Abstract
Objectives
To evaluate the association between carotid intima-media thickness (CIMT) and the presence of aortic arch plaques (AP) in a community-based cohort.
Background
Large AP are associated with ischemic stroke. CIMT is a marker of subclinical atherosclerosis and a strong predictor of cardiovascular disease and stroke. The association between CIMT and AP has been studied in stroke patients, but not in the general population. Aim of this study was to investigate this association in an elderly asymptomatic cohort, and the possibility to use CIMT to predict the presence or absence of large AP.
Methods
Stroke-free control subjects from the Aortic Plaque and Risk of Ischemic Stroke (APRIS) Study underwent transesophageal echocardiography and high-resolution B-mode ultrasound of the carotid arteries. CIMT was measured at the common carotid artery, bifurcation and internal carotid artery. The association between CIMT and AP was analyzed by multivariate regression models. Positive and negative predictive values of CIMT for large (≥ 4 mm) AP were calculated.
Results
Among 138 subjects, large AP was present in 35 (25.4%) subjects. Only CIMT at the bifurcation was associated with large AP after adjustment for atherosclerotic risk factors (p=0.007). Positive and negative predictive value for AP ≥ 4 mm of CIMT at the bifurcation above the 75th percentile (≥ 0.95 mm) were 42% and 80%, respectively. Negative predictive value increased to 87% when the median CIMT value (0.82 mm) was used.
Conclusions
CIMT at the bifurcation is independently associated with AP ≥ 4 mm. Its strong negative predictive value for large arch plaque indicates that CIMT may be used as an initial screening test to exclude severe arch atherosclerosis in the general population.
Carotid artery Intima Media Thickness (CIMT) is an established marker of subclinical atherosclerosis and a non-invasive correlate of atherosclerotic plaque at an early stage(1,2). There is epidemiological evidence that increased CIMT in subjects with vascular risk factors is an independent predictor of cardiovascular events and end-organ damage(3,4).
CIMT detected by B-mode ultrasound was shown to be a predictor of future coronary artery disease, cardiovascular events and stroke(5–8). Increased CIMT may help identify high-risk patients who would benefit from aggressive risk factor control(9,10).
The association between atherosclerotic disease of the aortic arch and the risk of ischemic stroke has been established in subjects over the age of 60(11–13). The stroke risk is associated with both the thickness of the aortic arch plaque (with 4 mm having been used as a cutoff for risk stratification) and its extension to the brachio-cephalic arteries(14).
The relationship between CIMT and aortic arch plaques has been only recently studied in patients with stroke(15), and the predictive value of an increased CIMT for the presence of large aortic plaques in the general population has not been established.
The present study examined the relationship between CIMT and the presence of aortic arch plaques in elderly asymptomatic individuals. In particular, it was aimed to evaluate whether an increased CIMT predicts the presence of large (≥4mm) aortic arch plaques, which carry the highest risk for ischemic stroke.
METHODS
Subjects
The study population consisted of 138 stroke-free control subjects, (66 men and 72 women), age 55 to 74 years from the NINDS (National Institute of Neurological Disorders and Stroke)-funded Aortic Plaque and Risk of Ischemic Stroke (APRIS) Study, a nested case-control study from the cohort of the Northern Manhattan Study (NOMAS). NOMAS is an ongoing, prospective, population-based epidemiological study designed to determine stroke incidence, risk factors, and outcomes in a multiethnic, urban population living in Northern Manhattan(16). All individuals that were potential matches for APRIS stroke subjects on the basis of age, sex and race-ethnicity were requested to participate in the study.
As part of NOMAS, baseline data was collected through interviews by trained bilingual research assistants using standardized data collection instruments, review of the medical records, physical and neurological examination by study physicians, and fasting blood was collected. Standardized questions were adapted from the Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System(17). Arterial hypertension was defined as a systolic blood pressure recording ≥140 mm Hg or a diastolic blood pressure recording ≥ 90 mm Hg based on the mean of two readings, a patient’s self-report of a history of hypertension, or antihypertensive medication use. Diabetes mellitus was defined by a patient’s self-report of such history, insulin use, oral hypoglycemic use, or fasting glucose ≥126 mg/dL. Hypercholesterolemia was defined as total serum cholesterol >240 mg/dL, a patient’s self-report of hypercholesterolemia or the presence of lipid-lowering treatment. Smoking was defined by current use (within a current year) of cigar or cigarettes.
Informed consent was obtained from all subjects. The study was approved by the Institutional Review Board of Columbia University Medical Center.
Detection of Aortic Plaques
Transesophageal echocardiography (TEE) was performed upon enrollment. TEE examination of the aorta was performed in a systematic fashion as previously described(18) using a multiplane transducer. The aortic arch was defined as the portion of aorta comprised between the curve at the end of the ascending portion and the takeoff of the left subclavian artery. A plaque was defined as a discrete protrusion of the intimal surface of the vessel at least 2 mm in thickness, different in appearance and echogenicity from the adjacent intact intimal surface. The presence and location of any plaque was recorded on VHS videotapes and interpreted off-line by a single experienced echocardiographer (MDT) blinded to the duplex carotid sonography findings. In cases of multiple plaques, the most advanced lesion was considered. Plaques were classified into small (>1mm and ≤3.9 mm) or large (≥ 4 mm). An example of large arch plaque by TEE is shown in Figure 1. Intra-observer variability for the chosen categorization was low (correlation coefficient 0.95).
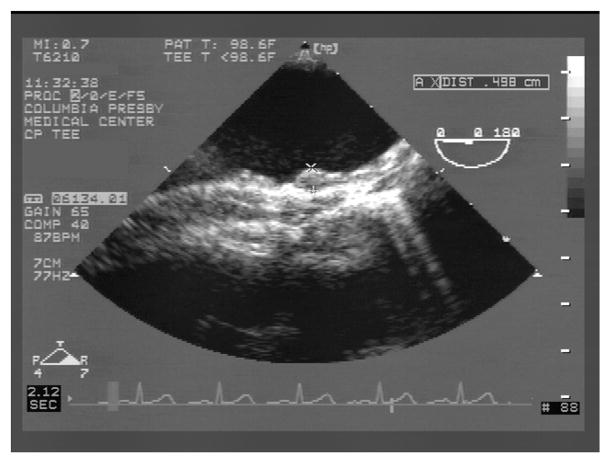
FIGURE 1.
Example of large atherosclerotic plaque in the mid portion of the aortic arch by transesophageal echocardiography (TEE). The maximum plaque thickness (0.5 cm) is measured perpendicular to the major axis of the vascular lumen.
Assessment of Carotid Artery Intima Media Thickness (CIMT)
CIMT was assessed by high-resolution B-mode carotid ultrasound (Diasonics 2D-Gateway, 7.5-MHz probe) according to the standardized scanning and reading protocols as previously described(19,20). The carotid IMT scanning protocol consisted of the near and the far wall of the 3 carotid segments, defined as follows: (1) 10 to 20 mm proximal to the tip of the flow divider into the common carotid artery (CCA); (2) the carotid bifurcation beginning at the tip of the flow divider and extending 10 mm proximal to the flow divider tip; and (3) the proximal 10 mm of the internal carotid artery (ICA). Measurements of IMT were performed off-line with the use of the M’Ath automatic computerized edge tracking system (Canevas)(21). The M’Ath program searches for the true wall boundaries using an intensity gradient detection algorithm. An example of IMT measurement is shown in Figure 2. Reproducibility studies in our laboratory have been previously reported(20,21), with an interobserver correlation coefficient of 0.77 (percent error 10.6%), and an intraobserver correlation coefficient of 0.94 (percent error 5.6%)(20). In each carotid segment, mean distance between intima and media were measured outside the portion of plaques. The total CIMT was calculated as a composite measure (mean of the 12 carotid sites) that combined the near and the far wall of the CCA IMT, the bifurcation IMT, and the ICA IMT of both sides of the neck.
FIGURE 2.
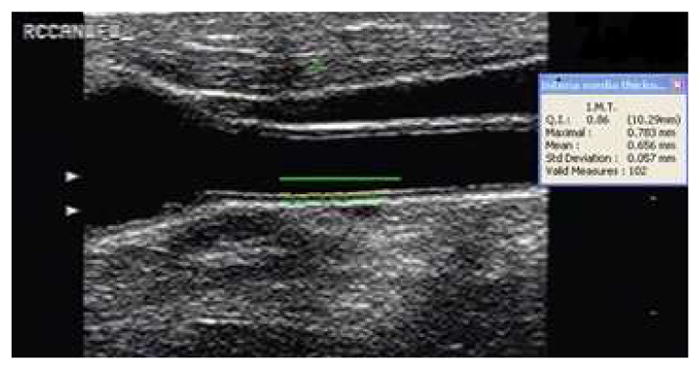
Carotid IMT measurements performed in the far wall of the right common carotid artery (RCCAFW) by the automated computer assisted edge detection software. Mean IMT in the RCCAFW is 0.656±0.058 mm.
Similarly, IMT in carotid bifurcation and internal carotid artery was measured. Total carotid IMT is an average measure of IMT measured in all carotid arteries of the both side of the neck.
Statistical Analysis
Descriptive statistics were performed and data are presented as mean values ± 1 standard deviation for continuous variables, and as proportions for categorical variables. Differences between proportions were assessed by the chi-square test, replaced by Fisher’s exact test when the expected cell count was less than 5. Differences between mean values were assessed by unpaired Student’s t-test.
The values of total CIMT and CIMT at the various carotid segments were analyzed. Multivariate logistic regression analysis was used to test the association between CIMT (independent variable) and large aortic arch plaque (dependent variable) after entering age, sex and atherosclerotic risk factors as potential confounding factors in the model. Diabetes mellitus and hypercholesterolemia were significantly associated with aortic arch plaques in univariate analysis, and therefore were entered as independent variables in the model, along with age and sex. Hypertension and smoking were not associated with large arch plaques and therefore not included in the final model.
For the CIMT significantly associated with arch plaques ≥ 4mm in the multivariate analyses, positive and negative predictive value were calculated, using the 75th percentile and the median value of the total CIMT distribution.
RESULTS
Subjects characteristics
Demographics, cardiovascular risk factors, aortic arch plaque, and CIMT values for the study population are summarized in Table 1.
Table 1.
Demographics and clinical characteristics of the study subjects
| Age (years, mean ± SD) | 66.3 ± 8.5 |
| Female Sex | 72 (52 %) |
| Race/Ethnicity | |
| White | 17 (12.3%) |
| Black | 42 (30.4%) |
| Hispanic | 77 (55.8%) |
| Other | 2 (1.5%) |
| Risk Factors | |
| Diabetes Mellitus | 33 (23.9%) |
| Arterial Hypertension | 83 (60.1%) |
| Hypercholesterolemia | 69 (50.0%) |
| Current Cigarette Smoking | 20 (14.7%) |
| Aortic Arch Plaque | |
| Any Thickness | 85 (61.6%) |
| Large (≥4mm) | 35 (25.4%) |
| Carotid plaque | 75 (54.4%) |
| Carotid IMT (mm, mean ± SD) | |
| Total | 0.74 ± 0.13 |
| CCA | 0.77 ± 0.17 |
| BIF | 0.84 ± 0.18 |
| ICA | 0.59 ± 0.12 |
IMT = Intima-media Thickness
Total = Common + Bifurcation + Internal
CCA = Common Carotid Artery
BIF = Carotid Bifurcation
ICA = Internal Carotid Artery
The mean age of the study subjects was 66.3 ± 8.5 years, 52% were women and the majority were Hispanics (55.8%). 60% of the subjects had hypertension, 50% hypercholesterolemia, 24% had diabetes mellitus, and 15% were current smokers.
Aortic arch plaques of any thickness were present in over 60% of the study group, and large (≥ 4mm) aortic arch plaques were present in 35 subjects (25.4%). Whites had a slightly higher prevalence of large plaques (35.3%) than Hispanics (26.0%) and Blacks (21.4%), but the differences were not statistically significant. Subjects with large arch plaques had significantly higher prevalence of hypercholesterolemia (68.6% vs. 43.7%; p=0.01) and lower prevalence of diabetes mellitus (11.4% vs. 28.2%; p<0.05) than those with small or no plaques. Prevalence of hypertension and smoking was not significantly greater in subjects with large plaques. The mean total CIMT was 0.74 ± 0.13 mm, and the highest mean CIMT was found in carotid bifurcation (BIF; 0.84 ± 0.18 mm; Table 1). Carotid plaque was present in 75 subjects (54.4%).
Correlation between CIMT and aortic arch atherosclerotic plaques
Table 2 shows the Spearman correlation coefficients of total CIMT and CIMT at different carotid sites (continuous variable) with the presence of any plaque or large plaque in the aortic arch. Total CIMT and CIMT in BIF were significantly associated with presence of both any aortic arch plaque and large aortic arch plaque. CIMT in CCA was significantly correlated with presence of aortic arch plaque of any thickness, but not with large aortic arch plaques. A scatter plot of CIMT at the bifurcation and aortic plaque thickness is shown in Figure 3. The presence of carotid plaque was associated with large aortic plaque (34.7% vs. 14.3%; odds ratio 3.18, 95% confidence interval 1.36–7.46, p=0.008).
Table 2.
Spearman correlation coefficients between carotid IMT and presence of aortic arch plaque
| Total CIMT | CCA IMT | BIF IMT | ICA IMT | ||
|---|---|---|---|---|---|
| Any Arch Plaque | Coefficient (P-Value) | 0.19740 (0.02) | 0.18200 (0.03) | 0.24764 (0.003) | −0.00057 (0.99) |
| Large (≥4mm) Arch Plaque | Coefficient (P-Value) | 0.22932 (0.007) | 0.16076 (0.06) | 0.27949 (0.001) | 0.07442 (0.39) |
CIMT = Carotid Intima-Media Thickness
CCA = Common Carotid Artery
BIF = Carotid Bifurcation
ICA = Internal Carotid Artery
FIGURE 3.
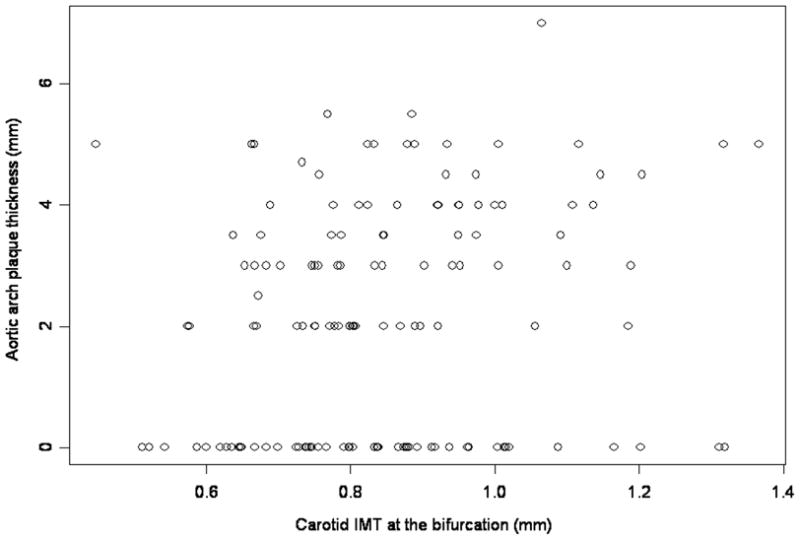
Scatter plot of carotid IMT at the bifurcation and aortic arch plaque thickness.
Association between CIMT and large aortic arch plaques
The association between CIMT and large aortic arch plaques was tested in univariate and multivariate models adjusting for demographic variables and established risk factors for aortic atherosclerosis (Table 3). Total CIMT was associated with large arch plaque in univariate analysis (p=0.02). The association was of borderline significance (p=0.05) after adjustment for age and sex, and no longer significant after adjustment for diabetes and hypercholesterolemia. In the analysis of CIMT in different carotid segments, only CIMT in BIF remained significantly associated with large arch plaque in a fully adjusted model (p=0.007), and also after further adjustment for the presence of carotid plaque (p<0.03; data not shown).
Table 3.
Association between carotid IMT and large aortic arch plaque (≥ 4mm)
| Total CIMT | CCA | BIF | ICA | |||||
|---|---|---|---|---|---|---|---|---|
| Model | Estimate (se) | P | estimate (se) | P | estimate (se) P | estimate (se) | P | |
| Unadjusted | 3.39 (1.46) | 0.02 | 1.95 (1.18) | 0.10 | 3.38 (1.14) | 0.003 | 1.31 (1.55) | 0.40 |
| Adjusted for age and sex | ||||||||
| 3.00 (1.51) | 0.05 | 1.65 (1.22) | 0.18 | 3.15 (1.16) | 0.007 | 0.73 (1.63) | 0.66 | |
| Age | 0.03 (0.02) | 0.28 | 0.03 (0.02) | 0.20 | 0.02 (0.02) | 0.31 | 0.03 (0.02) | 0.15 |
| Sex | 0.17 (0.40) | 0.68 | 0.22 (0.40) | 0.58 | 0.19 (0.41) | 0.65 | 0.20 (0.40) | 0.61 |
| Adjusted for age, sex, and risk factors | ||||||||
| 3.02 (1.63) | 0.06 | 1.30 (1.30) | 0.32 | 3.45 (1.27) | 0.007 | 0.87 (1.73) | 0.62 | |
| Age | 0.03 (0.03) | 0.18 | 0.04 (0.03) | 0.11 | 0.03 (0.03) | 0.22 | 0.04 (0.03) | 0.08 |
| Sex | 0.26 (0.44) | 0.55 | 0.33 (0.43) | 0.45 | 0.22 (0.44) | 0.62 | 0.32 (0.43) | 0.45 |
| Diabetes | −1.23 (0.61) | 0.04 | −1.13 (0.60) | 0.06 | −1.39 (0.62) | 0.03 | −1.10 (0.60) | 0.07 |
| High Cholesterol | 1.15 (0.46) | 0.01 | 1.18 (0.46) | 0.01 | 1.10 (0.47) | 0.02 | 1.26 (0.45) | 0.005 |
se = standard error
CIMT = Carotid Intima-Media Thickness
CCA = Common Carotid Artery
BIF = Carotid Bifurcation
ICA = Internal Carotid Artery
For CIMT in BIF, positive and negative predictive values for presence of large arch plaque were calculated. CIMT at BIF level above the 75th percentile of the CIMT distribution (0.95 mm) yielded a 42% positive predictive value for large aortic arch plaque presence and a negative predictive value of 80% (Table 4). A value of CIMT in BIF below the median (0.82 mm) had a positive predictive value of 37%, but negative predictive value of 87% (Table 5).
Table 4.
Frequency of CIMT at the bifurcation above the 75th Percentile (0.95 mm) by large aortic plaque status.
| Large Arch Plaque | No Large Arch Plaque | Total | |
|---|---|---|---|
| BIF ≥ 0.95 mm | 14 | 19 | 33 |
| BIF <0.95 mm | 21 | 84 | 105 |
| Total | 35 | 103 | 138 |
BIF = Carotid IMT at the bifurcation
Sensitivity = 40% (14/35)
Specificity = 82% (84/103)
Positive Predictive Value = 42% (14/33)
Negative Predictive Value = 80% (84/105)
Table 5.
Frequency of CIMT at the bifurcation above the median value (0.82 mm) by large aortic plaque status.
| Large Arch Plaque | No Large Arch Plaque | Total | |
|---|---|---|---|
| BIF ≥ 0.82 mm | 26 | 44 | 70 |
| BIF <0.82 mm | 9 | 59 | 68 |
| Total | 35 | 103 | 138 |
BIF = Carotid IMT at the bifurcation
Sensitivity = 74% (26/35)
Specificity = 57% (59/103)
Positive Predictive Value = 37% (26/70)
Negative Predictive Value = 87% (59/68)
DISCUSSION
The association between CIMT and risk of cardiovascular events has been established in large studies(19,22). Its association with the presence of significant arch atherosclerosis has only been studied in patients with ischemic stroke(15). Our study examined the relationship between CIMT and the presence of aortic arch plaques in an asymptomatic elderly cohort. CIMT was measured at three different carotid segments (CCA, BIF and ICA) and the total CIMT as a mean value of CIMT in all carotid segments was also considered. The association of CIMT with arch atherosclerosis could have preventive implications, especially if the rapidly obtainable and noninvasive CIMT determination were to be used to predict or exclude significant atherosclerotic lesions in asymptomatic patients. Large arch plaques (usually defined as ≥4 mm in thickness) are a risk factor for stroke in the elderly, and their unsuspected presence is associated with increased stroke risk in patients undergoing open heart surgery(23,24) or invasive diagnostic tests that, like coronary angiography, involve the proximal segment of the aorta(25,26). Since performing a TEE in every elderly asymptomatic patient about to undergo a cardiac procedure or surgery appears excessive, the availability of a simple non-invasive method for excluding large aortic plaques would be desirable.
CIMT and aortic atherosclerosis
We found that CIMT at the carotid bifurcation was the measurement that best correlated with the presence of any aortic plaque, and the only measurement independently associated with aortic arch plaque ≥4mm. Carotid anatomy and hemodynamic factors, such as variations in shear stress along the different aortic and carotid levels, may account for this observation. In particular, CIMT at BIF was a stronger predictor of arch plaque than the total CIMT used in previous studies(15), suggesting that measurement at the bifurcation should be preferred when the relationship between CIMT and arch plaques is analyzed, or when CIMT is used as a predictor of aortic arch atherosclerosis.
Recently, CIMT has been proposed as a useful tool in cardiovascular risk stratification of asymptomatic subjects with multiple risk factors, and has been shown to be an independent predictor of future vascular events across a wide age range(27). CIMT assessed by high resolution B-mode ultrasound has been considered to be the most helpful screening measure among other non-invasive tools for measurement of subclinical atherosclerosis, such as assessment of plaque burden by cardiovascular magnetic resonance and detection of coronary calcium by electron bean computed tomography(28). In asymptomatic persons over 45 years of age, carefully performed carotid ultrasound examination with CIMT measurement can provide incremental information to that contained in the assessment of traditional risk factors (29).
Our study adds more evidence to this concept by showing that CIMT at the bifurcation may be a useful initial screening test to exclude severe aortic arch atherosclerosis in the general population. However, the best negative predictive value that we observed (87% for CIMT at bifurcation) still means that large plaques are present in 13% of subjects with normal IMT. Therefore, the performance of TEE could still be entertained in patients that are considered at higher risk because of multiple atherosclerotic risk factors.
Comparison with previous studies
Although CIMT at BIF was independently correlated with large aortic arch plaques, its positive predictive value for the presence of aortic arch plaques was low, ranging from 37% to 42% for different CIMT cutoff levels. This confirms previous data(14), and underlines how the role of CIMT is not in the prediction of aortic plaque presence, but rather in the exclusion of significant arch atherosclerosis without the need for more invasive or costly diagnostic imaging. Harloff et al. described that CIMT was an independent predictor of aortic wall thickness, and found that the combination of CIMT and carotid distensibility measurements increased the power of carotid ultrasound for excluding significant aortic atherosclerosis(15). In that study, conducted in a group of patients with ischemic stroke, total IMT <0.9 mm had a 92% negative predictive value for complex aortic arch plaque. Our study confirms these results, but extends them to a cohort of stroke-free subjects, for which the use of CIMT for screening and risk stratification purposes appears more appropriate. Besides including only stroke patients, in whom aortic atherosclerosis is more likely to be investigated by TEE for diagnostic reasons, the study of Harloff and al. was conducted in an entirely Caucasian population. Our study, on the other hand, was conducted in a tri-ethnic sample with large representation of minority subjects and therefore a higher burden of traditional risk factors for atherosclerosis. These differences, and the different cutoff levels used (50th or 75th percentile of the distribution in our study, an arbitrarily chosen cutoff of 0.9 mm in the previous study) may account for the slightly lower negative predictive value of CIMT (87% when the 50th percentile was used) observed in our study.
Role of associated factors
CIMT is affected by many factors, including traditional vascular risk factors and lifestyle. Also, socioeconomic status affects the progression of the CIMT, as shown in the Atherosclerosis Risk in Communities (ARIC) Study(30). In addition, different underlying genetic and environmental mechanisms seem to contribute to a moderate proportion of variability of CIMT(31). We observed an association between CIMT and aortic arch plaques that was independent of vascular risk factors, indicating that common underlying atherosclerotic mechanism may exist in the formation of both lesions that may not be completely explained by traditional vascular risk factors.
Ethnic differences may also play a role in atherogenesis. Increased CIMT and attenuated endothelium dependent vasodilation have been described in African-American subjects compared with Caucasians(32). Conversely, environmental factors may contribute to different prevalence of precursors of atherosclerosis even in subjects of similar ethnicity(33). Our study showed an association between CIMT and aortic atherosclerosis in a multiethnic cohort living in the same geographic area and therefore with similar environmental exposures, reinforcing the role of CIMT as a marker of early atherosclerosis in subjects of different ethnicities.
Our study has several limitations. We did not assess carotid distensibility, whose combination with CIMT increased the negative predictive value for significant aortic atherosclerosis in the study of Harloff et al.(15). However, CIMT, rather than distensibility, was the only variable significantly associated with aortic wall thickness in that study(14), suggesting its predominant role in the prediction of aortic plaque. Also, the relatively small sample size prevented a separate analysis of the relationship between CIMT and aortic arch plaques in different race/ethnic subgroups.
In conclusion, our data showed a significant association between CIMT at the bifurcation and severe aortic arch atherosclerosis. Although its positive predictive value for large aortic plaques is limited, CIMT at the bifurcation can reliably exclude the presence of such plaques in the majority of patients, and could therefore be used as a screening tool in asymptomatic subjects at intermediate cardiovascular risk.
Acknowledgments
The study was supported by R01 NS36286 from the National Institute of Neurological Disorders and Stroke (NINDS). Dr. Marco Di Tullio was the recipient of a NINDS Mid-Career Award in Patient-Oriented Research (K24 NS02241).
The Authors wish to thank Inna Titova, MPH, and Gabrielle Gaspard, MPH, for their assistance in the collection of the data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 2.Kallikazaros IE, Tsioufis CP, Stefanadis CI, Pitsavos CE, Toutouzas PK. Closed relation between carotid and ascending aortic atherosclerosis in cardiac patients. Circulation. 2000;102:III263–III268. doi: 10.1161/01.cir.102.suppl_3.iii-263. [DOI] [PubMed] [Google Scholar]
- 3.Rohani M, Jogestrand T, Ekberg M, van der LJ, Kallner G, Jussila R, et al. Interrelation between the extent of atherosclerosis in the thoracic aorta, carotid intima-media thickness and the extent of coronary artery disease. Atherosclerosis. 2005;179:311–316. doi: 10.1016/j.atherosclerosis.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Kitagawa K, Hougaku H, Yamagami H, Hashimoto H, Itoh T, Shimizu Y, et al. Carotid intima-media thickness and risk of cardiovascular events in high-risk patients. Results of the Osaka Follow-Up Study for Carotid Atherosclerosis 2 (OSACA2 Study) Cerebrovasc Dis. 2007;24:35–42. doi: 10.1159/000103114. [DOI] [PubMed] [Google Scholar]
- 5.Ebrahim S, Papacosta O, Whincup P, Wannamethee G, Walker M, Nicolaides AN, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: the British Regional Heart Study. Stroke. 1999;30:841–850. doi: 10.1161/01.str.30.4.841. [DOI] [PubMed] [Google Scholar]
- 6.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 7.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 8.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Hurst RT, Ng DW, Kendall C, Khandheria B. Clinical use of carotid intima-media thickness: review of the literature. J Am Soc Echocardiogr. 2007;20:907–914. doi: 10.1016/j.echo.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 10.Couturier G, Voustaniouk A, Weinberger J, Fuster V. Correlation between coronary artery disease and aortic arch plaque thickness measured by non-invasive B-mode ultrasonography. Atherosclerosis. 2006;185:159–164. doi: 10.1016/j.atherosclerosis.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 11.Amarenco P, Cohen A, Tzourio C, Bertrand B, Hommel M, Besson G, et al. Atherosclerotic disease of the aortic arch and the risk of ischemic stroke. N Engl J Med. 1994;331:1474–1479. doi: 10.1056/NEJM199412013312202. [DOI] [PubMed] [Google Scholar]
- 12.Di Tullio MR, Sacco RL, Gersony D, Nayak H, Weslow RG, Kargman DE, et al. Aortic atheromas and acute ischemic stroke: a transesophageal echocardiographic study in an ethnically mixed population. Neurology. 1996;46:1560–1566. doi: 10.1212/wnl.46.6.1560. [DOI] [PubMed] [Google Scholar]
- 13.Atherosclerotic disease of the aortic arch as a risk factor for recurrent ischemic stroke. The French Study of Aortic Plaques in Stroke Group. N Engl J Med. 1996;334:1216–1221. doi: 10.1056/NEJM199605093341902. [DOI] [PubMed] [Google Scholar]
- 14.Fujimoto S, Yasaka M, Otsubo R, Oe H, Nagatsuka K, Minematsu K. Aortic arch atherosclerotic lesions and the recurrence of ischemic stroke. Stroke. 2004;35:1426–1429. doi: 10.1161/01.STR.0000127788.32550.d4. [DOI] [PubMed] [Google Scholar]
- 15.Harloff A, Strecker C, Reinhard M, Kollum M, Handke M, Olschewski M, et al. Combined measurement of carotid stiffness and intima-media thickness improves prediction of complex aortic plaques in patients with ischemic stroke. Stroke. 2006;37:2708–2712. doi: 10.1161/01.STR.0000244763.19013.dc. [DOI] [PubMed] [Google Scholar]
- 16.Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study Stroke. 1995;26:14–20. doi: 10.1161/01.str.26.1.14. [DOI] [PubMed] [Google Scholar]
- 17.Gentry EM, Kalsbeek WD, Hogelin GC, Jones JT, Gaines KL, Forman MR, et al. The behavioral risk factor surveys: II. Design, methods, and estimates from combined state data. Am J Prev Med. 1985;1:9–14. [PubMed] [Google Scholar]
- 18.Di Tullio MR, Sacco RL, Homma S. Ultrasound examination of the aortic arch in stroke. In: Welch M, Caplan LR, Reis D, Siesjo B, Weir B, editors. Primer on cerebrovascular diseases. Academic Press; 1997. pp. 628–634. [Google Scholar]
- 19.Heiss G, Sharrett AR, Barnes R, Chambless LE, Szklo M, Alzola C. Carotid atherosclerosis measured by B-mode ultrasound in populations: associations with cardiovascular risk factors in the ARIC study. Am J Epidemiol. 1991;134:250–256. doi: 10.1093/oxfordjournals.aje.a116078. [DOI] [PubMed] [Google Scholar]
- 20.Rundek T, Elkind MS, Pittman J, Boden-Albala B, Martin S, Humphries SE, et al. Carotid intima-media thickness is associated with allelic variants of stromelysin-1, interleukin-6, and hepatic lipase genes: the Northern Manhattan Prospective Cohort Study. Stroke. 2002;33:1420–1423. doi: 10.1161/01.STR.0000015558.63492.B6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Touboul PJ, Prati P, Scarabin PY, Adrai V, Thibout E, Ducimetiere P. Use of monitoring software to improve the measurement of carotid wall thickness by B-mode imaging. J Hypertens Suppl. 1992;10:S37–S41. [PubMed] [Google Scholar]
- 22.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 23.van der LJ, Hadjinikolaou L, Bergman P, Lindblom D. Postoperative stroke in cardiac surgery is related to the location and extent of atherosclerotic disease in the ascending aorta. J Am Coll Cardiol. 2001;38:131–135. doi: 10.1016/s0735-1097(01)01328-6. [DOI] [PubMed] [Google Scholar]
- 24.Doty JR, Wilentz RE, Salazar JD, Hruban RH, Cameron DE. Atheroembolism in cardiac surgery. Ann Thorac Surg. 2003;75:1221–1226. doi: 10.1016/s0003-4975(02)04712-4. [DOI] [PubMed] [Google Scholar]
- 25.Karalis DG, Quinn V, Victor MF, Ross JJ, Polansky M, Spratt KA, et al. Risk of catheter-related emboli in patients with atherosclerotic debris in the thoracic aorta. Am Heart J. 1996;131:1149–1155. doi: 10.1016/s0002-8703(96)90090-3. [DOI] [PubMed] [Google Scholar]
- 26.Keeley EC, Grines CL. Scraping of aortic debris by coronary guiding catheters: a prospective evaluation of 1,000 cases. J Am Coll Cardiol. 1998;32:1861–1865. doi: 10.1016/s0735-1097(98)00497-5. [DOI] [PubMed] [Google Scholar]
- 27.Lorenz MW, von KS, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS) Stroke. 2006;37:87–92. doi: 10.1161/01.STR.0000196964.24024.ea. [DOI] [PubMed] [Google Scholar]
- 28.Kathiresan S, Larson MG, Keyes MJ, Polak JF, Wolf PA, D’Agostino RB, et al. Assessment by cardiovascular magnetic resonance, electron beam computed tomography, and carotid ultrasonography of the distribution of subclinical atherosclerosis across Framingham risk strata. Am J Cardiol. 2007;99:310–314. doi: 10.1016/j.amjcard.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 29.Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, et al. Prevention Conference V: Beyond secondary prevention: identifying the high-risk patient for primary prevention: noninvasive tests of atherosclerotic burden: Writing Group III. Circulation. 2000;101:E16–E22. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 30.Ranjit N, ez-Roux AV, Chambless L, Jacobs DR, Jr, Nieto FJ, Szklo M. Socioeconomic differences in progression of carotid intima-media thickness in the Atherosclerosis Risk in Communities study. Arterioscler Thromb Vasc Biol. 2006;26:411–416. doi: 10.1161/01.ATV.0000198245.16342.3d. [DOI] [PubMed] [Google Scholar]
- 31.Juo SH, Rundek T, Lin HF, Cheng R, Lan MY, Huang JS, et al. Heritability of carotid artery distensibility in Hispanics: the Northern Manhattan Family Study. Stroke. 2005;36:2357–2361. doi: 10.1161/01.STR.0000185926.05011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lip GY, Boos CJ. Ethnic differences in arterial responses, inflammation, and metabolic profiles: possible insights into ethnic differences in cardiovascular disease and stroke. Arterioscler Thromb Vasc Biol. 2005;25:2240–2242. doi: 10.1161/01.ATV.0000188507.89134.ef. [DOI] [PubMed] [Google Scholar]
- 33.Kalra L, Iveson E, Rambaran C, Sherwood R, Chowienczyk P, Ritter J, et al. An international matched cohort study of the contribution of metabolic impairments to subclinical atherosclerosis in United Kingdom and Jamaican African-Caribbeans. Atherosclerosis. 2008;199:95–101. doi: 10.1016/j.atherosclerosis.2007.10.013. [DOI] [PubMed] [Google Scholar]