Abstract
Background
Numerous recommendations have been made for treating idiopathic toe-walking (ITW), but the treatment results have been questioned. The purpose of this study was to investigate whether botulinum toxin A (BTX) improves the walking pattern in ITW as examined with 3-D gait analysis.
Participants and methods
A consecutive series of 15 children (aged 5–13 years) were enrolled in the study. The children underwent a 3-D gait analysis prior to treatment with a total of 6 units/kg bodyweight Botox® in the calf muscles and an exercise program. The gait analysis was repeated 3 weeks and 3, 6, and 12 months after treatment. A classification of toe-walking severity was made before treatment and after 12 months. The parents rated the perceived amount of toe-walking prior to treatment and 6 and 12 months after treatment.
Results
Eleven children completed the 12-month follow-up. The gait analysis results displayed a significant improvement, indicating decreased plantarflexion angle at initial contact and during swing phase and increased dorsiflexion angle during midstance at all post-treatment testing instances. According to the parents’ perception of toe-walking, 3/11 children followed for 12 months had ceased toe-walking completely, 4/11 decreased toe-walking, and 4/11 continued toe-walking. After 6–12 months, the toe-walking severity classification improved in 9 of the 14 children for whom data could be assessed.
Conclusions
A single injection of BTX in combination with an exercise program can improve the walking pattern in children with ITW seen at gait analysis, but the obvious goal of ceasing toe-walking is only occasionally reached.
Keywords: Idiopathic toe-walking, Habitual toe-walking, Toe-walking, Gait analysis, 3-D gait analysis, Botulinum toxin A
Introduction
Some children have a toe-walking gait due to underlying pathology, such as cerebral palsy. In other children, no explanation is found and the diagnosis idiopathic toe-walking (ITW), consequently one of exclusion, is used (synonymous with habitual toe-walking). Children who toe-walk without a known reason are frequently referred to a pediatric orthopedic surgeon.
Several causes of ITW have been suggested, such as delayed development of the cortico-spinal tract [1], vestibular dysfunction [2], congenital short Achilles tendon [3], and even being part of normal gait development [4]. The natural history is not fully evaluated. In a follow-up study of 136 idiopathic toe-walkers [5], only a few of the 49 untreated patients had normal heel–toe gait and 50% of the 49 patients/parents rated the toe-walking as unchanged over a follow-up time of 2–12 years.
A relationship has been reported between persistent toe-walking and the development of ankle equinus [6], which has been associated with several foot problems, for example, plantar fasciitis, metatarsalgia, posterior tibial tendonitis, and Morton’s neuroma [7].
A variety of treatment recommendations have been suggested for ITW, such as physiotherapy [8], serial casting [8–11], and open or percutaneous lengthening of the Achilles tendon [3, 8, 12], but the treatment results have been questioned. Some studies report no difference between serial casting or orthotic treatment versus non-treatment [5, 13]. In a follow-up study of 46 patients treated with Achilles tendon lengthening, only 37% had a normal gait at follow-up after 2–21.5 years and 26% rated themselves as having an unchanged walking pattern [5].
Botulinum toxin A (BTX) has increasingly been used for more than a decade to treat muscular hyperactivity in children with cerebral palsy or dystonia. The effect of BTX is a reversible blockage of cholinergic vesicles, thus, causing a flaccid paralysis of the muscle [14]. In cerebral palsy, the effect of BTX lasts for 3–6 months [15]. BTX treatment has also been introduced in children with ITW. The reported results from two pilot studies on children with ITW, one study on five patients [16] and another in which a combination of BTX, casting, and bracing were used [17], indicate a promising effect, but there is still a need for results from a larger patient population and over a longer follow-up period.
In our orthopedic clinical practice, we frequently receive referrals for the assessment and treatment of children with ITW. Due to our broad experience in the use of BTX in the cerebral palsy population and due to promising preliminary data [16, 17], we were interested in evaluating whether BTX has an effect on gait in children with ITW. Alvarez et al. [18] have recently proposed a classification of ITW based on kinematic and kinetic gait data; however, there is no generally accepted classification of gait for ITW. The primary purpose of this study was to investigate whether BTX treatment improves the walking pattern in children with ITW as examined with 3-D gait analysis and, secondarily, to classify the severity of the toe-walking pattern.
Patients and methods
Participants
A consecutive series of children referred to the pediatric orthopedic clinic at Astrid Lindgren Children’s Hospital between November 2003 and May 2005 were, after examination by a pediatric orthopedic surgeon, considered for study participation. Patient exclusion criteria were previous treatments such as Achilles tendon surgery, casting, orthotics, and BTX. Twenty children met the criteria and were invited to participate in the study, of which 15 children (10 boys and 5 girls, median age 9 years, range 5–13 years) and their parents gave informed consent to participate (Table 1). All children underwent a neurological examination by a pediatric neurologist confirming no underlying neurological or muscular pathology. At each follow-up, the Movement Assessment Battery for Children (Movement ABC) [19] was performed in all children by a physiotherapist and no balance disturbance was found in any child at any follow-up. The same examiners performed all examinations at initial assessment and during the follow-up period.
Table 1.
Patient characteristics, maximum ankle dorsiflexion pre-treatment and 12 months post-treatment, and parent rating of toe-walking pre-treatment and at the 6- and 12-month follow-ups
| Subject | Gender | Age (years) | Max. dorsiflexion of ankle | Parents rating of toe-walking (%) | |||
|---|---|---|---|---|---|---|---|
| Pre | Post 12 m | Pre | Post 6 m | Post 12 m | |||
| 1 | m | 6 | 10 | 5 | 100 | 50 | 100 |
| 2 | m | 11 | 10 | 10 | 75 | 0 | 0 |
| 3 | m | 11 | 5 | 5 | 100 | 25 | 50 |
| 4 | f | 6 | −25 | −20 | 100 | 100 | 100 |
| 5 | f | 9 | 5 | 10 | 75 | 0 | 0 |
| 6 | f | 5 | 20 | 20 | 75 | 25 | 50 |
| 7 | f | 11 | 5 | – | 75 | 50 | – |
| 8 | f | 6 | 0 | – | 100 | 100 | – |
| 9 | m | 5 | 0 | 10 | 100 | 100 | 75 |
| 10 | m | 9 | 0 | – | 100 | – | – |
| 11 | m | 11 | 5 | – | 100 | 50 | – |
| 12 | m | 10 | 10 | 5 | 75 | 75 | 75 |
| 13 | m | 11 | 5 | 5 | 75 | 25 | 0 |
| 14 | m | 13 | 10 | 10 | 100 | 100 | 100 |
| 15 | m | 9 | 15 | 15 | 75 | 50 | 25 |
Max. dorsiflexion of ankle maximum passive ankle dorsiflexion with the knee extended; Pre pre-treatment; Post post-treatment; m months
Negative values indicate plantarflexion
The study was approved by the Medical Ethical Committee at the Karolinska Hospital.
According to the parents, all children had a normal perinatal period, except for one child adopted as an infant whose perinatal period was unknown. All children began walking before 18 months of age. Toe-walking started at walking debut in 10 children, at 24 months in one child (walking debut 10 months), at 36 months in three children (walking debut at 12, 12, and 18 months, respectively), and at 60 months in one child (walking debut at 11 months). Six children had a family history of toe-walking according to their parents.
Botulinum toxin A treatment and stretching program
The children underwent bilateral treatment with a total of 6 units/kg bodyweight Botox® (Allergan, Irvine, CA, USA) with a maximum of 400 units. One hour before the injection, all children were given oral paracetamol (40 mg/kg) and a topical anesthetic cream (EMLA®, AstraZeneca, Sweden) was applied at the injection sites. For patients/parents who requested sedation, 0.3–0.5 mg/kg midazolam was given 15 min prior to injection. Four injection sites in each calf, two in the proximal third of the lateral and medial gastrocnemius bellies and two distally in the gastrocnemius–soleus complex, were administered. All injections were given with electromyogram amplifier guidance to ensure intramuscular position.
After the BTX treatment, the children/parents were instructed by a physiotherapist to perform stretch exercises of the calf muscles five times a week and to walk on heels at least 50 steps a day. The instructions were also given in written form. No orthotic treatment was used in this study.
Gait analysis
Before BTX injection and 3 weeks and 3, 6, and 12 months after treatment, all children underwent 3-D gait analysis using an eight-camera system (Vicon®, Oxford, UK) with 15 retro-reflective markers placed on anatomical landmarks [20]. The children walked barefoot at a self-selected speed along a 10-m walkway and were instructed to walk in their usual manner. Kinematics (joint or segment motion) and kinetics (joint moment and power) data in the three anatomical planes of motion, as well as temporal–spatial parameters, were analyzed for each side. Three trials were analyzed, each containing a single right and left gait cycle. Twenty-seven discrete kinematic and kinetic values from each gait cycle, e.g., maximum dorsiflexion angle or knee extension angle in mid-stance, were obtained from each gait cycle and average values were calculated for each side of each child. Temporal–spatial parameters (cadence, walking speed, step and stride length) were also registered. The classification of ITW severity as per Alvarez et al. [18] was performed based on the initial pre-treatment and again on the final post-treatment gait analysis results. The classification identifies three severity types of ITW (mild, moderate, severe) based on the presence of first ankle rocker (i.e., heel contact), early third ankle rocker (i.e., early heel rise), and predominant ankle plantarflexion moment during loading response (i.e., forefoot loading).
Joint range of motion measurement
Before BTX injection and 3 weeks and 3, 6, and 12 months after treatment, all children underwent an examination by the physiotherapist, during which passive range of motion in the hip, knee, and ankle joints were measured with a goniometer in the supine position. Ankle range of motion was measured with the knee in the extended position.
Parents’ perception of toe-walking and side effects
The parents were asked to rate the time which their child spent on their toes during barefoot walking in the range of 0, 25, 50, 75, or 100% before treatment and at 6 and 12 months after BTX treatment. They were also asked whether they noticed any side effects from the treatment.
Data and statistical analyses
All statistical analysis was based on the intention-to-treat (ITT) principle, i.e., patients included in the study are part of the statistical analysis, even if they withdrew from follow-up.
Gait data were analyzed with a mixed model using commercially available statistical software (SPSS Inc., Chicago, IL, USA). Measurements were performed before treatment and 3 weeks and 3, 6, and 12 months after treatment. The within-subject factors in the mixed model were time (five testing occasions) and side (left and right). Patterns over time were evaluated by Helmert contrast [21], which compares the mean of the dependent variable at time j with the average of the subsequent means, thereby, indicating the time point of the appearance of the treatment effect. A P value < 0.05 was considered to be statistically significant. Passive joint ranges of movement, before treatment and after the 12-month follow-up, were analyzed with the Wilcoxon signed-rank test.
Results
Eleven of 15 children completed the 12-month study period. Three participants were evaluated for 6 months and one patient was evaluated for 3 months. Of the three participants who were followed for 6 months, one child did not attend the 12-month examination due to unrelated illness, one child moved out of the area, and one child (subject 8) opted for other treatment (BTX and below-knee walking plaster for 4 weeks) due to a lack of effect of the original treatment. In one subject, only the 3-month follow-up could be performed due to personal reasons.
Joint range of motion measurement
All children had a normal range of motion in the hip and knee joints before and after treatment. One patient had a 25° equinus contracture and three children achieved a neutral ankle joint position but no dorsiflexion range. There was no significant difference in the passive range of motion of the ankle between the 12-month follow-up and baseline values before treatment (Table 1).
Parents’ perception of toe-walking and side effects
Of the 11 children who were followed for 12 months, three children were reported to completely cease toe-walking and four children decreased their toe-walking from 100 to 50, 100 to 75, 75 to 50, and 75 to 25%, respectively. In four children, the amount of toe-walking (100, 100, 100, and 75%, respectively) was reported as unchanged. In the three children followed for 6 months, the amount of toe-walking decreased in two from 100 to 50 and 75 to 50%, respectively, and in one child, the parents perceived an unchanged 100% toe-walking.
The parents of three children reported that their child had experienced moderate pain in the calves for 2–3 weeks after injection. Two of the children described it as “overuse pain”.
Gait analysis
There were no significant differences in the pelvis and hip parameters during the follow-up period.
Results for the entire study group at the 12-month follow-up compared to pre-treatment showed decreased plantarflexion angle at initial contact (P < 0.001) and during swing phase (P < 0.001), and increased dorsiflexion angle during stance (P < 0.001). Maximum plantarflexion during the gait cycle decreased (P < 0.001). The timing of maximum dorsiflexion and transition from dorsiflexion to plantarflexion ankle position occurred later in the gait cycle at the 12-month follow-up compared to pre-treatment (P < 0.001 and P < 0.001 respectively) (Table 2).
Table 2.
Ankle sagittal plane kinematics and timing in the gait cycle during all follow-ups
| Reference valuea | Pre (N = 15) | Post 3 w (N = 15) | Post 3 m (N = 15) | Post 6 m (N = 14) | Post 12 m (N = 11) | |
|---|---|---|---|---|---|---|
| Ankle angle at icb | 2.1 | −17.1 (9.0) | −6.1 (6.5) | −5.4 (8.1) | −6.3 (8.0) | −6.1 (5.4) |
| Max. df in swingb | 6.1 | −12.2 (8.9) | −3.4 (6.7) | −4.1 (8.4) | −3.2 (7.9) | −2.4 (5.8) |
| Max. df in stanceb | 15.2 | −3.1 (9.2) | 7.3 (7.9) | 6.6 (8.8) | 6.7 (6.2) | 7.6 (5.6) |
| Max. pfb | −12.3 | −29.6 (8.9) | −19.8 (8.4) | −20.1 (9.9) | −20.2 (9.4) | −19.4 (7.1) |
| Timing of max. dfc | 41.5 | 19.4 (7.7) | 31.7 (13.1) | 33.2 (12.6) | 32.3 (12.0) | 32.8 (12.3) |
| Timing of df to pfc | 53.0 | 19.8 (17.5) | 41.8 (18.0) | 43.1 (17.0) | 38.4 (17.2) | 43.2 (16.0) |
Values for pre- and post-treatment are presented as mean (SD)
Pre pre-treatment; Post post-treatment; ic initial contact, df ankle dorsiflexion, pf ankle plantarflexion w weeks; m months
aReference values from the laboratory pediatric control database of 23 children (aged 5–14 years) with typical motor development
bValues are in degrees, where positive values indicate dorsiflexion and negative values indicate plantarflexion
cValues in percent of gait cycle
Analysis with Helmert contrast showed that the observed significant changes in gait analysis variables occurred between the pre-treatment gait evaluation and later follow-ups (P < 0.001), i.e., between the pre-treatment value and the mean of all post-treatment values. There was no significant change between any of the post-treatment follow-up evaluations.
Ankle angle at initial contact, maximum ankle dorsiflexion in stance and in swing for each participant are outlined in (Table 3).
Table 3.
Ankle angle at initial contact, maximum ankle dorsiflexion in stance and in swing for each participant
| Subject | Ankle angle at ica | Max ankle df in stancea | Max ankle df in swinga | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre BTX injection | Post 3 w | Post 12 m | Pre | Post 3 w | Post 12 m | Pre | Post 3 w | Post 12 m | |
| 1 | −9.5 | −6.2 | −5.2 | 2.9 | 8.0 | 3.0 | −9.2 | −5.1 | −4.8 |
| 2 | −18.0 | −4.2 | −4.7 | −1.6 | 6.1 | 3.4 | −12.2 | 2.5 | −4.2 |
| 3 | −5.9 | −3.2 | −6.0 | 12.2 | 7.7 | 13.3 | −0.7 | −1.5 | −0.2 |
| 4 | −14.7 | −8.2 | −15.5 | −1.4 | 0.1 | −7.1 | −16.4 | −9.5 | −16.5 |
| 5 | −16.4 | 1.4 | −0.2 | 1.8 | 9.6 | 8.9 | −8.1 | 4.9 | 3.8 |
| 6 | −12.3 | 2.8 | −2.7 | 1.0 | 18.2 | 10.5 | −8.4 | 6.3 | 0.1 |
| 7 | −22.1 | −3.5 | −5.6 | 10.6 | −18.7 | −2.8 | |||
| 8 | −37.1 | −5.2 | −19.5 | 10.1 | −26.3 | −0.8 | |||
| 9 | −28.6 | −24.6 | −9.3 | −22.3 | 13.5 | 18.5 | −27.5 | −20.9 | 3.6 |
| 10 | −21.4 | −7.5 | −2.3 | 8.7 | −16.9 | −7.8 | |||
| 11 | −20.5 | −14.5 | −7.1 | 9.2 | −9.7 | −6.1 | |||
| 12 | −20.6 | −9.7 | −8.7 | −4.0 | 7.0 | 4.2 | −12.7 | −8.4 | −8.4 |
| 13 | −12.1 | −0.4 | −8.1 | −1.1 | 13.8 | 6.9 | −11.7 | 0.7 | −1.8 |
| 14 | −6.0 | −7.3 | −2.7 | −1.7 | −2.2 | 9.9 | −4.1 | −5.4 | 0.4 |
| 15 | −11.8 | −0.4 | −4.3 | 2.7 | 15.8 | 12.3 | 0.4 | 2.9 | 1.5 |
aValues in degrees
Negative values indicate plantarflexion
ic initial contact; df dorsiflexion; Pre pre-treatment; Post post-treatment w weeks, m months
Dorsi-/plantarflexion angles in two subjects during the entire follow-up period are outlined in (Fig. 1), one subject whose parents reported that toe-walking had ceased (a) and one subject whose parents reported ongoing toe-walking (b).
Fig. 1.
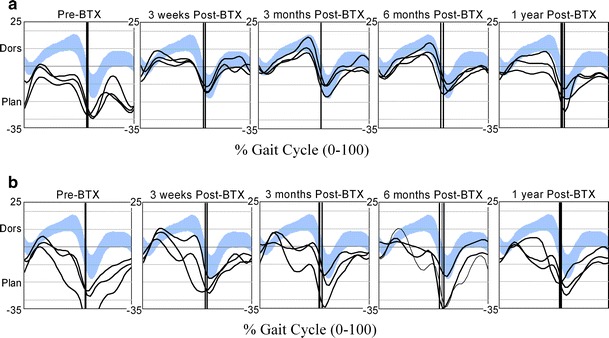
Ankle dorsiflexion angles throughout the gait cycle for three right strides during the evaluation period (before treatment and 3 weeks and 3, 6, and 12 months after treatment) in two participants, shown together with the laboratory pediatric control database of 23 children with typical motor development, aged 5–14 years (mean ± 1 SD, in blue). The parents of the participant in a (subject 2) reported that toe-walking had ceased, and the parents of the participant in b (subject 1) reported that toe-walking had continued
No significant changes in any kinetic or temporal–spatial parameters (cadence, walking speed, step and stride length) were observed.
According to the classification of ITW severity at the initial assessment and the 12-month follow-up in the 14 children for whom all relevant data was available, 9/14 children displayed improvement (Table 4). Four children went from severe to moderate and three from severe to mild (right foot).
Table 4.
Classification of severity of idiopathic toe-walking (ITW) according to Alvarez et al. [18]
| Subject | Pre-treatment | Post-treatment | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| 1 | 3 | 3 | ||
| 2 | 3 | 2 | 2 | 2 |
| 3 | 2 | 2 | 2 | 2 |
| 4 | 3 | 3 | 2 | 2 |
| 5 | 3 | 3 | 1 | 2 |
| 6 | 3 | – | 1 | 2 |
| 7 | 2 | 2 | 2a | 2a |
| 8 | 3 | 2 | 2a | – |
| 9 | – | 3 | 2 | 2 |
| 10 | 2 | 3 | 2a | 2a |
| 11 | 2 | 2 | 2a | 2a |
| 12 | 3 | 3 | 3 | 3 |
| 13 | 3 | 2 | 2 | 1 |
| 14 | 3 | 3 | 1 | 2 |
| 15 | 2 | 2 | 2 | 2 |
1 mild; 2 moderate; 3 severe. Right and left foot presented separately
Post-treatment represents classification at 12 months, except a = 6 months
No value indicates incomplete data for classification
Discussion
This is, to our knowledge, the largest study of the effects of BTX in children with ITW. As measured with 3-D gait analysis, the amount of ankle dorsiflexion angle achieved in stance improved significantly during the follow-up period. A significant improvement was observed in the ankle angle at initial contact and at peak ankle dorsiflexion in swing; however, the ankle positions were still in a plantarflexed position after treatment in nearly all children. This is also confirmed by the parents, who reported that only 3 of 15 children had ceased toe-walking after the treatment period. In the present study, an improvement was found in the timing of both maximum dorsiflexion and transition from dorsiflexion to plantarflexion during stance, i.e., the premature timing in both variables present before treatment were delayed after treatment. This might be an expression of the characteristic gait pattern in ITW with a premature peak dorsiflexion and switch from dorsiflexion to plantarflexion during the gait cycle as described by Crenna et al. [22].
There are several reports [9, 16, 23] about electromyographic changes in ITW with out-of-phase gastrocnemius activity during the swing phase. Brunt et al. [16] showed that swing phase gastrocnemius activity and an early offset of tibialis anterior activity may lead to a toe strike. BTX was reported to change the gastrocnemius activity, resulting in heel strike or nearly heel strike, enabling extended tibialis anterior activity to be present at terminal swing and possibly at loading response. The observed improvement of reduced plantarflexion that was seen in the present study may be attributed to a similar effect. The prolonged effect of BTX on the walking pattern after only one BTX injection is hypothesized to be caused by a modified walking pattern adopted by some children under the influence of BTX.
We did not find any relationship between passive ankle dorsiflexion and the amount of toe-walking, which is in accordance with other studies [22, 24]. Passive range of motion of the ankle was unchanged after BTX treatment; thus, the treatment effect on the walking pattern cannot be attributed to improved passive range of motion of the ankle. The patient with a fixed 25° plantarflexor contracture (subject 4) was included in the study because of a report from a colleague of a similar case with a positive treatment effect. This patient went on to lengthening of the Achilles tendon, tibialis posterior tendon, flexor digitorum communis tendon, and capsulotomies after the study period with a favorable outcome. We now regard a fixed contracture to be a contraindication for BTX treatment.
The children were instructed to walk in their “usual manner” at the gait analysis. It is reported that idiopathic toe-walkers can spontaneously adopt both a toe/forefoot and a heel contact pattern during the same gait analysis [22]. This is very likely the reason why, in this study, less consistency between individual gait cycles was seen compared to other patient populations examined with 3-D gait analysis. It could, thus, be questioned whether a gait analysis represents the child’s most common gait pattern. It might be possible that a child with ITW walks less on her toes when being observed due to activation of higher cerebral functions to monitor the walking pattern, which is normally automatically regulated on the spinal cord level [25]. As the gait analyses were undertaken in the same environment and with the same staff member giving identical instructions, these possible bias effects on the outcome both before and after treatment were hopefully minimized.
We found a significant improvement in several gait analysis parameters, even though only 3 of 15 children ceased toe-walking. According to the parents’ perception of their children’s toe-walking, six children reduced their toe-walking. Even if the questionnaire was not a validated tool, we, nevertheless, regard the parents’ opinion to be very important, as it gives a good indication of the child’s walking pattern in an unobserved environment.
The children who responded to the treatment and ceased toe-walking (subjects 2, 5, and 13) also had a favorable outcome in the long term, as confirmed through telephone contact 3 to 5 years after the end of the study. At that time, two children (subjects 1 and 4) had been operated with Achilles tendon lengthening and ceased toe-walking. Two children (subjects 12 and 14) still had 75–100% toe-walk and were considered for further treatment. The child (subject 8) who was treated with BTX and plaster after the 6-month follow-up ceased toe-walking after that treatment. Two children (subjects 6 and 15) who had decreased their toe-walking during the study period had completely ceased toe-walking or only occasionally walked on their toes. Subjects 3 and 9 still had 50 and 25% toe-walk, but they were not interested in further treatment. Overall, the 12-month follow-up was a good indicator in this study for the outcome in the 3–5-year perspective.
There was no classification available based on gait analysis parameters at the initiation of this study, but since the classification by Alvarez et al. had been published at the time of data analysis [18], this classification was applied. The results for the left and right sides were analyzed separately, but it was occasionally not possible to perform the classification bilaterally due to difficulties in collecting force plate data. Nine out of fourteen children improved their walking pattern with this classification, meaning that either the presence of first ankle rocker, early third ankle rocker, and predominant ankle moment during loading response shifted towards normalization at the gait analysis, even though this does not mean that they stopped toe-walking.
Comparing our result with BTX for ITW versus other treatment options would, of course, have been easier if a generally accepted classification for ITW existed and had been used in previous studies. Improvement after percutaneous lengthening of the Achilles tendon followed by 4 weeks below-knee walking casts was reported in ten patients by Kogan and Smith [12] up to 6 years after treatment, demonstrating the discontinuation of toe-walking in all patients. Stricker and Angulo [13] and Hemo et al. [26] each reported on 15 children with the diagnosis of ITW, who nearly all stopped toe-walking, most of them presenting with an equinus contracture treated by open or percutaneous Achilles tendon lengthening. In the present study, two patients went on to Achilles tendon lengthening after the end of the study period with discontinuing of toe-walking. It seems reasonable to perform an Achilles tendon lengthening when an equinus contracture has developed. When no contracture is present, the question is whether there is a less invasive method available. In this study, we chose one injection of BTX based on the fact that repeated injections of BTX are both expensive and time consuming.
In conclusion, our findings show that a single injection of BTX in combination with an exercise program can improve the walking pattern in children with ITW seen at gait analysis, but the obvious goal of ceasing toe-walking is only occasionally reached. Further studies are needed to evaluate whether repeated injections, BTX treatment in combination with plaster treatment and/or orthotics, as commonly used in the cerebral palsy population, can improve the outcome. Before these studies are conducted, the treatment should be regarded as experimental.
Acknowledgments
We thank the children and their families for participating in this study. We also thank Lotta Duffke and Lars-Olof Olsson for coordinating the follow-ups and gait analyses. Funding of this project was provided by grants from Landstinget Blekinge, Sällskapet Barnavård, and Stiftelsen Konung Oscar II:s och Drottning Sophias Guldbröllopsminne.
Conflict of interest statement
None.
References
- 1.Tachdjian MO. The foot and leg. In: Tachdjian MO, editor. Pediatric orthopedics. Philadelphia: WB Saunders; 1972. [Google Scholar]
- 2.Montgomery P, Gauger J. Sensory dysfunction in children who toe walk. Phys Ther. 1978;58:1195–1204. doi: 10.1093/ptj/58.10.1195. [DOI] [PubMed] [Google Scholar]
- 3.Hall JE, Salter RB, Bhalla SK. Congenital short tendo calcaneus. J Bone Joint Surg Br. 1967;49:695–697. [PubMed] [Google Scholar]
- 4.Weber D. “Toe-walking” in children with early childhood autism. Acta Paedopsychiatr. 1978;43:73–83. [PubMed] [Google Scholar]
- 5.Eastwood DM, Menelaus MB, Dickens DR, Broughton NS, Cole WG. Idiopathic toe-walking: does treatment alter the natural history? J Pediatr Orthop B. 2000;9:47–49. doi: 10.1097/01202412-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Sobel E, Caselli MA, Velez Z. Effect of persistent toe walking on ankle equinus. Analysis of 60 idiopathic toe walkers. J Am Podiatr Med Assoc. 1997;87:17–22. doi: 10.7547/87507315-87-1-17. [DOI] [PubMed] [Google Scholar]
- 7.Hill RS. Ankle equinus. Prevalence and linkage to common foot pathology. J Am Podiatr Med Assoc. 1995;85:295–300. doi: 10.7547/87507315-85-6-295. [DOI] [PubMed] [Google Scholar]
- 8.Tachdjian MO. The child’s foot. Philadelphia: WB Saunders; 1985. [Google Scholar]
- 9.Griffin PP, Wheelhouse WW, Shiavi R, Bass W. Habitual toe-walkers. A clinical and electromyographic gait analysis. J Bone Joint Surg Am. 1977;59:97–101. [PubMed] [Google Scholar]
- 10.Brouwer B, Davidson LK, Olney SJ. Serial casting in idiopathic toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop. 2000;20:221–225. [PubMed] [Google Scholar]
- 11.Fox A, Deakin S, Pettigrew G, Paton R. Serial casting in the treatment of idiopathic toe-walkers and review of the literature. Acta Orthop Belg. 2006;72:722–730. [PubMed] [Google Scholar]
- 12.Kogan M, Smith J. Simplified approach to idiopathic toe-walking. J Pediatr Orthop. 2001;21:790–791. [PubMed] [Google Scholar]
- 13.Stricker SJ, Angulo JC. Idiopathic toe walking: a comparison of treatment methods. J Pediatr Orthop. 1998;18:289–293. [PubMed] [Google Scholar]
- 14.Graham HK, Aoki KR, Autti-Rämö I, Boyd RN, Delgado MR, Gaebler-Spira DJ, Gormley ME, Guyer BM, Heinen F, Holton AF, Matthews D, Molenaers G, Motta F, García Ruiz PJ, Wissel J. Recommendations for the use of botulinum toxin type A in the management of cerebral palsy. Gait Posture. 2000;11:67–79. doi: 10.1016/S0966-6362(99)00054-5. [DOI] [PubMed] [Google Scholar]
- 15.Koman LA, Mooney JF, 3rd, Smith B, Goodman A, Mulvaney T. Management of cerebral palsy with botulinum-A toxin: preliminary investigation. J Pediatr Orthop. 1993;13:489–495. doi: 10.1097/01241398-199307000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Brunt D, Woo R, Kim HD, Ko MS, Senesac C, Li S. Effect of botulinum toxin type A on gait of children who are idiopathic toe-walkers. J Surg Orthop Adv. 2004;13:149–155. [PubMed] [Google Scholar]
- 17.Jacks LK, Michels DM, Smith BP, Koman LA, Shilt J. Clinical usefulness of botulinum toxin in the lower extremity. Foot Ankle Clin. 2004;9:339–348. doi: 10.1016/j.fcl.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Alvarez C, De Vera M, Beauchamp R, Ward V, Black A. Classification of idiopathic toe walking based on gait analysis: development and application of the ITW severity classification. Gait Posture. 2007;26:428–435. doi: 10.1016/j.gaitpost.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Henderson SE, Sugden DA (1992) Movement ABC. The Movement Assessment Battery for Children. The Psychological Corporation, London
- 20.Davis RB, 3rd, Öunpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci. 1991;10:575–587. doi: 10.1016/0167-9457(91)90046-Z. [DOI] [Google Scholar]
- 21.Crowder MJ, Hand DJ. Analysis of repeated measures. London: Chapman & Hall; 1990. [Google Scholar]
- 22.Crenna P, Fedrizzi E, Andreucci E, Frigo C, Bono R. The heel-contact gait pattern of habitual toe walkers. Gait Posture. 2005;21:311–317. doi: 10.1016/j.gaitpost.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Kalen V, Adler N, Bleck EE. Electromyography of idiopathic toe walking. J Pediatr Orthop. 1986;6:31–33. doi: 10.1097/01241398-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Stott NS, Walt SE, Lobb GA, Reynolds N, Nicol RO. Treatment for idiopathic toe-walking: results at skeletal maturity. J Pediatr Orthop. 2004;24:63–69. doi: 10.1097/01241398-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Kandel ER, Schwartz JH. Principles of neural science. 2. New York: Elsevier; 1985. [Google Scholar]
- 26.Hemo Y, Macdessi SJ, Pierce RA, Aiona MD, Sussman MD. Outcome of patients after Achilles tendon lengthening for treatment of idiopathic toe walking. J Pediatr Orthop. 2006;26:336–340. doi: 10.1097/01.bpo.0000217743.44609.44. [DOI] [PubMed] [Google Scholar]


