Abstract
Introduction
Increasing physical activity has been associated with reduced risk of mortality and of cardiovascular disease (CVD). The proportion of people doing no physical activity in a week varies between countries, but can reach nearly 25% in Europe and the Americas.
Methods and outcomes
We conducted a systematic review and aimed to answer the following clinical questions: Does counselling people to increase physical activity lead to increased physical activity in healthy people without existing CVD? What are the health benefits of increasing physical activity in relation to cardiovascular outcomes in healthy people without existing CVD? We searched: Medline, Embase, The Cochrane Library, and other important databases up to September 2008 (Clinical Evidence reviews are updated periodically; please check our website for the most up-to-date version of this review). We included harms alerts from relevant organisations such as the US Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA).
Results
We found 21 systematic reviews, RCTs, or observational studies that met our inclusion criteria. We performed a GRADE evaluation of the quality of evidence for interventions.
Conclusions
In this systematic review, we present information relating to the effectiveness and safety of the following interventions: counselling people to increase physical activity, and to perform higher-intensity exercise programmes.
Key Points
Increasing physical activity has been associated with reduced risk of mortality and CVD.
The proportion of people doing no physical activity in a week varies between countries, but can reach nearly 25% in Europe and the Americas.
In this review, we have looked at healthy people older than 18 years who have no evidence of existing CVD.
Counselling people to increase physical activity may increase people's activity levels over 3–12 months, particularly if accompanied by written materials and telephone follow-up.
However, the nature of the counselling interventions varied widely among RCTs, and results varied by the exact counselling intervention employed.
Counselling people to do higher-intensity exercise may increase activity levels more than counselling people to do lower-intensity exercise.
People counselled to perform a higher-intensity exercise programme were also found to adhere to it better than those given a more moderate-intensity programme.
We don't know whether counselling people to increase physical activity compared with no counselling reduces CVD, or whether counselling people to do higher-intensity exercise compared with counselling them to perform lower-intensity exercise reduces CVD, as we found insufficient evidence.
About this condition
Definition
There are no internationally agreed definitions of physical activity. It has been defined as "any bodily movement produced by contraction of skeletal muscle that substantially increases energy expenditure". Activities include formal exercise programmes as well as walking, hiking, gardening, sport, and dance. The common element is that these activities result in substantial energy expenditure, although the intensity and duration can vary considerably. Exercise is considered a subcategory of physical activity and may be defined as planned, structured, and repetitive bodily movements performed to improve or maintain one or more components of physical fitness. Level of physical activity is important in the causes of many chronic diseases. Individual change in behaviour has the potential to decrease the burden of chronic disease, particularly CVD. This review focuses on the evidence that specific interventions may lead to increases in physical activity, and that these changes may prevent CVD. The relationship between physical activity and physical fitness is complex. There is consensus that increasing levels of both activity and fitness may reduce CVD. However, it is unclear whether activity or fitness is more important for health. There are many types of physical fitness — cardiovascular fitness, muscular strength, muscular endurance, flexibility, coordination, speed, and power. The most common descriptor of physical fitness is cardiovascular fitness, which is usually determined using either prediction or direct measurement of maximum oxygen uptake. It is important to note that moderate-intensity physical activity may not necessarily lead to an increase in physical fitness (as defined by maximum oxygen uptake), but studies suggest that there will still be benefits from such activity in terms of lowering disease risk. We have therefore, in this review, assessed outcomes of both increases in intensity, frequency, and duration of physical activity, and increases in physical fitness. Primary prevention in this context is the long-term management of people at increased risk of CVD, but with no evidence of overt ischaemic CVD. We have only included studies in adults aged over 18 years who are free-living and healthy, and excluded studies if more than 10% of participants had a reported diagnosis such as obesity, diabetes, or hypertension. Prevention of cerebrovascular events is discussed in detail elsewhere in Clinical Evidence (see review on stroke prevention). In this review, we have included interventions involving counselling or advising people to increase physical activity however given (e.g., from a physician, exercise therapist, whether administered directly, by telephone, or through media [e.g., videos, television programmes]), but have excluded interventions where counselling did not form the major part of the intervention, involved intensive monitoring, or where incentives to change behaviour were a major focus of the intervention.
Incidence/ Prevalence
For general health benefits, it is recommended in government guidelines that adults achieve a minimum of 30 minutes a day of at least moderate-intensity aerobic (endurance) physical activity on 5 or more days of the week, or vigorous-intensity aerobic physical activity for a minimum of 20 minutes on 3 days each week. Combinations of moderate- and vigorous-intensity activity can be performed to meet this recommendation. The recommended levels of activity can be achieved either by doing all the daily activity in one session, or through several shorter bouts of 10 minutes or more. The activity can be lifestyle activity, or structured exercise or sport, or a combination of these. In addition, all adults are advised to perform activities that maintain or increase muscular strength and endurance for a minimum of 2 days each week. Activity levels in England are low. About 60% of men and 70% of women report less than 30 minutes of moderate-intensity physical activity a day on at least 5 days per week. Levels of physical activity in the UK fall just below the EU average. In a survey of 15 EU countries, the percentage of adults reporting no moderate physical activity (e.g., "carrying light loads, cycling at a normal pace, doubles tennis") ranged from 8% to 53%. International comparisons of physical activity/inactivity are difficult, because there are no internationally agreed definitions. Some data are available from the WHO, however, and these indicate that the prevalence of complete inactivity ("doing no or very little physical activity at work, home, for transport or in discretionary [leisure] time") is: 11% to 12% in Africa; 20% to 23% in the Americas; 18% to 19% in the Eastern Mediterranean; 17% to 24% in Europe; 15% to 17% in South East Asia; and 16% to 17% in the Western Pacific region.
Aetiology/ Risk factors
Low levels of physical activity and lack of physical fitness are strong risk factors for CHD. Both confer an increased risk similar to that associated with smoking, hypertension, and high blood cholesterol. The most frequently cited reasons for inactivity in the general population are increased urbanisation and mechanisation. Most occupations now involve little physical activity, while television viewing and computer use compete with more active pursuits in leisure time. Greater use of cars along with an increase in the use of labour-saving devices has also reduced the need for physical activity. There has been a decline in walking and cycling as modes of transport — a 2001 survey in the UK reported that the number of miles travelled by each person a year on foot and on bicycle declined by about a quarter between 1975–1976 and 1999–2001 (see figure 1 ). One proposed reason for the decline in walking is increased fears over personal safety. Barriers to physical activity include physical barriers such as an injury, emotional barriers such as embarrassment, motivational barriers such as a perceived lack of energy, time barriers, and availability barriers such as lack of facilities.
Figure 1.
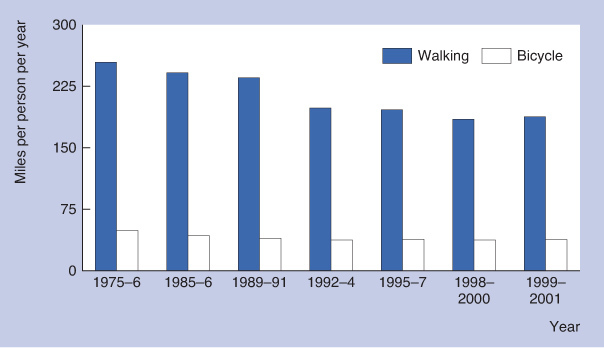
Trends in average miles travelled per person per year on foot and by bicycle, England, 1975–1976 to 1999–2001.
Prognosis
Increases in physical activity may lower the risk of CVD by exerting favourable changes on CVD risk factors (lowering blood pressure, triglyceride concentrations, and blood cholesterol concentrations, and raising high-density lipoprotein cholesterol concentrations) and by exerting direct effects on the heart (reduced heart rate, increased stroke volume) and on blood vessels (improved endothelial function, which increases the ability of blood vessels to vasodilate and enhance blood supply when necessary). In the Harvard Alumni Health study (10,269 men aged 45–84 years), men who reported changing their lifestyles after baseline to include moderately vigorous activity (4 METs or more) had a 23% lower risk of all-cause mortality at follow-up after about 20 years compared with men who continued not to engage in such activity (RR 0.77, 95% CI 0.58 to 0.96; P <0.02). The main cause of death was CVD. In the Aerobics Centre Longitudinal Study (9777 men aged 20–82 years), men classified as unfit on their first examination but fit on their second (mean of 4.9 years between examinations) had a 52% lower risk of CVD mortality during follow-up (RR 0.48, 95% CI 0.31 to 0.74) than men classified as unfit on both examinations. Fitness was assessed by a treadmill test, and the 20% of people with lowest treadmill times were classed as "unfit". The Nurses' Health Study (72,488 female nurses aged 40–65 years) assessed physical activity using a questionnaire. It found that women reporting higher levels of energy expenditure had lower rates of coronary events over 6 years. Women who walked the equivalent of 3 hours or more a week at a brisk pace (5 km an hour [3 miles an hour] or more) had significantly lower rates of coronary events compared with women who walked infrequently (RR 0.65, 95% CI 0.47 to 0.91). Similar results were found in the Women's Health Initiative prospective cohort study of 73,743 postmenopausal women.
Aims of intervention
To increase intensity, frequency, and duration of physical activity; to increase physical fitness; and to reduce the risk of CVD, with minimal adverse effects.
Outcomes
Increasing physical activity/exercise: Increase in intensity, frequency, and duration of physical activity. Can be self-reported — for example, by using self-report questionnaires such as the Behavioral Risk Factor Surveillance System (BRFSS) in the USA, and the International Physical Activity Questionnaire (IPAQ), or by recording number of steps a day using a pedometer or movement counts using an accelerometer. Rate of CVD: Incidence of fatal and non-fatal cardiovascular events. Cardiovascular risk factors: Changes in individual risk factors: weight, BMI, blood pressure, and maximum oxygen uptake.
Methods
Clinical Evidence search and appraisal September 2008. The following databases were used to identify studies for this systematic review: Medline 1966 to September 2008, Embase 1980 to September 2008, and The Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Clinical Trials 2008, Issue 3 (1966 to date of issue). An additional search was carried out of the NHS Centre for Reviews and Dissemination (CRD) — for Database of Abstracts of Reviews of Effects (DARE) and Health Technology Assessment (HTA). We also searched for retractions of studies included in the review. Abstracts of the studies retrieved from the initial search were assessed by an information specialist. Selected studies were then sent to the contributor for additional assessment, using predetermined criteria to identify relevant studies. Study design criteria for evaluation in this review were: published systematic reviews of RCTs and RCTs in any language containing more than 20 individuals, of whom more than 80% were followed up for 6 months or more. We included studies described as "open", "open label", or not blinded, as blinding was impossible. We included systematic reviews of RCTs, and RCTs where harms of an included intervention were studied, applying the same study design criteria for inclusion as we did of benefits. In addition, we use a regular surveillance protocol to capture harms alerts from organisations such as the FDA and the MHRA, which are added to the reviews as required. We excluded studies in which more than 10% of the participants had CVD at baseline. We considered ages 70 years and above as a definition for older adults. We included studies of older adults if they were not the sole focus of the study and the group was generally healthy at baseline (e.g., age range was 40–79 years). To aid readability of the numerical data in our reviews, we round many percentages to the nearest whole number. Readers should be aware of this when relating percentages to summary statistics such as relative risks (RRs) and odds ratios (ORs). We have performed a GRADE evaluation of the quality of evidence for interventions included in this review (see table). The categorisation of the quality of the evidence (high, moderate, low, or very low) reflects the quality of evidence available for our chosen outcomes in our defined populations of interest. These categorisations are not necessarily a reflection of the overall methodological quality of any individual study, because the Clinical Evidence population and outcome of choice may represent only a small subset of the total outcomes reported, and population included, in any individual trial. For further details of how we perform the GRADE evaluation and the scoring system we use, please see our website (www.clinicalevidence.com).
Table.
GRADE Evaluation of interventions for Primary prevention of CVD: physical activity.
| Important outcomes | Cardiovascular risk factors, Physical activity, Rate of cardiovascular disease | ||||||||
| Studies (Participants) | Outcome | Comparison | Type of evidence | Quality | Consistency | Directness | Effect size | GRADE | Comment |
| Does counselling people to increase physical activity lead to increased physical activity in healthy people without existing CVD? | |||||||||
| 15 (11,851) | Physical activity | Counselling people to increase physical activity versus no counselling | 4 | –2 | –1 | –2 | 0 | Very low | Quality points deducted for incomplete reporting of results and unclear description of counselling intervention. Consistency point deducted for conflicting results. Directness points deducted for diverse interventions and subjective outcome assessment |
| 2 (632) | Physical activity | Counselling people to perform higher- versus lower-intensity exercise | 4 | 0 | 0 | –2 | 0 | Low | Directness points deducted for short-term results in 1 RCT (at 6 months) and limited outcomes reported in 1 RCT (adherence to exercise) |
| What are the health benefits of increasing physical activity in relation to cardiovascular outcomes in healthy people without existing CVD? | |||||||||
| 3 (1335) | Cardiovascular risk factors | Counselling people to increase physical activity versus no advice | 4 | –1 | 0 | –1 | 0 | Low | Quality point deducted for incomplete reporting of results. Directness point deducted for no statistical comparison with no intervention group in 1 RCT |
| 1 (492) | Cardiovascular risk factors | Counselling people to perform higher- versus lower-intensity exercise programmes | 4 | –1 | 0 | –1 | 0 | Low | Quality point deducted for incomplete reporting of results. Directness point deducted for use of surrogate outcome (maximum oxygen uptake) |
We initially allocate 4 points to evidence from RCTs, and 2 points to evidence from observational studies. To attain the final GRADE score for a given comparison, points are deducted or added from this initial score based on preset criteria relating to the categories of quality, directness, consistency, and effect size. Quality: based on issues affecting methodological rigour (e.g., incomplete reporting of results, quasi-randomisation, sparse data [<200 people in the analysis]). Consistency: based on similarity of results across studies. Directness: based on generalisability of population or outcomes. Effect size: based on magnitude of effect as measured by statistics such as relative risk, odds ratio, or hazard ratio.
Glossary
- BMI
A measure of body composition defined as weight (kg) divided by the square of the height (m2).
- Low-quality evidence
Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
- MET
A multiple of the resting metabolic rate. 1 MET is the energy expenditure at rest. An exercise intensity of 3 METs indicates an energy expenditure that is three times higher than at rest. A MET may be quantified as 3.5 mL of oxygen per kilogram of body mass per minute (mL/kg/minute).
- Maximum oxygen uptake
The maximum amount of oxygen that can be consumed by the body. This is usually expressed in litres of oxygen per minute (L/minute) or in millilitres of oxygen per kilogram of body mass per minute (mL/kg/minute). Maximum oxygen uptake can be assessed by direct laboratory or field test where participants are exercised to maximum effort. It can also be predicted from submaximal tests, usually involving stepping, walking, running, or cycling below maximum effort.
- Moderate-intensity physical activity
is defined as activity that produces an increase in breathing rate; an increase in heart rate, to the level where the pulse can be felt; and a feeling of warmth, possibly accompanied by sweating on hot or humid days. This equates to an intensity of 3–6 METs. Examples include painting/decorating (3.0 METs), walking at 5 km an hour (3 miles an hour; 3.3 METs), walking at 6 km an hour (4 miles an hour; 5.0 METs), using a vacuum cleaner (3.5 METs), doubles tennis (5.0 METs), and cycling at 16–18 km an hour (10–12 miles an hour; 6.0 METs).
- Very low-quality evidence
Any estimate of effect is very uncertain.
Primary prevention of CVD: diet and weight loss
Primary prevention of CVD: treating dyslipidaemia
Primary prevention: hypertension
Diabetes: prevention of cardiovascular events
Stroke prevention
Angina (chronic stable)
Secondary prevention of ischaemic cardiac events
Disclaimer
The information contained in this publication is intended for medical professionals. Categories presented in Clinical Evidence indicate a judgement about the strength of the evidence available to our contributors prior to publication and the relevant importance of benefit and harms. We rely on our contributors to confirm the accuracy of the information presented and to adhere to describe accepted practices. Readers should be aware that professionals in the field may have different opinions. Because of this and regular advances in medical research we strongly recommend that readers' independently verify specified treatments and drugs including manufacturers' guidance. Also, the categories do not indicate whether a particular treatment is generally appropriate or whether it is suitable for a particular individual. Ultimately it is the readers' responsibility to make their own professional judgements, so to appropriately advise and treat their patients.To the fullest extent permitted by law, BMJ Publishing Group Limited and its editors are not responsible for any losses, injury or damage caused to any person or property (including under contract, by negligence, products liability or otherwise) whether they be direct or indirect, special, incidental or consequential, resulting from the application of the information in this publication.
References
- 1.Howley ET. Type of activity: resistance, aerobic and leisure versus occupational activity. Med Sci Sports Exerc 2001;33 (6 suppl):S364–S369. [DOI] [PubMed] [Google Scholar]
- 2.Blair SN, Cheng Y, Holder JS. Is physical activity or physical fitness more important in defining health benefits? Med Sci Sports Exerc 2001;33 (6 suppl):S379–S399. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. At least five a week: evidence on the impact of physical activity and its relationship to health. London, UK: Department of Health, 2004. Available at http://www.sportkeighley.com/documents/Information/five_a_week.pdf (last accessed 06 September 2010). [Google Scholar]
- 4.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1423–1434. [DOI] [PubMed] [Google Scholar]
- 5.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1435–1445. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. Health survey for England 2006: CVD and risk factors adults, obesity and risk factors children.. London, UK: The Stationery Office, 2008. Available at http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england (last accessed 06 September 2010). [Google Scholar]
- 7.European Opinion Research Group EEIG. Special Eurobarometer: physical activity. Brussels, Belgium: European Commission, 2003. Special Eurobarometer 183-6/Wave 58.2. Available at http://ec.europa.eu/public_opinion/archives/ebs/ebs_183_6_en.pdf (last accessed 06 September 2010). [Google Scholar]
- 8.The World Health Report 2002. Reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organization, 2002. Available at http://www.who.int/whr/2002/en/whr02_en.pdf (last accessed 06 September 2010). [Google Scholar]
- 9.Hardman AE, Stensel DJ. Physical activity and health: the evidence explained. 2nd ed. London, UK: Routledge Taylor and Francis Group, 2009. [Google Scholar]
- 10.Department for Transport. National travel survey; 1999–2001 update. London: Department of Transport, 2001. Available at: http://www.dft.gov.uk/pgr/statistics/datatablespublications/personal/mainresults/nts19992001 (last accessed 06 September 2010). [Google Scholar]
- 11.Buckley J, Holmes J, Mapp G. Exercise on prescription. Cardiovascular activity for health. Oxford, UK: Butterworth Heinemann, 1999. [Google Scholar]
- 12.Health Education Authority. Allied Dunbar national fitness survey. London, UK: Sports Council and Health Education Authority, 1992. [Google Scholar]
- 13.Paffenbarger RS Jr, Hyde RT, Wing AL, et al. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med 1993;328:538–545. [DOI] [PubMed] [Google Scholar]
- 14.Blair SN, Kohl HW 3rd, Barlow CE, et al. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 1995;273:1093–1098. [PubMed] [Google Scholar]
- 15.Manson JE, Hu FB, Rich-Edwards JW, et al. A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. New Engl J Med 1999;341:650–658. [DOI] [PubMed] [Google Scholar]
- 16.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. New Engl J Med 2002;347:716–725. [DOI] [PubMed] [Google Scholar]
- 17.Lawlor DA, Hanratty B. The effect of physical activity advice given in routine primary care consultations: a systematic review. J Public Health Med 2001;23:219–226. [DOI] [PubMed] [Google Scholar]
- 18.Petrella RJ, Lattanzio CN. Does counseling help patients get active? Systematic review of the literature. Can Fam Physician 2002;48:72–80. [PMC free article] [PubMed] [Google Scholar]
- 19.Eden KB, Orleans CT, Mulrow CD, et al. Does counseling by clinicians improve physical activity? A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002;137:208–215. [DOI] [PubMed] [Google Scholar]
- 20.Foster C, Hillsdon M, Thorogood M. Interventions for promoting physical activity. In: The Cochrane Library, Issue 3, 2008. Chichester, UK: John Wiley & Sons, Ltd. Search date 2004. [Google Scholar]
- 21.Norris SL, Grothaus LC, Buchner DM, et al. Effectiveness of physician-based assessment and counseling for exercise in a staff model HMO. Prev Med 2000;30:513–523. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein MG, Pinto BM, Marcus BH, et al. Physician-based physical activity counseling for middle-aged and older adults: a randomized trial. Ann Behav Med 1999;21:40–47. [DOI] [PubMed] [Google Scholar]
- 23.Burton LC, Paglia MJ, German PS, et al. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services Research Team. Prev Med 1995;24:492–497. [DOI] [PubMed] [Google Scholar]
- 24.Stevens W, Hillsdon M, Thorogood M, et al. Cost-effectiveness of a primary care based physical activity intervention in 45–74 year old men and women: a randomised controlled trial. Br J Sports Med 1998;32:236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kerse NM, Flicker L, Jolley D, et al. Improving the health behaviours of elderly people: randomised controlled trial of a general practice education programme. BMJ 1999;319:683–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steptoe A, Doherty S, Rink E, et al. Behavioural counselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease: randomised trial. BMJ 319:943–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harland J, White M, Drinkwater C, et al. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ 1999;319:828–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halbert JA, Silagy CA, Finucane PM, et al. Physical activity and cardiovascular risk factors: effect of advice from an exercise specialist in Australian general practice. Med J Aust 2000;173:84–87. [DOI] [PubMed] [Google Scholar]
- 29.Green BB, McAfee T, Hindmarsh M, et al. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med 2002;22:177–183. [DOI] [PubMed] [Google Scholar]
- 30.Hillsdon M, Thorogood M, White I, et al. Advising people to take more exercise is ineffective: a randomized controlled trial of physical activity promotion in primary care. Int J Epidemiol 2002;31:808–815. [DOI] [PubMed] [Google Scholar]
- 31.Elley CR, Kerse N, Arroll B, et al. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herrera-Sanchez B, Mansilla-Dominguez JM, Perdigon-Florencio P, et al. Effectiveness of clinical counselling after increasing physical activity. A prospective randomized study. Med Clin (Barc) 2006;126:361–363. [In Spanish] [DOI] [PubMed] [Google Scholar]
- 33.Kolt GS, Schofield GM, Kerse N, et al. Effect of telephone counseling on physical activity for low-active older people in primary care: a randomized, controlled trial. J Am Geriatr Soc 2007;55:986–992. [DOI] [PubMed] [Google Scholar]
- 34.Sevick MA, Napolitano MA, Papandonatos GD, et al. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Prev Med 2007;45:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nies MA, Partridge T. Comparison of 3 interventions to increase walking in sedentary women. Am J Health Behav 2006;30:339–352. [DOI] [PubMed] [Google Scholar]
- 36.Duncan GE, Anton SD, Sydeman SJ, et al. Prescribing exercise at varied levels of intensity and frequency: a randomized trial. Arch Intern Med 2005;165:2362–2369. [DOI] [PubMed] [Google Scholar]
- 37.Castro CM, King AC, Brassington GS. Telephone versus mail interventions for maintenance of physical activity in older adults. Health Psychol 2001;20:438–444. [PubMed] [Google Scholar]


