Abstract
Purpose
To determine the outcome of part-time occlusion therapy in children with anisometropic amblyopia detected after they were 8 years of age.
Methods
We analyzed 29 eyes with anisometropic amblyopia in children 8 years of age and older. The mean age was 8.79±0.98 (range 8~12) years old. The subjects whose best-corrected visual acuity (BCVA) did not improve by two lines or better within 2 weeks of wearing glasses full-time were prescribed occlusion therapy for 6 hours a day outside of school hours, along with the instruction to wear glasses full-time. Subjects who complied with occlusion for more than 3 hours a day were considered to comply well.
Results
The major component of the anisometropia was hyperopia in 51.7% of the subjects, and hyperopia plus astigmatism was found in 24.1%. The mean pretreatment BCVA score was 0.51±0.23 (LogMAR). Compliance was 89.66%. The mean posttreatment BCVA was 0.03±0.01 (LogMAR), and the success rate, based on a posttreatment BCVA of 0.1 (LogMAR) and better, was 96.43%. It took an average of 4.79±3.35 months to reach the desired posttreatment BCVA. The mean posttreatment stereopsis was 79.78±37.61 seconds of arc. The recurrence rate was 8%. The visual improvement was related to the degree of compliance (p=0.000). The time taken to reach the posttreatment BCVA was shorter in subjects with a better pretreatment BCVA (p=0.019), but it did not relate to the compliance (p=0.366).
Conclusions
The most common component of anisometropia detected after 8 years of age was hyperopia. The part-time occlusion therapy, which had been carried out after school hours, was successful in most cases.
Keywords: Anisometropic amblyopia, Part-time occlusion
Amblyopia, which occurs in two percent of the total population,1 is the visual deterioration of one or both eyes in the absence of organic abnormalities. It is classified into three categories including strabismic amblyopia, anisometropic amblyopia and visual deprivation amblyopia according to the cause.2,3 While strabismic amblyopia has commonly been reported to be more than anisometropic amblyopia, it was reported that anisometropic amblyopia is more common in the case of amblyopia detected for the first time after 7 or 8 years of age. The reason might be that strabismic amblyopia is easier to detect at an earlier date due to its manifest strabismus.4-8 Full-time occlusion has been the preferred method of amblyopia treatment, and it has been reported that full-time occlusion was more effective in anisometropic amblyopia compared with part-time occlusion.9 However, full-time occlusion may not be suitable in children older than 8 years, considering that they will be attending elementary school and should adapt themselves to a group environment. In the case of the children undergoing full-time occlusion therapy, they might be jeered or shunned by classmates and the compliance rate of occlusion therapy would likely decrease.10
The present study focused on researching the clinical pattern of anisometropic amblyopia detected for the first time at the age of 8 years or older. In the same way, the subjects performed part-time occlusion therapy outside of school hours in order to determine whether the amblyopia could be effectively treated with part-time occlusion therapy in those patients.
Materials and Methods
Anisometropic amblyopia, with a difference in best-corrected visual acuity (BCVA) of over two lines between both eyes, was detected for the first time by a corresponding author in subjects ages 8 years or older after they had entered elementary school. Anisometropia was defined as the difference of spherical equivalent exceeding 0.5 diopters or of astigmatism exceeding 1.5 diopters.11 Patients who had not had any ophthalmic treatment, who did not show any symptom of strabismus, who had never worn glasses before, and whose BCVA in their sound eye was 1.0 diopters (LogMAR=0.0) were selected. All patients who met the above conditions and who had been prescribed the treatment and follow-up regimen described below starting in 2000 were included. Finally, the subjects were 29 school-aged children.
An ophthalmic examination including visual acuity, szlit-lamp biomicroscopy, manifest and cycloplegic refraction, an alternate prism cover test, a test of versions/ductions and a fundus examination was given in each patient. Cycloplegic refractions were performed at 90 minutes after the instillation of 1% cyclopentolate eye drops. At the initial prescription, full astigmatic refractive errors were corrected and in each case spherical diopters were adjusted to the lens power that correspond to the patient's best-corrected visual acuity after full cycloplegic correction in a trial frame. Every lens power over the amblyopic eye was determined by one specialist (a corresponding author) and was re-evaluated at each visit and whenever there were any changes or new glasses were prescribed. Visual acuity was tested with Dr. Hahn's standard test chart for 5m, and stereoscopic visual acuity was evaluated with the Titmus-fly test and the Randot Stereotest. Near stereopsis was graded with normal being 25~60 seconds of arc, near normal as 70~100 seconds of arc, and sub-normal being over 100 seconds of arc. All visual acuities were transposed to the logarithm of the minimal angle of resolution (LogMAR) for calculations.12
If the BCVA did not improve by two lines or better within 2 weeks after wearing glasses full-time, a 6-hour occlusion using a 3 M orthoptic eye patch worn over the sound eye combined with a full-time wearing of glasses was prescribed. Occlusion was instructed to be done outside of school hours and under parental observation. The subject were advised to do activities such as watching TV, reading and computer operating for at least one hour while their sound eye was patched. The subjects were observed at 1-month intervals until they achieved their final BCVA, and their parents were asked at every visit to report the average occlusion times. Compliance was determined by parental reports and those who had covered their eyes for over 3 hours a day were considered to comply well.
The period of occlusion therapy was determined by the time at which the BCVA reached a plateau of its highest level. The patients who had no further changes in visual acuity of the amblyopic eye for three consecutive visits after attainment of significant improvement were considered to reach a plateau. This period did not include the consecutive follow-up period after arriving at their plateau or the time period during which daily short-time occlusion was continued in some patients who complied well in order to maintain the achieved final visual acuity (period of maintenance). Successful treatment of the amblyopia was defined as cases who achieved a posttreatment BCVA of 0.8 (LogMAR=0.1) or better.
We also tried to determine if there were any factors associated with treatment outcomes in our patients. The subjects were divided into three groups according to the occlusion time reported by the parents. The first group underwent occlusion therapy for 6 hours a day, the second group for 4 or 5 hours a day and the third group for 3 hours or less daily. Visual improvement was determined by subtracting posttreatment BCVA (LogMAR) from pretreatment BCVA, and the correlation between visual improvement and occlusion time was examined. The correlation between occlusion time and the period of occlusion therapy was also investigated. In addition, to compare means the subjects were divided into three groups according to pretreatment BCVA, in order of 0.1~0.2 (LogMAR=1.0~0.8), 0.2~0.3 (LogMAR=0.7~0.5) and 0.4~0.6 (LogMAR=0.4~0.2). We also examined the correlation between pretreatment BCVA and the period of occlusion therapy, and between pretreatment BCVA and occlusion time.
Statistical analyses were performed including an ANOVA test and a Pearson correlation using SPSS (Statistical Package for the Social Sciences) for Windows version 9.0. P values of less than 0.05 were considered statistically significant.
Results
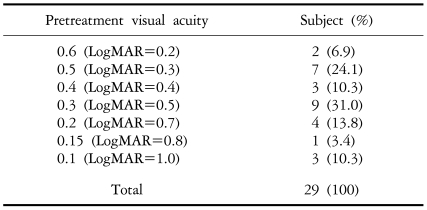
There were 19 male and 10 females subjects, and their mean age was 8.79±0.98 (range: 8~12) years (Table 1). The mean follow-up period after the initiation of treatment was 20.6±17.2 (range: 6~60) months. Mean pretreatment BCVA of amblyopic eyes was LogMAR 0.51±0.23 (Table 2). The classification types of anisometropia induced myopia plus astigmatism in three subjects (10.3%), hyperopia plus astigmatism in seven subjects (24.1%), myopia in one subject (3.4%), hyperopia in 15 subjects (51.7%) and astigmatism in three subjects (10.3%). Hyperopia accounted for the highest proportion.
Table 1.
Distribution of the patients' ages
Table 2.
Pretreatment best-corrected visual acuities of the amblyopic eyes
In two cases visual acuity improved by 1.0 diopter (LogMAR=0.0) through simply wearing glasses for one month (Table 3). The other 27 cases performed the occlusion therapy, and the compliance rate was 88.9% (n = 24/27) (Fig. 1). As previously mentioned, the subjects were composed of three groups, the first group of 17 cases (58.62%) underwent occlusion therapy for 6 hours a day, the second group of seven cases (24.14%) underwent 4 or 5 hours of treatment a day, and the third group of two cases (6.9%) underwent 3 hours or less of occlusion therapy daily. In one case (3.45%) the treatment was abandoned and the subject did not pursue further occlusion therapy (Table 3).
Table 3.
This table shows the clinical pattern of the patients who had undergone 3 hours or less of occlusion treatment, whose visual acuity was improved only by wearing spectacles, and also the single subject who gave up continuing the occlusion therapy
Fig. 1.
Distribution of the daily occlusion hours. When subjects who had covered their strong eyes for more than 3 hours a day were considered to comply well, the compliance of part-time occlusion therapy was 88.9%.
*: One subject disontinued the occlusion therapy before his corrected visual acuity reached the plateau.
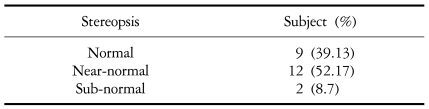
Mean posttreatment BCVA was LogMAR 0.03±0.01. Classification of the posttreatment BCVA showed 1.0 (LogMAR=0.0) in 22 cases (75.86%), 0.8~0.9 (LogMAR=0.1) in five cases (17.24%) and 0.5 (LogMAR=0.3) in one case (3.45%). The posttreatment BCVA of one child who failed to continue the occlusion was 0.1 (LogMAR=1.0). The success rate was 93.1% (n=27/29) (Fig. 2). At the end of the period of occlusion therapy, the posttreatment stereopsis was examined in 23 cases, and the mean was 79.78±37.61 seconds of arc. The subjects mostly showed good posttreatment stereopsis of 100 seconds of arc or better (Table 4). Both the pretreatment and posttreatment stereopsis were examined in 17 cases. Among those, 14 showed improved posttreatment stereopsis, one exhibited a worsened posttreatment stereopsis and two had no change compared with preteatment stereopsis. In addition, the BCVA of their sound eyes continuously maintained a visual acuity of 1.0 (LogMAR=0.0).
Fig. 2.
Distribution of posttreatment best-corrected visual acuities. The mean was LogMAR 0.03±0.01. The success rate was 93.1% based on the cases where the final best-corrected visual acuity was 0.8 (LogMAR=0.1) or higher.
Table 4.
Distribution of posttreatment stereopsis in anisometropic amblyopes (Total subjects=23)
During the follow-up study, two children had a relapse. The first child's BCVA reached 0.9 (LogMAR=0.1) after the sixth month of occlusion therapy but had fellen by 0.7 (LogMAR=0.2) at the 13-month follow-up. This patient's BCVA had been maintained at 0.7 (LogMAR=0.2) since 11 months after the relapse, and her parents did not want to redo the occlusion therapy. The second child's BCVA reached 1.0 (LogMAR=0.0) after the seventh month but fell by 0.6 (LogMAR=0.2) by the 36th month of follow-up. In this second case, the visual acuity returned to 1.0 (LogMAR=0.0) after the 6-hour patching was repeated for 2 months. The overall relapse rate was 7.96 % (n=2/26).
Visual improvement and occlusion time showed a significantly positive correlation (Pearson correlation coefficient=0.566; p=0.001). Statistically significant differences were in mean visual improvements between the three classes divided by the occlusion time (ANOVA test, p=0.000). The visual improvement of the 6-hour group was 0.53±0.22, the 4~5-hour group improved to 0.46±0.22, and the less-than-3-hour group was 0.1±0.0 (Fig. 3).
Fig. 3.
The graph of monthly visual acuity changes according to the occlusion time.
The mean period of occlusion therapy overall was 4.79±3.35 months. (Fig. 4) The mean period of occlusion therapy in the 6-hour group was 5.31±3.20 months, was 5.00±3.56 months in the 4~5-hour group, and was 1.00±0.00 month in the less-than-3-hour group. However, occlusion time and the period of occlusion therapy did not show a significant correlation (Pearson correlation coefficient=0.193; p=0.366) and no difference was seen in the mean period of occlusion therapy between the three classes when divided by occlusion time (ANOVA test, p=0.938). The preteatment LogMAR BCVA was positively correlated with the period of occlusion therapy (Pearson correlation coefficient=0.442; p=0.019). As a result of dividing the pretreatment BCVA into three groups, the period of occlusion therapy between the groups showed significant differences (ANOVA test, p=0.027). We determined that the worse the pretreatment BCVA was, the longer the period of required occlusion therapy.
Fig. 4.
The period of occlusion therapy determined by the time at which the pretreatment best-corrected visual acuity reached a plateau of its best level. In most cases it took less than 6 months, and the mean period of occlusion therapy was 4.79±3.35 months.
Occlusion time and the pretreatment LogMAR BCVA did not show a significant correlation (Pearson correlation coefficient=0.207; p=0.322). As a result of dividing the pretreatment BCVA patients into three groups, the occlusion time between groups did not show differences (ANOVA test, p=0.938).
Discussion
Occlusion of the nonamblyopic eye has been the major therapy of amblyopia. Though full-time occlusion has been classically used as an effective method, there is no proven advantage of longer daily occlusion hours. Opinions vary on the number of daily occlusion hours, and there have not been conclusions about the most effective and optimal regimen.13,14 In addition, Yeom et al.8 reported that solitary 6-hour occlusion therapy revealed an effective improvement of the best-corrected visual acuity and provided good maintenance of improvement in the treatment for monocular amblyopes aged 3 to 8 years.
PEDIG15 reported the effectiveness of prescribing 2-hour and 6-hour patching in the treatment of strabismic and anisometropic amblyopia of a moderate degree in children from the ages of 3 to 7 years. Both regimens appeared to be equally effective in improving the overall 4-month visual acuity.
There is overwhelming clinical agreement on the concept that amblyopia treatment is less effective in older children and that amblyopia needs to be treated at an age younger than 6 or 7 years.13,16 Flynn et al.17 reported that the patient's age was the factor most firmly related to a successful result in amblyopia treatment. However, whether treatment is really ineffective over certain age limits is controversial. Rustein and Fuhr18 and Epelbaum et al.16 reported that the efficiency of amblyopia treatment was substantially poorer in children older than 8 to 12 years, and that this efficiency decreased as a function of age. However, Oliver et al.19 reported that children over 8 years-old who fully complied with the full-time occlusion therapy had an improvement similar to that seen in younger patients. Other articles that have prescribed full-time occlusion have reported that this regimen appears to be effective in improving the visual acuity in these older children.20 The lower treatment efficiency in older children might be related to their poor compliance, and good results were correlated with good compliance in past reports.19,21 Compliance is the most important factor to derive a successful result in occlusion therapy 22,23, and Noh and Cho24 reported that part-time occlusion is more easily practiced than full-time occlusion, which concerns children above six years of age.
We aimed to reduce mental and social problems through part-time occlusion therapy taking place outside of school hours and targeting school children whose anisometropic amblyopia was detected for the first time at the age of 8 years and older. We also evaluated whether the treatment would be effective in this age group. In addition, we strongly instructed the parents to cover their children's sound eye outside of school hours and to observe their children during the occlusion time as much as possible. They were also advised to have their children do activities such as watching TV, reading or computer operating for at least one hour during the occlusion time. Such detailed instructions gave the parents a realistic opportunity to adhere to the treatment, and its compliance was relatively good at 88.9%.
The success rate in this study was 93.1% based on the posttreatment BCVA of LogMAR 0.1 or better. Most children showed stereopsis greater than 100 seconds of arc at the end of the treatment period. We could not practically include a full-time patched group and an untreated control group in this study. However the success rate of 93.1% and the mean improvement of 0.51 Log MAR unit in our subjects was comparable to the results of earlier studies which reported that all patients in a full-time occlusion therapy group experienced a visual acuity improvement ranging from 0.12 to 1.0 (mean 0.46) LogMAR units20 Earlier studies also reported that the final vision in 94% of the patients improved by at least two lines after full-time occlusion therapy21, but a direct comparison was not possible between these studies and the present study because their definition of a successful outcome was different from that used in our study.
Occlusion therapy for unilateral amblyopia is based on longstanding clinical experience indicating that a significant improvement of visual acuity in the amblyopic eye is rarely obtained without sound-eye occlusion due to unbalanced retinal rivalry between the two eyes. Even though we could not compare our findings with an untreated group, we started occlusion therapy only in subjects in which the BCVA did not improve by two lines or better after 2 weeks of wearing glasses.
The mean period of occlusion therapy was 4.79±3.35 months and improvement in visual acuity usually occurred within 6 months. Improvement was not longer than that of other reported studies.19-21 Oliver et al.19 reported that during the first quarter (0~3 months) of the amblyopia treatment there were 3.6 lines of improvement for the oldest group and 4.1 lines for the youngest group, while relatively minor improvements were obtained at later dates. Mohan et al.20 reported that the duration required to achieve a stable vision improvement had been 5.77, 6.31, 5.27 and 5.22 months in patients aged 11, 12, 13 and 14 to 15 years, respectively, while Park et al.21 found that the average treatment duration had been 10 months (range of 3~27 months), and improvement in visual acuity had mostly occurred in the initial 3~6 months of treatment. The occlusion time and the period of occlusion therapy did not have a significant relationship (p=0.366) in this study. However, it appeared that the patients with the worst pretreatment BCVA scores needed a longer period of occlusion therapy (p=0.019).
Visual improvement, which was calculated by subtracting the posttreatment LogMAR BCVA from the pretreatment LogMAR BCVA, and occlusion time showed a positive function of correlation (p=0.001). We think this fact could have two aspects in our study subjects. First, the subjects who completed longer occlusion hours experienced, a greater visual improvement. Because our subjects mostly achieved a posttreatment BCVA of over 0.8 (LogMAR=0.2), the greater visual improvement roughly means that even though the initial visual acuity may have been poor, the compliance rate of the subjects was high. Though it is not statistically significant (p=0.322), occlusion time and pretreatment LogMAR BCVA showed a weakly positive function (Pearson correlation coefficient=0.207), and occlusion time among the three classes regarding pretreatment BCVA did not have any differences (ANOVA test, p=0.938). The reason for such good compliance even in the group with the worst initial visual acuity might be that the parents and children could be aware of the seriousness of the treatment and were also instructed on how to perform the treatment, it might also be attributed to a detailed discussion between the physician and the patients.
The reported recurrence of treated amblyopia varies in articles from 9%20 to 75%.18 By PEDIG,25 in the amblyopes younger than 8 years of age who stopped patching, the reported relapse rate was 25%, and in those who stopped atropine penalization the relapse rate was 21%. The relapse rate of 7.96% (n=2/26) in the present study was relatively low, and the factors that daily occlusion hours were short and the children were older than the usual amblyopia group might contribute the lower recurrence but it is necessary to continue further studies on amblyopia treatment using large samples and control groups to confirm our results.
Considering the types of anisometropia seen in our subjects, the children who had only hyperopia and the ones who had hyperopia simultaneously with astigmatism accounted for 51.7% and 24.1%, respectively. This showed that the anisometropic amblyopia, which was hidden in the children over 8 years old, is mostly caused by hyperopia.
In conclusion, the part-time occlusion therapy with at least one instructed hour of active visual activity practiced out of school hours was effective in anisometropic amblyopes who were diagnosed at the age of 8 years and older, and the patients complied well with the treatment. Moreover, its success rate was not low compared with the full-time occlusion. It is expected that the part-time occlusion therapy outside of school hours can be effectively used as a therapy in relatively older amblyopes.
Footnotes
This study was presented at the Korean Ophthalmological Society's 93rd Spring Meeting, April 2005, Busan, Korea.
References
- 1.Duke-Elder S, Wybar K. Ocular motility and strabismus. 1st ed. St Louis: CV Mosby, Kimpton; 1973. p. 294. [Google Scholar]
- 2.Leguire LE, Komaromy KL, Nairus TM, Rogers GL. Long-term follow-up of L-dopa treatment in children with amblyopia. J Pediatr Ophthalmol Strabismus. 2002;39:326–330. doi: 10.3928/0191-3913-20021101-05. [DOI] [PubMed] [Google Scholar]
- 3.Pandey PK, Chaudhuri Z, Kumar M, et al. Effect of levodopa and carbidopa in human amblyopia. J Pediatr Ophthalmol Strabismus. 2002;39:81–89. doi: 10.3928/0191-3913-20020301-07. [DOI] [PubMed] [Google Scholar]
- 4.Von Noorden GK. Classification of amblyopia. Am J Ophthalmol. 1967;63:238–244. doi: 10.1016/0002-9394(67)91543-7. [DOI] [PubMed] [Google Scholar]
- 5.Jin YH. Strabismology. 2nd ed. Ulsan: Ulsan University Press; 1999. pp. 205–229. [Google Scholar]
- 6.Kim YT, Chang HR. Follow-up Results of the Monocular Amblyopia. J Korean Ophthalmol Soc. 1998;39:305–311. [Google Scholar]
- 7.Park MH, Rah SH, Kim SH. The analysis of improvement of visual acuity by occlusion therapy in amblyopic children above 6 years of age. J Korean Ophthalmol Soc. 1994;35:190–195. [Google Scholar]
- 8.Yeom HY, Han SH, Lee JB. Effects of solitary part-time occlusion for the treatment of monocular amblyopia patients. J Korean Ophthalmol Soc. 2004;45:1134–1140. [Google Scholar]
- 9.Scott WE, Stratton VB, Fabre J. Full-time occlusion therapy for amblyopia. Am Orthopt J. 1980;30:125–130. [Google Scholar]
- 10.Moon CS, Jin YH. Timing of amblyopia therapy in pure anisometropic amblyopia. J Korean Ophthalmol Soc. 1998;39:185–192. [Google Scholar]
- 11.Repka MX, Cotter SA, Beck RW, et al. A Randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–2085. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 12.Sloan LL. Measurement of visual acuity. AMA Arch Ophthalmol. 1951;45:704–725. doi: 10.1001/archopht.1951.01700010719013. [DOI] [PubMed] [Google Scholar]
- 13.Von Noorden GK, Campos EC. Binocular vision and Ocular motility. 6th ed. St. Louis: Mosby; 2002. pp. 246–287. [Google Scholar]
- 14.Hiscox F, Strong N, Thompson JR, et al. Occlusion for amblyopia a comprehensive survey of outcome. Eye. 1992;6:300–304. doi: 10.1038/eye.1992.59. [DOI] [PubMed] [Google Scholar]
- 15.The Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 16.Epelbaum M, Milleret C, Buisseret P, Dufier JL. The sensitive period for strabismic amblyopia in humans. Ophthalmology. 1993;100:323–327. doi: 10.1016/s0161-6420(13)32170-8. [DOI] [PubMed] [Google Scholar]
- 17.Flynn JT, Schiffman J, Feuer W, Corona A. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of publishied studies. Trans Am Ophthalmol Soc. 1998;96:431–450. [PMC free article] [PubMed] [Google Scholar]
- 18.Rutstein RP, Fuhr PS. Efficacy and stability of amblyopia therapy. Optom Vis Sci. 1992;69:747–754. doi: 10.1097/00006324-199210000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Oliver M, Neumann R, Chaimovitch Y, et al. Compliance and results of treatment for amblyopia in children more than 8 years old. Am J Ophthalmol. 1986;102:340–345. doi: 10.1016/0002-9394(86)90008-5. [DOI] [PubMed] [Google Scholar]
- 20.Mohan K, Saroha V, Sharma A. Successful occlusion therapy for amblyopia in 11- to 15-year-old children. J Pediatr Ophthalmol Strabismus. 2004;41:89–95. doi: 10.3928/0191-3913-20040301-08. [DOI] [PubMed] [Google Scholar]
- 21.Park KH, Hwang JM, Ahn JK. Efficacy of amblyopia therapy initiated after 9 years of age. Eye. 2004;18:571–574. doi: 10.1038/sj.eye.6700671. [DOI] [PubMed] [Google Scholar]
- 22.Searle A, Norman P, Harrad R, Vedhara K. Psychosocial and clinical determinants of compliance with occlusion therapy for amblyopic children. Eye. 2002;16:150–155. doi: 10.1038/sj.eye.6700086. [DOI] [PubMed] [Google Scholar]
- 23.Beardsell R, Clarke S, Hill M. Outcomes of occlusion treatment for amblyopia. J Pediatr Ophthalmol Strabismus. 1999;36:19–24. doi: 10.3928/0191-3913-19990101-05. [DOI] [PubMed] [Google Scholar]
- 24.Roh GH, Cho YA. Compliance of patching therapy for amblyopia. J Korean Ophthalmol Soc. 1993;34:103–109. [Google Scholar]
- 25.The Pediatric Eye Disease Investigator Group. Risk of amblyopia recurrence after cessation of treatment. J AAPOS. 2004;8:420–428. doi: 10.1016/S1091853104001612. [DOI] [PubMed] [Google Scholar]