Abstract
Purpose
Accurate evaluation of patient compliance with scoliosis brace usage has been a challenge for physicians treating patients with adolescent idiopathic scoliosis. This inability to accurately measure compliance has resulted in difficulty in determining brace treatment efficacy. This prospective study was performed to demonstrate the efficacy of using a new electronic brace compliance monitor, the Cricket.
Methods
The Cricket is a small encased circuit that can be attached to the brace and, by means of a temperature sensor, can record brace wear times. This study included ten subjects with adolescent idiopathic scoliosis who were prescribed the Wilmington scoliosis brace (thoraco-lumbo-sacral orthosis) into which the Cricket sensor was incorporated. Subjects kept a diary of brace wear times.
Results
Comparisons of data for the Cricket, subject diaries, and prescribed brace wear were evaluated. The mean error between the diary times and Cricket recording was 2%. Patient compliance was 78%.
Conclusions
The Cricket is a reliable, accurate, and sensitive device to determine patient compliance with scoliosis brace usage.
Keywords: Idiopathic scoliosis, Thoraco-lumbo-sacral orthosis, Brace compliance, Compliance sensor, Scoliosis brace efficacy
Introduction
Bracing is a non-operative treatment used to contain spine curvature due to adolescent idiopathic scoliosis (AIS). The effectiveness of bracing is still a matter of considerable debate. There have been no multi-center, multi-brace, randomized studies that have investigated brace efficacy in containing scoliosis. One of the factors affecting the outcome is brace wear compliance, which also provides a reliable measure of internal validity for a study. The lack of actual compliance data has made current reports of brace efficacy for the treatment of idiopathic scoliosis unreliable.
Previous studies have used either questionnaires to determine compliance [1, 2] or verbal reports on the number of hours worn to a nurse at the clinic [3, 4]. The number of wear hours reported in these studies was subjective and difficult to verify due to reliance on patient recall, with the possibility of false reporting. Others have looked at developing objective ways of measuring brace wear compliance by using pressure monitoring [5–7] or temperature sensing [8–12]. These sensors worked; however, they were bulky.
In a previous study by this group [13, 14], an electronic compliance monitor was shown to objectively measure brace wear compliance for patients with AIS. The study highlighted some shortcomings in the old sensors, such as being bulky, difficult to attach to the brace, difficult to download, being fragile, not being waterproof, and not having an LCD readout for daily feedback to the patient and family. The purpose of this study was to address some of the earlier technical shortcomings and to determine the efficacy of using the Cricket as a reliable and accurate means of measuring the compliance of Wilmington brace wear in the treatment of idiopathic scoliosis.
Materials and methods
After Institutional Review Board approval, ten patients (two boys and eight girls, mean age 13.3 years) with AIS from the existing outpatient clinic of J. Richard Bowen, M.D. at the Alfred. I. duPont Hospital for Children agreed to participate in the study (Table 1). Inclusion criteria for patients in this study were AIS, treatment with the Wilmington scoliosis brace, and agreement to keep a daily manual diary of brace wear. The Wilmington brace is a custom brace made of low-temperature plastic. Prescribed regimens for brace wear time were 8 (night time) or 12 h per day, depending on the severity of the scoliosis.
Table 1.
Patient demographics and curve characteristics
| Patient | Age (years) | Gender | Curve | Curve (°) | Risser | Prescribed time (h) |
|---|---|---|---|---|---|---|
| 1 | 13.1 | Female | T6-T12 | 30 | 0 | 12 |
| 2 | 13.5 | Female | T11-L3 | 41 | 2 | 12 |
| 3 | 15 | Male | T4-T7 | 23 | 3 | 12 |
| 4 | 13.7 | Female | T4-T11 | 24 | 0 | 12 |
| 5 | 14.2 | Female | T9-L3 | 26 | 4 | 8 |
| 6 | 16.4 | Male | T12-L4 | 28 | 0 | 8 |
| 7 | 12.6 | Female | T11-L3 | 28 | 0 | 8 |
| 8 | 10.3 | Female | T5-T12 | 30 | 0 | 12 |
| 9 | 13.2 | Female | T6-T11 | 46 | 1 | 12 |
| 10 | 11.4 | Female | T5-T11 | 20 | 0 | 8 |
The Cricket is a novel compliance sensor designed by this group from the ground up specifically for this purpose. It is 3 cm in diameter and 1 cm in thickness. It is a self-contained circuit that includes a thermistor for temperature sensing, sufficient memory to record 9 months at one reading every 10 min, and an LCD readout that displays the average daily wear time (Fig. 1). The sensor was placed in the lumbar mold cavity, putting it on the outside of the brace. The thermistor protrudes from the sensor, allowing it to go into a hole in the brace so that it is flush with the inside of the brace. The Cricket was attached and launched at the initial visit and removed after approximately 1 month of brace wear, at which time the data were downloaded and the manual brace wear diary was collected. The data were downloaded wirelessly from the Cricket.
Fig. 1.

a Shows the front and back of the cricket sensor. b Cricket mounted on the lumbar mold
The custom-designed software (Creative Micro Designs, Newark, DE) for the Cricket allows the retrieval of temperature data, which is converted to an Excel file. This file includes the date of launch, days worn, average daily wear in hours, and graphs daily brace wear and a graph that shows the percentage likelihood of the subject wearing the brace at a given time in a 24-h period. This is shown in Fig. 2 for one of the subjects.
Fig. 2.
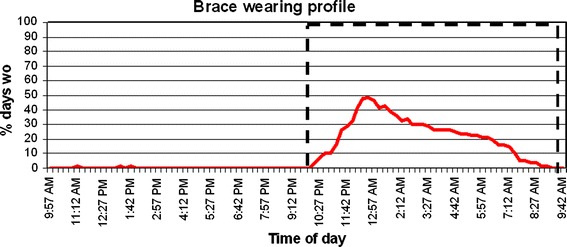
Brace-wearing profile of a typical subject. The y-axis represents the number of days worn, expressed as a percentage of the total days. The x-axis is the time in a 24-h period
The graph in Fig. 2 shows that this patient only wore the brace at night. Peak wearing time was around 1:00 a.m., when she wore it only 50% of the total number of days. The compliance drops off at other times during the night, which indicates that the brace was taken off during the night for some of the nights. Ideally, one would like to see a square-shaped graph with an amplitude of 100% for the duration of the prescribed wear time (Fig. 2). This would indicate that the patient wore the brace every day for the prescribed period. Subjects were also asked to keep a manual diary of wear times for a 1-month period.
Results
The computer reads the raw data as temperature values that are measured every 10 min. If the brace is being worn, the temperature measured will be close to skin temperature. If the brace is not being worn, it will record ambient temperature, which, typically, will be much lower than the skin temperature.
Temperature data files were converted to hours worn by setting a threshold temperature. Temperatures above and below this threshold were categorized as brace-on and brace-off conditions, respectively. Brace-on hours were aggregated, and actual hours worn for each monitoring period were calculated. Compliance is defined as the ratio of measured brace wear time to prescribed brace wear time. Compliance was determined by the percentage of actual hours worn in accordance with the prescribed regimen during brace treatment.
Table 2 describes the compliance data by patient. The prescribed brace wear time is 8 or 12 h per day and is based on the severity of the scoliosis. Diary time is calculated by manually aggregating the daily worn time from the patient diary. Sensor worn time is obtained from the Cricket sensor as described earlier. The percentage error is the difference between sensor and diary times. The compliance rates are obtained from the following formula: (sensor wear time × 100)/prescribed time. Patient 4 had an error of 37.9%. Additionally, this was a very non-compliant subject, as can be seen from the worn times for both the manual diary and electronic sensor. The errors for the remaining subjects were between −1.6 and 5.3%. The negative error indicates that this patient’s manual diary time was reported to be less than the time measured by the sensor.
Table 2.
Wear time results for the ten subjects wearing their scoliosis braces
| Patient | Prescribed time (h) | Worn time (diary) | Worn time (sensor) | Error (%) | Compliance (%) |
|---|---|---|---|---|---|
| 1 | 12 | 11.77 | 11.71 | 0.5 | 97.6 |
| 2 | 12 | Software error | |||
| 3 | 12 | 8.74 | 8.7 | 0.5 | 72.5 |
| 4 | 12 | 5.8 | 3.6 | 37.9 | 30.0 |
| 5 | 8 | 7.6 | 7.2 | 5.3 | 90.0 |
| 6 | 8 | 2.8 | 2.8 | 0.0 | 35.0 |
| 7 | 8 | 6.6 | 6.6 | 0.0 | 82.5 |
| 8 | 12 | 12.9 | 13.1 | −1.6 | 109.2 |
| 9 | 12 | 10.4 | 10.0 | 3.8 | 83.3 |
| 10 | 8 | 8.6 | 8.2 | 4.7 | 102.5 |
Ten patients completed the study. The sensor for patient 2 did not yield useful data as a previous version of the software was inadvertently loaded, resulting in bad data.
Discussion
Bracing is a commonly used non-operative treatment for AIS [15–20]. However, many orthopedists, including the authors, are not sure whether bracing works in many cases or, if it does, for which curves it is most effective or for how long the brace must be worn. Brace compliance to prescribed brace usage has traditionally been obtained by questioning the patient and family, which may be inaccurate. Some researchers have used a questionnaire to determine the number of hours that the brace is worn [1, 2]. There are other reports in which the number of hours worn was reported to a nurse at the clinic [3, 4]. The number of hours reported by patients in these previous studies has been subjective and is probably not accurate. Some authors did not exclude the non-compliant patients from their studies because of the difficulty in distinguishing between compliant and non-compliant patients [18–20]. Bassett et al. found that the key prognostic factors for success of the Wilmington brace for AIS treatment appeared to be the severity and flexibility of the curve at the start of treatment [15]. However, brace compliance has been difficult, if not impossible, to determine objectively.
A prior study by us [13] and several others more recently have shown the ability to accurately measure the number of hours of brace wear using a thermal sensor [9, 10] or pressure monitor [6, 7]. We developed a de novo compliance sensor, the Cricket, that overcomes these undesirable features and the purpose of this paper is to describe its usefulness. The Cricket is small, being only 1-cm thick and having a 1.5-cm radius. Therefore, it is much easier to place in standard braces. Typically, the Cricket is hidden in the brace molds, which allows the surface of the brace to be smooth and contoured. The Cricket is shock-proof and sealed to prevent water penetration. The LCD is placed toward the outside of the brace, which allows the patient and parents to read daily wear or accumulated usage. This supports the patients’ understanding of compliance and allows parents to encourage proper brace usage. Although feedback from the LCD data were not used in this paper, anecdotal evidence from parents showed that the readout was a positive attribute and helped the patient stay on track with prescribed wear time.
Overall, with the exception of one patient, the diary had good agreement with the electronic sensor, with the error being 2% on average. A previous study by Dolan et al. [9] also compared manual diary with the sensor for compliance; however, they used brace-wearing volunteers and concluded that electronic monitoring was an accurate and reliable proxy for the manual logging of data. We believe that all but one patient was very diligent with their manual diary. This study did meet its designed goal of prospectively documenting that the Cricket is a reliable, accurate, and sensitive device to determine patient compliance with scoliosis brace usage. The main drawback of the study was the small number of patients and the absence of a gold standard for measuring compliance.
Conclusions
A new electronic compliance sensor, the Cricket, has been shown to be effective and reliable in measuring brace-wearing times in the treatment of AIS. The new sensor is compact, robust and can be easily mounted by an orthotist. The software provides valuable clinical information, such as daily brace wear times and average wearing habits of patients being treated for adolescent idiopathic scoliosis (AIS) with a thoraco-lumbo-sacral orthosis. The use of compliance sensors for monitoring brace wear can eliminate a significant variable in the investigation of brace efficacy.
Acknowledgments
We would like to thank Lawall Prosthetics and Orthotics for integrating the sensors into the braces and Creative Micro Designs for manufacturing and providing the Cricket sensors.
Contributor Information
Tariq Rahman, Phone: +1-302-6516831, FAX: +1-302-6516895, Email: trahman@nemours.org.
Battugs Borkhuu, Email: bbattugs@yahoo.com.
Aaron G. Littleton, Email: aglittleton@yahoo.com
Whitney Sample, Email: wsample@nemours.org.
J. Richard Bowen, Email: jrbowen@nemours.org.
References
- 1.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76:1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Wiley JW, Thomson JD, Mitchell TM, Smith BG, Banta JV. Effectiveness of the Boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine. 2000;25:2326–2332. doi: 10.1097/00007632-200009150-00010. [DOI] [PubMed] [Google Scholar]
- 3.Gurnham RB. Adolescent compliance with spinal brace wear. Orthop Nurs. 1983;2:13–17. doi: 10.1097/00006416-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 4.DiRaimondo CV, Green NE. Brace-wear compliance in patients with adolescent idiopathic scoliosis. J Pediatr Orthop. 1988;8:143–146. doi: 10.1097/01241398-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Houghton GR, McInerney A, Tew A. Brace compliance in adolescent idiopathic scoliosis. J Bone Joint Surg Br. 1997;69:852. [Google Scholar]
- 6.Lou E, Raso JV, Hill DL, Durdle NG, Mahood JK, Moreau MJ. The daily force pattern of spinal orthoses in subjects with adolescent idiopathic scoliosis. Prosthet Orthot Int. 2002;26:58–63. doi: 10.1080/03093640208726622. [DOI] [PubMed] [Google Scholar]
- 7.Havey R, Gavin T, Patwardhan A, Pawelczak S, Ibrahim K, Andersson GBJ, Lavender S. A reliable and accurate method for measuring orthosis wearing time. Spine. 2002;27:211–214. doi: 10.1097/00007632-200201150-00018. [DOI] [PubMed] [Google Scholar]
- 8.Lavelle JR, Smith K, Platts R, Morley TR, Ransford AO, Edgar MA. An assessment of brace compliance in adolescent idiopathic scoliosis using a new brace timer. J Bone Joint Surg Br. 1996;78:162. [Google Scholar]
- 9.Dolan LA, Sabesan VJ, Shurr DG, Weinstein SL (2004) Reliability and validity of electronic temperature reading as proxy for TLSO wear time. In: Proceedings of the Association of Children’s Prosthetics–Orthotics Clinics (ACPOC) Annual Meeting, Banff, Alberta, Canada, March 2004
- 10.Katz DE, Browne RH (2005) The influence of how much a scoliosis orthosis is worn and its ability to prevent curve progression in adolescent idiopathic scoliosis. In: Proceedings of the Association of Children’s Prosthetics–Orthotics Clinics (ACPOC) Annual Meeting, Orlando, Florida, March 2005
- 11.Nicholson GP, Ferguson-Pell MW, Smith K, Edgar M, Morley T. The objective measurement of spinal orthosis use for the treatment of adolescent idiopathic scoliosis. Spine. 2003;28:2243–2251. doi: 10.1097/01.BRS.0000085098.69522.52. [DOI] [PubMed] [Google Scholar]
- 12.Helfenstein A, Lankes M, Ohlert K, Varoga D, Hahne HJ, Ulrich HW, Hassenpflug J. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine. 2006;31:339–344. doi: 10.1097/01.brs.0000197412.70050.0d. [DOI] [PubMed] [Google Scholar]
- 13.Takemitsu M, Bowen JR, Rahman T, Glutting JJ, Scott CB. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine. 2004;29:2070–2074. doi: 10.1097/01.brs.0000138280.43663.7b. [DOI] [PubMed] [Google Scholar]
- 14.Rahman T, Bowen JR, Takemitsu M, Scott C. The association between brace compliance and outcome for patients with idiopathic scoliosis. J Pediatr Orthop. 2005;25:420–422. doi: 10.1097/01.bpo.0000161097.61586.bb. [DOI] [PubMed] [Google Scholar]
- 15.Bassett GS, Bunnell WP, MacEwen GD. Treatment of idiopathic scoliosis with the Wilmington brace. Results in patients with a twenty to thirty-nine-degree curve. J Bone Joint Surg Am. 1986;68:602–605. [PubMed] [Google Scholar]
- 16.Winter RB, Lonstein JE, Drogt J, Noren CA. The effectiveness of bracing in the nonoperative treatment of idiopathic scoliosis. Spine. 1986;11:790–791. doi: 10.1097/00007632-198610000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Emans JB, Kaelin A, Bancel P, Hall JE, Miller ME. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine. 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:815–822. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from The Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:823–827. doi: 10.2106/00004623-199506000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:664–674. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]


