Abstract
BACKGROUND:
The true prevalence of mitral valve prolapse (MVP) in the population has been controversial.
OBJECTIVE:
To evaluate the prevalence of MVP and associated valvular abnormalities in healthy teenage students.
METHODS:
The Anthony Bates Foundation performed screening echocardiography in high schools across the United States. A total of 2072 students between 13 and 19 years of age were identified for the present study.
RESULTS:
Total prevalence of MVP was 0.7%. The prevalence of MVP was significantly higher among female teenagers (nine of 690 female teenagers [1.3%] versus five of 1382 male teenagers [0.4%], P=0.01, OR 3.6, CI 1.21 to 10.70). The prevalence of mitral regurgitation (MR) and tricuspid regurgitation (TR) was higher in teenagers with MVP. MR occurred in five of 14 teenagers (35.7%) with MVP versus 15 of 2058 controls (0.7%) (P<0.001, OR 75.6, CI 22.6 to 252.5). TR occurred in one of 14 teenagers (7.1%) with MVP versus nine of 2058 controls (0.4%) (P<0.001, OR 17.5, CI 2.0 to 148.3).
CONCLUSION:
The prevalence of MVP in this cohort of healthy teenage students was less than 1%. Furthermore, the prevalence of MVP was higher in female teenagers and was associated with a higher prevalence of MR and TR.
Keywords: Adolescence, Mitral valvar prolapse, MVP, Screening, Teenagers, Valvular disease
Mitral valve prolapse (MVP) has been described as a common disorder in the general population. The estimated prevalence of MVP in some studies is reported to be between 0.4% and 35% (1,2). There is limited literature regarding the prevalence of MVP in teenagers 13 to 19 years of age using the current standard diagnostic methods. We recently published the prevalence of MVP in young athletes undergoing screening echocardiography and found it to be less than 1% (3). A frequent diagnosis of MVP and emphasis on possible complications may have physical, mental and socioeconomic effects in this young teenage population. Using an echocardiographic database of a teenage population undergoing screening echocardiography mostly in Arizona (USA), we studied the prevalence of MVP and its associated valvular regurgitations (including trace regurgitations of mitral, tricuspid and aortic valves).
METHODS
The Anthony Bates Foundation, a nonprofit organization, is actively promoting public outreach programs through education and awareness of the need to provide heart screening events for youth. Participation in these health screenings was voluntary. History and physical questionnaires, blood pressure recordings, electrocardiograms and echocardiograms were part of the health screening. Echocardiograms were reviewed by several experienced cardiologists. A database was created from these health screenings and is frequently updated. A total of 2072 subjects between 13 and 19 years of age participated in the health screenings.
MVP was defined according to current standard guidelines as single or bileaflet prolapse at least 2 mm beyond the long-axis annular plane, with or without leaflet thickening in the long-axis parasternal view and the other views (4). SPSS 15.0 software (SPSS Inc, USA) was used for statistical analysis.
RESULTS
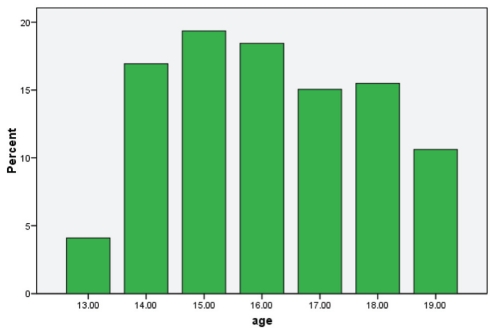
Age demographics of the screened teenagers are shown in Figure 1. The majority of the teenagers were 15 years of age. The mean (± SD) age of teenagers with MVP was 16.07±1.4 years versus 16.12±1.7 years in the control group (P=0.9). Female teenagers represented 33% of the study population (n=690).
Figure 1).
Age demographics (in years) of the screened teenagers
The prevalence of MVP in the entire study population was 0.7% (14 of 2072). The prevalence of MVP was significantly higher among the female teenagers at 1.3% (nine of 690) compared with male teenagers at 0.4% (five of 1382) (P=0.01, OR 3.6, CI 1.21 to 10.70). The prevalence of mild mitral regurgitation (MR) in subjects with MVP was 35.7% (five of 14) compared with 0.7% (15 of 2058) of controls (P<0.001, OR 75.6, CI 22.6 to 252.5). Similarly, the prevalence of tricuspid regurgitation was 7.1% (one of 14) in subjects with MVP compared with 0.4% (nine of 2058) of controls (P<0.001, OR 17.5, CI 2.0 to 148.3) (Table 1). There was no aortic regurgitation in subjects with MVP, but prevalence was 0.1% (three of 2058) in the control population.
TABLE 1.
Prevalence of mitral valve prolapse (MVP)
| Prevalence, n/n (%) | |
|---|---|
| Total prevalence of MVP | 14/2072 (0.7) |
| Female subjects with MVP | 9/690 (1.3) |
| Male subjects with MVP | 5/1382 (0.4) |
| Associated mitral regurgitation | 5/14 (35.7) |
| Associated tricuspid regurgitation | 1/14 (7.1) |
DISCUSSION
There is a limited literature that addresses the prevalence of MVP in the healthy teenage population (2,5). Studies in the 1970s and early 1980s based diagnosis on either auscultation or nonspecific echocardiography views. McLaren et al (5) studied 12,050 black children for auscultatory evidence of MVP and reported prevalences of 1.85% and 1.80% in 11- to 14-year-olds and 15- to 18-year-olds, respectively. Warth et al (2), in an echocardiography-based study of 193 children, described a prevalence of 35% in 11- to 18-year-olds. Warth et al (2) defined MVP as superior systolic motion of the mitral valve in, at minimum, a single view. This wide variation of MVP prevalence noted in the literature could be secondary to the variety of study populations, ranging from healthy volunteers to hospital-based populations, and the use of several diagnostic modalities including auscultation, phonocardiography, non-specific views of two-dimensional echocardiography and M-mode echocardiography (6,7). Levy and Savage (8), in a comprehensive review analysis of prevalence studies, noted an MVP prevalence rate of 2.5% to 5% in the general population. We recently published the results of two large databases of teenage athletes (similar to our population age) and patients who were referred for echocardiographic examination for clinical reasons. In these two independent populations, we found a prevalence of MVP of less than 1%, similar to our finding in the present study (3,9). This low prevalence in the young population was also noted by McLaren et al (5), who found an MVP prevalence of 1% in school children when multiple echocardiographic views were used to define MVP. Similarly, Freed et al (10), using the current standard definition of MVP in a large community-based sample of adults between 26 and 84 years of age, concluded that the prevalence of MVP and its complications was lower than previously expected. Earlier studies suggested that the prevalence of MVP increases throughout childhood and peaks in the early 20s (11,12). The noted prevalence in our study may increase over the next few years as the subjects advance to adulthood. However, our recent findings, using a large echocardiographic database that included adults, showed a low prevalence of MVP in the general population (9). Our study showed that female participants had a statistically significant higher prevalence of MVP compared with male participants. Several studies have demonstrated similar results (8,12). A more recent community-based study by Freed et al (10) noted no significant sex differences in the prevalence of MVP. The mean age of their study population was 54.7±10 years. As mentioned earlier, the prevalence of MVP usually peaks in early adulthood and then tends to decline in females (11,12). This probably explains the lack of significant differences, although they found numerical differences in prevalence, with more female subjects having MVP than the male subjects.
In our study, association of MR with MVP was significantly higher in subjects with MVP than in subjects without MVP. Most of the MR noted was of trace severity. Our findings are in concordance with previous studies demonstrating a similar association between MVP and MR (10,13,14). Also noted in our study, tricuspid regurgitation was significantly associated with MVP compared with teenagers without MVP. We did not find increased prevalence of aortic regurgitation in teenagers with MVP.
LIMITATIONS
Our study is a retrospective review of a database. The echocardiography technique and interpretation depended on the individual cardiologist. Hemodynamic effects of the valvular abnormalities on the study population were unavailable and could not be accommodated in our study. We had no physical examination data available, limiting our findings to echocardiographic documentation of MVP. We could not perform inter-reader agreement tests because the diagnosis of MVP was performed on site by a cardiologist during screening.
REFERENCES
- 1.Rizzon P, Biasco G, Brindicci G, Mauro F. Familial syndrome of midsystolic click and late systolic murmur. Br Heart J. 1973;35:245–59. doi: 10.1136/hrt.35.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warth DC, King ME, Cohen JM, Tesoriero VL, Marcus E, Weyman AE. Prevalence of mitral valve prolapse in normal children. J Am Coll Cardiol. 1985;5:1173–7. doi: 10.1016/s0735-1097(85)80021-8. [DOI] [PubMed] [Google Scholar]
- 3.Hepner AD, Morrell H, Greaves S, Greaves J, Movahed MR. Prevalence of mitral valvar prolapse in young athletes. Cardiol Young. 2008;18:402–4. doi: 10.1017/S104795110800245X. [DOI] [PubMed] [Google Scholar]
- 4.ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease) J Am Coll Cardiol. 1998;32:1486–588. doi: 10.1016/s0735-1097(98)00454-9. [DOI] [PubMed] [Google Scholar]
- 5.McLaren MJ, Hawkins DM, Lachman AS, Lakier JB, Pocock WA, Barlow JB. Non-ejection systolic clicks and mitral systolic murmurs in black schoolchildren of Soweto, Johannesburg. Br Heart J. 1976;38:718–24. doi: 10.1136/hrt.38.7.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markiewicz W, London E, Popp RL. Effect of transducer placement on echocardiographic mitral valve motion. Am Heart J. 1978;96:555–6. doi: 10.1016/0002-8703(78)90172-2. [DOI] [PubMed] [Google Scholar]
- 7.Markiewicz W, Peled B, Hammerman H, Greif Z, Hir J, Riss E. Contribuiton of M-mode echocardiography to cardiac diagnosis. An assessment in 1,000 successive patients. Am J Med. 1978;65:803–7. doi: 10.1016/0002-9343(78)90799-4. [DOI] [PubMed] [Google Scholar]
- 8.Levy D, Savage D. Prevalence and clinical features of mitral valve prolapse. Am Heart J. 1987;113:1281–90. doi: 10.1016/0002-8703(87)90956-2. [DOI] [PubMed] [Google Scholar]
- 9.Hepner AD, Ahmadi-Kashani M, Movahed MR. The prevalence of mitral valve prolapse in patients undergoing echocardiography for clinical reason. Int J Cardiol. 2007;123:55–7. doi: 10.1016/j.ijcard.2006.11.130. [DOI] [PubMed] [Google Scholar]
- 10.Freed LA, Levy D, Levine RA, et al. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med. 1999;341:1–7. doi: 10.1056/NEJM199907013410101. [DOI] [PubMed] [Google Scholar]
- 11.Hickey AJ, Wilcken DE. Age and the clinical profile of idiopathic mitral valve prolapse. Br Heart J. 1986;55:582–6. doi: 10.1136/hrt.55.6.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Savage DD, Devereux RB, Garrison RJ, et al. Mitral valve prolapse in the general population. 2. Clinical features: The Framingham Study. Am Heart J. 1983;106:577–81. doi: 10.1016/0002-8703(83)90705-6. [DOI] [PubMed] [Google Scholar]
- 13.Olson LJ, Subramanian R, Ackermann DM, Orszulak TA, Edwards WD. Surgical pathology of the mitral valve: A study of 712 cases spanning 21 years. Mayo Clin Proc. 1987;62:22–34. doi: 10.1016/s0025-6196(12)61522-5. [DOI] [PubMed] [Google Scholar]
- 14.Zuppiroli A, Rinaldi M, Kramer-Fox R, Favilli S, Roman MJ, Devereux RB. Natural history of mitral valve prolapse. Am J Cardiol. 1995;75:1028–32. doi: 10.1016/s0002-9149(99)80718-8. [DOI] [PubMed] [Google Scholar]