Abstract
Objective
The management and the diagnostic modalities used in cases of undisplaced greenstick and torus fractures of the distal radius in children vary between different treatment centres. The aim of this study was twofold: firstly, to analyse the sensitivity of X-rays versus ultrasound to diagnose these fractures; secondly, to compare three available treatment options (plaster cast, Futuro splints, and double Tubigrip) in terms of pain, analgesia requirements, grip strength, deformity, stiffness and interference with a child’s activities of daily living.
Methods
We prospectively included 79 patients suffering from undisplaced greenstick and torus fractures of the distal radius. Patients were randomized (single blindly) to the studied treatment groups.
Results
In terms of diagnosis, the ultrasound was found to be more sensitive than X-rays for diagnosing these fractures. Our results also showed that Tubigrip was superior in terms of interference with a child’s ADLs, stiffness and grip strength. However, there was no difference in the levels of pain, analgesia required, and deformity.
Conclusion
These results support the idea that ultrasound is an effective and sensitive tool for detecting undisplaced greenstick and torus fractures of the distal radius in children. Treating these fractures with functional nonrigid devices (Tubigrip) results in improved function without increased discomfort or deformity.
Keywords: Torus, Greenstick, Ultrasound
Introduction
The management of minimally angulated greenstick and torus fractures of the distal radius in children varies between different centres [7]. The diagnosis is established mainly by the clinical findings and confirmed by plain X-rays [6]. The treatment most commonly offered includes immobilization for a short period of time in plaster-of-Paris, either a backslab or a full cast [3, 7]. Alternative treatment includes immobilization with a Futuro wrist splint [3]. Follow-up arrangements may or may not be made, with some centres performing further X-rays [1, 4, 7, 12]. These fractures are usually stable and heal without difficulty [11].
The literature suggests that in other long bones where stable fractures exist, early functional treatment, avoiding splints and immobilisation lead to superior results [7, 9]. Stable fractures of the ankle in children have been successfully treated with double Tubigrip devices, and outcomes are superior to those treated with plaster cast immobilisation [8]. Questions that often arise whenever such stable fractures in children are treated with minimal splintage and early function include the following. Will it be too painful for the child? Will it be adequate to prevent further injury or displacement of the fracture? Do splints in children cause unnecessary stiffness, weakness, and interference with a child’s activities of daily living, which can be minimised through early functional treatment if applied appropriately? Is an X-ray required for the diagnosis, or is ultrasound an alternative investigation?
This study was designed to try to answer these questions. Three treatment regimes assigned randomly, using either plaster cast, Futuro wrist splints or double Tubigrip, were evaluated. X-ray and ultrasound of the injured limb was performed on every patient at the initial visit to the clinic, and at a follow-up visit within 4–6 weeks.
Patients and methods
Inclusion criteria included all children aged 0–16 sequentially attending our treatment centre, at the University Hospitals of Coventry and Warwickshire, who had sustained a minimally angulated greenstick or torus fracture of the distal third of the radius, as confirmed by either X-ray or ultrasound. The term “minimally angulated” was defined as a complete absence of any discernible clinical deformity, which on a plain X-ray would be less than 10° of angulation in any plane. All patients meeting the criteria received a plain X-ray in the accident and emergency department, and also received an ultrasound scan of the injury within the first 2–3 days of the injury (mean 1.4 days) using an Aloka SSD-500 echo camera ultrasound machine (Aloka Co., Japan) with a 7.5 MHz probe. The child was offered an opaque pot containing equal numbers of sweets of three different colours in such a way that they could not see what colour they were picking. Each colour was a code for the treatment that would be applied to the child, be it a plaster cast, a Futuro wrist splint, or a double Tubigrip. Once applied, the parent and child were given advice, a follow-up appointment within 4–6 weeks (32.9 ± 3.6 days for the POP group, 34.5 ± 2.9 days for the Futuro group, and 32.7 ± 3.7 days for the Tubigrip group), and an arrangement to return sooner in the event of concerns or problems regarding the child. At the follow-up appointment, a single observer carried out a clinical and radiological assessment after the treatment device had been removed in a separate room and the child had been sent for an X-ray. The clinical assessment involved recordings of the injury with respect to date and standard data collection of the patient’s age, sex, address, etc. In addition, a visual analogue scale of 0–10 was used to quantify the average pain level of the preceding weeks, with a separate recording of analgesic requirement, classified as none, occasional or regular. These groupings were given scores of 0, 5, and 10, respectively. A “paediatric disability score” was devised by scoring 0–10 in five separate areas (total of 50) relevant to a child. These areas included the following, with their respective scores: (a) interference with play (minimal, 0; moderate, 5; severe, 10); (b) help needed with feeding (none, 0; some, 5; lots, 10); (c) help needed with washing and dressing (none, 0; some, 5; lots, 10); (d) sleep disturbance (none, 0; some nights, 5; most nights, 10); (e) missed days of school (none, 0; 1–5 days, 5; >5 days, 10). The child was further assessed with regards to the presence of a clinical deformity, and the magnitude was recorded in degrees of angulation. The grip strength of the child was recorded as 0–5 using the MRC grading system [5]. Stiffness in the wrist was then recorded as degrees of lost movement. Finally, an ultrasound was carried out to assess the appearance of healing callus and the disappearance of the hypoechoic zone. A final appointment in 12 weeks was given to ensure that all children had returned to full function.
Results
A total of 90 patients who sequentially attended the paediatric fracture clinics, met the inclusion criteria, and provided their consent were recruited into the study over a period of ten months. There were only two cases where parents declined consent, and these were treated with a plaster cast and not included in the study. Eleven patients were lost to follow up due to non-attendance at the follow-up clinic. This left 79 patients for whom results were obtained. Of these 79 patients, there were 32 females and 47 males, with a mean age of 9 (range 2–16). All of the fractures fulfilled the criteria of being in the distal third of the radius, of being either a greenstick or torus fracture, and of being angulated <10° without a clinical deformity. Twenty-six patients received treatment in a Futuro wrist splint, 24 in a plaster cast, and 29 in a double Tubigrip.
X-ray versus ultrasound for diagnosis and follow-up
The appearance of a fracture on ultrasound is that of a hypoechoic zone transcending through the bone originating at the cortex (Figs. 1, 2). All 79 fractures were seen on ultrasound. Four fractures were not obvious on X-rays, and the remaining 75 were seen on X-rays. All 79 fractures showed radiologically visible signs of healing on both X-ray and ultrasound modalities (Fig. 2).
Fig. 1.
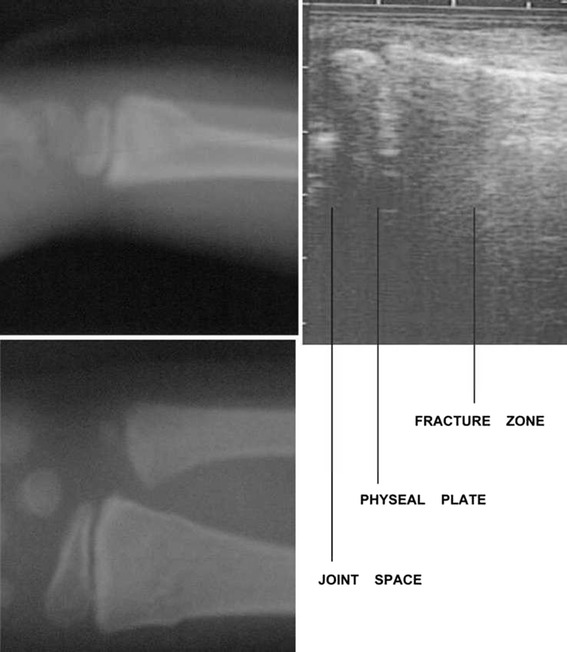
X-ray and ultrasound appearance of an acute undisplayed fracture of the distal third of the radius. The fracture appears on ultrasonography as a hypoechoic zone
Fig. 2.
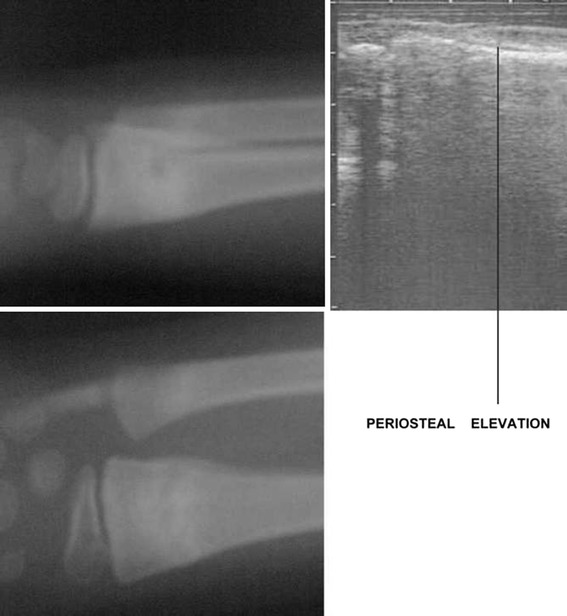
X-ray and ultrasound appearance of the same fracture at 6 weeks. Note the appearance of callus as seen on ultrasonography
Pain scores
The Futuro splint group had pain scores ranging from 0–9, with a mean of 3.1 (Fig. 3). The plaster cast group had pain scores ranging from 0–9, with a mean of 2.9. The Tubigrip group had pain scores ranging from 0–8, with a mean of 2.3. A one-way analysis of variance resulted in a F value with 2 and 76 degrees of freedom of 0.91, which is not significant at the P < 0.05 level.
Fig. 3.
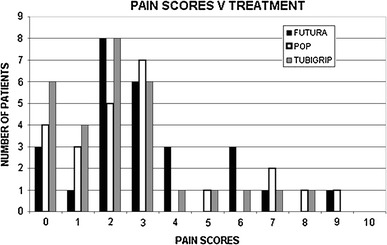
Graphical representation of pain scores vs. treatment results
Analgesic requirement
No difference in the analgesic requirements was observed irrespective of the treatment used (Fig. 4). A one-way analysis of variance gave a F value (degrees of freedom 2, 76) of 1.48, which is not significant at the P < 0.05 level.
Fig. 4.
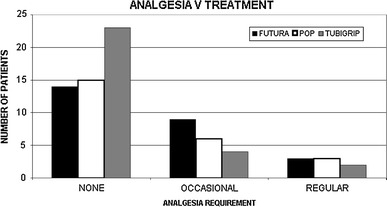
Graphical representation of analgesia requirement vs. treatment results
Paediatric disability score
The Futuro splint group had a PDS ranging from 0–30 (mean 7.7) (Fig. 5). The plaster cast group had a PDS range of 0–35 (mean 10). The Tubigrip group had a PDS range of 0–10 (mean 1.9). One-way analysis of variance gave a F value (degrees of freedom 2, 76) of 10.72, which is significant at the P < 0.001 level.
Fig. 5.
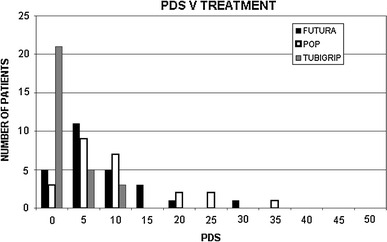
Graphical representation of paediatric disability score vs. treatment results
Deformity
There was an increase in the deformity seen in four patients (Fig. 6). All were less than five degrees of clinical deformity. Two occurred in patients treated in a Futuro splint, one for whom treatment comprised a plaster cast and the other for whom the treatment involved a double Tubigrip. One-way analysis of variance gave a F value (degrees of freedom 2, 76) of 0.24, which is not significant at the P < 0.05 level.
Fig. 6.
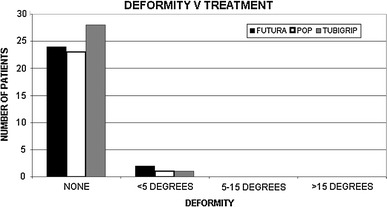
Graphical representation of deformity vs. treatment results
Grip strength
The range for the Futuro group was 4–5 (mean 4.9), for the plaster cast group 4–5 (mean 4.6), and for the Tubigrip group 5 (mean 5) (Fig. 7) One-way analysis of variance resulted in a F value (degrees of freedom 2, 76) of 8.36, which is significant at the P < 0.001 level.
Fig. 7.
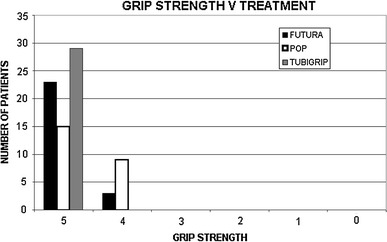
Graphical representation of grip strength vs. treatment results
Stiffness
The range of movement lost in degrees for the Futuro group was 0–20 (mean 3), for the plaster cast group 0–20 (mean 5), and for the Tubigrip group 0 (mean 0) (Fig. 8). One-way analysis of variance gave a F value (degrees of freedom 2, 76) of 5.49, which is significant at the P < 0.01 level.
Fig. 8.
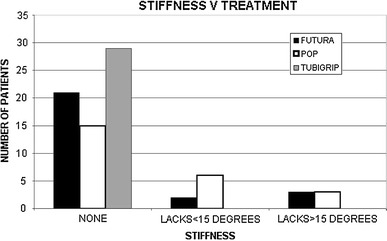
Graphical representation of stiffness vs. treatment results
Discussion
Three million children attend accident and emergency departments each year in the UK [7]. Distal forearm fractures account for approximately 30% of all fractures in children [2]. A significant proportion of these fractures are diagnosed as torus or greenstick fractures [2]. A torus fracture results from a compressive force acting on the metaphysis of the bone, which is a point of decreased strength [14]. Greenstick fractures occur in the same way, but more severe forces are applied, and the disruption of one cortex occurs while the other is bent [7]. In this study we included torus fractures and minimally angulated greenstick fractures (less than 10° angulation), as both types present and treated in the same manner. In addition, in many cases it is difficult to radiologically differentiate these two types of fracture.
The first part of the study investigated the sensitivity of ultrasound for the detection of these fractures. The results showed that ultrasound is more sensitive in terms of detecting the fractures than X-rays, and both are equivalent with respect to assessing radiological signs of healing. Other than being difficult to interpret, and operator dependent, it has many advantages over plain X-rays with regards to cost and ionising radiation [10, 15]. The patient can have an ultrasound in the accident and emergency department. With appropriate measures in place, it is conceivable that the management of such injuries could bypass the fracture clinic altogether.
In terms of management, traditional treatments involve up to four weeks of immobilization in a rigid below-elbow cast [3, 7]. Alternative treatments include removable splints [13], wool and bandage [14], or soft tubular elasticated bandage (i.e. Tubigrip). Cast immobilization is the traditional treatment of choice, but there is no consensus regarding the best treatment modality.
Our results showed that there is no difference in pain scores or analgesic requirements, regardless of the treatment modality used. The paediatric disability score was significantly lower in the group treated with a Tubigrip in comparison with the other two treatment groups. The form of treatment does not bear any significant relation to further deformity at the fracture site. The grip strength and stiffness were significantly improved in the Tubigrip group as compared to the other two treatment groups.
The logical explanation for the results that show improved grip strength and stiffness in the Tubigrip group over the plaster cast and Futuro splint groups is that the former does not immobilise the joint or restrict muscular activity in the limb beyond that which is within the limits of pain. The PDS scores are also lower in this group compared to the other two groups for the same reasons. By allowing the child to use the limb within the limits of their own pain, less interference with function is encountered than when splinting the arm and immobilising the wrist joint.
The results showing an increase in deformity are a little harder to explain. It would seem that by not rigidly splinting the arm, there is a higher risk of further deformity occurring at the fracture site. The history of each patient in whom further angulation occurred was scrutinised in a more detailed manner. It was found that all four children were not compliant with the treatment and advice given. These children had a higher level of personal energy and their injuries were associated with high-risk activities that included skateboarding, biking, and roller skating. The boy who received treatment with a plaster cast and exhibited further deformation appeared to have been using his plaster cast arm as a weapon, and had incurred recurrent beatings from his sibling, often involving his head. Re-injury was found to be the reason for the occurrence of further deformation, rather than an element of instability at the fracture site. The vulnerability of the arm when it is not encased in a protective splint lends itself to increased protection on the part of the patient, and this is probably why re-injury was not common in the group who were treated with a Tubigrip.
Conclusion
The present study supports the idea that ultrasound is an effective and sensitive tool for detecting these fractures. In regard to the treatment options, nonrigid devices (e.g. a Tubigrip) result in improved function without increased discomfort or deformity.
Acknowledgments
Conflict of interest statement
None of the authors had any conflicts of interest.
Contributor Information
Ippokratis Pountos, Email: pountos@doctors.org.uk.
Asim Siddiqui, Phone: +78-70-343280, Email: asim.siddiqui@cht.nhs.uk.
References
- 1.Bochang C, Katz K, Weigl D, Jie Y, Zhigang W, Bar-On E. Are frequent radiographs necessary in the management of closed forearm fractures in children? J Child Orthop. 2008;2:217–220. doi: 10.1007/s11832-008-0101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyer BA, Overton B, Schrader W, Riley P, Fleissner P. Position of immobilization for paediatric forearm fractures. J Pediatr Orthop. 2002;22:185–187. [PubMed] [Google Scholar]
- 3.Davidson JS, Brown DJ, Barnes SN, Bruce CE. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br. 2001;83:1173–1175. doi: 10.1302/0301-620X.83B8.11451. [DOI] [PubMed] [Google Scholar]
- 4.Donald S. Pediatric distal radius and forearm fractures. J Hand Surg. 2008;33:1911–1923. doi: 10.1016/j.jhsa.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 5.Dyck PJ, Boes CJ, Mulder D, Millikan C, Windebank AJ, Dyck PJ, Espinosa R. History of standard scoring, notation, and summation of neuromuscular signs. A current survey and recommendation. J Peripher Nerv Syst. 2005;10:158–173. doi: 10.1111/j.1085-9489.2005.0010206.x. [DOI] [PubMed] [Google Scholar]
- 6.Farbman KS, Vinci RJ, Cranley WR, Creevy WR, Bauchner H. The role of serial radiographs in the management of pediatric torus fractures. Arch Pediatr Adolesc Med. 1999;153:923–925. doi: 10.1001/archpedi.153.9.923. [DOI] [PubMed] [Google Scholar]
- 7.Firmin F, Crouch R. Splinting versus casting of “torus” fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs. 2009;17:173–178. doi: 10.1016/j.ienj.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Gleeson AP, Stuart MJ, Wilson B, Phillips B. Ultrasound assessment and conservative management of inversion injuries of the ankle in children: plaster of Paris versus Tubigrip. J Bone Joint Surg Br. 1996;78:484–487. [PubMed] [Google Scholar]
- 9.Howes MC, Cutting P, Thomas M. Splinting of buckle fractures of the distal radius in children. Emerg Med J. 2008;25:222–223. doi: 10.1136/emj.2008.058172. [DOI] [PubMed] [Google Scholar]
- 10.Hubner U, Schlicht W, Outzen S, Barthel M, Halsband H. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br. 2000;82:1170–1173. doi: 10.1302/0301-620X.82B8.10087. [DOI] [PubMed] [Google Scholar]
- 11.Plint AC, Perry JJ, Correll R, Gaboury I, Lawton L. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics. 2006;117:691–697. doi: 10.1542/peds.2005-0801. [DOI] [PubMed] [Google Scholar]
- 12.Symons S, Rowsell M, Bhowal B, Dias JJ. Hospital versus home management of children with buckle fractures of the distal radius. A prospective, randomised trial. J Bone Joint Surg Br. 2001;83:556–560. doi: 10.1302/0301-620X.83B4.11211. [DOI] [PubMed] [Google Scholar]
- 13.van Bosse HJ, Patel RJ, Thacker M, Sala DA. Minimalistic approach to treating wrist torus fractures. J Pediatr Orthop. 2005;25:495–500. doi: 10.1097/01.bpo.0000161098.38716.9b. [DOI] [PubMed] [Google Scholar]
- 14.West S, Andrews J, Bebbington A, Ennis O, Alderman P. Buckle fractures of the distal radius are safely treated in a soft bandage—a randomized prospective trial of bandage versus plaster cast. J Pediatr Orthop. 2005;25:322–325. doi: 10.1097/01.bpo.0000152909.16045.38. [DOI] [PubMed] [Google Scholar]
- 15.Williamson D, Watura R, Cobby M. Ultrasound imaging of forearm fractures in children: a viable alternative? J Accid Emerg Med. 2000;17:22–24. doi: 10.1136/emj.17.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]


