Abstract
Purpose
Paranasal sinus mucocele is a benign, expansile mass which can occur as a result of trauma or spontaneous obstruction of a sinus tract. The purpose of this study was to describe and compare the clinical characteristics of primary mucoceles occurring in patients with no previous sinus surgery history or known cause of mucoceles and secondary mucoceles resulting as a complication following endoscopic sinus surgery or the Caldwell-Luc operation.
Materials and Methods
We performed a retrospective chart review of 33 cases of primary mucoceles and 60 cases of secondary mucoceles which were diagnosed and surgically corrected between 1996 and 2008.
Results
The most common presenting symptoms in primary mucoceles were nasal obstruction (19.4%) and rhinorrhea (17.7%). In secondary mucoceles, the most common symptoms were cheek pain (31.7%) and nasal obstruction (18.3%). The most common origins of primary mucoceles were the ethmoid sinus (45.5%) and the maxillary sinus (18.2%). In secondary mucoceles, the maxillary sinus was the most common site (86%), followed by the ethmoid sinus (7.1%). All patients with secondary mucoceles had a history of sinus surgery.
Conclusion
The maxillary sinus was the most common site of secondary mucoceles while the ethmoid sinus was the most common origin of primary mucoceles. Cases of secondary mucoceles that occurred following sinus endoscopic surgery developed more frequently in the ethmoid sinus than in those following the Caldwell-Luc procedure, therefore, we suggest that the incidence of maxillary sinus mucoceles in the Asian population would decrease as the rate of endoscopic sinus surgery increases.
Keywords: Mucocele, sinusitis, endoscopy, paranasal sinus disease, iatrogenic disease
INTRODUCTION
A mucocele is a benign expansile paranasal sinus lesion which is most commonly found in the frontal sinus, and found occasionally in the ethmoid and sphenoid sinuses.1 Maxillary sinus mucoceles are relatively rare, accounting for no more than 10% of all mucocele cases reported in the English literature.2 However, maxillary sinus mucoceles are more commonly reported in Korea and Japan as a postoperative cheek cyst (POCC), typically occurring as a long-term complication of the Caldwell-Luc procedure.3,4 The explanation for this discrepancy is not immediately apparent.5 Etiologies of mucoceles include chronic infection, allergic sinonasal disease, trauma and prior sinus surgery, however, in many cases the cause remains unknown.6,7
The purpose of this study was to describe and compare the clinical characteristics of primary mucoceles occurring in patients with no known cause or history of previous sinus surgery and secondary mucoceles occurring as a complication following endoscopic sinus surgery or the Caldwell-Luc procedure.
MATERIALS AND METHODS
We carried out a retrospective chart review of 33 cases of primary mucoceles and 60 cases of secondary mucoceles which were diagnosed and surgically corrected between 1996 and 2008. The international review board at our institution approved this study and required neither patient approval nor informed consent for review of images and records. The group including primary mucoceles had no history of previous sinus surgery, while all cases of secondary mucoceles had undergone endoscopic sinus surgery or the Caldwell-Luc procedure. Almost all patients were treated with endoscopic approach, however, Caldwell-Luc operation was performed in other patients, because they were less amenable to endoscopic treatment due to a lateral-type mucocele, severe thickening of the medial bony wall, compartmentalization of the mucocele. Diagnosis was based on previous history of sinus surgery and physical examination including nasal endoscopy, computed tomography (CT) and histopathologic findings. Mucoceles are defined as an expansion of an existing sinus with associated erosion of septations within the sinus and the walls of the sinus. Medical records were reviewed for patient demographics, presenting symptoms, preoperative CT findings, surgical history, resolution of symptoms and need for revision surgery.
All diagnoses and operations were performed by one otorhinolaryngologist in the clinic. Preoperative and postoperative complications were also assessed.
RESULTS
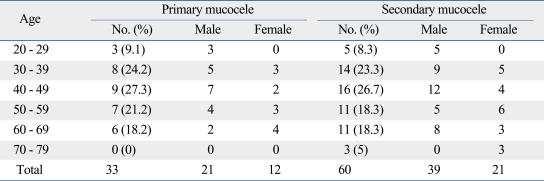
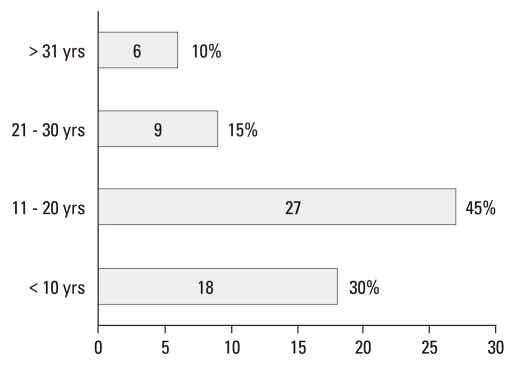
A total of 33 patients (21 men and 12 women) with a mean age of 44.7 years (range 20-69 years) were included in the primary mucocele group. The secondary mucocele group comprised 60 patients (39 men and 21 women) with a mean age of 48.6 years (range 20-78 years) (Table 1). All patients with secondary mucoceles had a history of sinus surgery (12 endoscopic sinus surgeries, 48 Caldwell-Luc operations). The time elapsed between the initial procedure and the development of symptoms ranged from 2 to 42 years (average, 18.8 years). In the majority of cases (45%), 11-20 years had passed since the primary procedure (Fig. 1).
Table 1.
Age and Sex Distribution of Primary and Secondary Mucocele
Fig. 1.
Duration of periods after previous operation of secondary mucocele.
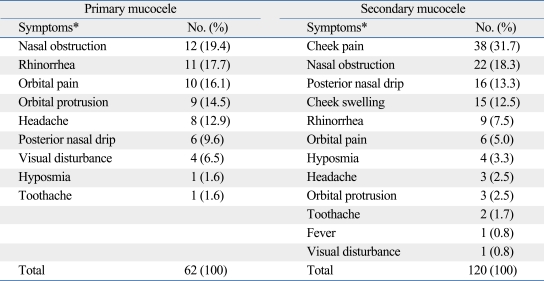
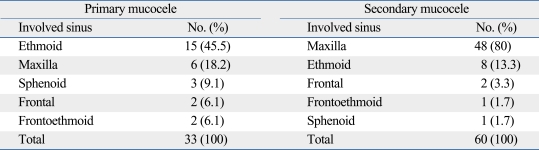
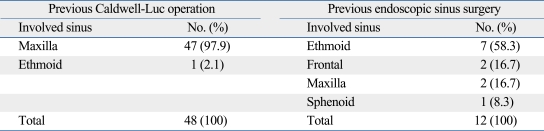
The most common presenting symptoms in primary mucoceles were nasal obstruction (19.4%), rhinorrhea (17.7%) and orbital pain (16.1%). Cheek pain (31.7%), nasal obstruction (18.3%) and posterior nasal drip (13.3%) were most frequently reported in patients with secondary mucoceles (Table 2). Preoperative CT scans were performed in all patients. Mucocele which was located in maxillary sinus was 58.0% (n = 54) and 24.7% (n = 23) in ethmoid sinus. Location of mucocele in operative field was also checked, similar to previous CT finding. The origins of primary mucoceles were the ethmoid (45.5%), maxillary (18.2%), sphenoid (9.1%), frontal (6.1%), and frontoethmoid sinus (6.1%). In secondary mucoceles, the maxillary sinus was the most common site (80%), followed by the ethmoid (13.3%), frontal (3.3%), sphenoid (1.7%), and frontoethmoid sinus (1.7%) (Table 3). However, the most common mucocele site in patients who had previously undergone endoscopic sinus surgery, as opposed to the Caldwell-Luc procedure, was the ethmoid sinus (58.3%) (Table 4).
Table 2.
Presenting Symptoms of Primary and Secondary Mucocele
*Multiple responses were allowed for each patient.
Table 3.
Involved Sinuses of Primary and Secondary Mucocele
Table 4.
Involved Sinuses of Secondary Mucocele According to Surgical Method
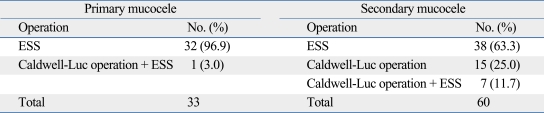
All patients (n = 93) underwent corrective sinus surgery between 1996 and 2008. The majority (96.9%) of patients with primary mucoceles underwent endoscopic sinus surgery. Only one patient (3.0%) underwent both endoscopic sinus surgery and the Caldwell-Luc procedure. In secondary mucoceles, 63.3% of patients underwent endoscopic sinus surgery, 25.0% were managed with the Caldwell-Luc operation, and 11.7% received both treatments (Table 5). The mean follow-up period from the initial operation in the secondary mucocele group was 4.7 years (range 1.4-7.3 years) and 5.5 years (range 1.2-9.8 years) in the primary mucocele group. There were no reported intra- or postoperative complications during admission.
Table 5.
Surgical Method for Primary and Secondary Mucocele
ESS, endoscopic sinus surgery.
A revision procedure was performed in 3 patients (9.1%) with primary mucoceles due to persistent sinusitis, as evidenced by residual symptoms and lesions on CT. Twelve patients (20.0%) with secondary mucoceles experienced recurrence necessitating a revision procedure. The origin of recurrence of secondary mucoceles was predominantly the maxillary sinus (11 maxillary, 1 ethmoid), while all primary mucocele recurrences originated in the ethmoid sinus. All three cases of primary mucocele recurrence achieved symptom relief by revision endoscopic sinus surgery after several years of follow-up. In the secondary mucocele group, 4 patients (33.3%) underwent revision Caldwell-Luc operation, including patients that had formerly undergone endoscopic sinus surgery. The remaining 8 patients (66.6%) underwent an endoscopic revision procedure.
DISCUSSION
Mucoceles of the paranasal sinus are benign, cyst-like, expansile lesions lined with pseudostratified columnar epithelium.1 A mucocele is a mucoid-filled mass that develops following obstruction of the sinus ostium and drainage pattern, which explains the high incidence of mucoceles in the frontal sinus caused by variations in the nasofrontal duct.8 Most mucoceles occur in the frontal sinus (60%) followed by the ethmoid sinus (30%), maxillary sinus (10%) and rarely in the sphenoid sinus.8 Maxillary sinus mucoceles are more commonly reported in Korea and Japan as POCC,3,4 accounting for more than 50% of all paranasal sinus mucoceles in Korean literature9 and 131 of 132 cases of sinus mucoceles in Japan.3 The explanation for the difference in incidence between Asian and Caucasian populations remains unclear.5 Mucoceles that develop following the Caldwell-Luc operation are presumed to result from entrapped sinus mucosa.4 Secondary mucoceles following sinus surgery generally develop as a delayed complication, typically 10 to 30 years postoperatively.10 Similar to previous reports, the mean duration between the initial surgery and the development of secondary mucoceles was 18.8 years in the present study. In the majority of cases (45%), 11 to 20 years had passed since the previous sinus surgery, with the longest interval being 42 years. Diagnosis of mucoceles was made on the basis of symptoms, imaging, surgical exploration and histological confirmation. The most informative radiologic evaluation is CT, which shows a mucocele as a homogenous lesion, isodense with brain tissue and without contrast enhancement, unless infected.1
Traditional surgical management of maxillary sinusitis requires complete drainage through an open approach. Depending on the extent of the sinusitis, this might include either a simple sublabial approach or a lateral rhinotomy incision.11 With the increasing popularity of minimally invasive surgery, functional endoscopic sinus surgery has become the standard procedure for most surgical cases of chronic sinusitis. Therefore, the use of the Caldwell-Luc operation is on the decline and is now only recommended in selected cases.12 This trend has increased the relative incidence of frontal and ethmoid sinus mucoceles. The causes of this change are presumed to be narrow sinus orifice, poor surgical view and outflow tract stenosis after endoscopic widening.4,13 Likewise, in this study, although the maxillary sinus was the most common site of mucoceles, the most common site of primary mucoceles was the ethmoid sinus. Cases of secondary mucoceles following previous sinus endoscopic surgery, as opposed to the Caldwell-Luc operation, also developed more frequently in the ethmoid sinus.
Despite advances in endoscopic equipment and techniques, several indications for the Caldwell-Luc operation remain. Although the most common cause of failure in endoscopic sinus surgery is an obstructed ostium, some patients have pathologic mucosal disease.14,15 In this selected patient population, the Caldwell-Luc operation may be necessary to treat the underlying mucosal disease. Comparison of the results of different surgical techniques is heavily affected by many confounding factors including, but not limited to, different study populations, inaccurate diagnostics and disparate follow-up care. Similar to the delayed occurrence of POCC following the Caldwell-Luc operation, long-term observation is necessary for patients undergoing endoscopic sinus surgery to monitor for recurrence.
Based on the results of this study, we suggest that the incidence of maxillary sinus mucoceles in Asian populations will decrease as the practice of endoscopic sinus surgery increases.
ACKNOWLEDGEMENTS
This study does not have any financial relationship with certain organizations. But, we want to acknowledge alumni of Department of Otolaryngorhinology, Kangbuk Samsung Hospital, for various supports.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Busaba NY, Salman SD. Maxillary sinus mucoceles: clinical presentation and long-term results of endoscopic surgical treatment. Laryngoscope. 1999;109:1446–1449. doi: 10.1097/00005537-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Caylakli F, Yavuz H, Cagici AC, Ozluoglu LN. Endoscopic sinus surgery for maxillary sinus mucoceles. Head Face Med. 2006;2:29. doi: 10.1186/1746-160X-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Busaba NY, Kieff D. Endoscopic sinus surgery for inflammatory maxillary sinus disease. Laryngoscope. 2002;112:1378–1383. doi: 10.1097/00005537-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Kim SS, Kang SS, Kim KS, Yoon JH, Lee JG, Park IY. Clinical characteristics of primary paranasal sinus mucoceles and their surgical treatment outcomes. Korean J Otolaryngol - Head Neck Surg. 1998;41:1436–1439. [Google Scholar]
- 5.Hasegawa M, Kuroishikawa Y. Protrusion of postoperative maxillary sinus mucocele into the orbit: case reports. Ear Nose Throat J. 1993;72:752–754. [PubMed] [Google Scholar]
- 6.Lund VJ, Milroy CM. Fronto-ethmoidal mucoceles: a histopathological analysis. J Laryngol Otol. 1991;105:921–923. doi: 10.1017/s0022215100117827. [DOI] [PubMed] [Google Scholar]
- 7.Marks SC, Latoni JD, Mathog RH. Mucoceles of the maxillary sinus. Otolaryngol Head Neck Surg. 1997;117:18–21. doi: 10.1016/S0194-59989770200-6. [DOI] [PubMed] [Google Scholar]
- 8.Arrué P, Kany MT, Serrano E, Lacroix F, Percodani J, Yardeni E, et al. Mucoceles of the paranasal sinuses: uncommon location. J Larlyngol Otol. 1998;112:840–844. doi: 10.1017/s0022215100141854. [DOI] [PubMed] [Google Scholar]
- 9.Song HM, Park HW, Chung YS, Jang YJ, Lee BJ. Primary mucoceles of the maxillary sinus. Korean J Otolaryngol - Head Neck Surg. 2006;49:47–51. [Google Scholar]
- 10.Kaneshiro S, Nakajima T, Yoshikawa Y, Iwasaki H, Tokiwa N. The postoperative maxillary cyst: report of 71 cases. J Oral Surg. 1981;39:191–198. [PubMed] [Google Scholar]
- 11.Athevino CC, Atherino TC. Maxillary sinus mucocele. Arch Otolaryngol. 1984;110:200–202. doi: 10.1001/archotol.1984.00800290064014. [DOI] [PubMed] [Google Scholar]
- 12.Barzilai G, Greenberg E, Uri N. Indications for the Caldwell-Luc approach in the endoscopic era. Otolaryngol Head Neck Surg. 2005;132:219–220. doi: 10.1016/j.otohns.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Har-El G, Balwally AN, Lucente FE. Sinus mucoceles: is marsupialization enough? Otolaryngol Head Neck Surg. 1997;117:633–640. doi: 10.1016/S0194-59989770045-7. [DOI] [PubMed] [Google Scholar]
- 14.Cutler JL, Duncavage JA, Matheny K, Cross JL, Miman MC, Oh CK. Results of Caldwell-Luc after failed endoscopic middle meatus antrostomy in patients with chronic sinusitis. Laryngoscope. 2003;113:2148–2150. doi: 10.1097/00005537-200312000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Richtsmeier WJ. Top 10 reasons for endoscopic maxillary sinus surgery failure. Laryngoscope. 2001;111:1952–1956. doi: 10.1097/00005537-200111000-00015. [DOI] [PubMed] [Google Scholar]