Abstract
Recent research on individuals with autism spectrum disorders (ASD) highlights that they may be at increased risk for health problems when compared to the general population, and that these differences appear to increase with age. Relatively little research has examined the psychosocial impact of poorer health in this population, even though the clinical literature suggests that health problems put individuals with ASD at risk for elevated behavioral problems and their mothers at risk for elevated caregiving burden. This study examined the associations of physical health and behavior problems, as well as the associations of these factors with maternal burden, using longitudinal data. Results indicated that prior ratings of physical health problems predicted subsequent levels of behavior problems. Further, behavior problems partially mediated the effect of health problems on maternal burden. Implications for policies and interventions that focus on health promotion in conjunction with treatment of behavior problems are discussed, along with directions for future research.
Keywords: Autism, caregiver burden, health, behavior problems
Introduction
Many individuals who have autism spectrum disorders (ASD) experience elevated levels of health problems (Filipek, 2005; Volkmar & Wiesner, 2004). Both global physical health problems and specific physical health symptoms, such as gastrointestinal (GI) problems, have received particular attention in recent studies (Erickson et al., 2005; Filipek, 2005). Anecdotal and clinical literature has reported the association between physical health and behavior problems in ASD (e.g., Goldson & Bauman, 2007; Volkmar & Wiesner, 2004). Clinicians recognize that physical health is often compromised in adolescents and adults with ASD (Barnhill, 2007), and speculate that the unique features of autism (i.e., impairments in communication and social interaction) can make it difficult for individuals to cope with their physical health problems and associated pain, often leading to behavior outbursts (Carr & Owen-DeSchryver, 2007; Groden, Cautela, Prince, & Berryman, 1994).
Despite the clinical literature, studies demonstrating the association of the physical health of individuals with ASD with behavioral functioning are rare (Horvath & Perman, 2002). Although it is recognized that health problems can lead to behavior problems (Volkmar & Wiesner, 2004), behavioral management programs for individuals with ASD have rarely considered physical health problems in their treatment protocols. Traditionally, the first line of treatment for behavior problems includes behavior modification strategies that focus on targeting the overt behavior problems displayed by the individual with autism, as well as pharmacological treatments (Dawson, Matson, & Cherry, 1998; Eldevik, Eikeseth, Jahr, & Smith, 2006; Horner, Carr, Strain, Todd, & Reed, 2002; McDougle et al., 2005). However, if physical health is an underlying contributor to behavior problems, it would suggest another important strategy for intervention.
Of additional importance is impact of physical health problems in individuals with autism on the well-being of their caregivers. Mothers, who are often the primary caregivers of individuals with ASD, may worry about a son or daughter's health, and health problems can necessitate additional caregiving responsibilities, such as increased frequency of doctor visits and medication management. Some studies have noted a relationship between health problems in adolescents and adults with ASD and maternal well-being (e.g., Kring, Greenberg, & Seltzer, 2008; Lounds, Seltzer, Greenberg, & Shattuck, 2007), and the relationship between behavior problems and maternal burden has been well established (e.g., Abbeduto et al., 2004; Blacher & McIntyre, 2006; Hastings et al., 2005; Herring et al., 2006; Lecavalier, Leone, & Wiltz, 2006). However, studies have yet to examine how health and behavior problems might operate in conjunction to exacerbate maternal burden.
This study begins to fill these gaps by examining two research questions:
What is the impact of physical health problems on the level of behavior problems in adolescents and adults with ASD?
Is the presence of health problems in adolescents and adults with ASD related to higher levels of maternal burden? Do behavior problems mediate the relationship between physical health in adolescents and adults with ASD and maternal burden?
Prevalence of Physical Health Problems in ASD
Comparative studies have found that children with ASD have poorer health (Gurney, McPheeters, & Davis, 2006) and more compromised immunity, such as more ear infections and higher use of antibiotics (Niehus & Lord, 2006), than typically developing children. Approximately one out of every four individuals with autism experiences seizures, which is remarkably higher than rates in the general population (Filipek, 2005; Danielsson, Gillberg, Billstedt, Gillberg, & Olsson, 2005). While seizures can be evident as early as infancy, they often develop around the onset of puberty (Billstedt, Gillberg, & Gillberg, 2005; Fombonne, 2003). Similarly, studies of gastrointestinal (GI) problems in individuals with ASD, such as diarrhea and constipation, often have their onset during adolescence (Azfal et al., 2003; Horvath, Papadimitriou, Rabsztyn, Drachenberg, & Tildon, 1999; Molloy & Manning-Courtney, 2003; Valicenti-McDermott et al., 2006). Thus, the available research indicates that adolescence is a period of increased risk for developing chronic health problems in individuals with autism.
Behavioral Implications of Physical Health Problems
Horvath and Perman (2002) reported higher rates of sudden aggression in a sample of children with ASD who had GI problems compared to those with ASD and no GI problems. Studies in the general developmental disabilities (DD) literature have demonstrated an association between health problems and behavior problems. Carr and Owen-DeSchryver (2007) found an association between illness and problem behavior, as well as pain and problem behavior, in a small clinical sample of individuals with DD who had low verbal ability. Carr, Smith, Giacin, Whelan, and Pancari (2003) found that a multifaceted intervention providing pain reduction and other health-related supports during menstrual discomfort was effective in reducing behavior problems for three women diagnosed with developmental disabilities. In a single-subject design study on adults with DD, different types of seizures were associated with different patterns of problem behaviors (Roberts, Yoder, & Kennedy, 2005). The clinical literature similarly suggests an association between health and behavior problems (Kennedy & Thompson, 2000), and particularly suggests consideration of health antecedents in behavioral treatment (Kennedy & O'Reilly, 2006)
Impacts of Physical Health and Behavior Problems on Maternal Well-Being
Many studies have demonstrated that mothers of children with ASD experience higher levels of stress and mental health symptoms than mothers of typically developing children and children with other types of disabilities (Abbeduto et al., 2004; Blacher & McIntyre, 2006; Eisenhower, Baker, & Blacher, 2005; Greenberg, Seltzer, Krauss, Chou, & Hong, 2004; Weiss, 2002). Studies consistently find a strong association between behavior problems and compromised maternal well-being (Abbeduto et al., 2004; Allik, Larsson, & Smedje, 2006; Hastings, 2003; Hastings et al., 2005; Herring et al., 2006; Lecavalier et al., 2006). By contributing to an increase in behavior problems, chronic health problems in individuals with autism may indirectly take a long-term toll on the well-being of maternal caregivers.
In addition, there is growing evidence that poorer health in adolescents and young adults with ASD is related to a poorer quality mother–child relationship, higher levels of maternal anxiety, and higher levels of maternal burden (Kring et al., 2008; Lounds et al., 2007; Orsmond, Seltzer, Greenberg, & Krauss, 2006). Thus, health problems in adolescents and adults with autism may have both direct and indirect (via behavior problems) effects on maternal burden.
Research Aims and Hypotheses
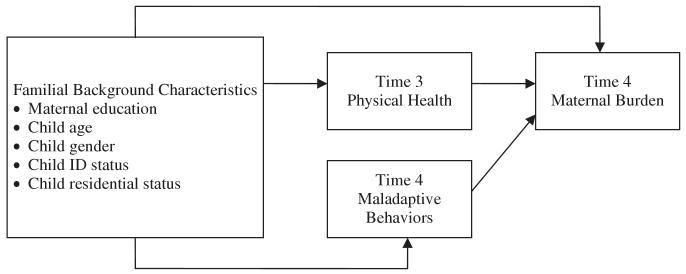
The first research question focused on the relationship between physical health and behavior problems. Based on the available clinical and research literature, we hypothesized that initial levels of physical health would predict behavior problems 18 months later in individuals with ASD, controlling for initial levels of behavior problems. We analyzed a lagged model because we expected the effects of health problems would unfold over time, leading to increasing behavior problems. For our second research question, we predicted that behavior problems would mediate the relationship between health problems in individuals with ASD and maternal burden. The conceptual model illustrating the hypothesized mediation effect is portrayed in Figure 1.
FIGURE 1.
Conceptual model for mediation.
Methods
Sample and Procedures
The present analysis used a subsample drawn from our larger ongoing longitudinal study of families of adolescents and adults with autism (n = 406; Seltzer et al., 2003). The criteria for inclusion in the larger study were that the son or daughter with ASD was age 10 or older (age range = 10–52 at the beginning of the study), had received an ASD diagnosis (autistic disorder, Asperger disorder, or pervasive developmental disorder-not otherwise specified [PDD-NOS]) from an educational or health professional, and had a research-administered Autism Diagnostic Interview–Revised (ADI–R; Lord, Rutter, & Le Couteur, 1994) profile consistent with the diagnosis. Nearly all (94.6%) of the sample members met the ADI–R lifetime criteria for a diagnosis of autistic disorder. Case-by-case review of the other sample members (5.4%) determined that their ADI–R profile was consistent with their autism spectrum diagnosis (i.e., meeting the cut-offs for reciprocal social interaction and repetitive behaviors for Asperger's disorder, and meeting the cutoff for reciprocal social interaction and the cut-off for either impaired communication or repetitive behaviors for PDD-NOS). Half of the participants lived in Wisconsin (n = 202), and half in Massachusetts (n = 204), and identical recruitment and data collection methods were used at both sites. Families were recruited through service agencies, schools, and clinics. Four rounds of data (Time 1 through Time 4) have been collected thus far (every 18 months, spanning a 4.5 year period) via self-administered questionnaires and in-home interviews with primary caregivers (usually the mother) that typically lasted two to three hours. In addition, a separate component of the study, referred to as the Daily Diary Study, was offered to families whose sons and daughters were still living at home. This substudy, conducted shortly after the completion of the Time 4 interview, gathered data via telephone about daily stressors in the lives of mothers of adolescents and adults with ASD (for further information see Smith et al., in press).
The present analysis examined a subset of families who were still participating fully at the third (Time 3) and fourth (Time 4) time points of the study, and who had complete data on the measures of interest (n = 275). The later waves of the study were analyzed to ensure that all the individuals with autism had entered adolescence, a period when chronic health problems often emerge (Azfal et al., 2003, Horvath et al., 1999). Since the beginning of the study (Time 1), a total of 79 families dropped out; 37 families could not be located; two families no longer participated because the son or daughter with ASD died; and in seven families the mother died. In addition, 6 families remained in the study at Time 4, but were missing data on the dependent variables of interest. For descriptive purposes, we compared the Time 1 characteristics of the current sample of 275 families to the 131 families that were not included in these analyses to determine if any variables were associated with attrition. The two groups were not significantly different on any characteristics of the son or daughter with ASD, including age, gender, rates of intellectual disability (ID), residential status, or initial ADI–R scores (an indicator of severity of their autism). Regarding the characteristics of the mothers, who were the primary respondents, those who remained in the study had higher education levels than mothers who did not participate (57.8% vs. 38.9% with college education, respectively; χ2(df = 3) = 15.776, p < .01), and were more likely to identify as White (95.6% vs. 85.3%; χ2(df = 1) = 11.401, p < .01).
The individuals with ASD in the present analysis ranged in age from 12.7 to 51.8 at Time 3 (M = 24.8, SD = 9.4). Nearly two-thirds (60.7%) lived with their mothers. Approximately three-fourths were male (76%). Just over two-thirds (68.4%) had intellectual disability (i.e., I.Q. scores below 70 and significant limitations in functional abilities). Sample gender characteristics and rates of intellectual disability were similar to those expected based on epidemiological studies of autistic disorder (Bryson & Smith, 1998; Fombonne, 2003). Mothers ranged in age from 35.3 to 84.8 (mean = 53.9, SD = 10.3). Just over half of families in the present analysis (55.3%) lived in Wisconsin, and the rest lived in Massachusetts.
Measures
The key measures for the study focus on the health and behavior problems of the son or daughter with ASD and maternal burden. Overall physical health was measured by a maternal rating of her son or daughter's current health status (1 = poor to 4 = excellent). Such ratings of health have been shown to be valid assessments of morbidity and predictive of mortality across a variety of populations (for a review, see Idler & Benjamini, 1997). Behavior problems were assessed via the Scales of Independent Behavior–Revised (SIB–R; Bruininks, Woodcock, Weatherman, & Hill, 1996). This measure consists of eight behavior problems: behavior that is hurtful to self, unusual or repetitive, withdrawn or inattentive, socially offensive, uncooperative, hurtful to others, disruptive, and destructive of property. The mother rates each of these behaviors on both frequency and severity during the past 6 months. Standard algorithms translate these scores into a general maladaptive index that reflects clinical categories of maladaptive behavior (1 = normal to 5 = very serious). Higher scores are indicative of more problematic behavior. Reliability and validity have been established (Bruininks et al., 1996), and reliability is high in this sample (α = .84 at Time 3 and α = .86 at Time 4).
Mothers completed the 29-item Burden Interview (Zarit, Reever, & Bach-Peterson, 1980), a questionnaire that assesses subjective burden related to caregiving demands. The items ask mothers to rate their level of agreement with statements, such as, “Because of my involvement with my son/daughter, I don't have enough time for myself” (0 = not at all, 1 = somewhat, 2 = extremely). Scores can range from 0 to 58, with higher scores reflecting greater burden (Cronbach's alpha = .88).
Several background characteristics were used as control variables in the regression models. Maternal education is categorized as: “1” high school graduate or less, “2” some college, “3” bachelor's degree, “4” graduate degree. Race/ethnicity is coded “0” for White and “1” if she indicated belonging to another racial or ethnic group. Age is a continuous variable. Because a mother's age highly correlates with her son or daughter's age (r = 0.863, p < .001), only the age of the son or daughter is included. Gender of the son or daughter is coded “0” for male and “1” for female. Residential status is coded “0” if the son or daughter lives at home with the mother and “1” if the individual with ASD lives elsewhere. Intellectual disability (ID) status is a dichotomous variable that indicates whether the individual has a valid diagnosis of intellectual disability (coded “1”) or not (coded “0”). ID status was determined using a variety of sources. Standardized IQ was obtained by administering the Wide Range Intelligence Test (WRIT; Glutting, Adams, & Sheslow, 2000) and adaptive behavior was assessed by the Vineland Screener (Sparrow, Carter, & Cicchetti, 1993). Individuals with standard scores of 70 or below on both measures were classified as having ID, consistent with diagnostic guidelines (Luckasson et al., 2002). For cases where the individual with ASD scored above 70 on either measure, or for whom either of the measures was missing, a review of records by three psychologists, combined with a clinical consensus procedure, was used to determine ID status.
Data Analysis
Correlations, means, and standard deviations are provided for descriptive purposes (see Table 1). Also, we describe changes in health and behavior problems over time. Differences between the initial and later measures of health and behavior problems were tested using paired t-tests. The amount of change over time in behavior problems and self-rated health are presented as well. Standardized mean differences (D scores) between the initial and later measurements were calculated for each variable, following procedures outlined by Kline (2004). The standard deviation of the variable at Time 3 was used in creating D scores. The D scores were classified into three categories. D scores within one-half of a standard deviation above or below the initial score mean (i.e., between −.5 and .5) were classified as no change. D scores that were more than one-half of a standard deviation above or below the initial score were considered to have increased or decreased. The one-half standard deviation interval is a well-established guideline for what constitutes a medium effect size, and is sometimes also referred to as a clinically noticeable difference in clinical research (Cohen, 1988; Kline, 2004).
TABLE 1.
Correlation matrix with descriptive statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Time 3 physical health | 1 | ||||||||||
| 2. Time 3 behavior problems | −0.147 | 1 | |||||||||
| 3. Time 4 physical health | 0.606 | −0.121 | 1 | ||||||||
| 4. Time 4 behavior problems | −0.211 | 0.665 | −0.165 | 1 | |||||||
| 5. Time 4 maternal burden | −0.252 | 0.460 | −0.279 | 0.489 | 1 | ||||||
| 6. Child age | −0.158 | −0.222 | −0.059 | −0.218 | −0.198 | 1 | |||||
| 7. Gender | −0.014 | 0.018 | −0.104 | 0.008 | −0.042 | 0.107 | 1 | ||||
| 8. ID status | 0.018 | 0.139 | −0.039 | 0.202 | 0.033 | 0.200 | 0.040 | 1 | |||
| 9. Child residential status | −0.117 | −0.051 | −0.035 | −0.009 | −0.173 | 0.402 | 0.013 | 0.236 | 1 | ||
| 10. Race/ethnicity | 0.095 | 0.014 | 0.071 | 0.013 | −0.069 | 0.023 | 0.038 | 0.008 | 0.152 | 1 | |
| 11. Mother education | 0.059 | 0.098 | 0.102 | 0.187 | 0.176 | −0.188 | 0.070 | −0.084 | 0.054 | −0.083 | 1 |
| Mean | 2.23 | 1.82 | 2.13 | 1.64 | 33.80 | 24.79 | 0.24 | 0.68 | 0.39 | 0.96 | 2.70 |
| SD | 0.69 | 1.03 | 0.66 | 0.97 | 9.34 | 9.39 | 0.43 | 0.47 | 0.49 | 0.20 | 1.20 |
Correlations with absolute values greater than 0.120 are significant at the p < .05 level. Correlations with absolute values greater than 0.155 are significant at the p < .01 level.
Hierarchical regression analysis was used to examine our research questions. Control variables included age, gender, ID status, and residential status of the son or daughter with ASD, as well as maternal education. In preliminary analyses, we also included race as a control, but this was never significant, so it was dropped from the final models. For our first research question, in examining the effects of health at Time 3 on behavior problems at Time 4, the measure of behavior problems at Time 3 was included in the model to control for prior levels of behavior problems. To investigate our second research question, which hypothesized that behavior problems mediated the effect of health problems on caregiver burden (see Figure 1), we used procedures outlined by Baron and Kenny (1986). The criteria for mediation are: (1) that the independent variable (Time 3 physical health) is significantly related to the dependent variable (Time 4 maternal burden); (2) that the independent variable is related to the mediator (Time 4 behavior problems); and (3) the association between the independent and dependent variables is reduced or eliminated after the mediator is entered into the analysis.
In addition to the quantitative analyses, we compiled qualitative data from the Daily Diary Study. We provide brief excerpts from these interviews to illustrate the relationships between the health and behavior problems of the adolescent or adult with autism and maternal burden. To protect confidentiality, identifying information has been altered.
Results
Change in Health and Behavior Problems
As shown in Table 2a, paired t-tests indicate that behavior problems and health declined significantly between Time 3 and Time 4. Behavior problems became less severe, while health problems became more severe over the 18-month study period.
TABLE 2.
Sample change in health and behavior between time 3 and time 4
| 2a. Mean level change | ||||||
|---|---|---|---|---|---|---|
| Time 3 | Time 4 | |||||
| M | SD | M | SD | t-value | D | |
| Physical healtha | 2.23 | 0.69 | 2.13 | 0.66 | −2.51* | −.13 |
| Behavior problemsb | 1.82 | 1.03 | 1.64 | 0.97 | −3.54*** | −.17 |
| 2b. Percentage of the sample who decreased, had no change, or increased | ||||||
| Decreased | No change | Increased | ||||
| n | % | n | % | n | % | |
| Physical health | 57 | 20.7% | 186 | 67.6% | 32 | 11.6% |
| Behavior problems | 72 | 26.2% | 163 | 59.3% | 40 | 14.5% |
p < .05,
p < .001.
For physical health, decreasing scores from Time 3 to Time 4 indicates that the individuals' health was rated as poorer.
For behavior problems, decreasing scores from Time 3 to Time 4 indicates that the individuals' behavior was rated as better, or more normal.
Although there was significant mean-level change, the majority of sample members showed profiles of stability in health and behavior problems. As shown in Table 2b, a majority (67.6%) had no change in their health scores from Time 3 to Time 4. However, of those who changed, more (20.7%) experienced poorer health as compared to the proportion that had improved health (11.6%) between the two time points. Behavior problems showed a similar pattern of stability, where a majority (59.3%) had no change in their behavior scores from Time 3 to Time 4. However, fewer members of the sample (14.5%) experienced an increase in behavior problems as compared to the proportion whose behavior improved (26.2%) between the two time points.
Predicting Change in Behavior Problems
For our first research question, we examined the effects of health problems at Time 3 on behavior problems at Time 4 of individuals with autism. Table 3 presents the results of the ordinary least squares hierarchical regression analysis (OLS). In the first step, control variables were entered as well as the Time 3 level of behavior problems. In the second step, the independent variable, Time 3 health, was entered to determine its effect on Time 4 behavior problems, net of the control variables and prior levels of behavior problems.
TABLE 3.
Regression models for health and behavior problems
| Dependent variable: Time 4 behavior problems | ||||
|---|---|---|---|---|
| Step 1 | Step 2 | |||
| β | t-value | β | t-value | |
| Time 3 Behavior problems | .613 | 13.279*** | .580 | 12.542*** |
| Child age | −.095 | −1.850 | −.123 | −2.416* |
| Gender | −.008 | −.171 | −.007 | −.165 |
| ID status | .142 | 3.036** | .159 | 3.446** |
| Child residential status | .021 | .417 | .008 | .158 |
| Maternal education | .121 | 2.633** | .130 | 2.885** |
| Time 3 Physical health | −.155 | −3.450** | ||
| R2 | .480 | F = 41.16*** | .502 | F = 38.41*** |
p < .05,
p < .01,
p < .001.
As expected, higher levels of behavior problems at Time 3 were significantly predictive of later behavior problems, suggesting stability of behavior problems. In addition, individuals with ASD tended to have higher levels of behavior problems at Time 4 if they were younger or had a co-morbid diagnosis of ID. Further, higher levels of maternal education were a significant predictor of higher levels of behavior problems in sons and daughters.
The independent variable of interest, Time 3 health, was entered in the second step. As hypothesized, Time 3 physical health significantly predicted later levels of behavior problems, net of the control variables and the prior level of behavior problems. Those who rated their health as worse at Time 3 showed a pattern of increasing behavior problems over time. The addition of this variable accounted for a 2.3% of the total variance.
The following quotation from a mother in the Daily Diary Study speaks to how the child's health problems affected her daughter's behavior:
Kelly had another episode with her gastric reflux today. When she has a full blown episode like this she gets self injurious. She'll hit herself or try to hurt herself by hitting other things. I had to restrain her until her medication started working.
Mediation of the Relationship between Health and Maternal Burden
Our second research question examined whether behavior problems mediated the relationship between health problems and maternal burden. Regarding the predictors of maternal burden, as shown in Table 4, Step 1, better child health at Time 3 was related to lower levels of maternal burden at Time 4, net of control variables, satisfying Baron and Kenny's (1986) first criterion for mediation. As shown in Table 1, the measure of child behavior problems was significantly related to maternal burden (r = .489, p < .001), satisfying the second criterion for mediation. The third criterion for mediation is that the mediator (behavior problems) would eliminate or attenuate the relationship between physical health of the son or daughter with ASD and maternal burden. When the behavior problems variable was entered in the second step, higher levels of behavior problems were associated with higher levels of maternal burden. The effect of physical health on maternal burden was reduced, but still significant. A Sobel test was performed to test the mediation for significance, which determined there was a significant mediation effect (t = −4.06, p < .001). Thus, behavior problems partially mediated the relationship between physical health and maternal burden.
TABLE 4.
Mediation model for health and behavior problems on maternal burden
| Dependent variable: Time 4 maternal burden | ||||
|---|---|---|---|---|
| Step 1 | Step 2 | |||
| β | t-value | β | t-value | |
| Child age | −.159 | −2.515* | −.042 | −.697 |
| Gender | −.045 | −.806 | −.050 | −.970 |
| ID status | .133 | 2.304* | .018 | .333 |
| Mother education | .189 | 3.303** | .119 | 2.222* |
| Child residential status | −.186 | −2.988** | −.185 | −3.249** |
| Time 3 physical health | −.313 | −5.573*** | −.202 | −3.754*** |
| Time 4 behavior problems | .410 | 7.207*** | ||
| R2 | .182 | F = 9.96*** | .315 | F = 17.58*** |
p < .05,
p < .01,
p < .001.
With respect to the control variables, as shown in Table 4, Step 2, mothers with higher levels of education reported more burden. Also, mothers felt less burdened when their child lived outside the parental home.
In the Daily Diary Study, several mothers spoke about how the physical health of their sons and daughters directly affected their own well-being. As an example, the excerpt that follows shows how the health concerns of her son created an added burden to an already over-extended mother:
At lunchtime we found out Jacob had really high blood sugar, over 400. Whenever you see your child's blood sugar skyrocket, you worry. We figured out that he must have forgotten to take his 24 hour shot for the day. We took care of it. But, it's stressful, because if I hadn't been there and he hadn't taken care of it, well, he'd go into a coma eventually.
The aforementioned quote suggests how their child's health problems were a direct source of stress for these mothers. Another mother spoke of the rippling effects of her child's health problems, leading to behavior problems and eventually increasing her level of stress.
Sue has these stomach problems on most days. I have to drop everything immediately. Many nights I don't get the sleep I need. I feel useless because I can't make her feel better. We've been dealing with this for 5 years and we can't seem to find any treatment to manage it. It limits what activities she can do and what we can do as a family. We can't really go out and do anything until this gets resolved, but I feel depressed and hopeless that it's not going to get better.
Discussion
This study's longitudinal design made it possible to examine the effects of prior health problems on subsequent behavior problems in adolescents and adults with ASD and the data suggested that prior levels of health problems are associated with increasing levels of behavior problems over an 18-month period. While one study of individuals with ASD has examined cross-sectionally the relationship between health symptom and behavior problems (Horvath & Perman, 2002), this is the first longitudinal study utilizing a large community-based sample to establish that behavior problems in adolescents and adults with autism are in part due to their health problems. These findings suggest that, for some individuals, interventions focused on ameliorating behavior problems might be more effective if they also target health problems. Future studies are needed to examine the effects of remediation of physical health problems for individuals with ASD, and examine whether these treatments have an impact on the behavior problems and the psychological well-being of their caregivers.
Although adolescents and adults with ASD have elevated levels of health problems, it is important to note that a majority of individuals in this study were rated by their mothers as having “good” or “excellent” health. Further, behavior appears to be improving in these individuals over time, which is consistent with findings based on our larger study over a 4.5 year period (Shattuck et al., 2007). Health, on the other hand, appears to be declining, even over this 1.5 year period, which alone suggests a need for service providers and policymakers to attend to the health needs of adolescents and adults with ASD.
Both health and behavior problems were independently associated with higher levels of maternal burden, which is consistent with previous research literature (e.g., Abbeduto et al., 2004; Hastings et al., 2005; Kring et al., 2008; Lecavalier et al., 2006; Lounds et al., 2008). The results from this study indicate that health problems may also increase maternal burden by exacerbating behavior problems. This finding suggests yet another potential implication of improving physical health of adolescents and adults with ASD, by reducing both the direct and indirect strains placed on their mothers. Future intervention studies could examine whether addressing the health problems of sons and daughters with ASD is effective in reducing caregiving burden.
The findings of this study have several important implications for social work practice. First, on the policy front, social workers should advocate for better training for health care practitioners, adequate health screening, and health care services for adolescents and adults with ASD. In addition, social workers who work with adolescents or adults with ASD displaying behavior problems should attend to the health needs of their clients and may consider whether a health assessment is in order. Finally, social work practitioners may have an integral role helping to remediate the burdens of family caregivers by helping them find and coordinate health care services and behavior management services. Family psychoeducation programs, which have proven highly effective in helping family caregivers of adults with mental illness (Leff, 2005) and families caring for a frail elders (Hepburn et al., 2005), could be adapted to help families of individuals with autism learn new strategies to cope with difficult behaviors as well as learn about community resources that might help them better coordinate services for their child's health needs. Such psychoeduction programs, which can be both a source of information and support, are particularly important for families who have an adult child with an autism diagnosis because there currently are no interventions that are available to support such families after their child reaches adulthood.
There are some important limitations of this study that should be noted. While the longitudinal nature of the study provides insights about change over time, these results should be interpreted with caution, as they are based on correlational data, so causal relationships cannot be confirmed. Additionally, all variables are based on subjective reports by mothers. Studies that include more objective indicators of health (i.e., medical exams) and behavior problems (i.e., independent raters) could overcome this limitation, although the measures of health and behavior problems have been shown to be valid indicators. Finally, there is limited diversity in the sample, which limits the generalizability of the study findings.
Despite these limitations, the insights provided by this study provide new information about the directional relationship between health and behavior problems in adolescents and adults with ASD, a population of individuals particularly vulnerable to both problems. It further illustrates how these processes operate together to contribute to maternal burden. Improved understanding of the impacts of physical health on behavior problems in adolescents and adults with ASD can increase our ability to tailor future interventions and policies for both individuals and families.
Acknowledgments
This article was prepared with support from the National Institute on Aging (R01 AG08768; Seltzer, PI) the National Institute of Mental Health (T32 MH065185; Greenberg, PI), the National Institute of Child Health and Human Development (P30 HD03352 to the Waisman Center at the University of Wisconsin–Madison), and the National Institute for Disability and Rehabilitation Research (H133B031134) through the Rehabilitation Research and Training Center on Aging and Developmental Disabilities at the University of Illinois at Chicago.
References
- Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Osmond G, Murphy MM. Psychological well-being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. American Journal on Mental Retardation. 2004;109:237–254. doi: 10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Allik H, Larsson JO, Smedje H. Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health and Quality of Life Outcomes. 2006;4:1–8. doi: 10.1186/1477-7525-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azfal N, Murch S, Thirrupathy K, Berger L, Fagbemi A, Hueschkel R. Constipation with acquired megarectum in children with autism. Pediatrics. 2003;112(4):939–942. doi: 10.1542/peds.112.4.939. [DOI] [PubMed] [Google Scholar]
- Barnhill GP. Outcomes in adults with Asperger syndrome. Focus on Autism and Other Developmental Disabilities. 2007;22:116–126. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blacher J, McIntyre LL. Syndrome specificity and behavior disorders in young adults with intellectual disability: Cultural differences in family impact. Journal of Intellectual Disability Research. 2006;50:184–198. doi: 10.1111/j.1365-2788.2005.00768.x. [DOI] [PubMed] [Google Scholar]
- Billstedt E, Gillberg C, Gillberg C. Autism after adolescence: Population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders. 2005;35:351–360. doi: 10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- Bruininks RH, Woodcock RW, Weatherman RF, Hill BK. Scales of Independent Behavior–Revised. Rolling Meadows, IL: Riverside Publishing; 1996. [Google Scholar]
- Bryson SE, Smith IM. Epidemiology of autism: Prevalence, associated characteristics, and implications for research and service delivery. Mental Retardation and Developmental Disabilities Research Reviews. 1998;4:97–103. [Google Scholar]
- Carr EG, Owen-DeSchryver JS. Physical illness, pain, and problem behavior in minimally verbal people with developmental disabilities. Journal of Autism and Developmental Disorders. 2007;37:413–424. doi: 10.1007/s10803-006-0176-0. [DOI] [PubMed] [Google Scholar]
- Carr EG, Smith CE, Giacin TA, Whelan BM, Pancari J. Menstrual discomfort as a biological setting event for severe problem behavior: Assessment and intervention. American Journal on Mental Retardation. 2003;108:117–133. doi: 10.1352/0895-8017(2003)108<0117:MDAABS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. New York: Academic Press; 1988. [Google Scholar]
- Danielsson S, Gillberg IC, Billstedt E, Gillberg C, Olsson I. Epilepsy in young adults with autism: A prospective population-based follow-up study of 120 individuals diagnosed in childhood. Epilepsia. 2005;46(6):918–923. doi: 10.1111/j.1528-1167.2005.57504.x. [DOI] [PubMed] [Google Scholar]
- Dawson JE, Matson JL, Cherry KE. An analysis of maladaptive behaviors in persons with autism, PDD-NOS and mental retardation. Research in Developmental Disabilities. 1998;19(5):439–448. doi: 10.1016/s0891-4222(98)00016-x. [DOI] [PubMed] [Google Scholar]
- Eldevik S, Eikeseth S, Jahr E, Smith T. Effects of low-intensity behavioral treatment for children with autism and mental retardation. Journal of Autism and Developmental Disorders. 2006;36(2):211–224. doi: 10.1007/s10803-005-0058-x. [DOI] [PubMed] [Google Scholar]
- Eisenhower AS, Baker BL, Blacher J. Preschool children with intellectual disability: Syndrome specificity, behavior problems, and maternal well-being. Journal of Intellectual Disability Research. 2005;49:657–671. doi: 10.1111/j.1365-2788.2005.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson CA, Stigler KA, Corkins MR, Posey DJ, Fitzgerald JF, McDougle CJ. Gastrointestinal factors in autistic disorder: A critical review. Journal of Autism and Developmental Disorders. 2005;35(6):713–727. doi: 10.1007/s10803-005-0019-4. [DOI] [PubMed] [Google Scholar]
- Filipek PA. Medical aspects of autism. In: Volkmar FR, Rhea P, Klin A, Cohen D, editors. Handbook of autism and pervasive developmental disorders. Hoboken, NJ: John Wiley & Sons, Inc; 2005. pp. 534–578. [Google Scholar]
- Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders. 2003;33:365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- Glutting J, Adams W, Sheslow D. Wide Range Intelligence Test. Wilmington, DE: Wide Range, Inc; 2000. [Google Scholar]
- Goldson E, Bauman M. Medical health assessment and treatment issues in autism. In: Gabriels RL, Hill DE, editors. Growing up with autism: Working with school aged children. New York: Guilford Press; 2007. pp. 39–57. [Google Scholar]
- Greenberg JS, Seltzer MM, Krauss MW, Chou RJ, Hong J. The effect of quality of the relationship between mothers and adult children with schizophrenia, autism, or Down syndrome on maternal well-being: The mediating role of optimism. American Journal of Orthopsychiatry. 2004;74:14–25. doi: 10.1037/0002-9432.74.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groden J, Cautela J, Prince S, Berryman J. The impact of stress and anxiety on individuals with autism and developmental disabilities. In: Schopler E, Mesibov GB, editors. Behavioral issues in autism. New York: Plenum Press; 1994. pp. 177–195. [Google Scholar]
- Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Archives of Pediatrics & Adolescent Medicine. 2006;160(8):825–830. doi: 10.1001/archpedi.160.8.825. [DOI] [PubMed] [Google Scholar]
- Hastings RP. Child behaviour problems and partner mental health as correlates of stress in mothers and fathers of children with autism. Journal of Intellectual Disability Research. 2003;47:231–237. doi: 10.1046/j.1365-2788.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Kovshoff H, Ward NJ, degli Espinosa F, Brown T, Remington B. Systems analysis of stress and positive perceptions in mothers and fathers of pre-school children with autism. Journal of Autism and Developmental Disorders. 2005;35:635–644. doi: 10.1007/s10803-005-0007-8. [DOI] [PubMed] [Google Scholar]
- Hepburn KW, Lewis M, Narayan S, Tornatore J, Brmer KL, Kirk LN. Partners in caregiving: A psychoeducation program affecting dementia family caregivers' distress and caregiving outlook. Clinical Gerontologist. 2005;29:53–69. [Google Scholar]
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, Einfeld S. Behavior and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. Journal of Intellectual Disability Research. 2006;50:874–882. doi: 10.1111/j.1365-2788.2006.00904.x. [DOI] [PubMed] [Google Scholar]
- Horner RH, Carr EG, Strain PS, Todd AW, Reed HK. Problem behavior interventions for young children with autism: A research synthesis. Journal of Autism and Developmental Disorders. 2002;32:423–446. doi: 10.1023/a:1020593922901. [DOI] [PubMed] [Google Scholar]
- Horvath K, Papadimitriou JC, Rabsztyn A, Drachenberg C, Tildon JT. Gastrointestinal abnormalities in children with autistic disorder. Journal of Pediatrics. 1999;135(5):559–563. doi: 10.1016/s0022-3476(99)70052-1. [DOI] [PubMed] [Google Scholar]
- Horvath K, Perman JA. Autistic disorder and gastrointestinal disease. Current Opinion in Pediatrics. 2002;14(5):583–587. doi: 10.1097/00008480-200210000-00004. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benjamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Kennedy CH, Thompson T. Health conditions contributing to problem behavior among people with mental retardation and developmental disabilities. In: Wehmeyer M, Patten J, editors. Mental retardation in the 21st century. Austin, TX: ProEd; 2000. pp. 211–231. [Google Scholar]
- Kennedy CH, O'Reilly ME. Pain, health conditions, and problem behavior in people with developmental disabilities. In: Oberlander TF, Symons FJ, editors. Pain in children and adults with developmental disabilities. Baltimore: Paul H. Brookes; 2006. pp. 121–138. [Google Scholar]
- Kline RB. Beyond significance testing: Reforming data analysis methods in behavioral research. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Kring SR, Greenberg JS, Seltzer MM. Adolescents and adults with autism with and without co-morbid psychiatric disorders: Differences in maternal well-being. Journal of Mental Health Research in Intellectual Disabilities. 2008;1:53–74. doi: 10.1080/19315860801988228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research. 2006;50:172–183. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- Leff J. Advanced family work for schizophrenia: An evidenced-based approach. London: Gaskell Publications; 2005. [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview–Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lounds JJ, Seltzer MM, Greenberg JS, Shattuck P. Transition and change in adolescents and young adults with autism: Longitudinal effects on maternal well-being. American Journal on Mental Retardation. 2007;112:401–417. doi: 10.1352/0895-8017(2007)112[401:TACIAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Luckasson R, Borthwick-Duffy S, Buntinx WHE, Coulter DL, Craig EM, Reeve A, Schalock RL, Snell M, Spitalnik DM, Spreat S, Tasse MJ. Mental retardation: Definition, classification, and systems of support. 10th. Washington, DC: American Association on Mental Retardation; 2002. [Google Scholar]
- McDougle CJ, Scahill L, Aman MG, McCracken JT, Tierney E, Davies M, Arnold LE, Posey DJ, Martin A, Ghuman JK, Shah B, Chuang SZ, Swiezy NB, Gonzalez NM, Hollway J, Koenig K, McGough JJ, Ritz L, Vitiello B. Risperidone for the core symptom domains of autism: Results from the study by the Autism Network of the Research Units on Pediatric Psychopharmacology. American Journal of Psychiatry. 2005;162:1142–1148. doi: 10.1176/appi.ajp.162.6.1142. [DOI] [PubMed] [Google Scholar]
- Molloy CA, Manning-Courtney P. Prevalence of chronic gastrointestinal symptoms in children with autism and autistic spectrum disorders. Autism. 2003;7(2):165–171. doi: 10.1177/1362361303007002004. [DOI] [PubMed] [Google Scholar]
- Niehus R, Lord C. Early medical history of children with autism spectrum disorders. Developmental and Behavioral Pediatrics. 2006;27(2):120–127. doi: 10.1097/00004703-200604002-00010. [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Seltzer MM, Greenberg JS, Krauss MW. Mother-child relationship quality among adolescents and adults with autism. American Journal on Mental Retardation. 2006;111:121–137. doi: 10.1352/0895-8017(2006)111[121:MRQAAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Roberts C, Yoder PJ, Kennedy CH. Descriptive analysis of epileptic events and the occurrence of self-injury and aggression. American Journal on Mental Retardation. 2005;110:405–412. doi: 10.1352/0895-8017(2005)110[405:DAOESA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33:565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, Orsmond GI, Kring S, Bolt D, Lounds J, Lord C. Changes in autism symptoms and maladaptive behaviors among adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:1735–1747. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L, Seltzer MM, Almeida D, Greenberg JS, Hong J, Bishop S. Daily experiences of mothers of adolescents and adults with ASD. Journal of Autism and Developmental Disabilities. doi: 10.1007/s10803-009-0844-y. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Carter AS, Cicchetti DV. Vineland Screener: Overview, reliability, validity, administration, and scoring. New Haven, CT: Yale University Child Study Center; 1993. [Google Scholar]
- Valicenti-McDermott M, McVicar K, Rapin I, Wershil BK, Cohen H, Shinnar S. Frequency of gastrointestinal symptoms in children with autistic spectrum disorders and association with family history of autoimmune disease. Journal of Developmental & Behavioral Pediatrics. 2006;27(Suppl. 2):S128–S137. doi: 10.1097/00004703-200604002-00011. [DOI] [PubMed] [Google Scholar]
- Volkmar FR, Wiesner LA. Healthcare for children on the autism spectrum: A guide to medical, nutritional, and behavioral issues. Bethesda, MD: Woodbine House Inc; 2004. [Google Scholar]
- Weiss MJ. Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism. 2002;6:115–130. doi: 10.1177/1362361302006001009. [DOI] [PubMed] [Google Scholar]
- Zarit S, Reever K, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]