Abstract
Purpose
The surgical technique for intermittent exotropia 「X(T)」 is quite simple. However, in many cases, the condition recurs due to any one of a number of causes, including undercorrection. This study examined the factors associated with undercorrection on X(T) patients.
Methods
The study examined 199 X(T) patients who underwent bilateral recession of the lateral rectus muscle or unilateral recession of the lateral rectus muscle and resection of the medial rectus muscle, and who were followed-up for more than a year. Patients whose near and far distance angles of deviation were 9 prism diopters (PD) or more at one year after surgery were designated as group 1. Those whose PD was 8 or below or who had orthophoria were assigned to group 2. Various factors were compared and analyzed.
Results
One day after surgery, group 1 showed an average overcorrection of 1.9 and 4.1 PD at near and far, respectively, and group 2 showed an average overcorrection of 6.3 and 7.6 PD at near and far, respectively. A statistically significant difference was observed between the two groups (p<0.05). Factors such as the age of onset of strabismus, age at the time of surgery, the interval from the onset of strabismus to surgery, the preoperative angle of deviation, the dissociated vertical deviation, amblyopia, anisometropia and vertical strabismus had no influence on the undercorrection of X(T) patients (p>0.05).
Conclusions
Of the many factors that might influence the surgical results of X(T) patients, the angle of deviation during the initial postoperative period is the most important factor.
Keywords: Intermittent exotropia, Overcorrection, Strabismus, Undercorrection
The cause of intermittent exotropia 「X(T)」 is unclear but X(T) is the most frequently acquired exotropia which develops in Korean children. Surgery is mainly used to treat X(T). X(T) can be cured through surgery but there is a 20-50% recurrence rate depending on the follow-up period.1 In Korea, Kim and Cho2 reported the incidence of postoperative undercorrection of X(T) to be 27%. In other countries, Richard and Parks3 reported an incidence of 38% and Clarke and Noel4 an incidence of 50%.
Among the factors associated with the outcome of surgery for X(T), the surgical methods, type of strabismus, preoperative deviation angle, and deviation angle in the initial postoperative period have been reported to have significant influence. Many studies on the factors associated with the success of surgery have been performed but there are few reports on undercorrection.
Therefore, this study examined the factors associated with undercorrection in 199 patients who were diagnosed with X(T), who underwent surgery, and were available for an average long-term follow-up of more than 2 years. The relationship of undercorrection with the following factors was examined: the age of onset, age at the time of surgery, near and far preoperative deviation angle, amblyopia, anisometropia, dissociated vertical deviation, inferior oblique overaction, the presence of concomitant vertical strabismus, and the deviation angle at the initial postoperative period.
Materials and Methods
The study was performed from January 1999 to February 2004 on 199 patients who were diagnosed with X(T) at our hospital and were available for follow-up for more than 1 year. There were 83 males and 116 females. Of the types of X(T) encountered, the basic type was most prevalent and occurred in 151 cases. This was followed by 29 cases of the pseudodivergence excess type, 5 cases of the convergence insufficiency type, and 14 cases of the divergence excess type. Among the patients who underwent unilateral recession of the lateral rectus muscle and resection of the medial rectus muscle (60 cases) or bilateral recession of the lateral rectus muscle (139 cases), at the last follow-up, the group with deviation angles more than 9 prism diopters (PD) at near and far distance was designated as group 1 (undercorrection group). The group with orthophoria or deviation angles less than 8 PD was designated as group 2 (success group). Eighty patients were included in group 1 and 119 patients were included group 2.
The age at onset was assessed during the examination and age at the time of surgery was also recorded. In all patients, a refraction was performed after applying 1% Cyclogyl®. The refractive error, was calculated in diopters as the spherical equivalent, or the addition of the spherical power and half the magnitude of the cylinder power. Anisometropia was defined as an absolute difference of the spherical equivalent of 2 or more diopters between the right and left eyes. In cases where the uncorrected visual acuity was less than 20/30, the refractive error was corrected and the visual acuity was assessed with an alternate prism cover test to measure the deviation angle. The function of the extraocular muscle, its overaction and underaction were assessed by monocular and binocular movements. The same surgeon performed the surgical procedure for all patients. The deviation angle at near and far distance was measured 1 day, 1 week, 1 year, and at the last follow-up after surgery. In the two groups, the relationship between the postoperative deviation angle and the age at onset, age at the time of surgery, near and far preoperative deviation angle, amblyopia, anisometropia, dissociated vertical deviation, inferior oblique overaction, and the presence of concomitant vertical strabismus were examined. For statistical analysis, the near and far deviation angle was analyzed using a 2-sample t-test, and the other factors were analyzed by a Chi-square test. A p value <0.05 was considered significant.
Results
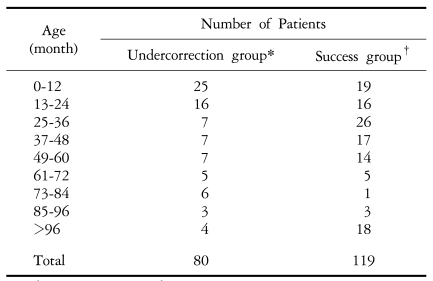
The average postoperative follow-up period was 26 months (12-80 months). Table 1 shows the age of onset in the undercorrection and success groups at the last follow-up. There was no statistically significant difference between the two groups.
Table 1.
Age at onset
P value=0.375, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria.
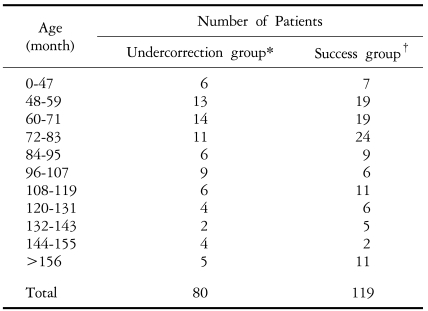
Regarding the age at the time of surgery, there were 6 patients younger and 74 patients older than 4 years in the undercorrection group, and 7 patients younger and 112 patients older than 4 years in the success group. There was no statistically significant difference between the two groups (p=0.385) (Table 2).
Table 2.
Age at the time of surgery
P value=0.385, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria.
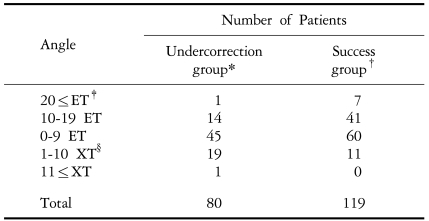
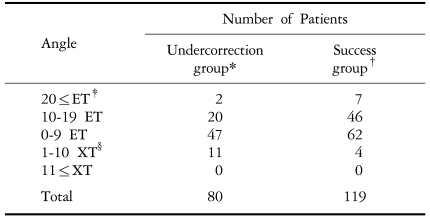
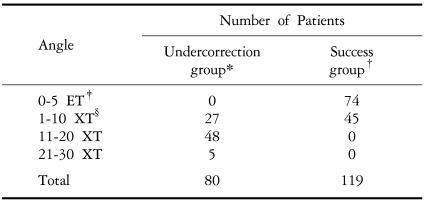
One day after surgery, an average overcorrection of 1.9 and 4.1 PD at near and far distance, respectively, were observed in the undercorrection group. On the other hand, the success group had an average overcorrection of 6.3 and 7.6 PD at near and far distance, respectively, which was statistically significant (p=0.000). Table 3 shows the distribution of each group 1 day after surgery according to the near deviation angle. In the undercorrection and the success groups, 15 patients (19%) and 48 patients (40%) respectively showed overcorrection of more than 10 PD (Table 3). Regarding the distribution of the far angle of deviation at 1 day after surgery, in the undercorrection group, 2 patients had an esodeviation at 20 with 20 PD or greater, 20 patients had an esodeviation at 10 with 19 PD, 47 patients had orthophoria or the esodeviation at 1 with 9 PD, and 11 patients had exodeviation at 1 with 10 PD. However, in the success group, the distribution of the far deviation angle among the above categories was 7, 46, 62, and 4 patients, respectively. This represented a statistically significant difference between the two groups (p=0.000) (Table 4).
Table 3.
Distribution according to the near angle of deviation 1 day after surgery
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
Table 4.
Distribution according to deviation angle at far distances 1 day after surgery
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
Regarding to the distribution of the near deviation angle 1 week after surgery, 49 patients in the undercorrection group showed esodeviation and 30 patients showed exodeviation. The success group, in contrast, had 101 patients showing esodeviation and 17 patients showing exodeviation (Table 5). Regarding the distance deviation angle at 1 week after surgery, 47 patients showed esodeviation and 32 patients showed exodeviation in the undercorrection group. On the other hand, 105 patients showed esodeviation and 13 patients showed exodeviation in the success group. There was a statistically significant difference between the two groups (p=0.000) (Table 6). Because 1 patient in each group did not visit our hospital in the first week after surgery, 79 patients were included in the success group and 118 patients were included in the undercorrection group.
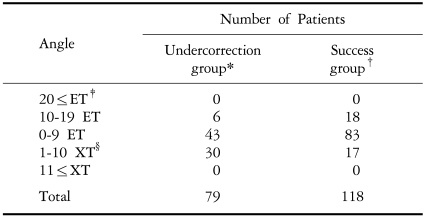
Table 5.
Distribution according to the near angle of deviation 1 week after surgery
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
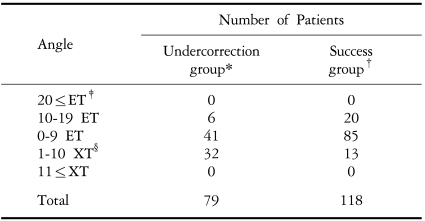
Table 6.
Distribution according to the far angle of deviation 1 week after surgery
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
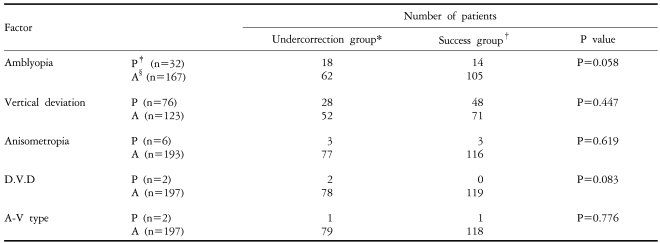
Amblyopia, the rate of anisometropia, the presence of dissociated vertical deviation and A-V type strabismus in the two groups was similar (P=0.058, 0.619, 0.083, 0.776). In the case of vertical strabismus, there were 28 cases in the undercorrection group and 48 cases in the success group but there was no significant difference (p=0.447) (Table 7).
Table 7.
Surgical outcome according to the preoperative factors5
P value >0.05, Chi-Sqaure test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: presence, §: absence.
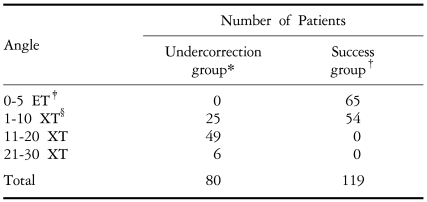
At the last follow-up, the undercorrection group showed an average 14.4 PD and 14.3 PD deviation angle at near and far distance, respectively, and average of 0.88 weeks were required to turn the postoperative overcorrection into the orthophoria. The undercorrection group showed that an average of 36.3 weeks was required to achieve exotropia of more than 9 PD from the orthophoria and an average of 36.9 weeks were needed to achieve exotropia of less than 9 PD. Tables 8 and 9 show the deviation angle distribution at near and far distance in the undercorrection group and success group at the last follow-up.
Table 8.
Distribution according to the deviation angle at near distance on final visitl
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
Table 9.
Distribution according to the deviation angle at far distance on final visit
P value=0.000, 2 sample t-test.
*: The group whose near and far angle of deviation 1 year after surgery was 9 or more. †: The group whose near and far angle of deviation was 8 or below or who had orthophoria. ‡: esodeviation, §: exodeviation.
Discussion
For X(T), a satisfactory outcome can be obtained by the resection or recession of the extraocular muscle of the horizontal muscle according to the preoperative deviation angle. However, in many cases, additional surgery is required for cases of undercorrection. In some cases both the surgeons and the patients may be embarrassed. Postoperative undercorrection may appear immediately after surgery but it can also develop a few months or a few years after surgery. Therefore, numerous studies have been performed pertaining to the factors causing undercorrection.
The success rate of surgery for X(T) has been reported to be diverse depending on the skill of the surgeon and the duration of follow-up. Richard and Parks3 reported a low success rate of 56%. In Korea, various surgery success rates ranging from 58.8% to 86.5% have been reported.2,5,6 Scott et al7 have reported the level of the preoperative deviation angle, the difference in deviation angle at near and far, the amount of change in the deviation angle during the upward or downward gaze, age at the time of surgery, and refractive power to be major factors influencing the outcome of surgery for exotropia.
As a postoperative factor, this study measured the deviation angle 1 day, 1 week, and 1 year after surgery as well as at the last follow-up. The preoperative factors, amblyopia, anisometropia, dissociated vertical deviation, inferior oblique overaction and the presence of concomitant vertical strabismus were compared and analyzed. Only the deviation angle at 1 day and 1 week after surgery were significantly different between the undercorrection and the success groups. Among the preoperative and postoperative factors that influence the outcome of surgery for X(T), Keenan and Willshaw8 reported that the age at onset, age at the time of surgery, amblyopia, refractive error, the presence of anisometropia, nor the surgical method had any effect, and only moderate overcorrection at the initial postoperative period influenced the surgical outcome.
Similarly, Ko and Min6 reported that the deviation angle immediately after the bilateral recession of the lateral rectus muscle was an important factor influencing the surgical outcome. In particular, the group showing an overcorrection between 6 and 9 PD immediately after surgery had a 95.6% success rate. Some authors9,10 have reported that a better result could be obtained by performing surgery allowing for a 10-20 PD overcorrection immediately after surgery in comparison to undercorrection. Other authors11 have reported that the initial deviation angle on 1 day after the surgery for X(T) could be a predictive factor influencing the surgical outcome. Depending on the surgical techniques, a good result could be obtained by an overcorrection with esodeviation of 1-10 PD at the initial postoperative period in a unilateral recession of lateral rectus muscle, and resection of the medial rectus muscle with an overcorrection of 11-20 PD esodeviation in the bilateral recession of the lateral rectus muscle. In this study, an overcorrection of 1.9 and 4.1 PD at near and far distance, respectively, was detected in the undercorrection group, and an average overcorrection of 6.3 and 7.6 PD at near and far distance, respectively, was observed in the success group. There was a significant difference between the two groups. Therefore, deviation angle as measured at the initial postoperative period is an important factor mediating the effect of the undercorrection, and overcorrection may be important for the success of the surgery.
In this study, preoperative factors such as the age at onset, age at the time of surgery, difference in the deviation angle at near and far distances, amblyopia, anisometropia, dissociated vertical deviation, inferior oblique overaction, and the presence of concomitant vertical strabismus were not found to affect the surgical outcome. Other authors12 have reported that among the preoperative factors, age at the time of surgery, type of exotropia, presurgical deviation angle, amblyopia, dissociated vertical deviation, inferior oblique overaction and the A-V type strabismus did not have a significant effect on the surgical outcome, with a good surgical outcome obtained in the group with diplopia caused by overcorrection. In most studies,6,13,14 the age at the onset of strabismus was not associated with the success of surgery. However, Ko and Min6 reported that the highest success rate, 92.9%, was detected at the onset age between 4 and 7 years but this was not statistically significant. Richard and Parks3 divided 111 X(T) patients who underwent bilateral recession of the lateral rectus muscle into 3 groups; younger than 3 years, between 3 and 6 years and older than 6 years. They found that the age at the time of surgery and the surgical outcome did not influence the outcome. In Korea, Cho and Lim13 also reported no significant difference in success rates of patients younger than 3 years, between 3 and 6 years and older than 6 years. Kim et al14 reported concomitant inferior oblique overaction to be a preoperative factor affecting the incidence of recurrence. However, other studies6,12 reported that the preoperative inferior oblique overaction had no influence on the surgical outcome.
There are many preoperative and postoperative factors influencing the undercorrection of X(T). Our experience indicates that many preoperative factors including age at the time of surgery does not affect successful alignment after surgery but deviation angle at the initial postoperative period does. Therefore, postponing the time of surgery does not improve the chance for obtaining a satisfactory result. Because overaction of the inferior oblique muscle, overaction of the superior oblique muscle, dissociated vertical deviation and hypertropia do not affect the surgical result, it is not necessary to always correct these conditions.
As reported by others, the deviation angle at the initial postoperative period may be an important factor influencing the undercorrection of X(T). For this reason, it is believed that overcorrection to some degree may be required to reduce the recurrence of exotropia. Therefore, a longer follow-up study after surgery for X(T) involving a larger number of subjects will be needed in order to compare and analyze surgical outcome according to postoperative angle of deviation and various other factors prospectively rather than retrospectively.
Footnotes
This study was presented at the Korean Ophthalmological Society's 94nd Annual Meeting, Korea, October, 2004.
References
- 1.Min EJ, Lee MK, Park BI. A clinical study on strabismus in children. J Korean Ophthalmol Soc. 2001;32:379–388. [Google Scholar]
- 2.Kim MM, Cho ST. Long-term surgical results of intermittent exotropia. J Korean Ophthalmol Soc. 1994;35:1321–1326. [Google Scholar]
- 3.Richard JM, Parks MM. Intermittent exotropia: surgical results in different age groups. Ophthalmology. 1983;90:1172–1177. [PubMed] [Google Scholar]
- 4.Clarke WN, Noel LP. Surgical results intermittent exotropia. Can J Ophthalmol. 1981;16:66–69. [PubMed] [Google Scholar]
- 5.Lee JY, Choi DG. The clinical analysis of recurrence after surgical correction of intermittent exotropia. J Korean Ophthalmol Soc. 2002;43:2220–2226. [Google Scholar]
- 6.Ko KH, Min BM. Factors related to surgical results of intermittent exotropia. J Korean Ophthalmol Soc. 1996;37:179–184. [Google Scholar]
- 7.Scott AB, Marsh AJ, Jampolsky A. Quantitative guidelines for exotropia surgery. Invest Ophthalmol. 1975;14:428–436. [PubMed] [Google Scholar]
- 8.Keenan JM, Willshaw HE. The outcome of strabismus surgery in childhood exotropia. Eye. 1994;8:632–637. doi: 10.1038/eye.1994.158. [DOI] [PubMed] [Google Scholar]
- 9.Rabb EL, Parks MM. Recession of the lateral recti. Early and late postoperative alignments. Arch Ophthalmol. 1969;82:203–208. doi: 10.1001/archopht.1969.00990020205010. [DOI] [PubMed] [Google Scholar]
- 10.Scott WE, Keech R, Mash AJ. The Postoperative results and stability of exodeviation. Arch Ophthalmol. 1981;99:1814–1818. doi: 10.1001/archopht.1981.03930020688013. [DOI] [PubMed] [Google Scholar]
- 11.Lee SY, Lee YC. Comparision of surgical Results by initial postoperative alignment following bilateral lateral rectus recession and unilateral lateral rectus recession-medial rectus resection in intermittent exotropes. J Korean Ophthalmol Soc. 1999;40:2604–2610. [Google Scholar]
- 12.Choi DG, Kim PS. The Surgical outcome of intermittent exotropia and the prognostic factors. J Korean Ophthalmol Soc. 1998;39:1255–1263. [Google Scholar]
- 13.Cho HY, Lim KH. Related factors of surgical outcome of unilateral R&R for basic type intermittent exotropia in children. J Korean Ophthalmol Soc. 2003;44:2844–2849. [Google Scholar]
- 14.Kim HW, Yang JW, Won IK. Clinical study for risk factors of recurrence in intermittent exotropia. J Korean Ophthalmol Soc. 2000;41:1417–1424. [Google Scholar]