Abstract
Background. The feasibility, cost-effectiveness and best means to implement population screening for type 2 diabetes remain to be established.
Objective. To learn from the experiences of practice staff undertaking a diabetes screening programme in order to inform future screening initiatives.
Methods. Qualitative analysis of interviews with staff in six general practices in the ‘ADDITION-Cambridge’ trial; three randomly allocated to intensively manage screen-detected patients and three providing usual care. We conducted semi-structured interviews with seven nurses, four doctors, three health care assistants and four managers. Four researchers analysed the transcripts practice by practice, preparing vignettes and comparing interpretations. Participants commented on a summary report.
Results. Each practice team implemented the screening and intervention programme differently, depending on numbers at risk and decisions about staff contributions. Several emphasized the importance of administrative support. As they screened, they extended the reach of the programme, testing patients outside the target group if requested, checking other risk factors, providing health information and following up people with impaired glucose tolerance. Staff felt that patients accepted the screening and subsequent management as any other clinical activity.
Conclusions. Although those developing screening programmes attempt to standardize them, primary care teams need to adapt the work to fit local circumstances. Staff need a sense of ownership, training, well-designed information technology systems and protected time. Furthermore, screening is more than measurement; at the individual level, it is a complete health care interaction, requiring individual explanations, advice on health-related behaviour and appropriate follow-up. The UK ‘NHS Health Checks’ programme should embrace these findings.
Keywords: Attitude of health personnel, delivery of health care, implementation, mass screening, primary health care, (MeSH terms): type 2 diabetes mellitus
Introduction
Type 2 diabetes is a progressive condition and although initially it may cause few symptoms, its complications impose a substantial medical and financial burden.1 Retinopathy can be present at diagnosis, suggesting an onset some years before clinical recognition.2 This has prompted calls for screening and earlier intervention. The ADDITION-Cambridge trial was established to assess key uncertainties in relation to cost-effectiveness by screening people aged 40–69 years deemed to be at risk of undiagnosed type 2 diabetes and by comparing the impact of intensive treatment with usual care among the screen-detected patients.3,4
In ADDITION-Cambridge people at high risk were identified using routine data and invited to attend for a finger prick blood test. An alternative strategy would be to test patients when they consult for other problems,5 an approach supported by some screening studies that identified few new cases, because most of those at risk had already been tested in routine care.6,7 Disadvantages of relying on opportunistic testing are that some people attend their GP infrequently and abnormal results are not always followed up appropriately.8 This may be partly because some professionals and patients are unsure how seriously to take type 2 diabetes.9 Also, some initiatives to promote opportunistic testing have been implemented in an ad hoc way. While enthusiasts report that it is usually possible to detect diabetes before symptoms develop,10 a national pilot programme that did not tightly specify the target group or mechanism for screening identified few new cases.11
Although some GPs are uncertain how to manage impaired glucose regulation (IGR),12 economic modelling suggests that screening may be more cost-effective if people with IGR can be identified and offered lifestyle advice than if programmes focus solely on diagnosing diabetes.13 This and the potential to identify other modifiable risk factors have prompted the UK Department of Health to introduce a national programme of ‘NHS Health Checks’, including random glucose tests for those at risk.14 The impact assessment for the programme suggests that screening those aged 40–74 years every 5 years would cost £4506 million, giving a net benefit of £55 304 million over 20 years, and a cost per quality adjusted life year of £3505.15 Although general practice teams would provide medical management for conditions diagnosed, the proposals envisage that pharmacists and others might also undertake screening.
When developing public health initiatives, it is important to learn from similar programmes because understanding their implementation can provide lessons about possible improvements.16 This paper reports the experiences of the GPs, nurses and other practice staff in the ADDITION-Cambridge trial and considers the implications for screening and early intervention.
Methods
For this process evaluation, we adopted a qualitative approach in order to understand what screening involved from the perspectives of practice staff undertaking the work.
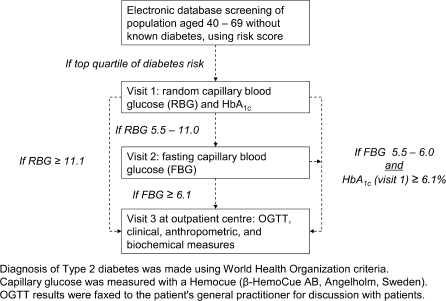
In the ADDITION-Cambridge trial, 49 practices screened for type 2 diabetes and 5 others were randomized to serve as no-screening controls. Screening practices were randomly allocated to offer either routine care or intensive multifactorial treatment to those diagnosed.3 The stepwise screening procedure is shown in Figure 1. People whose records suggested that they were in the top quartile of risk of diabetes when assessed using a validated risk score17 were invited by letter to a screening clinic. Random capillary blood glucose (RBG) was measured and a laboratory sample sent for glycated haemoglobin (HbA1c). If RBG was >5.5 mmol/l, arrangements were made for a fasting blood glucose (FBG) test at the practice; if RBG was >11.0 mmol/l, an oral glucose tolerance test (OGTT) was arranged at a referral centre.18 Relevant practice staff received training, a study manual and bespoke software to identify patients and support the screening. Practices randomized to offer intensive treatment received an academic detailing session with a local diabetologist and GP opinion leader to describe the treatment algorithms and targets and present the evidence underpinning intensive treatment, followed by interactive feedback sessions at 6 and 14 months. In these practices, patients with screen-detected diabetes received theory-based educational materials.
FIGURE 1.
The ADDITION-Cambridge trial screening programme
Sampling
Practices undertook screening between 2002 and 2006, but we selected practices that had screened during the latter 2 years to avoid problems with recall. We purposively sampled three routine care and three intensive treatment practices and practices with high and low yields of screen-detected patients. In order to compare the perspectives of staff with different roles, we sought to interview doctors, practice nurses, health care assistants (HCAs) and managers who had been involved in the work. We asked the manager at each practice to suggest potential interviewees. Individual staff was free to make their own decision on participation and assured about confidentiality.
Data collection
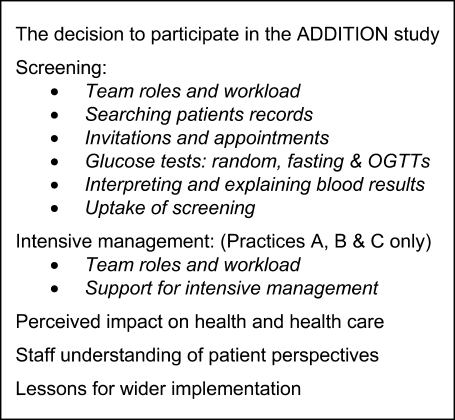
The interview schedule explored the participant's experiences of screening and if relevant intensive management as part of the ADDITION study (Fig. 2). After piloting this in a separate practice, SM, an academic GP registrar, visited each practice to conduct the individual semi-structured interviews. Seven practice nurses, four doctors, three HCAs and four managers took part. Eight worked in practices allocated to provide routine care and 10 in the intensive treatment practices. Interviews (mean duration 47; range 26–72 min) were audio recorded and transcribed verbatim. JG and SM listened to and discussed the audio recordings during the interview phase.
FIGURE 2.
Interview schedule
Analysis
The analysis was informed by grounded theory.19 We used NVivo8 (QSR International) for coding and retrieval. Four researchers (JG, JPG, KW and SC) read all the transcripts and met regularly to prepare summaries for each practice. In order to improve the validity of the findings, we adopted a process of triangulation, comparing the accounts given by participants working in different disciplines and practices. As we systematically compared our interpretations as researchers, a number of themes emerged. These were not predetermined, but we reassessed ideas that arose from consideration of the earlier interviews during later discussions. We invited participants to comment on the draft findings.
Results
Practice size varied widely, from two to nine partners, serving between 2751 and 12 631 patients. The population age distribution and numbers at risk also varied (Table 1). Across the six practices, 82 (3.2%) of those attending for random glucose tests were eventually found to have diabetes and 58 (2.2%) impaired glucose regulation (IGR)—either impaired fasting glycaemia (IFG) or impaired glucose tolerance (IFT).
TABLE 1.
Screening activity in the six practices
| Intensive treatment |
Routine care |
|||||||||||
| A |
B |
C |
D |
E |
F |
|||||||
| No of GPsa | 2 WTE | 4.2 WTE | 9 WTE | 2 WTE | 3.2 WTE | 6.2 WTE | ||||||
| List size | 3613 | 6640 | 12 631 | 2751 | 5562 | 10 620 | ||||||
| Aged 40–69 years | 1170 | 2611 | 5216 | 1163 | 2312 | 1586 | ||||||
| Positive risk scoreb | 330 | 28.2% | 627 | 24% | 1372 | 26.3% | 325 | 27.9% | 590 | 25.5% | 291 | 18.3% |
| People screened | ||||||||||||
| Random glucosec | 252 | 76.4% | 436 | 69.5% | 1039 | 75.7% | 216 | 66.5% | 456 | 77.3% | 181 | 62.2% |
| Fasting glucose | 110 | 117 | 435 | 54 | 211 | 53 | ||||||
| Cases detected | ||||||||||||
| Diabetes | 10 | 15 | 26 | 7 | 16 | 8 | ||||||
| IFG or IGT | 7 | 6 | 22 | 8 | 13 | 2 | ||||||
| Screening rate | ||||||||||||
| Time spent screening (months) | 9 | 19 | 14 | 11 | 8 | 16 | ||||||
| People screened per month (average) | 28 | 23 | 72 | 20 | 60 | 11 | ||||||
| Practice setting | Large village: small team. Felt they had good communication. Collective decision to take part. | Country town: decision to take part led by staff involved in diabetes care, reflecting the way the team devolved work. | Rural: active in research. Saw taking part as a way to standardize diabetes care. | Rural: their approach was based on their view of themselves as a small organization. | Rural: medium-sized, self-sufficient practice in reasonably affluent area. | City: based at two sites. Few elderly patients at high risk of diabetes. | ||||||
| Implementation | Took a systematic approach based on the study protocol and shared out tasks flexibly. The HCA had an administrative role, arranging screening clinics for the nurse. | Nurses and HCA arranged clinics as well as screening in ordinary surgeries. In retrospect, they would have liked more administrative support. (Screening was delayed by staff sickness.) | Administrative staff made appointments and assisted the nurses and HCAs in recording data. They had large numbers to screen and despite being well organized found it hard to manage the workload. | Needed help with computer searches but felt that taking part improved their records and systems. They discussed lifestyle with many study patients, including those whose tests did not detect diabetes. | Staff devised plan to implement the work. The nurse and reception manager saw patients together and focussed tightly on the study tasks. One nurse screened and the other followed up people newly diagnosed. | One nurse led the study. When screening she covered a range of topics including diet, exercise, blood pressure and cholesterol tests. She saw this as a means to take a proactive, patient-centred approach. | ||||||
WTE, whole time equivalent.
The risk score was calculated to select people in the top 25% of the age group by risk of diabetes. The percentage shown is of all those aged 40–69 years.
Percentage shown is of those with positive risk score.
Implementation in different settings
Each practice team adopted a rather different approach towards implementation. In the two smaller practices (A and D), staff shared out tasks flexibly, with each team member covering several tasks. They described a sense of identity as a small organization.
I think it was just generally decided between us. We're very small anyway. There's only eight of us. Can we handle the admin? And then we decided to go ahead. Manager (Practice D)
In contrast, the larger practices (C and F) took a more structured approach. Individual staff had particular tasks and roles overlapped less. Sometimes nurses and administrative staff worked side by side to see patients and record data. Both small and large practices saw benefits from their respective size.
Usually, the practice manager or administrator undertook the search of the practice electronic records to identify those at risk. After initial training, some found the search queries easy to use, but others needed ongoing assistance. Several regarded the software provided to generate invitation and reminder letters as vital for the programme's success.
Most arranged clinics in the afternoon but if patients requested appointments in normal surgery because of work commitments, they normally arranged this. If OGTTs were needed, these were done at an outpatient centre. Sending specific appointments seemed to work well.
A lot of them thought it was handy having the appointments sent to them. Because I think if they'd have just got a letter they wouldn't have made the appointment. So they said it was a lot easier to have an appointment. HCA (B)
Several nurses and HCAs commented that the programme involved significantly more work than they had expected and there was a need for administrative support.
I found that I was using lunch hours to do this admin work. And that's part of the reason why we got behind I think. Because there wasn't time to do the initial mail merging and organise the clinics on a regular basis. So it was a little bit ad-hoc and we should have been more organised about it. Nurse (B)
In contrast, Practice E, who did make provision for administrative support, completed their screening quickest. One of the nurses described how they ‘developed a system and whizzed through the patients quite nicely’ Nurse 1 (E).
Several nurses commented that diabetes was ‘their’ territory, a view endorsed by the GPs, who did little of the actual screening. One referring to the practice nurse said ‘You know she is diabetes for us in this practice’ (Dr C). Taking part enabled HCAs to develop their role and gave one reception manager direct patient contact that she enjoyed (Practice E). Although the burden of ongoing screening was considerable, interviewees described a sense of responsibility to see it through.
However, not all those interviewed had a grasp of the screening programme as a whole, particularly if the nurses undertaking screening were not involved in the ongoing management of those diagnosed (Practices A and E). One who joined the practice after the study began was unsure how newly diagnosed patients were informed of the diagnosis.
Sometimes you'd say to the patient you know you've been diagnosed with type 2 and they'd go: ‘Have I?’ … . It would have been nice perhaps to have known in more detail what they'd been told … . Well to be fair I wasn't ever involved in the entirety of how it was working … . So in all fairness I was never part of any initial sit down ‘this is how it's going to work’ meeting. Nurse 2 (E)
Extending the scope of the programme
Although the criteria for screening were tightly specified within the ADDITION Study protocol, several responders described ways that they had extended the scope of the programme. Some had screened spouses or others outside the target group or tested for conditions such as hypertension or raised blood lipids.
We were picking up the blood pressures so that made a difference as well. But I mean that wasn't anything to do with the study. We just we grabbed the opportunity while we had the chance. HCA (C)
One nurse gave health promotion advice when telling people their blood results, even if the result was negative.
I'd emphasise to them very strongly that diabetes is not about sugar. You know it's about their circulation and it's about the link with their blood pressure and their cholesterol and so it's all about having a healthy diet—more oily fish, less salt, less cheese. ‘And we'll be checking you again in a year’. And you know perhaps a bit of weight loss and so you're working with them … . It's ongoing prevention really. Nurse (F)
There were also differences in how practices responded if patients did not attend. Some flagged the notes of non-attenders so they could be screened when they next attended. Staff in Practice B telephoned them and offered to rebook the appointment.
We tried really hard. Because if they DNA'd the first time we were going to send them another appointment. And then we actually phoned them as well. So I think you can only do so much. You can't badger people. If they want to have it done they'll come. HCA (B)
Although these adaptations might be seen as treating screening as any other clinical activity that needs to be tailored to the individual's needs, it was interesting that some resisted pressure to extend the work. Practice E arranged brief appointments which they limited to tests in the protocol.
I mean obviously everyone tries to get a little bit more information or whatever from you at the start. You know asking to be checked for this or that. We had to be pretty strong to say it's all we are going to do today. Nurse 1 (E)
The ways that practice teams adapted the programme provide insight into their understanding of screening and how it fitted within routine clinical care. Whereas some appeared primarily focussed on the needs of the individual patient, others thought more in terms of the needs of the population to be screened. However, these local adaptations did not affect who was sampled for the study, the tests done or how the diagnosis was made.
Perceived impact
Although some staff retained an open mind, waiting for the results to find out whether screening was worth the effort, most believed it was worthwhile, particularly if they had a family member with diabetes. They referred to particular patients whose health had improved after being diagnosed by screening; this motivated them to continue their efforts. Several described benefits for their practice from participating. These included updated records, improvements to their procedures for diagnosing diabetes and greater awareness of the condition which they tested for more often. Most established new systems to follow up people with IFG or IGT, although they were not always sure of the benefit.
We obviously found more pre-diabetes which we wouldn't have picked up earlier … . They would come in to see me in the diabetic clinic at least once a year. Just to give advice. We'd send them to see the dietician and give them as much information as we could. Obviously quite a few of the pre-diabetes that came through from the Addition have already tipped over into diabetes. Even with the education. I mean they were usually obese anyway. And you weren't gonna do an awful lot for them. Nurse (C)
Staff in the three intensive management practices particularly valued the meetings with the research team to review individual patients.
I learnt quite a lot about diabetes. We went through patient by patient so we as a group could decide what they needed. If it was a question of increasing hypoglycaemic treatment or if it was a question of starting a statin or working on their weight or their smoking or whatever it happened to be. GP (A)
So it was highlighting that we weren't doing as well as we thought. Well everyone thinks that they're doing better than they really are doing. GP (C)
When asked about the impact of the study, staff in the routine care practices responded in terms of benefits from screening, but said their management of diabetes had not changed. In contrast, several staff in intensive management practices referred to aiming for tighter control of risk factors, which then became the norm for other patients in the practice.
Relationships with patients
Patients’ experiences of screening within the ADDITION study have been reported separately.20 Most of those invited for screening did attend, but staff in the city practice, which had the lowest attendance, encountered more scepticism about the value of screening than those in the rural practices who said that patients generally followed their advice (Table 1). One doctor reported that men working away from home were less likely to attend.
The people that you really want to get your hands on and I have quite a few of them here. The ones that are businessmen that are abroad and they are classic of the diabetics that never attend. I know exactly who they are and we never see them and they're the people that we couldn't get in. Dr (B)
The pre-existing relationship with patients influenced the programme in various ways. The staff respondents felt that it improved attendance, medication adherence and patients’ response to lifestyle advice. It offered the opportunity to discuss screening in future consultations if people did not attend. But the strength of these relationships varied—comparing the language used in different accounts, it appeared that some interviewees were closer to the patients than others.
Staff in the intensive management practices were asked how patients reacted to the approach, particularly if this meant that they were prescribed medication at an earlier stage than they might have been. While the doctors believed the patients were unaware that they were being treated differently, some nurses said they did explain the more intensive approach. Although most patients appeared to accept their treatment as for any other problem, some resisted medication when they did not feel ill.
Well that was a problem with a few people who don't like tablets anyway … . I think the frequent nurse follow-up to persuade them was useful. I think most patients didn't have a problem. But some did because they didn't feel unwell. GP (A)
It is noteworthy that the language the interviewees used was the language of the staff room, rather than the careful words employed in research literature. They referred to ‘hounding DNAers’ (patients who did not attend); one doctor laughed at the idea that patients might have a choice about having intensive treatment and a nurse referred to the consent form as ‘the instruction sheet’. Taken together, these apparent indiscretions illustrate how the ADDITION screening and treatment programme was seen as part of everyday health care, rather than something specific to a research study.
Twelve of the 18 staff commented on the draft report, with each practice represented. All agreed that it was valid and several were interested to compare their experiences with the accounts from other practices.
Discussion
Summary of main findings
This study illustrates how screening for diabetes can be implemented in routine general practice. While the workload can be estimated from demography, each of the practice teams implemented the programme in their own way, but all required protected time. They adapted the work according to the size of the practice, the numbers to be screened, the way that they made decisions in the team and their particular interests. Although some limited their role to the protocol tasks, most extended this, giving explanations and advice, following up people with IGR and screening family members if requested. This flexibility enabled staff to identify with and make sense of the intervention, but in turn may have modified its impact.
At the individual level, screening was seen as a complete health care transaction, rather than just measurement. The process of identifying people as being at risk of diabetes invites the questions ‘Why me?’ and ‘What can I do about it?’ It inevitably includes elements of health promotion and support for behaviour change. As when considering weight, blood pressure, cholesterol and behaviours such as physical activity, the aim is to reduce risk, rather than just to detect abnormal cases.
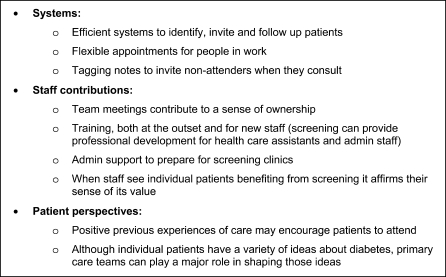
At the population level, screening requires systems to identify, invite and test those at risk, with follow-up to give people their results. Factors that appeared to facilitate this are summarized in Figure 3.
FIGURE 3.
Factors that facilitate screening
Strengths and limitations of the study
This study compared the experiences of staff from different disciplines in different practices. Each understood their particular part of the screening programme, enabling us to construct a coherent picture of implementation in each practice. We learnt about screening in the world of everyday practice that may be useful to others implementing similar programmes.
Practical constraints limited the number and location of practices that could be included. None were in deprived urban areas or had significant minority ethnic communities. However, the central finding, that initiatives are adapted during implementation in different contexts, seems even more relevant for these areas. Since practice team members were interviewed after they had finished screening, some had difficulty recalling specific details. Furthermore, because analysis was not done concurrently with the interviews, there was little scope to test emerging concepts in later interviews. Instead, these were tested by comparison within the interviews and by seeking participants’ comments on the draft report.
Comparison with existing literature
GPs and practice nurses who have not undertaken diabetes screening have been found to draw on their perceptions of patient preferences and a range of experiential knowledge, rather than formal evidence of effectiveness in assessing its worth.21 Our findings suggest that when asked to undertake such a programme, these ‘common sense’ perspectives also shape their approach to implementation.
It may be necessary to adapt standardized programmes as they are delivered, but this raises questions about how much freedom local services should have in doing so. Comparison with other initiatives may help here. In a less tightly specified UK pilot programme, only 1.4% of those tested were found to have diabetes. Some practices screened outside the target group and around a third of people found to have abnormal results were not followed up.11
In contrast, the ADDITION-Cambridge protocol and information systems provided a framework to offer participants the core screening intervention, but as we found, this was implemented in different ways in the different practices. Hawe et al.22 argue that this context level adaptation is necessary if complex interventions are to be effective; they see the key aim of a trial to standardize the function and process of the intervention, not every aspect of its delivery.
Implications for future research and clinical practice
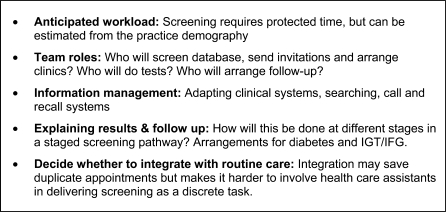
In some respects, the ADDITION screening programme resembled the arrangements planned for NHS Health Checks. People aged 40–74 years will be invited for checks, including weight, blood pressure, smoking and cholesterol measurement.23 Those selected by a filter incorporating blood pressure and body mass index with thresholds adjusted for ethnicity will be offered diabetes screening. This will involve either arranging an FBG test or testing HbA1c at the time if returning for a fasting test is inconvenient, followed up by an OGTT if indicated, a simpler but probably less sensitive procedure than that followed in ADDITION-Cambridge. In implementing the national programme, practices may find it helpful to consider the issues that our work has identified as important (Fig. 4).
FIGURE 4.
Issues to address in implementing diabetes screening
Our findings suggest that the workload will vary between practices and may be considerable. Some primary care trusts are commissioning pharmacists and alternative providers to undertake the initial screening, which may share the burden but could fragment care and duplicate tests already done in general practice.14 Whether or not they undertake the initial checks, practices will still need systems to assess those identified as having diabetes, hypertension, kidney disease or raised blood lipids. It will therefore be important that the new programme is evaluated as a coherent whole to ensure that it merits the resources invested.
Screening consultations are not simply a means to conduct tests. Instead, like all conversations in the consulting room, they offer an extraordinary opportunity to engage with people and promote health. The challenge in implementing screening programmes is to achieve this in as efficient a way as possible.
Declaration
Funding: National Institute for Health Research Programme Grant for Applied Research (RP-PG-0606-1259). The ADDITION-Cambridge trial has been funded by the Wellcome Trust, the Medical Research Council and NHS R&D Support Funding.
Ethical approval: Cambridgeshire 4 Research Ethics Committee (Ref: 02/5/54).
Conflict of interest: none.
Acknowledgments
We thank the practice staff who agreed to be interviewed. Rabia Hassam contributed to the analysis and David Simmons and Erica Borgstrom provided helpful comments on the draft manuscript.
References
- 1.Alberti KGMM. The costs of non-insulin-dependent diabetes mellitus. Diabet Med. 1997;14:7–9. doi: 10.1002/(SICI)1096-9136(199701)14:1<7::AID-DIA321>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 2.Rajala U, Laakso M, Qiao Q, Keinanen-Kiukaanniemi S. Prevalence of retinopathy in people with diabetes, impaired glucose tolerance, and normal glucose tolerance. Diabetes Care. 1998;21:1664–9. doi: 10.2337/diacare.21.10.1664. [DOI] [PubMed] [Google Scholar]
- 3.Echouffo-Tcheugui JB, Simmons RK, Williams KM, et al. The ADDITION-Cambridge trial protocol—a cluster-randomised controlled trial of screening for type 2 diabetes and intensive treatment for screen-detected patients. BMC Public Health. 2009;9:136. doi: 10.1186/1471-2458-9-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lauritzen T, Griffin S, Borch-Johnsen K, et al. The ADDITION study: proposed trial of the cost-effectiveness of an intensive multifactorial intervention on morbidity and mortality among people with Type 2 diabetes detected by screening. Int J Obes Relat Metab Disord. 2000;24(suppl 3):S6–1. doi: 10.1038/sj.ijo.0801420. [DOI] [PubMed] [Google Scholar]
- 5.Greaves CJ, Stead JW, Hattersley AT, et al. A simple pragmatic system for detecting new cases of type 2 diabetes and impaired fasting glycaemia in primary care. Fam Pract. 2004;21:57–62. doi: 10.1093/fampra/cmh113. [DOI] [PubMed] [Google Scholar]
- 6.Cogneau J, Balkau B, Weill A, Liard F, Simon D. Assessment of diabetes screening by general practitioners in France: the EPIDIA Study. Diabet Med. 2006;23:803–7. doi: 10.1111/j.1464-5491.2006.01877.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janssen PGH, Gorter KJ, Stolk RP, Rutten GEHM. Low yield of population-based screening for Type 2 diabetes in the Netherlands: the ADDITION Netherlands study. Fam Pract. 2007;24:555–61. doi: 10.1093/fampra/cmm052. [DOI] [PubMed] [Google Scholar]
- 8.Ealovega MW, Tabaei BP, Brandle M, Burke R, Herman WH. Opportunistic screening for diabetes in routine clinical practice. Diabetes Care. 2004;27:9–12. doi: 10.2337/diacare.27.1.9. [DOI] [PubMed] [Google Scholar]
- 9.Saint Lamont S, Whitford D, Crosland A. ‘Slightly more serious than a cold’: do patients, nurses and GPs take type 2 diabetes seriously? Prim Health Care Res Dev. 2002;3:75–84. [Google Scholar]
- 10.Evans P, Langley P, Gray DP. Diagnosing Type 2 diabetes before patients complain of diabetic symptoms—clinical opportunistic screening in a single general practice. Fam Pract. 2008;25:376–81. doi: 10.1093/fampra/cmn052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyder E, Wild S, Fischbacher C, Carlisle J, Peters J. Evaluating the impact of a national pilot screening programme for type 2 diabetes in deprived areas of England. Fam Pract. 2008;25:370–5. doi: 10.1093/fampra/cmn054. [DOI] [PubMed] [Google Scholar]
- 12.Wylie G, Hungin AP, Neely J. Impaired glucose tolerance: qualitative and quantitative study of general practitioners' knowledge and perceptions. BMJ. 2002;324:1190. doi: 10.1136/bmj.324.7347.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gillies CL, Lambert PC, Abrams KR, et al. Different strategies for screening and prevention of type 2 diabetes in adults: cost effectiveness analysis. BMJ. 2008;336:1180–5. doi: 10.1136/bmj.39545.585289.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kmietowicz Z. Five yearly checks for over 40s will save 650 lives a year, says government. BMJ. 2009;338:b1334. [Google Scholar]
- 15.Department of Health. Putting Prevention First; Vascular Checks: Risk Assessment and Management. Impact Assessment. London: Department of Health; 2008. pp. 1–67. [Google Scholar]
- 16.Oakley A, Strange V, Bonell C, Allen E, Stephenson J. Health services research—process evaluation in randomised controlled trials of complex interventions. BMJ. 2006;332:413–6. doi: 10.1136/bmj.332.7538.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffin SJ, Little PS, Hales CN, Kinmonth AL, Wareham NJ. Diabetes risk score: towards earlier detection of type 2 diabetes in general practice. Diabetes Metab Res Rev. 2000;16:164–71. doi: 10.1002/1520-7560(200005/06)16:3<164::aid-dmrr103>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 18.WHO Department of Noncommunicable Disease Surveillance. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. WHO/NCD/NCS/99.2. Geneva: WHO; 1999. [Google Scholar]
- 19.Glaser BG, Strauss AL. The Discovery of Grounded Theory. Chicago, IL: Aldine; 1967. [Google Scholar]
- 20.Eborall H, Davies R, Kinmonth AL, Griffin S, Lawton J. Patients' experiences of screening for type 2 diabetes: prospective qualitative study embedded in the ADDITION (Cambridge) randomised controlled trial. BMJ. 2007;335:490. doi: 10.1136/bmj.39308.392176.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whitford DL, Lamont SS, Crosland A. Screening for Type 2 diabetes: is it worthwhile? Views of general practitioners and practice nurses. Diabet Med. 2003;20:155–8. doi: 10.1046/j.1464-5491.2003.00892.x. [DOI] [PubMed] [Google Scholar]
- 22.Hawe P, Shiell A, Riley T. Complex interventions: how “out of control” can a randomised controlled trial be? BMJ. 2004;328:1561–3. doi: 10.1136/bmj.328.7455.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Department of Health. Putting Prevention First. NHS Health Check: Vascular Risk Assessment and Management. Best Practice Guidance. London: Department of Health; 2009. [Google Scholar]