Abstract
Objective
To compare accuracy of blood pressure measurements using a live subject and a simulator arm, and to determine students' preferences regarding measurement.
Methods
This was a crossover study comparing blood pressure measurements from a live subject and a simulator arm. Students completed an anonymous survey instrument defining opinions on ease of measurement.
Results
Fifty-seven students completed blood pressure measurements on live subjects while 72 students completed blood pressure measurements using the simulator arm. There were no significant systematic differences between the 2 measurement techniques. Systolic blood pressure measurements from a live subject arm were less likely to be within 4 mm Hg compared with measurements of a simulator arm. Diastolic blood pressure measurements were not significantly different between the 2 techniques.
Conclusions
Accuracy of student measurement of blood pressure using a simulator arm was similar to the accuracy with a live subject. There was no difference in students' preferences regarding measurement techniques.
Keywords: blood pressure, simulator, assessment, hypertension
INTRODUCTION
Using patient simulators in medical, nursing, and pharmacy education has increased.1-4 Simulators can be used as an effective teaching strategy to facilitate learning and improve knowledge, provide controlled and safe practice opportunities, and aid in the development of strong clinical skills.2,3 Patient simulators can range from using technology and volunteers portraying patients to high-fidelity full-body human patient simulators.5
The increased use of patient simulators in pharmacy education is probably related to the greater emphasis on critical thinking and problem-solving skills.5 The Accreditation Council for Pharmacy Education (ACPE) supports the use of a variety of effective teaching strategies such as simulations and case studies (guidelines 11.2 and 25.7). In addition, ACPE recommends that schools have laboratories dedicated to professional curriculum instruction and practice simulation (guideline 27.1).6 At the time of this study, several colleges and schools of pharmacy were using patient simulators in a variety of courses to provide students with the opportunity to apply knowledge and skills learned in the classroom in a controlled practice environment.4,5,7,8
Students enrolled in a patient assessment course traditionally have been taught techniques for appropriate blood pressure measurement using a live subject, ie, fellow student. However, mastering the proper technique does not ensure accuracy of the blood pressure measurement. Because ACPE recommends the use of simulators, and several schools of pharmacy utilize mechanical patient simulators to teach physical assessment skills, we chose to introduce the use of simulator arms as a teaching strategy for blood pressure measurement. Our primary objective was to compare the accuracy in blood pressure measurements of the arm of a live subject and the Nasco Life/form Blood Pressure Simulator Arm LF01095U (NASCO, Fort Atkins, WI) within 4 mm Hg for systolic and diastolic blood pressure measurements. Our secondary objective was to determine students' preferences regarding the different methods for learning blood pressure measurement.
DESIGN
This study was designed as a prospective, cross-over study. Students in their third professional year at the University of Connecticut School of Pharmacy Introduction to Clinical Practice were invited and consented to participate in January 2009. The study was approved by the Institutional Review Board (IRB) at the University of Connecticut.
One hundred students consented to participate in the study and were divided into 2 groups (the 56 students in group 1 were those who self-enrolled in laboratory section 1, and the 44 students in group 2 were those who self-enrolled in laboratory section 2). At the beginning of the study, students in both groups were taught techniques for appropriate blood pressure measurement using the arm of a live subject, ie, fellow student, as well as blood pressure measurement using a simulator arm. During the study, students in group 1 obtained a manual blood pressure measurement on an arm of a live subject while students in group 2 obtained a manual blood pressure measurement on a simulator arm. For students in group 1, study investigators used a dual-head stethoscope to assess accuracy of student blood pressure measurement. Blood pressure measurements obtained by students were self-documented and compared with the blood pressure measurement determined by study investigators. One of 10 predetermined blood pressure settings was used to preset the simulator arm by the study investigators for each student in group 2. Blood pressure measurements obtained by students in group 2 were compared with the blood pressure setting of the simulator arm to assess accuracy. In the subsequent week, students in groups 1 and 2 were crossed over to the alternate intervention. Blood pressure measurements obtained by students with each of the described methods were deidentified with the use of a student-generated code to ensure student confidentiality and prevent bias.
At the completion of the study, students were asked to complete a 5-item anonymous survey instrument using a 5-point Likert scale on which 1 = strongly disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, and 5 = strongly agree. The survey instrument also included questions concerning students' opinions about their preferred learning method for blood pressure measurement and the method which yielded greater accuracy. The purpose of this survey was to determine ease of measurement using the 2 described methods.
Statistical analysis was conducted using StatsDirect, version 2.4.5 (StatsDirect Ltd, Cheshire, UK) and Prism 5 for Mac OS (GraphPad Software, Inc., LaJolla, CA). A p value of < 0.05 was considered significant. Bland-Altman plots were used to compare limits of agreement between the 2 described methods. Chi-square test (2X2) was used to determine if differences for systolic and diastolic readings existed between groups.
EVALUATION AND ASSESSMENT
One-hundred students enrolled in Introduction to Clinical Practice consented to participate in the study. Although all students in the class agreed to participate in the study, data from only 57 students who performed blood pressure measurements on the live subject arm and 72 students who completed blood pressure measurements on the simulator arm were included. Data was excluded if the blood pressure reading was unattainable from the live subject using the dual-head stethoscope (the student or study investigator could not hear Korotkoff sounds due to noise barriers), a temporary malfunction of the simulator arm resulted in inaccurate readings, the blood pressure reading recorded by the student was illegible, or the student was absent from the laboratory session. Excluded data were not included in the study analysis.
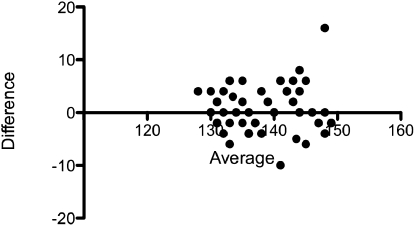
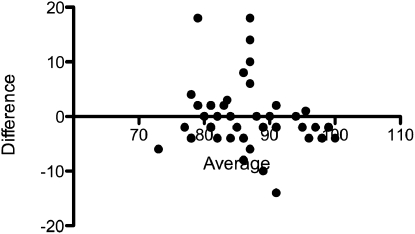
Bland-Altman plots were created to compare the 2 measurement techniques and display the individual data and the magnitude of the differences between 2 different measurements of blood pressure. The x axis represents the mean blood pressure measurements, while the y axis is the magnitude of the differences between 2 different measurements of blood pressure. Bland-Altman plots were used to compare agreement between dual-head stethoscope live subject arm blood pressure measurement, simulator arm blood pressure measurement, and blood pressure measurements determined by study investigators, which resulted in a line of agreement that is within the 95% confidence interval. The middle horizontal line indicates the mean difference. The 2 outer lines indicate the limits of agreement. Therefore, there is no significant difference between the 2 measurement techniques (Figures 1 and 2).
Figure 1.
Bland-Altman plot of simulator systolic blood pressure measurements.
Figure 2.
Bland-Altman plot of simulator diastolic blood pressure measurements.
A chi-square test was performed to examine the accuracy within 4 mm Hg for systolic and diastolic blood pressures comparing a live subject arm with a simulator arm. The relation between the systolic blood pressure variables was significant, x2 = 9.73, p = 0.0018. Systolic blood pressure measurements from a live subject arm were less likely to be within 4 mm Hg compared with systolic blood pressure measurements of a simulator arm.
A chi-square test was performed to examine the accuracy within 4 mm Hg for diastolic blood pressure measurement of a live subject arm and a simulator arm. The relationship between these variables was not significant (x2 = 0.40, p = 0.53). Diastolic blood pressure measurements from a live subject arm within 4 mm Hg were not significantly different compared with diastolic blood pressure measurements of a simulator arm.
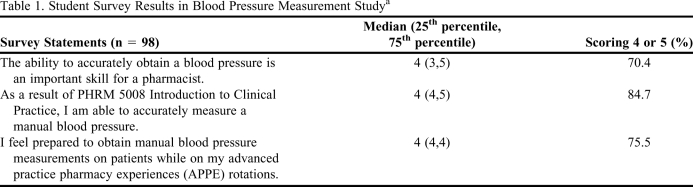
Ninety-eight students completed the anonymous survey instrument using a 5-point Likert scale. Survey results (Table 1) indicate students somewhat agreed that the ability to accurately obtain a blood pressure is an important skill for a pharmacist (median = 4). Students agreed somewhat in their ability to accurately measure a manual blood pressure (median = 4). In addition, students somewhat agreed to being prepared to obtain manual blood pressure measurements on patients while on APPEs (median = 4).
Table 1.
Student Survey Results in Blood Pressure Measurement Studya
Responses based on a Likert scale: 1 = strongly disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, 5 = strongly agree
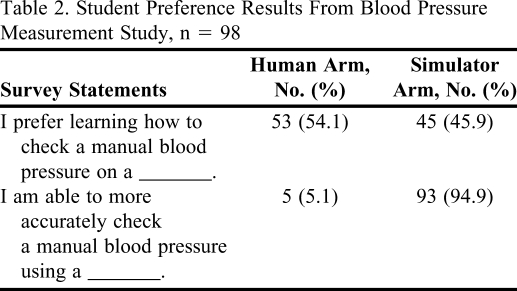
Students were surveyed to determine their preferred method to learn blood pressure measurements; 54.1% of students indicated a preference for using a live subject compared with 45.9% of students who preferred using a simulator arm for learning blood pressure measurement. At the conclusion of this study 94.9% of students surveyed indicated they thought they could measure a manual blood pressure more accurately using the simulator arm compared with a live arm (Table 2).
Table 2.
Student Preference Results From Blood Pressure Measurement Study, n = 98
SUMMARY
Using the simulator arm is an acceptable method for teaching blood pressure measurement skills to students. The simulator arm is life size and allows a student to practice the same skills and techniques in measuring a blood pressure as executed on a human subject. Systolic and diastolic number, heart rate, and volume settings are adjusted using an external control panel allowing for variability, as seen in clinical practice. The simulator arm closely resembles a human subject's arm anatomically, therefore the proper application of the blood pressure cuff and stethoscope is necessary to measure successfully the blood pressure. To determine if the simulator arms were performing properly, study investigators tested each arm before and after each class. If a simulator arm did not produce the correct blood pressure values, the settings were calibrated according to the manufacturer's recommendations to attain correct results. Simulators were determined accurate after the class session. Although the arm simulator allowed for assessment of blood pressure measurement accuracy, course instructors and students enrolled in the course indicated that it should not be the sole method by which students practice obtaining a blood pressure. Students indicated they were able to obtain a more accurate reading on the simulator, although slightly more students preferred to practice on live subjects. Some student comments suggested the volume setting for heartbeats (Korotkoff sounds) on the simulator was much louder and clearer than a human arm and therefore not realistic.
Students were more likely to obtain an accurate systolic blood pressure on the simulator arm compared with the arm of a living subject; however, their accuracy did not differ when obtaining diastolic blood pressure. Accurate operation of the simulator arm was assured by the instructors prior to the start of class with use of the manufacturer's calibration recommendations. Additionally, the manufacturer suggested 100% accuracy of the simulator arm when calibrated properly. Instructors' observations suggested that students often have difficulty releasing the air valve and maintaining a steady lowering of pressure while listening for the Korotkoff sounds. As a result, the students often missed the first Korotkoff sound. The students' perceived clarity of the simulator arm's Korotkoff sounds may have contributed to the improved systolic blood pressure accuracy on the simulator arm. In the future, course instructors will designate laboratory time to practice releasing the air valve and listening for the first Korotkoff sound.
There are several limitations to the study. The evaluation of students' accuracy in obtaining a blood pressure on an arm of a live subject relied on the assumption that the study investigator obtained a blood pressure reading that was accurate. Study investigators used a dual-head stethoscope for this evaluation which may have limited accuracy due to extraneous sounds from the multiple pieces of rubber tubing. In addition, despite calibration prior to the start of the study, temporary malfunction of the simulator arm resulted in a smaller sample size. Missing results could be attributable to a student's or study investigator's inability to record a systolic or diastolic blood pressure due to unattainable measurements. Continuing this assessment in future years should increase the sample size and power.
The overall success with the Nasco Life/form Blood Pressure Simulator Arm LF01095U has encouraged the study investigators to evaluate the potential of acquiring additional simulators such as those specific to heart and lung sound evaluation.
CONCLUSION
Accuracy of student measurement of blood pressure using the simulator arm was similar to a live arm. Whether the arm simulator can facilitate students' learning of blood pressure measurement on a live arm, or if a student's ability to measure blood pressure in the simulator is predictive of that student's ability to measure blood pressure in a live arm should be assessed in future studies.
REFERENCES
- 1.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–262. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 2.Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 3.Jarzemsky PA, McGrath J. Look before you leap: lessons learned when introducing clinical simulation. Nurse Educ. 2008;33(2):90–95. doi: 10.1097/01.NNE.0000299513.78270.99. [DOI] [PubMed] [Google Scholar]
- 4.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy degree. Chicago, Illinois 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed May 18, 2010.
- 7.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy-student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seybert AL, Kobulinski LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]