubMed] [Google Scholar]
- 3.Halabi CM, Sigmund CD. Peroxisome proliferator-activated receptor-gamma and its agonists in hypertension and atherosclerosis: mechanisms and clinical implications. Am J Cardiovasc Drugs. 2005;5:389–398. doi: 10.2165/00129784-200505060-00006. [DOI] [PubMed] [Google Scholar]
- 4.Duan SZ, Ivashchenko CY, Whitesall SE, D’Alecy LG, Duquaine DC, Brosius FC, 3rd, Gonzalez FJ, Vinson C, Pierre MA, Milstone DS, Mortensen RM. Hypotension, lipodystrophy, and insulin resistance in generalized PPARgamma-deficient mice rescued from embryonic lethality. J Clin Invest. 2007;117:812–822. doi: 10.1172/JCI28859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halabi CM, Beyer AM, de Lange WJ, Keen HL, Baumbach GL, Faraci FM, Sigmund CD. Interference with PPAR gamma function in smooth muscle causes vascular dysfunction and hypertension. Cell Metab. 2008;7:215–226. doi: 10.1016/j.cmet.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang N, Yang G, Jia Z, Zhang H, Aoyagi T, Soodvilai S, Symons JD, Schnermann JB, Gonzalez FJ, Litwin SE, Yang T. Vascular PPARgamma controls circadian variation in blood pressure and heart rate through Bmal1. Cell Metab. 2008;8:482–491. doi: 10.1016/j.cmet.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duan SZ, Ivashchenko CY, Russell MW, Milstone DS, Mortensen RM. Cardiomyocyte-specific knockout and agonist of peroxisome proliferator-activated receptor-gamma both induce cardiac hypertrophy in mice. Circ Res. 2005;97:372–379. doi: 10.1161/01.RES.0000179226.34112.6d. [DOI] [PubMed] [Google Scholar]
- 8.Nesto RW, Bell D, Bonow RO, Fonseca V, Grundy SM, Horton ES, Le Winter M, Porte D, Semenkovich CF, Smith S, Young LH, Kahn R. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Circulation. 2003;108:2941–2948. doi: 10.1161/01.CIR.0000103683.99399.7E. [DOI] [PubMed] [Google Scholar]
- 9.Ryan MJ, Didion SP, Mathur S, Faraci FM, Sigmund CD. PPAR(gamma) agonist rosiglitazone improves vascular function and lowers blood pressure in hypertensive transgenic mice. Hypertension. 2004;43:661–666. doi: 10.1161/01.HYP.0000116303.71408.c2. [DOI] [PubMed] [Google Scholar]
- 10.Zanchi A, Chiolero A, Maillard M, Nussberger J, Brunner HR, Burnier M. Effects of the peroxisomal proliferator-activated receptor-gamma agonist pioglitazone on renal and hormonal responses to salt in healthy men. J Clin Endocrinol Metab. 2004;89:1140–1145. doi: 10.1210/jc.2003-031526. [DOI] [PubMed] [Google Scholar]
- 11.Hackenthal E, Paul M, Ganten D, Taugner R. Morphology, physiology, and molecular biology of renin secretion. Physiol Rev. 1990;70:1067–1116. doi: 10.1152/physrev.1990.70.4.1067. [DOI] [PubMed] [Google Scholar]
- 12.Pan L, Gross KW. Transcriptional regulation of renin: an update. Hypertension. 2005;45:3–8. doi: 10.1161/01.HYP.0000149717.55920.45. [DOI] [PubMed] [Google Scholar]
- 13.Todorov VT, Desch M, Schmitt-Nilson N, Todorova A, Kurtz A. Peroxisome proliferator-activated receptor-gamma is involved in the control of renin gene expression. Hypertension. 2007;50:939–944. doi: 10.1161/HYPERTENSIONAHA.107.092817. [DOI] [PubMed] [Google Scholar]
- 14.Todorov VT, Desch M, Schubert T, Kurtz A. The Pal3 promoter sequence is critical for the regulation of human renin gene transcription by peroxisome proliferator-activated receptor-gamma. Endocrinology. 2008;149:4647–4657. doi: 10.1210/en.2008-0127. [DOI] [PubMed] [Google Scholar]
- 15.Shi Q, Gross KW, Sigmund CD. Retinoic acid-mediated activation of the mouse renin enhancer. J Biol Chem. 2001;276:3597–3603. doi: 10.1074/jbc.M008361200. [DOI] [PubMed] [Google Scholar]
- 16.He W, Barak Y, Hevener A, Olson P, Liao D, Le J, Nelson M, Ong E, Olefsky JM, Evans RM. Adipose-specific peroxisome proliferator-activated receptor gamma knockout causes insulin resistance in fat and liver but not in muscle. Proc Natl Acad Sci U S A. 2003;100:15712–15717. doi: 10.1073/pnas.2536828100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sequeira Lopez ML, Pentz ES, Nomasa T, Smithies O, Gomez RA. Renin cells are precursors for multiple cell types that switch to the renin phenotype when homeostasis is threatened. Dev Cell. 2004;6:719–728. doi: 10.1016/s1534-5807(04)00134-0. [DOI] [PubMed] [Google Scholar]
- 18.Sauter A, Machura K, Neubauer B, Kurtz A, Wagner C. Development of renin expression in the mouse kidney. Kidney Int. 2008;73:43–51. doi: 10.1038/sj.ki.5002571. [DOI] [PubMed] [Google Scholar]
- 19.Guan Y, Hao C, Cha DR, Rao R, Lu W, Kohan DE, Magnuson MA, Redha R, Zhang Y, Breyer MD. Thiazolidinediones expand body fluid volume through PPARgamma stimulation of ENaC-mediated renal salt absorption. Nat Med. 2005;11:861–866. doi: 10.1038/nm1278. [DOI] [PubMed] [Google Scholar]
- 20.Zhang H, Zhang A, Kohan DE, Nelson RD, Gonzalez FJ, Yang T. Collecting duct-specific deletion of peroxisome proliferator-activated receptor gamma blocks thiazolidinedione-induced fluid retention. Proc Natl Acad Sci U S A. 2005;102:9406–9411. doi: 10.1073/pnas.0501744102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang L, Villacorta L, Zhang J, Garcia-Barrio MT, Yang K, Hamblin M, Whitesall SE, D’Alecy LG, Chen YE. Vascular smooth muscle cell-selective peroxisome proliferator-activated receptor-gamma deletion leads to hypotension. Circulation. 2009;119:2161–2169. doi: 10.1161/CIRCULATIONAHA.108.815803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barroso I, Gurnell M, Crowley VE, Agostini M, Schwabe JW, Soos MA, Maslen GL, Williams TD, Lewis H, Schafer AJ, Chatterjee VK, O’Rahilly S. Dominant negative mutations in human PPARgamma associated with severe insulin resistance, diabetes mellitus and hypertension. Nature. 1999;402:880–883. doi: 10.1038/47254. [DOI] [PubMed] [Google Scholar]
- 23.Gurnell M, Wentworth JM, Agostini M, Adams M, Collingwood TN, Provenzano C, Browne PO, Rajanayagam O, Burris TP, Schwabe JW, Lazar MA, Chatterjee VK. A dominant-negative peroxisome proliferator-activated receptor gamma (PPARgamma) mutant is a constitutive repressor and inhibits PPARgamma-mediated adipogenesis. J Biol Chem. 2000;275:5754–5759. doi: 10.1074/jbc.275.8.5754. [DOI] [PubMed] [Google Scholar]
- 24.Vallon V, Hummler E, Rieg T, Pochynyuk O, Bugaj V, Schroth J, Dechenes G, Rossier B, Cunard R, Stockand J. Thiazolidinedione-induced fluid retention is independent of collecting duct alphaENaC activity. J Am Soc Nephrol. 2009;20:721–729. doi: 10.1681/ASN.2008040415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oppermann M, Mizel D, Kim SM, Chen L, Faulhaber-Walter R, Huang Y, Li C, Deng C, Briggs J, Schnermann J, Castrop H. Renal function in mice with targeted disruption of the A isoform of the Na-K-2Cl co-transporter. J Am Soc Nephrol. 2007;18:440–448. doi: 10.1681/ASN.2006091070. [DOI] [PubMed] [Google Scholar]
- 26.Castrop H, Oppermann M, Weiss Y, Huang Y, Mizel D, Lu H, Germain S, Schweda F, Theilig F, Bachmann S, Briggs J, Kurtz A, Schnermann J. Reporter gene recombination in juxtaglomerular granular and collecting duct cells by human renin promoter-Cre recombinase transgene. Physiol Genomics. 2006;25:277–285. doi: 10.1152/physiolgenomics.00302.2005. [DOI] [PubMed] [Google Scholar]
- 27.Kon Y, Hashimoto Y, Kitagawa H, Sugimura M, Murakami K. Renin immunohistochemistry in the adrenal gland of the mouse fetus and neonate. Anat Rec. 1990;227:124–131. doi: 10.1002/ar.1092270114. [DOI] [PubMed] [Google Scholar]
- 28.Morley SD, Viard I, Chung BC, Ikeda Y, Parker KL, Mullins JJ. Variegated expression of a mouse steroid 21-hydroxylase/beta- galactosidase transgene suggests centripetal migration of adrenocortical cells. Mol Endocrinol. 1996;10:585–598. doi: 10.1210/mend.10.5.8732689. [DOI] [PubMed] [Google Scholar]
- 29.Cole JM, Khokhlova N, Sutliff RL, Adams JW, Disher KM, Zhao H, Capecchi MR, Corvol P, Bernstein KE. Mice lacking endothelial ACE: normal blood pressure with elevated angiotensin II. Hypertension. 2003;41:313–321. doi: 10.1161/01.hyp.0000050650.52007.83. [DOI] [PubMed] [Google Scholar]
- 30.Paul M, Poyan Mehr A, Kreutz R. Physiology of local renin-angiotensin systems. Physiol Rev. 2006;86:747–803. doi: 10.1152/physrev.00036.2005. [DOI] [PubMed] [Google Scholar]
- 31.Pluznick JL, Zou DJ, Zhang X, Yan Q, Rodriguez-Gil DJ, Eisner C, Wells E, Greer CA, Wang T, Firestein S, Schnermann J, Caplan MJ. Functional expression of the olfactory signaling system in the kidney. Proc Natl Acad Sci U S A. 2009;106:2059–2064. doi: 10.1073/pnas.0812859106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.