Abstract
Background
Although objective and subjective indicators of socioeconomic status (SES) are linked to cardiovascular disease (CVD), little is known about their relationship to endothelial dysfunction, which often precedes CVD.
Purpose
This study examined how objective and subjective SES relate to brachial artery flow-mediated dilation (FMD).
Methods
FMD was assessed in 72 healthy adults (mean age 36 years). The MacArthur Scale of Subjective Social Status assessed perceived social standing in the USA (SSS-USA) and local community (SSS-Community). Objective SES measures included income and the Hollingshead Two-Factor Index of Social Position (education, occupation).
Results
Adjusted regressions revealed that SSS-Community positively correlated with FMD (p < 0.05) and explained 8% of the variance. No other SES measures were significant for FMD. The association between FMD and SSS-Community remained significant (p < 0.01) after adjustment for objective SES and other covariates.
Conclusions
Lower subjective social status in one’s community may be linked to CVD via impaired vasodilation.
Keywords: Endothelial function, Socioeconomic status, Subjective social status, Vasodilation
Introduction
Researchers in several countries note that socioeconomic status (SES) shows graded inverse associations with cardiovascular morbidity and mortality, independent of traditional risk factors [1]. Recent declines in cardiovascular disease (CVD) have been less prominent in people of lower social classes [2]. Although reduced access to health care likely plays a role in many countries, such as the USA, the SES–CVD gradient also is found in countries with universal health care [3]. Social class differences in the prevalence of adverse health behaviors, such as smoking and physical inactivity, also contribute to the inverse relationship between SES and CVD [4]. However, studies show that the SES–CVD gradient is still found after adjusting for differences in health behaviors and traditional risk factors [1, 2].
Although SES has been linked to a variety of CVD measures [5–7], little is known about the relationship between SES and endothelial dysfunction. Endothelial dysfunction refers to shifts in endothelial processes that lead to decreased vasodilation. With normal function of the endothelium, vascular homeostasis is maintained, and vasoconstriction is limited by secretion of a variety of substances (e.g., nitric oxide), which cause vascular smooth muscle relaxation and artery dilation [8]. Endothelial dysfunction is observed in the early stages of atherosclerosis and is associated with increased plaque rupture in myocardial infarction and other adverse outcomes [8, 9]. Endothelial function can be evaluated with the emerging technique of flow-mediated dilation (FMD), which noninvasively measures endothelium-dependent vasodilation elicited by reactive hyperemia [10]. In response to increased shear stress induced by reactive hyperemia, the endothelium is stimulated to produce and release nitric oxide, which relaxes vascular smooth muscle and produces a measurable increase in artery diameter. FMD refers to the percentage of post-stimulation change in brachial artery diameter relative to baseline [11]. It is highly correlated with invasive endothelial testing and is inversely associated with cardiovascular risk [12–15]. Several prospective studies support a prognostic value for FMD in predicting adverse cardiovascular outcomes among community samples and patient populations [16–21].
Parallel to research on behavioral and psychosocial risk factors for CVD [2], several studies suggest that unhealthy behaviors (e.g., physical inactivity) [22] and a variety of psychosocial characteristics (e.g., depressed mood, stress) [23–26] are linked to endothelial impairment. Despite the substantial literature linking CVD to SES, endothelial function has not been well studied with regard to SES among adults. However, some null findings have been reported for FMD in studies of childhood SES, as measured by the occupational status of the children’s parents [27–29]. Those nonsignificant findings for childhood SES could have been due in part to the young ages of the subjects and to the potential limitations of objectively measured SES (e.g., parental occupation). Although occupational status and other objective measures of SES (e.g., education, income) have been linked to CVD [1–4], these narrowly defined measures cannot capture all the dimensions of social status that have potential relevance to health [30].
Perceptions about one’s standing in society or on the “social ladder” relative to other people may reflect a “cognitive averaging” of several standard markers of social class (e.g., income, education, occupation, spouse’s occupation, home ownership), along with more nuanced aspects of social status, such as one’s feelings about current position and future prospects [31]. Context can alter views of social standing, such that individuals’ subjective views of status may be different when they are comparing themselves socially to others in their local community or to the nation as a whole. The MacArthur Scale of Subjective Social Status (SSS) assesses where individuals perceive themselves to be on the “social ladder” in the nation’s society overall (SSS-USA) and in their local community (SSS-Community) [32].
To date, most investigations examining the relationship of subjective SES to physical and/or mental health measures have focused solely on the SSS-USA scale (or a modified scale used for other countries), which asks individuals to indicate their perceived status relative to people in their nation’s society with the “most money, most education, and best jobs” [33–37]. Lower scores on the SSS-USA (and versions modified for other countries) have been linked to hypertension, diabetes, and other factors associated with increased risk for CVD, even after adjusting analyses for objective measures of SES [5, 31, 37–40]. Although SSS-Community has been studied in relation to self-reported health among older adults in Taiwan [41] and with respect to cortisol responses among college undergraduates in a dormitory “community” [7], its use in cardiovascular research has been limited. No studies were found that examined FMD for relationships to SSS-Community or to SSS-USA. However, Ghaed and Gallo [42] found that lower SSS-Community scores were related to higher ambulatory diastolic blood pressure (BP) in middle-aged women, after adjustments for objective SES (e.g., education, occupation, income), body mass index (BMI), and other cardiovascular risk factors (e.g., exercise). Thus, research to date suggests that both SSS-USA and SSS-Community may exhibit significant associations with cardiovascular health, beyond what is accounted for by objective indicators of SES.
Given the scarcity of previous research examining how endothelial function relates to SES in adults, the current study is not designed to test a priori hypotheses. Rather, it aims to begin filling this literature gap by investigating FMD for associations with social status and assessing whether objective or subjective measures of SES are most strongly correlated with FMD among adults. In keeping with prior research, the study also will examine whether any associations found between subjective SES and FMD remain significant after adjustments for objective SES [5, 31, 37–40] and a variety of factors associated with cardiovascular risk [2, 23–26, 32, 43]. The current work will differ from prior studies of subjective SES and health outcomes by including an adjustment for differences in social desirability, which could contribute to biased responses on self-report measures, such as the MacArthur Scale of SSS [44, 45].
Methods
Participants
The sample included 72 employed (30+ h/week; paid/unpaid) young to middle-aged adults (50% women/50% men; 43% black/57% white) of upper, middle, and lower SES, who were recruited via community advertisements or referrals between 2005 and 2008 to participate in a larger cardiovascular study (“Stress, Blood Pressure and Ethnicity”) [46]. The study’s physician found all participants to be medication-free with no major medical or psychiatric conditions based on physical examinations and evaluation of medical histories. However, ten participants were found at screening to exhibit hypertensive levels of BP (seven were mildly hypertensive and three were moderately hypertensive). Antihypertensive medication had been used by only two of these volunteers, who were then placed on a 3-week closely monitored drug-tapering program prior to being accepted into the study. Approximately 18% of subjects were current smokers. The study excluded persons with diagnoses of secondary hypertension, diabetes (or a fasting glucose >120 mg/dL), morbid obesity (BMI ≥ 40 kg/m2), known sleep disorders (e.g., narcolepsy), current drug or alcohol abuse, creatinine levels >1.4 mg/dl, proteinuria or hematuria by dipstick analysis, or renal bruit upon examination. Women were ineligible if they were pregnant, postmenopausal, taking oral contraceptives, or diagnosed with premenopausal syndrome. Informed consent was obtained from all participants in accordance with the Institutional Review Board of the University of California San Diego.
Procedures
After eligibility was confirmed (through physical examination and medical history), demographic and psychosocial data were collected, along with measures of resting mean arterial pressure (MAP) and BMI. At the General Clinical Research Center of the University of California San Diego, participants in the larger study completed an overnight stay on the unit, followed by a 6 a.m. fasting blood draw and a 9 a.m. test of FMD. During these stays, participants remained on the unit for over 12 h and were restricted from smoking and consumption of caffeine, alcohol, and foods containing high fat or nitrates before the morning assessment of FMD.
Measures
Endothelial Function
The noninvasive determination of endothelial dysfunction by FMD was performed according to the method described by Celermajer and colleagues [47]. Participants relaxed in the supine position for at least 30 min in a quiet room with room temperature maintained at 22–25°C to avoid mental stress, which can affect vasodilator responses [48]. The right brachial artery was visualized in longitudinal section 2 to 8 cm proximal to the antecubital fossa with a high-resolution 5–12-MHz broadband linear array transducer (ATL HDI5000 SonoCT System, Phylips). After optimal transducer positioning and adjusting the ultrasound depth and gain for the best images of the intimal layers, diameter was measured from the anterior to the posterior intima line at end diastole, synchronous with ECG R wave. Baseline brachial artery diameter was determined by averaging three diameter measurements taken immediately before cuff inflation. Then, the cuff was inflated to pressure 50 mmHg greater than the systolic BP. After 5 min, the cuff was deflated, and ultrasound scans were acquired for post-occlusion diameter measurements at 15-s intervals for 1 min and then at 30-s intervals for an additional 9 min. Maximum percentage change in brachial artery diameter (i.e., FMD) was calculated as the percentage difference between baseline diameter and the maximum diameter after cuff deflation.
Socioeconomic Position: Objective Measures
Education and Occupation
The Hollingshead Two-Factor Index of Social Position [49] is one of the most widely used measures of objective SES. It is computed by summing weighted values [1–7] that are applied to occupational and educational levels. Hollingshead social position index scores can range from 11 to 77, with lower scores representing higher SES. Although Hollingshead scores were converted to social class categories for easier reference in Table 1 (i.e., Sample Characteristics), all analyses in the present study utilized continuous index scores.
Table 1.
Sample characteristics (N = 72)
| Variable | Mean (SD) or % | Range |
|---|---|---|
| Age (years) | 36.0 (9.4) | 19.0–53.0 |
| Annual income | $31,872 ($18,471) | $0–100,000 |
| Hollingshead Social Index (education and occupation) | 39.0 (15.6) | 11–65 |
| Hollingshead Social Classes: I/II (upper) | 32% | |
| III (middle) | 35% | |
| IV/V (lower) | 33% | |
| MacArthur SSS-USA | 5.7 (1.8) | 2–9 |
| MacArthur SSS-Community | 6.3 (1.9) | 1–10 |
| Marlowe–Crowne Social Desirability Scale | 19.7 (6.2) | 3.0–32.0 |
| Perceived Stress Scale | 13.1 (6.7) | 0–29 |
| CES–D | 10.6 (7.2) | 0–32 |
| Leisure Time Exercise Questionnaire | 1.8 (0.7) | 1–3 |
| BMI (kg/m2) | 26.3 (3.9) | 19.1–34.6 |
| Total serum cholesterol (mg/dL) | 170.9 (38.6) | 98.0–366.0 |
| Resting MAP (mmHg) | 88.8 (10.8) | 68.7–119.4 |
| FMD (% change from baseline) | 14% (6%) | 2%–31% |
NOTE: Data shown as mean ± SD, unless otherwise noted
FMD: flow-mediated dilation, SSS: subjective social status, MAP: mean arterial pressure, BMI: body mass index, CES-D: Center for Epidemiologic Studies—Depression
Income
Participants provided their annual salary in response to the following question on the Job Content Questionnaire: “What is your total annual wage or salary from this job?” [50].
Socioeconomic Position: Subjective Measures
The MacArthur Scale of SSS asks respondents to indicate where they stand relative to other people on a ten-rung “social ladder” [32, 51]. It has shown adequate construct validity, criterion-related validity, and test–retest reliability in ethnically diverse epidemiological samples obtained from several countries [35–38]. With SSS scores ranging from 1 (bottom) to 10 (top), higher rung selections indicate higher levels of perceived social standing. The scale allows for assessment of perceived social status relative to others at two levels: (1) USA and (2) Community.
SSS-USA: Respondents indicate where they stand on the social ladder based on the following: “Think of this ladder as representing where people stand in the United States. At the top of the ladder are the people who are best off—those who have the most money, the most education, and the best jobs. At the bottom are the people who are worst off—who have the least money, least education, and the worst jobs or no job.”
SSS-Community: As with the SSS-USA, each respondent indicates their social position on a ladder, but this ladder represents their local community. They are instructed to consider “community” as follows: “People define community in different ways; please define it whatever way is most meaningful to you.”
Covariate Measures
The covariates selected for the primary analyses included age, resting MAP, exercise, and social desirability.
Resting MAP:
After 5 min of seated rest, three measures of MAP were obtained with a Dinamap 1846× monitor (Critikon; Tampa, FL) and averaged to compute resting MAP.
Social Desirability:
The Marlowe–Crowne Social Desirability Scale (33 true/false items) assesses socially desirable behaviors that are unlikely to occur in the general population [52]. Higher scores suggest a tendency to underreport information respondents believe may reflect negatively on them and to overreport positively viewed behaviors. We have previously found variations in participants’ willingness to report negative psychosocial information [44]; thus, social desirability scores are examined as a covariate to adjust for this form of response bias.
Exercise:
Participants were asked to complete the Leisure Time Exercise Questionnaire [53] because exercise can have a considerable effect on FMD [43]. This scale provides a “sweat score” that is derived from respondents answering how frequently (“often = 1”, “sometimes = 2”, or “never/rarely = 3”) they engage in physical activity “long enough to work up a sweat” (or make the heart beat more rapidly) during a typical 7-day period. This “sweat score” correlates significantly with cardiovascular fitness as measured by maximal oxygen uptake and treadmill tests [54]. Lower scores indicate a higher frequency of intense physical activity.
Other Measures
The following are other measures that were assessed for exploration in secondary analyses.
BMI:
Each participant’s BMI was derived from weight and height measured to the nearest 0.1 kg and 0.1 cm, respectively.
Cholesterol:
Fasting total serum cholesterol was determined from a blood draw via venous catheter upon awakening the morning after an overnight stay at the General Clinical Research Center.
Center for Epidemiologic Studies—Depression (CES-D):
The CES-D is a well-standardized 20-item self-report measure that assesses the frequency of depressive symptoms experienced in the past week [55].
Perceived Stress Scale:
This scale (ten items) assesses several sources of chronic stress with questions that ask respondents how frequently during the past month they felt that their lives were unpredictable, uncontrollable, or overloaded [56].
Data Analysis
Continuous scores were used to represent all variables (with the exception of categorical variables for sex, race, current smoking status, and hypertension status). Pearson correlational analyses were conducted on FMD, SES measures, and potential confounders to detect associations. Any SES measure showing an association with FMD (p < 0.10) was further examined in an adjusted regression of that particular SES measure on FMD.
Multiple regression models were adjusted for confounders that demonstrated theoretical relationships and/or significant simple correlations with FMD or SES measures. The primary regression model was adjusted for the covariates of age, resting MAP, socially desirable response bias (i.e., Marlowe–Crowne Social Desirability Scale scores), and exercise (i.e., Leisure Time Exercise Questionnaire scores). With consideration of statistical power, these covariates were selected based on the prior literature [43, 44], as well as the range of BP in this normotensive/hypertensive sample (e.g., resting MAP) and significant correlations (e.g., age, exercise, socially desirable response bias) with the primary variables of interest. Categorical variables of sex, race, smoking status, and hypertension status neither showed correlations nor group differences with regard to FMD (or SSS-Community); thus, these variables were not included in regression analyses. However, exploratory analyses were conducted to test the impact of adjustment for potential biological (e.g., BMI, cholesterol) and psychosocial confounders (e.g., depressive symptoms, perceived stress) not included in the original regression model. In addition, the SSS-Community on FMD model was further examined to test significance after adjustment for objective SES measures. All variables were normally distributed, with the exception of Marlowe–Crowne Social Desirability scores, which were square root transformed to reduce skew. Each regression model included covariates on the first step and the SES measure of interest on the last step.
Results
Sample Characteristics
Table 1 summarizes the sample’s characteristics. Participants ranged from 19 to 53 years of age (M = 36.0 years). As indicated by the conversion of Hollingshead social index scores to categories, the sample was comprised of roughly equal proportions of individuals from lower, middle, and upper social classes. The means of subjective SES measures reveal that participants reported higher perceived social status in their communities than in the US overall (M = 6.3 vs M = 5.7, p < 0.01). On average, the sample exhibited a 14% change in FMD.
Pearson Correlations
Table 2 shows how the subjective and objective measures of SES were related to each other and to FMD, as well as covariates. The only significant correlation found between subjective SES measures (i.e., SSS-Community, SSS-USA) and objective SES measures (i.e., annual income, Hollingshead index for education/occupation) was a positive association between SSS-Community and annual income (r = 0.22, p < 0.05). With regard to the relationship between social status and psychosocial distress, higher depressive symptoms correlated with lower perceived status in the community (i.e., SSS-Community) and lower education/occupation (p’s < 0.05). Higher perceived stress was associated with lower rankings on both the SSS-Community and the SSS-USA (p < 0.05 and p < 0.01, respectively). FMD demonstrated a positive correlation with age (p < 0.05). Finally, SSS-Community was the only one of the four SES measures that demonstrated a simple correlation with FMD (r = 0.27, p < 0.05). Thus, SSS-Community was the only SES measure that was further examined to test whether its association with FMD remained significant after adjustments for confounders in regression analyses.
Table 2.
Pearson correlations (r) of flow-mediated dilation and socioeconomic measures with covariates
| Variable | FMD | Income | Education/occupation | SSS-USA | SSS-Community |
|---|---|---|---|---|---|
| 1. FMD | – | – | – | – | – |
| 2. Annual income | −0.04 | – | – | – | – |
| 3. Education/occupation | 0.07 | −0.23* | – | – | – |
| 4. SSS-USA | 0.10 | 0.17 | −0.10 | – | – |
| 5. SSS-Community | 0.27* | 0.22* | −0.18 | 0.51*** | – |
| 6. Social desirability | 0.05 | 0.04 | 0.10 | 0.09 | 0.25* |
| 7. Age | 0.24* | 0.23* | 0.09 | −0.07 | 0.14 |
| 8. Resting MAP | −0.17 | 0.23* | −0.15 | −0.27** | −0.03 |
| 9. Leisure time exercise | 0.05 | −0.18 | 0.13 | −0.18 | −0.28* |
| 10. Fasting cholesterol | −0.05 | 0.18 | −0.06 | −0.16 | 0.06 |
| 11. BMI | −0.03 | 0.30** | −0.09 | −0.15 | −0.02 |
| 12. Perceived stress | −0.12 | 0.06 | 0.15 | −0.27** | −0.21* |
| 13. Depressive symptoms | −0.17 | 0.01 | 0.21* | −0.16 | −0.21* |
NOTE: Higher scores on the Hollingshead Two-Factor Index of Social Position (i.e., education/occupation) and the Leisure Time Exercise Questionnaire reflect lower levels of objective SES and exercise frequency, respectively
FMD: flow-mediated dilation, SSS: subjective social status, MAP: mean arterial pressure, BMI: body mass index
*p < 0.05 (two-tailed); **p < 0.01; ***p < 0.001
Primary Regression Analyses
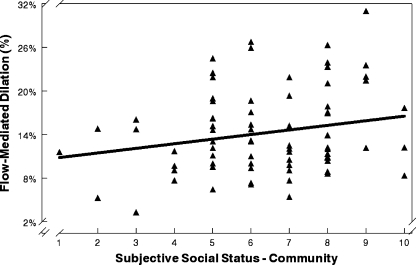
As shown in Table 3, regression analyses of SSS-Community on FMD were conducted with adjustment for age, resting MAP, socially desirable response bias, and exercise frequency. Results indicate that lower reported social status in the community was significantly associated with lower FMD (p < 0.05) and accounted for 8% of the total variance explained by the model (18%). The full model of SSS-Community on FMD including covariates was significant (F (5, 65) = 2.89; p < 0.05, R 2 = 0.18). Figure 1 illustrates how SSS-Community scores related to FMD.
Table 3.
Regression of subjective social status in the community on flow-mediated dilation (final step)
| Dependent variable | Steps | ΔR 2 | ΔF | B (SE) | β | p |
|---|---|---|---|---|---|---|
| Flow-mediated dilation | 1. Covariates | 0.10 | 1.89 | |||
| a. Age: | 0.16 (0.08) | 0.25 | 0.039* | |||
| b. Resting MAP: | −0.11 (0.06) | −0.21 | 0.075 | |||
| c. Social desirability: | −0.57 (0.82) | −0.08 | 0.488 | |||
| d. Exercise: | −0.92 (0.97) | 0.11 | 0.348 | |||
| 2. SSS-Community | 0.08 | 6.56 | 0.97 (0.38) | 0.31 | 0.013* |
NOTE: Higher scores on the Leisure Time Exercise Questionnaire (i.e., exercise frequency) reflect lower frequency of weekly exercise
SSS: subjective social status, MAP: mean arterial pressure
*p < 0.05
Fig. 1.
SS–Community scores were positively associated with flow-mediated dilation. Adults reporting lower levels of subjective social status in their community exhibited lower levels of endothelial functioning
Follow-Up Regression Analyses
Like previous studies [5, 31, 37–40], we wanted to examine whether subjective SES explained variance in FMD beyond what was accounted for by traditional objective indicators of SES. Follow-up regression analyses were conducted with annual income and Hollingshead social index scores (i.e., education/occupation) added as covariates to the original model of SSS-Community on FMD. As shown in Table 4, neither of the objective SES measures reached significance for FMD in the model. Furthermore, SSS-Community remained a significant predictor (p < 0.01) that explained 11% of variance in FMD, after adjustment for objective SES measures and other covariates in this model (F (7,63) = 2.67; p < 0.05, R 2 = 0.23).
Table 4.
Regression of subjective social status in the community on flow-mediated dilation with adjustments for objective socioeconomic measures (final step)
| Dependent variable | Steps | ΔR 2 | ΔF | B (SE) | β | p |
|---|---|---|---|---|---|---|
| Flow-mediated dilation | 1. Covariates | 0.12 | 1.42 | |||
| a. Age: | 0.15 (0.07) | 0.25 | 0.045* | |||
| b. Resting MAP: | −0.12 (0.06) | −0.22 | 0.068 | |||
| c. Social desirability: | −0.81 (0.81) | −0.12 | 0.322 | |||
| d. Exercise frequency: | 1.14 (0.95) | 0.14 | 0.237 | |||
| e. Education/occupation: | 0.02 (0.05) | 0.04 | 0.745 | |||
| f. Annual income: | 0.00 (0.00) | −0.10 | 0.431 | |||
| 2. SSS-Community | 0.11 | 9.17 | 1.14 (0.38) | 0.38 | 0.004** |
NOTE: Higher scores on the Hollingshead Two-Factor Index of Social Position (i.e., education/occupation) and higher scores on the Leisure Time Exercise Questionnaire (i.e., exercise frequency) reflect lower levels of objective SES and exercise frequency, respectively
SSS: subjective social status, MAP: mean arterial pressure
*p < 0.05; **p < 0.01
Exploratory Regression Analyses
Two exploratory regressions were conducted (data not shown) with modified versions of the original SSS-Community on FMD model to assess whether other potential confounders might account for the observed relationship between perceived status in the community and endothelial function. One exploratory regression added a pair of traditional CVD risk factors (i.e., BMI and fasting cholesterol) to the original covariates, and the other exploratory model added a pair of psychosocial risk factors (i.e., depressive and stress symptom scores on the CES-D and Perceived Stress Scale, respectively). No multicollinearity was detected, despite significant associations found within these pairs of exploratory covariates (p’s < 0.05). Results indicate that SSS-Community remained significantly associated with FMD in both of these exploratory regressions (p’s < 0.05), while none of the exploratory covariates approached significance for FMD.
Discussion
Using primarily objective measures of social status, many studies have shown that individuals with lower SES exhibit poorer cardiovascular health than those with higher SES, beyond the differences explained by traditional CVD risk factors, health behaviors, and access to health care [1–4]. However, subjective social status also might be a powerful predictor of cardiovascular health, even when analyses are adjusted for objective measures of SES [37–40, 42]. An individual’s subjective social status may involve a “cognitive averaging” of objective SES indicators and other nuanced aspects of social standing, whereby individuals judge their relative social standing in different contexts based on accumulated and anticipated life experiences [31]. The current study found that participants perceiving themselves to be of lower social status in their communities (i.e., SSS-Community scores) exhibited reduced endothelial function (i.e., lower FMD). Regressions showed that SSS-Community scores accounted for 8% of the variance in FMD, after adjustments for age, resting MAP, socially desirable response bias, and exercise frequency (p < 0.05). Moreover, this relationship was strengthened after additional adjustments for objective SES measures (income, education/occupation), such that SSS-Community accounted for 11% of the variance in FMD (p < 0.01) explained by this model.
Due to the lack of directly comparable research on the relationship between SES and FMD, it is difficult to synthesize our findings with the literature. In one of the few prior studies that assessed SSS-Community, no association was found with self-reported health at 3-year follow-up among older Taiwanese adults after analyses were adjusted for baseline self-reported health [41]. Although that study’s prospective design is beneficial, it may be limited by its self-report assessment of health (i.e., asking respondents to rate their current health as excellent, good, average, not so good, or poor) and its lack of adjustment for socially desirable response bias. A study that is more comparable to our work was conducted by Ghaed and Gallo [42] who reported that middle-aged women with lower SSS-Community exhibited increased ambulatory diastolic BP, after adjustments for objective SES and other confounders (e.g., exercise). They posited that this association was likely partially explained by the increased levels of stress, depression, anxiety, and pessimism found among those women with lower SSS-Community. Consistent with their work, lower SSS-Community in the current sample correlated with higher stress and higher depressive symptoms, as well as lower frequency of exercise (Table 2). However, our exploratory regressions showed that neither stress nor depressed mood (nor exercise) correlated with FMD and that SSS-Community remained significant for FMD after adjustments for these psychosocial variables. It would be helpful for future research on endothelial function and SSS-Community to assess other psychological characteristics, such as anxiety and pessimism, as well as neuroticism.
Endothelial dysfunction could be a pathway through which psychosocial factors, such as subjective social status, are linked to CVD. However, the exact nature of this mechanism needs further research. Harris and Matthews [24] posited that a predisposition for autonomic hyperactivity could disturb the functional antagonism that normally operates between the endothelium and the autonomic nervous system to regulate vascular tone in healthy arteries. It would be useful for future research to assess SSS-Community in relation to both endothelial and autonomic functioning. In a study by Gianaros and colleagues [33], SSS-USA was positively associated with gray matter volume in a brain region involved in the experience of emotions and the regulation of physiological and behavioral reactivity. It would be interesting to learn whether SSS-USA and SSS-Community scores show any differences in associations with these brain regions. While SSS-Community showed no correlations with BP, BMI, or cholesterol in our healthy sample, it would be informative to investigate whether the association between SSS-USA and metabolic syndrome reported by Manuck et al. [40] also would be found with SSS-Community.
The lack of correlation between FMD and objective SES measures in the current study is surprising, given that the SES–CVD literature is primarily based on objective SES. However, income was positively associated with resting MAP and BMI, which may have been due partly to age-related increases in all of these variables. The positive correlation between income and SSS-Community was the only significant association between an objective and a subjective SES measure, though they shared no common associations with other variables. Although both SSS measures were associated with perceived stress in this sample, SSS-Community seems to capture a fairly distinct dimension of social status and shows a largely different set of correlations than SSS-USA. Higher SSS-Community was correlated with higher FMD, higher frequency of exercise, and lower depressive symptoms, while SSS-USA showed no significant associations with these variables. Further study is needed to determine why endothelial function correlates with perceptions of social status in the local community, but not perceived status in the USA overall. One issue to consider is how respondents interpret each of these subjective measures. The SSS-USA asks respondents how they believe they rank compared to others in the nation based on traditionally defined SES dimensions (e.g., money, education, jobs), which are most often assessed by separate objective measures. In contrast, SSS-Community does not predefine social status dimensions or the comparison group parameters for respondents. It allows them to self-define their “community” and to determine what markers of social status are of value in this community’s social hierarchy [45]. Thus, the SSS-Community scale could be more subjective and capture broader dimensions of perceived social status than the SSS-USA scale.
Individuals might derive cardiovascular benefits from feeling that they have high community status within their neighborhood, religious group, social organization, workplace, or some other type of “community,” though they are not necessarily well educated with a prestigious occupation and/or a high salary. The reference groups of individuals in the community that respondents select for self-comparisons are likely much smaller, more specific, and “closer to home” than more vague comparisons to the rest of the nation. Such personally relevant comparisons to community members are potentially more directly related to indicators of physical (and emotional) health. Having contact with their “community” in daily life and being repeatedly reminded of one’s status relative to others in this group could be physically and psychologically beneficial or detrimental, depending on the perceived status [42]. Our statistical adjustments for perceived stress, depressed mood, social desirability, and cardiovascular risk factors only slightly attenuated the significant relationship between FMD and SSS-Community. Future studies should examine other potential influences on this relationship that reflect the social interchanges likely embedded in one’s perceptions of community status, such as social support, social networks, and social dominance.
Potential confounding effects on endothelial function were likely reduced by our relatively strict exclusion criteria, physician confirmation of health status, and inpatient testing environment, which limited the possible influence of smoking and dietary factors (e.g., caffeine, alcohol, high fat, nitrates). Other strengths include adjustments for varying levels of several traditional (i.e., BP, exercise, cholesterol, BMI) and psychosocial (i.e., stress, depressive symptoms) risk factors for CVD, as well as socially desirable response bias. In addition, the FMD and SSS-Community association remained significant after adjusting for objective SES measures (i.e., income, education/occupation) and other covariates.
Several limitations must be noted. Further research with larger samples would be beneficial in accommodating adjustments for additional potential confounders (e.g., menstrual phase) and in assessing generalizability to other populations. Although our participants showed no sex differences in FMD or in any of the SES measures, this may not generalize to other samples of men and women. Our inclusion/exclusion criteria were advantageous in reducing variance in this uniformly healthy sample. However, it is uncertain whether our findings generalize to populations in which medication use/comorbidity is the rule, not the exception. In addition, findings based on this sample of young to middle-aged adults may have limited generalizability to other age groups. It would be informative for future work to assess relationships between subjective social standing and FMD in older and less healthy populations. Finally, these cross-sectional data cannot establish perceived status in the community as the cause of the observed vasodilation differences and cannot determine the direction of the FMD and SSS-Community association. Still, it seems unlikely that endothelial function would influence one’s perceived social position in the community.
In sum, FMD was associated with SSS-Community, but not with the other subjective SES measure (i.e., SSS-US) or with either of the objective SES scales (i.e., income, education/occupation). We found that lower perceived social standing in one’s community was associated with poorer functioning of the endothelium in young to middle-aged adults, even after adjustment for objective SES and a variety of other covariates. These findings suggest that endothelial dysfunction could be a pathway linking subjective SES to CVD.
Acknowledgments
National Institutes of Health Grants HL36005, RR00827, and P60MD00220 supported this research.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Pickering T. Cardiovascular pathways: Socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896:262–277. doi: 10.1111/j.1749-6632.1999.tb08121.x. [DOI] [PubMed] [Google Scholar]
- 2.Strike PC, Steptoe A. Psychosocial factors in the development of coronary artery disease. Prog Cardiovasc Dis. 2004;46:337–347. doi: 10.1016/j.pcad.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Rosengren A, Wedel H, Wilhelmsen L. Coronary heart disease and mortality in middle-aged men from different occupational classes in Sweden. BMJ. 1988;297:1497–1500. doi: 10.1136/bmj.297.6662.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laaksonen M, Talala K, Martelin T, et al. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: A follow-up of 60 000 men and women over 23 years. Eur J Public Health. 2008;18:38–43. doi: 10.1093/eurpub/ckm051. [DOI] [PubMed] [Google Scholar]
- 5.Wright CE, Steptoe A. Subjective socioeconomic position, gender and cortisol responses to waking in an elderly population. Psychoneuroendocrinology. 2005;30:582–590. doi: 10.1016/j.psyneuen.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Thurston RC, Matthews KA. Racial and socioeconomic disparities in arterial stiffness and intima media thickness among adolescents. Soc Sci Med. 2009;68:807–813. doi: 10.1016/j.socscimed.2008.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gruenewald TL, Kemeny ME, Aziz N. Subjective social status moderates cortisol responses to social threat. Brain Behav Immun. 2006;20:410–419. doi: 10.1016/j.bbi.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Frick M, Weidinger F. Endothelial function: A surrogate endpoint in cardiovascular studies? Curr Pharm Des. 2007;13:1741–1750. doi: 10.2174/138161207780831211. [DOI] [PubMed] [Google Scholar]
- 9.Vita JA, Keaney JF., Jr Endothelial function: A barometer for cardiovascular risk? Circulation. 2002;106:640–642. doi: 10.1161/01.CIR.0000028581.07992.56. [DOI] [PubMed] [Google Scholar]
- 10.Corretti MC, Anderson TJ, Benjamin EJ, International Brachial Artery Reactivity Task Force et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–265. doi: 10.1016/S0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- 11.Korkmaz H, Onalan O. Evaluation of endothelial dysfunction: Flow-mediated dilation. Endothelium. 2008;15:157–163. doi: 10.1080/10623320802228872. [DOI] [PubMed] [Google Scholar]
- 12.Fronek A, Allison M. Non-invasive assessment of endothelial activity in patients with coronary heart disease and cardiovascular risk factors. Vasa. 2008;37:137–142. doi: 10.1024/0301-1526.37.2.137. [DOI] [PubMed] [Google Scholar]
- 13.Suzuki T, Hirata K, Elkind MS, et al. Metabolic syndrome, endothelial dysfunction, and risk of cardiovascular events: The Northern Manhattan Study (NOMAS) Am Heart J. 2008;156:405–410. doi: 10.1016/j.ahj.2008.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pálinkás A, Tóth E, Amyot R, Rigo F, Venneri L, Picano E. The value of ECG and echocardiography during stress testing for identifying systemic endothelial dysfunction and epicardial artery stenosis. Eur Heart J. 2002;23:1587–1595. doi: 10.1053/euhj.2002.3170. [DOI] [PubMed] [Google Scholar]
- 15.Venneri L, Poggianti E, Jambrik Z, Varga A, Palinkas A, Picano E. The elusive prognostic value of systemic endothelial function in patients with chest pain syndrome. Int J Cardiol. 2007;119:109–111. doi: 10.1016/j.ijcard.2006.07.069. [DOI] [PubMed] [Google Scholar]
- 16.Yeboah J, Hsu FC, Burke GL, Herrington DM. Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: The cardiovascular health study. Circulation. 2007;115:2390–2397. doi: 10.1161/CIRCULATIONAHA.106.678276. [DOI] [PubMed] [Google Scholar]
- 17.Brevetti G, Silvestro A, Schiano V, Chiariello M. Endothelial dysfunction and cardiovascular risk prediction in peripheral arterial disease: Additive value of flow-mediated dilation to ankle-brachial pressure index. Circulation. 2003;108:2093–2098. doi: 10.1161/01.CIR.0000095273.92468.D9. [DOI] [PubMed] [Google Scholar]
- 18.Gokce N, Keaney JF, Jr, Hunter LM, Watkins MT, Menzoian JO, Vita JA. Risk stratification for postoperative cardiovascular events via noninvasive assessment of endothelial function: A prospective study. Circulation. 2002;105:1567–1572. doi: 10.1161/01.CIR.0000012543.55874.47. [DOI] [PubMed] [Google Scholar]
- 19.Gokce N, Keaney JF, Jr, Hunter LM, et al. Predictive value of noninvasively determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003;41:1769–1775. doi: 10.1016/S0735-1097(03)00333-4. [DOI] [PubMed] [Google Scholar]
- 20.Huang AL, Silver AE, Shvenke E, et al. Predictive value of reactive hyperemia for cardiovascular events in patients with peripheral arterial disease undergoing vascular surgery. Arterioscler Thromb Vasc Biol. 2007;27:2113–2119. doi: 10.1161/ATVBAHA.107.147322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patti G, Pasceri V, Melfi R, et al. Impaired flow-mediated dilation and risk of restenosis in patients undergoing coronary stent implantation. Circulation. 2005;111:70–75. doi: 10.1161/01.CIR.0000151308.06673.D2. [DOI] [PubMed] [Google Scholar]
- 22.Gordon JL, Lavoie KL, Arsenault A, Ditto B, Bacon SL. Health behaviors and endothelial function. J Behav Med. 2008;31:5–21. doi: 10.1007/s10865-007-9129-0. [DOI] [PubMed] [Google Scholar]
- 23.Gottdiener JS, Kop WJ, Hausner E, McCeney MK, Herrington D, Krantz DS. Effects of mental stress on flow-mediated brachial arterial dilation and influence of behavioral factors and hypercholesterolemia in subjects without cardiovascular disease. Am J Cardiol. 2003;92:687–691. doi: 10.1016/S0002-9149(03)00823-3. [DOI] [PubMed] [Google Scholar]
- 24.Harris KF, Matthews KA. Interactions between autonomic nervous system activity and endothelial function: A model for the development of cardiovascular disease. Psychosom Med. 2004;66:153–164. doi: 10.1097/01.psy.0000116719.95524.e2. [DOI] [PubMed] [Google Scholar]
- 25.Narita K, Murata T, Hamada T, et al. Interactions among higher trait anxiety, sympathetic activity, and endothelial function in the elderly. J Psychiatr Res. 2007;41:418–427. doi: 10.1016/j.jpsychires.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Wagner JA, Tennen H, Mansoor GA, Abbott G. History of major depressive disorder and endothelial function in postmenopausal women. Psychosom Med. 2006;68:80–86. doi: 10.1097/01.psy.0000195868.68122.9e. [DOI] [PubMed] [Google Scholar]
- 27.Leeson CP, Whincup PH, Cook DG, et al. Flow-mediated dilation in 9- to 11-year-old children: The influence of intrauterine and childhood factors. Circulation. 1997;96:2233–2238. doi: 10.1161/01.cir.96.7.2233. [DOI] [PubMed] [Google Scholar]
- 28.Charakida M, Donald AE, Terese M, et al. ALSPAC (Avon Longitudinal Study of Parents and Children) study team. Endothelial dysfunction in childhood infection. Circulation. 2005;111:1660–1665. doi: 10.1161/01.CIR.0000160365.18879.1C. [DOI] [PubMed] [Google Scholar]
- 29.Kivimäki M, Smith GD, Juonala M, et al. Socioeconomic position in childhood and adult cardiovascular risk factors, vascular structure, and function: Cardiovascular risk in young Finns study. Heart. 2006;92:474–480. doi: 10.1136/hrt.2005.067108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schnittker J, McLeod JD. The social psychology of health disparities. Annu Rev Sociol. 2005;31:75–103. doi: 10.1146/annurev.soc.30.012703.110622. [DOI] [Google Scholar]
- 31.Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Soc Sci Med. 2003;56:1321–1333. doi: 10.1016/S0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- 32.Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000;19:586–592. doi: 10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 33.Gianaros PJ, Horenstein JA, Cohen S, et al. Perigenual anterior cingulate morphology covaries with perceived social standing. Soc Cogn Affect Neurosci. 2007;2:161–173. doi: 10.1093/scan/nsm013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen S, Alper CM, Doyle WJ, Adler N, Treanor JJ, Turner RB. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychol. 2008;27:268–274. doi: 10.1037/0278-6133.27.2.268. [DOI] [PubMed] [Google Scholar]
- 35.Kopp M, Skrabski A, Réthelyi J, Kawachi I, Adler NE. Self-rated health, subjective social status, and middle-aged mortality in a changing society. Behav Med. 2004;30:65–70. doi: 10.3200/BMED.30.2.65-72. [DOI] [PubMed] [Google Scholar]
- 36.Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol. 2000;19:613–618. doi: 10.1037/0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- 37.Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosom Med. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- 38.Adler N, Singh-Manoux A, Schwartz J, Stewart J, Matthews K, Marmot MG. Social status and health: A comparison of British civil servants in Whitehall-II with European- and African-Americans in CARDIA. Soc Sci Med. 2008;66:1034–1045. doi: 10.1016/j.socscimed.2007.11.031. [DOI] [PubMed] [Google Scholar]
- 39.Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: The role of subjective social status. Soc Sci Med. 2008;67:330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Manuck SB, Phillips JE, Gianaros PJ, Flory JD, Muldoon MF. Subjective socioeconomic status and presence of the metabolic syndrome in midlife community volunteers. Psychosom Med. 2010;72:35–45. doi: 10.1097/PSY.0b013e3181c484dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Collins AL, Goldman N. Perceived social position and health in older adults in Taiwan. Soc Sci Med. 2008;66:536–544. doi: 10.1016/j.socscimed.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghaed SG, Gallo LC. Subjective social status, objective socioeconomic status, and cardiovascular risk in women. Health Psychol. 2007;26:668–674. doi: 10.1037/0278-6133.26.6.668. [DOI] [PubMed] [Google Scholar]
- 43.Moens AL, Goovaerts I, Claeys MJ, Vrints CJ. Flow-mediated vasodilation: A diagnostic instrument, or an experimental tool? Chest. 2005;127:2254–2263. doi: 10.1378/chest.127.6.2254. [DOI] [PubMed] [Google Scholar]
- 44.Bardwell WA, Dimsdale JE. The impact of ethnicity and a socially desirable response style on the self-report of negative affect. J Appl Biobehav Res. 2001;6:27–38. doi: 10.1111/j.1751-9861.2001.tb00105.x. [DOI] [Google Scholar]
- 45.Adler N, Stewart J. The MacArthur Scale of subjective social status. Available at http://www.macses.ucsf.edu/Research/Psychosocial/notebook/subjective.html. Accessibility verified January 07, 2010.
- 46.Cooper DC, Mills PJ, Bardwell WA, Ziegler MG, Dimsdale JE. The effects of ethnic discrimination and socioeconomic status on endothelin-1 among blacks and whites. Am J Hypertens. 2009;22:698–704. doi: 10.1038/ajh.2009.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Celermajer DS, Sorensen KE, Gooch VM. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-F. [DOI] [PubMed] [Google Scholar]
- 48.Harris CW, Edwards JL, Baruch A, et al. Effects of mental stress on brachial artery flow-mediated vasodilation in healthy normal individuals. Am Heart J. 2000;139:405–411. doi: 10.1016/s0002-8703(00)90083-8. [DOI] [PubMed] [Google Scholar]
- 49.Hollingshead AB. Two factor index of social position. New Haven: Yale University Press; 1957. [Google Scholar]
- 50.Karasek R. Job content questionnaire and user’s guide. Lowell, MA: Department of Work Environment, University of Massachusetts-Lowell; 1985. [Google Scholar]
- 51.Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychol Health. 2004;19:237–246. doi: 10.1080/08870440310001638098. [DOI] [Google Scholar]
- 52.Crowne DP, Marlowe DA. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- 53.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- 54.Jacobs DR, Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25:81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 55.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psych Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 56.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]