Abstract
This study aimed to investigate prevalence of asymptomatic carotid artery stenosis (ACAS) in Korean patients with peripheral arterial disease (PAD) and identify predictive factors of ACAS in patients with PAD. Between 1994 and 2008, 546 patients who underwent bypass surgery due to PAD were identified in a single tertiary teaching hospital. Of those, 409 patients underwent preoperative screening carotid duplex ultrasonography (CDUS). Patients who had an episode of cerebrovascular event or previous carotid artery intervention were excluded and then a retrospective analysis was made of 340 patients. The degree of internal carotid artery (ICA) stenosis was determined by the criteria of Society of Radiologists in Ultrasound Consensus Conference. To determine the risk factors of ACAS, demographic, coexisting medical condition and lesion characteristics were tested with binary logistic regression model. The prevalence of ≥70% ICA stenosis was 14%. ICA occlusion was detected in 7.1%. Multivariate analysis revealed age >65 yr (OR: 2.610, 95% CI: 1.197-5.691) and coronary artery disease (CAD, OR: 2.333, 95% CI: 1.169-4.657) are predictive factors of ≥70% stenosis. A PAD patient who needs revascularization, particularly, >65 yr or has a concomitant CAD, can be a good candidate of screening CDUS.
Keywords: Duplex ultrasonography, Peripheral Vascular Diseases, Carotid Stenosis
INTRODUCTION
Cerebrovascular disease is the third leading cause of death in the United States (1) and the second leading cause in Korea (2). Approximately 88% of strokes are ischemic and about 20% of these originate from large artery stenosis (3, 4). To prevent ischemic stroke, carotid endarterectomy has been recommended for asymptomatic patients with severe carotid stenosis based on evidence from multicenter prospective randomized trials (5-8).
Carotid duplex ultrasonography (CDUS) is an accuracy-proven non-invasive diagnostic examination to detect asymptomatic carotid artery stenosis (ACAS). However, for the general population, CDUS has a limited role in screening of carotid disease because of a low overall prevalence of clinically relevant disease (9). Because coronary artery disease (CAD), cerebrovascular disease (CVD) and peripheral arterial disease (PAD) originate from atherosclerosis, these three diseases occasionally exist together (10). Therefore, screening CDUS may be useful for those populations. Several previous studies reported that the prevalence of ACAS was relatively high in PAD patients and the authors recommended routine CDUS (11, 12). For those with known transient ischemic attack or stroke within 6 months who are symptomatic should also perform CDUS. However, a generalized screening in PAD patients is controversial and the cost-effectiveness remains to be demonstrated.
In Korea, the prevalence of ACAS in PAD patients has not yet been reported. In this study, we attempted to investigate prevalence of ACAS in patients who underwent bypass surgery due to chronic lower extremity ischemia and identify predictive factors of ACAS.
MATERIALS AND METHODS
Between April 1996 and December 2008, 546 patients underwent one or more than one arterial bypass surgeries due to chronic atherosclerotic lower extremity ischemia. Among them, 409 patients underwent preoperative screening CDUS. Patients were excluded if they had a history of cerebrovascular symptoms or previous carotid surgery irrespective of time of incidence. Excluding 69 patients who had a previous history of stroke (n=61) or carotid artery intervention (n=8, 5 carotid endarterectomies and 3 carotid stentings), 340 neurologically asymptomatic patients were enrolled in this study. Medical records and findings of CDUS were retrospectively reviewed.
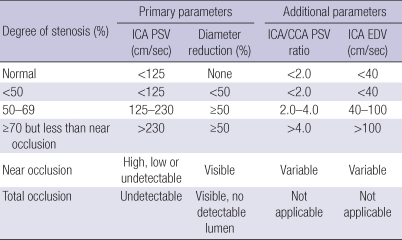
Duplex scan was performed by three registered vascular technologists. Duplex imaging included common carotid artery, internal carotid artery (ICA), external carotid artery and vertebral artery. Through gray-scale imaging and spectral Doppler waveform analysis, diameter reduction rate, peak systolic velocity and end diastolic velocity were measured. Degree of ICA stenosis was defined by the criteria of Society of Radiologists in Ultrasound Consensus Conference (Table 1). ICA stenosis ≥70% was regarded as critical stenosis. When both carotid arteries were diseased, the more stenotic site was used for statistical analysis.
Table 1.
Duplex ultrasonography criteria for diagnosis of ICA stenosis (13)
ICA, internal carotid artery; CCA, common carotid artery; PSV, peak systolic velocity; EDV, end diastolic velocity.
To identify risk factors of an asymptomatic critical ICA stenosis in PAD patients, univariate analysis and multivariate analysis with binary logistic regression model were conducted using patient demographic (age, gender) and clinical variables (smoking, hypertension, diabetes mellitus, coronary artery disease, chronic renal insufficiency, hypercholesterolemia, claudication vs. critical limb ischemia).
RESULTS
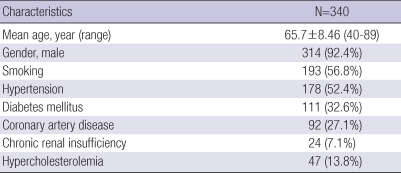
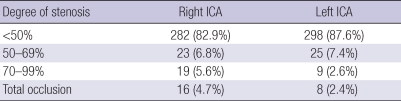
Table 2 demonstrates patient demographic and clinical data. Mean age of the patients was 65.7 yr, ranging from 40 to 89 yr. 92.4% were males. One hundred fifty (44.1%) patients presented with infrainguinal arterial disease, 116 patients (34.1%) showed aorto-iliac disease and 74 patients (21.8%) had combined lesions. Indications for treatment included claudication (72.1%) and critical limb ischemia (27.9%) due to atherosclerotic PAD. Concomitant carotid disease according to the severity of stenosis is shown in Table 3.
Table 2.
Patient demographic and clinical data
Table 3.
Degree of internal carotid artery (ICA) stenosis (N=340 patients)
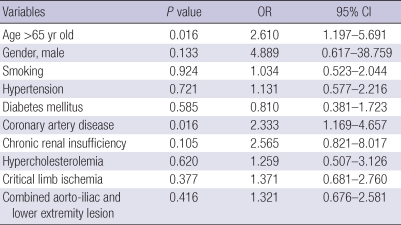
On univariate analysis, a critical ICA stenosis was more common in old-age patients (>65 yr old, P=0.013) and in patients with coronary artery disease (P=0.010). With regard to gender, smoking, hypertension, diabetes mellitus, chronic renal insufficiency, hypercholesterolemia, critical limb ischemia, location of lesion, there were no differences between patients with a significant stenosis and those without.
By multivariate analysis, the risk factors of a critical ICA stenosis of patients with PAD were age >65 (OR: 2.610, 95% CI: 1.197-5.691) and coronary artery disease (OR: 2.333, 95% CI: 1.169-4.657) (Table 4).
Table 4.
Multivariate analysis of risk factor of critical (>70%) asymptomatic carotid artery stenosis in patients with chronic lower extremity ischemia
OR, odds ratio; CI, confidence interval.
DISCUSSION
Although CDUS is the best non-invasive modality for screening of ACAS, previous studies failed to prove the benefit of screening CDUS in general population on cost-benefit analysis (14, 15).
There are no known data regarding the prevalence of ACAS in patients with PAD. A meta-analysis of 19 studies showed high prevalence of asymptomatic carotid artery stenosis exists in patients with PAD (16). A prevalence of >70% ACAS was 14% and the authors suggested targeting PAD patients rather than a healthy population if routine screening is performed. In terms of risk factors of ACAS, Gentile et al. (11) reported that carotid bruit and rest pain were risk factors of ≥50% stenosis and Marek et al. (12) announced that age >65 yr, ankle-brachial index <0.7 and carotid bruit were associated with ≥50% stenosis.
In this study, we obtained similar results with ≥70% stenosis or occlusion being evident in 13.8%. The risk factors of ACAS were old age (>65 yr old) and CAD. But, other atherosclerotic risk factors, such as smoking, hypertension, diabetes mellitusand hypercholesterolemia were not associated with the presence of ACAS.
In the Reduction of Atherothrombosis for Continued Health (REACH) Registry, the incidence of one-year cardiovascular events in PAD patients was higher than it is in CAD or CVD patients (17). One-year cardiovascular death, myocardial infarction or stroke rate was 5.35% for PAD patients and nonfatal stroke rate was 1.92%. Carotid endarterectomy or carotid stenting were performed for 1.53% of PAD patients within 1 yr. Sprengers et al. (18) reported that 120 events (27% nonfatal myocardial infarction, 27% nonfatal stroke, and 52% mortality from vascular cause) occurred in 800 PAD patients during a mean follow-up of 4.7 yr.
A preoperative screening CDUS provides important information of ACAS. CDUS can enable surgeons to select patients who are at high risk of stroke and offers an opportunity of more intensive management of carotid disease. Consequently it provides a better quality of life and a longer life.
Cerebral ischemia is one of the disastrous perioperative complications. Patients who have bilateral or critical carotid stenosis are vulnerable to hypotension and an episode of hypotension during operation may cause cerebral ischemic infarction in these patients. There is also a hidden risk of cerebral embolism during the placement of central venous catheter before surgery. Mispuncture of diseased carotid artery might produce free emboli which induce severe cerebral infarction. Therefore, more attention is needed for the patients with ACAS during central venous access. Moreover, if these neurologic complications occur in absence of preoperative evaluation of carotid artery disease, they might induce a legal problem of surgeon's negligence.
In summary, our results showed the prevalence of ACAS in Korean patients with chronic atherosclerotic lower extremity ischemia is as high as reported in Western countries. ACAS was more common in a patient who is older than 65 yr old or has concomitant CAD. Therefore, preoperative CDUS is a useful screening tool to detect ACAS and to assess perioperative risk of cerebrovascular complications in PAD patients who undergo revascularization, particularly, in patients who are older than 65 yr or have a concomitant CAD.
The major limitation of this study is a retrospective design. And this study did not include patients who underwent endovascular treatment or medical treatment because screening CDUS was not routinely performed for those patients. Further prospective study including all PAD patients is necessary.
References
- 1.Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O'Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Jr, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Lee WY, Bae HJ. Models and actual status of stroke unit services in developed countries. J Korean Neurol Assoc. 2009;27:195–205. [Google Scholar]
- 3.Ergin A, Muntner P, Sherwin R, He J. Secular trends in cardiovascular disease mortality, incidence, and case fatality rates in adults in the United States. Am J Med. 2004;117:219–227. doi: 10.1016/j.amjmed.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Petty GW, Brown RD, Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513–2516. doi: 10.1161/01.str.30.12.2513. [DOI] [PubMed] [Google Scholar]
- 5.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995;273:1421–1428. [PubMed] [Google Scholar]
- 6.Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, Thomas D. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004;363:1491–1502. doi: 10.1016/S0140-6736(04)16146-1. [DOI] [PubMed] [Google Scholar]
- 7.Hobson RW, 2nd, Mackey WC, Ascher E, Murad MH, Calligaro KD, Comerota AJ, Montori VM, Eskandari MK, Massop DW, Bush RL, Lal BK, Perler BA. Management of atherosclerotic carotid artery disease: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2008;48:480–486. doi: 10.1016/j.jvs.2008.05.036. [DOI] [PubMed] [Google Scholar]
- 8.Liapis CD, Bell PR, Mikhailidis D, Sivenius J, Nicolaides A, Fernandes e Fernandes J, Biasi G, Norgren L. ESVS guidelines. Invasive treatment for carotid stenosis: indications, techniques. Eur J Vasc Endovasc Surg. 2009;37(4 Suppl):1–19. doi: 10.1016/j.ejvs.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Wolff T, Guirguis-Blake J, Miller T, Gillespie M, Harris R. Screening for carotid artery stenosis: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2007;147:860–870. doi: 10.7326/0003-4819-147-12-200712180-00006. [DOI] [PubMed] [Google Scholar]
- 10.Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Rother J, Wilson PW. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295:180–189. doi: 10.1001/jama.295.2.180. [DOI] [PubMed] [Google Scholar]
- 11.Gentile AT, Taylor LM, Jr, Moneta GL, Porter JM. Prevalence of asymptomatic carotid stenosis in patients undergoing infrainguinal bypass surgery. Arch Surg. 1995;130:900–904. doi: 10.1001/archsurg.1995.01430080102016. [DOI] [PubMed] [Google Scholar]
- 12.Marek J, Mills JL, Harvich J, Cui H, Fujitani RM. Utility of routine carotid duplex screening in patients who have claudication. J Vasc Surg. 1996;24:572–577. doi: 10.1016/s0741-5214(96)70072-1. [DOI] [PubMed] [Google Scholar]
- 13.Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, Carroll BA, Eliasziw M, Gocke J, Hertzberg BS, Katanick S, Needleman L, Pellerito J, Polak JF, Rholl KS, Wooster DL, Zierler RE. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003;229:340–346. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- 14.Colgan MP, Strode GR, Sommer JD, Gibbs JL, Sumner DS. Prevalence of asymptomatic carotid disease: results of duplex scanning in 348 unselected volunteers. J Vasc Surg. 1988;8:674–678. doi: 10.1067/mva.1988.avs0080674. [DOI] [PubMed] [Google Scholar]
- 15.Longstreth WT, Jr, Shemanski L, Lefkowitz D, O'Leary DH, Polak JF, Wolfson SK., Jr Asymptomatic internal carotid artery stenosis defined by ultrasound and the risk of subsequent stroke in the elderly. The Cardiovascular Health Study. Stroke. 1998;29:2371–2376. doi: 10.1161/01.str.29.11.2371. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed B, Al-Khaffaf H. Prevalence of significant asymptomatic carotid artery disease in patients with peripheral vascular disease: a meta-analysis. Eur J Vasc Endovasc Surg. 2009;37:262–271. doi: 10.1016/j.ejvs.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Steg PG, Bhatt DL, Wilson PW, D'Agostino R, Sr, Ohman EM, Rother J, Liau CS, Hirsch AT, Mas JL, Ikeda Y, Pencina MJ, Goto S. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–1206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
- 18.Sprengers RW, Janssen KJ, Moll FL, Verhaar MC, van der Graaf Y. Prediction rule for cardiovascular events and mortality in peripheral arterial disease patients: Data from the prospective Second Manifestations of ARTerial disease (SMART) cohort study. J Vasc Surg. 2009;50:1369–1376. doi: 10.1016/j.jvs.2009.07.095. [DOI] [PubMed] [Google Scholar]