Abstract
Purpose
To evaluate the effect of intravitreal triamcinolone acetonide (IVT) reinjection on clinical and optical coherence tomographic features in refractory diabetic macular edema.
Methods
In a prospective interventional case series, all IVT treated patients enrolled in a previous clinical trial were recalled to have a new ophthalmologic examination and optical coherence tomography (OCT) performed. Eyes found suitable for reinjection received 4 mg IVT. Complete clinical examination and OCT were repeated at 2 and 4 months post-injection. The changes were statistically analyzed using a paired t test and were compared to the results of the first injections.
Results
Of all returning patients, 12 cases with complete records were considered candidates for reinjection. Visual acuity (VA) changes were not significant after the first and second interventions, although there was a relative improvement (0.14 logMAR) 2 months after the first injection. Reductions of central macular thickness (CMT) were 43±69 µm, and 40±69 µm after the first injection and 27±48 µm, 49±58 µm after the reinjection at 2 & 4 months, respectively. None of the mentioned changes was significant. After the second injection, however, intraocular pressure was elevated at both 2 & 4 months (3.6 & 2.4 mmHg respectively, P<0.05). Two months after the first administration, intraocular pressure was found to be raised significantly (5.58 mmHg, P=0.001).
Conclusions
The transient beneficial effects of IVT on diabetic macular edema are not repeated with second injections. However, IVT-related ocular hypertension is more persistent after reinjection.
Keywords: Diabetic macular edema, Intravitreal triamcinolone, Intraocular pressure, Macular thickness, Reinjection
Macular edema is the most important manifestation of non-proliferative diabetic retinopathy and a predominant cause of legal blindness in diabetic patients. According to the early treatment of diabetic retinopathy study (ETDRS), the treatment of choice for clinically significant macular edema (CSME) is laser therapy. However, some cases of CSME are refractory to laser therapy and do not have a good prognosis with such treatment.1
Recently, some promising results have been shown in different studies for the treatment of refractory diabetic macular edema with intravitreal triamcinolone acetonide (IVT).2-5 However, the follow-up periods in these studies were rather short and there were only limited reports concerning reinjection in these cases.
There is the possibility of a poor and/or transient response to the first administration, which would therefore require repeated injections. We performed a study on patients with diabetic macular edema who had already received one IVT injection. The purpose of this study was to discern both the long-term result of IVT in diabetic macular edema and, more importantly, the effect of reinjection on the eyes that were not completely improved.
Materials and Methods
In a prospective, interventional case series study, all of the patients in the treated group of a previous clinical trial who received one dose of 4 mg IVT for refractory diabetic macular edema were recalled for reexamination and reassessment of macular thickness by optical coherence tomography (OCT-2, Zeiss, Dublin, CA) about 10 months after their first injections. Both the primary trial and this part of the study were approved by the Review Board/Ethics Committee of the Ophthalmic Research Center.
The previous study included eyes meeting criteria for CSME based on the ETDRS definition, with an anticipated unfavorable visual outcome after initial or supplemental macular photocoagulation due to one or more of the following findings: 1- macular ischemia, 2- visual acuity (VA) ≤20/200, 3- diffuse macular edema, 4- severe hard exudates (HE) accumulation in the fovea, and 5- lack of response to previous laser photocoagulations with the last one being more than 3 months before. The patients were randomly assigned to the treatment (4 mg IVT) and placebo groups.
In the current study, all of the IVT-received patients in the initial part were recalled for a new clinical and tomographic evaluation. IVT reinjection was planned for all patients except for those who met the following criteria: (1) history of intraocular pressure (IOP) more than 30 mmHg after the first injection, (2) intraocular operation after the first injection, (3) VA ≥20/50, (4) IOP >21 mmHg and/or taking antiglaucoma medication at the time of reexamination, (5) lens opacity severe enough to interfere with visual acuity testing and performing OCT, (6) central macular thickness (CMT) less than 200 µm measured by OCT, (7) being candidate for intraocular surgery, (8) one-eyed patients, and (9) Non-compliance.
Injections were done under sterile conditions in the operating room with topical anesthesia and insertion of a lid speculum. Four milligrams (0.1 cc) triamcinolone acetonide (Kenacort) was injected intravitreally with a 27-gauge needle through the superotemporal quadrant. IOP was checked about 10 minutes after injection with a Goldman applanation tonometer and anterior chamber paracentesis was performed if IOP exceeded 30 mmHg.
Examinations were performed at 2 and 4 weeks after injection to monitor IOP and complications. In eyes with IOP >21 mmHg, timolol was prescribed twice daily, and in refractory cases, one drop of dorzolamide three times a day was added.
Complete ophthalmic examination and OCT were repeated 2 and 4 months after the second injections in an attempt to replicate the follow-up periods after the primary injections in the first part of the study.
Statistical analysis was performed using paired t and independent sample t tests for evaluating quantitative variable changes within and between injections, respectively. P values <0.05 were considered statistically significant. Data were analyzed using SPSS 11.5.
Results
The results are presented in two parts: first, the long-term follow-up results comparing the findings of the new exams with the previous data, and second, the results of intravitreal triamcinolone reinjection in cases who met the criteria for this intervention.
Of 45 patients who were in the treated group of the first part of the study, 23 (14 male, 9 female) returned for reevaluation. To asses whether these 23 patients could represent all of the cases, their previous data were compared with those of the remaining 22 patients who did not return for new examination. In this manner, it was confirmed that there was no significant difference in the effect of IVT in the first part of the study with respect to VA, CMT, and IOP between these two groups of patients (data are not shown).
1. Long-term follow up results
The mean time interval between the first injection and the new examination was 10.87±2.1 months (range: 8 to 18 months).
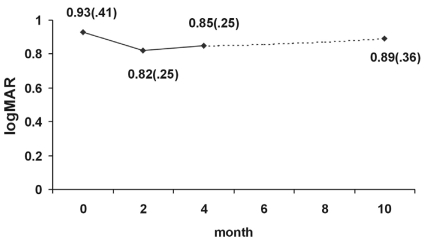
The comparison of VA changes between the new exam and each previous one (at months 0, 2, and 4 after the first injection) were not statistically significant. Fig. 1 demonstrates that VA remained relatively stable during 10 months of follow up. However, a transient but statistically insignificant improvement occurred by 2 months after the injection.
Fig. 1.
Mean visual acuity (SD) before, 2, 4 and about 10 months after the first intravitreal triamcinolone injection.
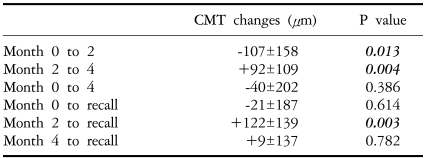
The assessment of CMT between the early phases and the time of recall are presented in Table 1. Paired t test shows statistically significant changes between months 0 and 2, months 2 and 4, and month 2 and the time of recall. Fig. 2 shows a transient reduction of CMT which occurred at 2 months post-injection and a steady thickness level from month 4 until month 10.
Table 1.
Changes of central macular thickness (CMT) between months 0, 2, 4, and the time of recall (paired t test)
+ & - Signs imply increase and decrease in CMT, respectively.
Fig. 2.
Mean central macular thickness before, 2, 4 and about 10 months after the first intravitreal triamcinolone injection.
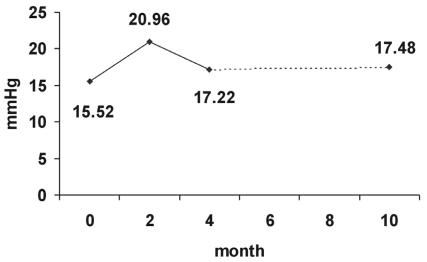
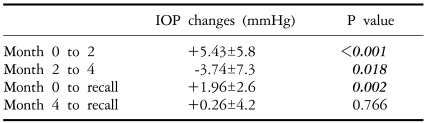
After a rise at 2 months, IOP decreased toward the normal level but did not return to its preinjection level (Fig 3). Comparison of the means of IOP (Table 2) confirmed the presence of a significant difference between IOP at 10 months post-injection compared to pre-injection levels (P=0.002).
Fig. 3.
Mean intraocular pressure before, 2, 4 and about 10 months after the first intravitreal triamcinolone injection.
Table 2.
Changes of intraocular pressure (IOP) between months 0, 2, 4, and the time of recall (paired t test)
+ & - Signs imply increase and decrease in IOP, respectively.
2. Results of reinjection
Eight of 23 returned cases (34.8%) were not candidates for reinjection of IVT for the following reasons: history of IOP >30 mmHg after the first injection, VA >20/50, IOP >20 mmHg, vitreous hemorrhage (two cases), and CMT <200 µm Another patient developed ocular hypertension after the firstintervention which persisted and necessitated long-term antiglaucoma medication. Non-compliance was the cause of the last excluded case.
Fifteen patients received reinjection of IVT without significant complications. Two of them were lost to follow-up and one was excluded because of cataract progression. Therefore, statistical analyses were performed on 12 eyes.
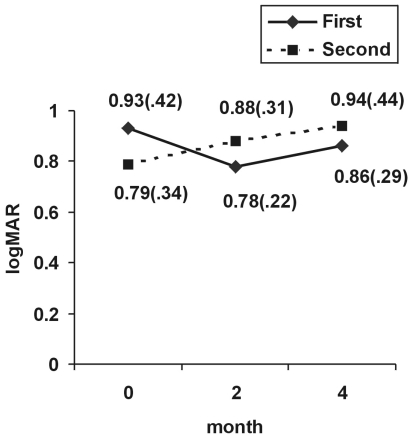
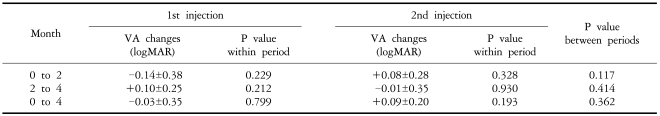
Evaluation of VA differences between the first and the second injection is shown in Fig. 4. Pretreatment visual acuity of the second intervention was better than that of the first, but these findings were not statistically significant (P=0.40). Although the comparisons of VA changes between and within the two injections did not show a statistically significant difference (Table 3), its improvement (0.14 logMAR) at 2 months following the first injection was not repeated after the second one.
Fig. 4.
Visual acuity changes (SD) after the first and the second injections.
Table 3.
Visual acuity (VA) changes following the first and the second IVT injections in a group of cases with diabetic macular edema (paired t and independent sample t tests for changes within and between periods, respectively).
+ & - Signs imply increase and decrease in logMAR notation that means decrease and increase in VA, respectively.
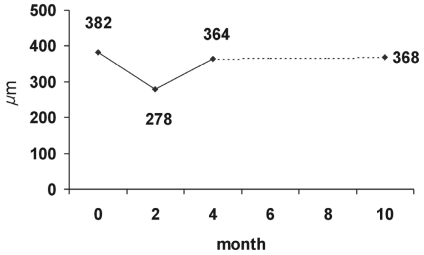
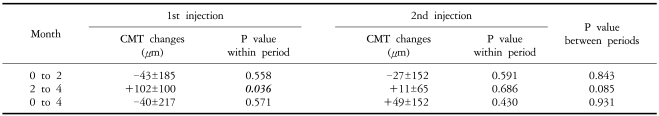
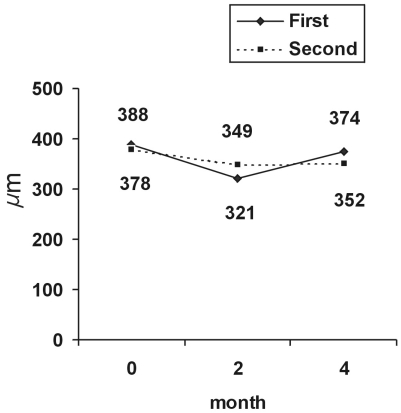
Baseline CMT was 388 and 378 microns before the first and the second injections respectively (P=0.89). Although not statistically significant, mean CMT reduction after the primary injection (43 µm) was greater than that of the reinjection (27 µm). Comparisons of thickness variations within and between the two injections did not show a significant difference except in one stage. As shown in Table 4, the thickness changes between 2 and 4 months following the first injection was significant (102 µm, P=0.036), which confirmed the reduction of IVT effect. Fig. 5 represents similar responses of macular thickness to each injection.
Table 4.
Central macular thickness (CMT) changes following the first and the second IVT injections in a particular group of cases with diabetic macular edema (paired t and independent sample t tests for changes within and between periods, respectively)
+ & - Signs imply increase and decrease in CMT, respectively.
Fig. 5.
Central macular thickness changes after the first and the second injections.
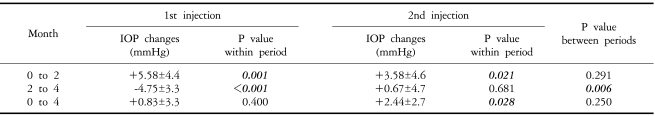
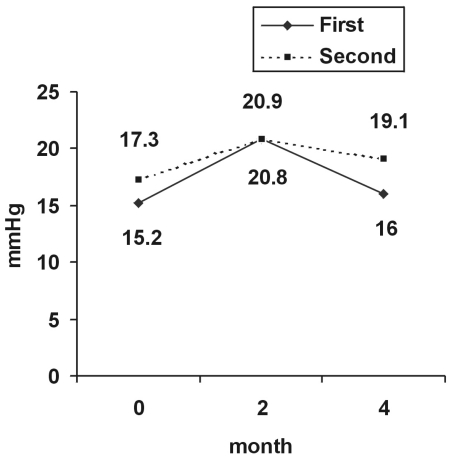
Mean initial IOP before the second injection was higher than that of the first one (P=0.037). Table 5 indicates that IOP rise after the first intervention (5.58 mmHg) was greater than that following the reinjection (3.58 mmHg); however, it persisted longer after the repeated injection (Fig. 6). The IOP changes between months 2 and 4 were -4.75 and +0.66 mmHg after the first and the second injections, respectively, and showed significant difference (P=0.006).
Table 5.
Intraocular pressure (IOP) changes following the first and the second IVT injections in a group of cases with diabetic macular edema (paired t and independent sample t tests for changes within and between periods, respectively).
+ & - Signs imply increase and decrease in IOP, respectively.
Fig. 6.
Intraocular pressure changes after the first and the second njections.
Discussion
According to the results, one can reach the following conclusions:
In diabetic patients, the first IVT injection induces relative VA improvement and macular thickness reduction at 2 months. These variables return to their initial levels by 4 months and thereafter remain stable until month 10.
The second IVT injection is not as effective as the first one.
Significant increase of IOP at month 2 normalizes by month 4 but does not return to its previous level even after 10 months of follow up.
IOP rise after reinjection is more refractory to treatment and does not decrease as rapidly as after the first administration.
Only about half of the patients returned for reevaluation. This would raise the possibility of a selection bias in this study. The reason for seeking additional medical care could imply that these patients were either good or poor responders to the primary IVT injection. To evaluate this possibility, we compared their previous data and it was shown that both returned and unreturned patients had similar responses to the primary IVT.
The long-term effect of IVT on diabetic macular edema is not well known. The mean follow up duration in the Jonas et al.6 study was 13.2±6.0 months. However, the records were completed for only 7 and 5 patients until 10 and 12 months, respectively. In their study, following the injection of 20-25 mg IVT, visual acuities reached a plateau level at 1-7 months and returned to initial levels after 8-9 months. The authors stated that there was a 7 to 8-month effect time for mega dose IVT in the management of diabetic macular edema. Two-line improvement of VA by months 5 and 7 in 40% and 54% of the eyes respectively were significant.2,7 The longer drug effect in these two study groups (6 and 7 months) in relation to that of ours may be the result of the higher drug dosage.
Similar to our study, Martidis3 and Ciardella4 showed that the maximum effect of 4 mg IVT on macular thickness occurred between 1 to 3 months. Due to recurrences, a few cases in these two studies received repeated injection.
Ocular hypertension is a familiar complication of IVT. However, before this study, the persistence of pressure above its initial level up to 10 months after injection had not been shown. In a few studies, the percentage of patients who developed IVT-related ocular hypertension were reported, but no comparison was performed between the first and the last mean IOP.3,5 Martidis el al.3 showed a 1.9-mmHg rise of the mean IOP in 8 patients for 6 months, which was comparable to the 1.96 mmHg in 23 cases of our study. Significant persistence of ocular hypertension for 5 and 6 months was also stated in two articles by Jonas.2,7 According to another of studies which was comparable to ours, the elevation of IOP was significant at 3 months and took 8-9 months to return to its previous level.8 In all mentioned studies, the reported means of IOP at each visit and the calculated time for their elevations were in spite of taking antiglaucoma medication. As with our findings, these studies stressed the long term effect of IVT on IOP.
We are unaware of any study that has been published with the stated purpose of evaluating the effect of IVT reinjection in diabetic macular edema. Three patients in the Martidis' et al.3 study received repeated injection, but the results were not reported.
In Ciardella's4 study, the second injection of IVT was performed for 12 eyes with 2- to 11-month (mean 5.7±2.6) intervals between the two injections. Mean VA increased form 0.27±0.15 to 0.42±0.25 one month after the reinjection. Mean macular thickness reduced from 463±115 µm to 213±63 µm. However, it was not stated whether this amount of reduction was specific to these 12 eyes or not.
To our knowledge, our study was the first report regarding the results of two IVT injections that were performed using the same time intervals for cases with diabetic macular edema. In this study, the changes of VA, CMT, and IOP after the second injection were compared to the changes of these variables that occurred in the same eyes within similar phases after the first injection.
According to the present study and other published data, the therapeutic effect of IVT does not last for 10 months. Therefore, we may conclude that the changes after the reinjection are independent of the long-lasting effect of primary IVT. To confirm this assumption, we refer to Beer's9 article in which the measurable amount of triamcinolone in non-vitrectomized eyes was found until 93±28 days after injection. It should be noticed, however, that there is a report about the persistence of IVT after 1.5 years, but this occurred following 20-25 mg of drug injection.10
Initial mean VA in our 12 eyes before the primary injection (0.93 logMAR) was lower than that before the secondary injection (0.79 logMAR). This might be the reason for detecting more improvement in VA following the first intervention. Mean VA after the reinjection not only showed no improvement but even some worsening.
CMT reduction was observed after both of the injections. Although these changes were not statistically significant, the reduction was more pronounced at month 2 after the initial injection.
One of the limitations in our study was the low number of cases who received both injections. This might have decreased the power of the study to detect a difference following the two interventions. In spite of this limitation, the difference in the pattern of IOP changes between the two injections was significant. This study showed that repeated injection (even after 10 months) had an additive effect on IOP. After reaching a maximum level at 2 months following both injections, IOP decreased to its previous level after the second injection but this effect was less pronounced than the first one. Considering that IVT does not remain effective in the eye for more than 10 months,9 it might be suggested that a long-lasting or even irreversible effect of the drug on the anterior chamber angle component may be the reason for persistently increased IOP levels. This observation is not unexpected considering the side effects observed with other routes of corticosteroid administrations. In this method, however, a highly potent corticosteroid is in persistent contact with the anterior chamber angle with no major barrier like the cornea or sclera.
No definitive cause could be discerned for the lower therapeutic effect after the reinjection. It has been found that the vitreous concentration of triamcinolone after 4-mg injection is 10,000 times greater than that required to occupy all of the corticosteroid receptors.11 Therefore, the lower response to repeated rejections might be due in part to receptor down-regulation following this high dosage because of decreased affinity and/or number of receptors. Another hypothesis could be the worsening of macular edema during 10 months of follow-up.
Considering the greater adverse effects and slightly lower therapeutic response following the second administration, we would not recommend repeated IVT injections for diabetic macular edema as a routine treatment strategy. However, the number of cases in this report is rather low and complementary studies are suggested.
Footnotes
Supported by the Ophthalmic Research Center of Shaheed Beheshti University of Medical Sciences.
References
- 1.William E, Benson . Duane's Clinical Ophthalmology [book on CD-ROM] Lippincott: Williams & Wilkins Publishers; 2004. Diabetic Retinopathy. chap 30. [Google Scholar]
- 2.Jonas JB, Kreissig I, Sofker A, Degenring RF. Intravitreal injection of triamcinolone for diabetic macular edema. Arch Ophthalmol. 2003;121:57–61. [PubMed] [Google Scholar]
- 3.Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920–927. doi: 10.1016/s0161-6420(02)00975-2. [DOI] [PubMed] [Google Scholar]
- 4.Ciardella AP, Klancnik J, Schiff W, et al. Intravitreal triamcinolone for the treatment of refractory diabetic macular oedema with hard exudates: an optical coherence tomography study. Br J Ophthalmol. 2004;88:1131–1136. doi: 10.1136/bjo.2004.041707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutter FK, Simpson JM, Gillies MC. Intravitreal triamcinolone for diabetic macular edema that persists after laser treatment: three-month efficacy and safety results of a prospective, randomized, double-masked, placebo-controlled clinical trial. Ophthalmology. 2004;111:2044–2049. doi: 10.1016/j.ophtha.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Jonas JB, Degenring RF, Kamppeter BA, et al. Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol. 2004;138:158–160. doi: 10.1016/j.ajo.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 7.Jonas JB, Kreissig I, Degenring R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol. 2003;87:24–27. doi: 10.1136/bjo.87.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonas JB, Degenring RF, Kamppeter BA, et al. Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol. 2004;138:158–160. doi: 10.1016/j.ajo.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 9.Beer PM, Bakri SJ, Singh RJ, et al. Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology. 2003;110:681–686. doi: 10.1016/S0161-6420(02)01969-3. [DOI] [PubMed] [Google Scholar]
- 10.Jonas JB. Intraocular availability of triamcinolone acetonide after intravitreal injection. Am J Ophthalmol. 2004;137:560–562. doi: 10.1016/j.ajo.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Diabetic retinopathy clinical research network. A randomized trial comparing intravitreal triamcinolone acetonide and laser photocoagulation for diabetic macular edema. Version 4.0. 2005. chap. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]